Tissue-Engineered Nanomaterials Play Diverse Roles in Bone Injury Repair
Abstract
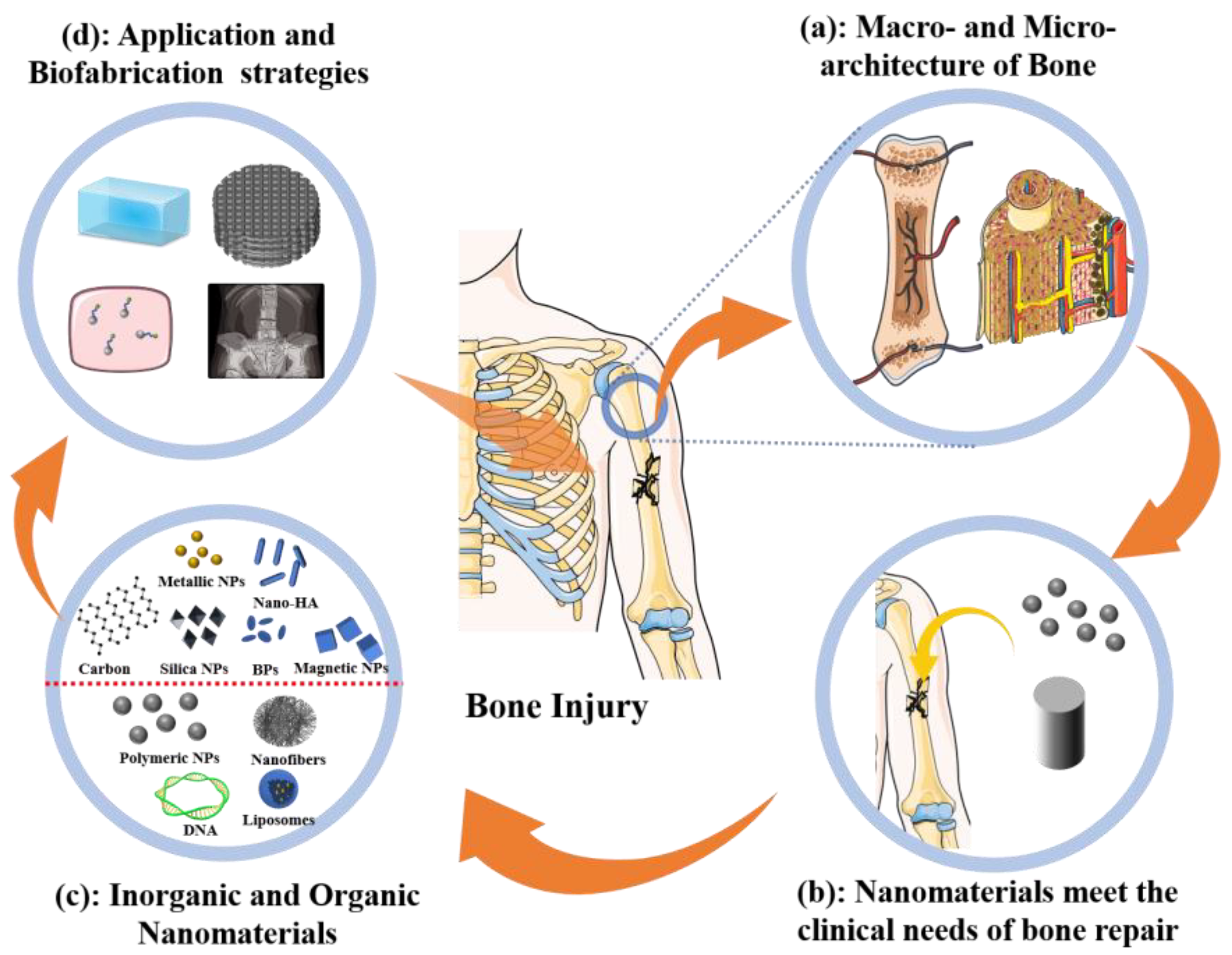
:1. Introduction
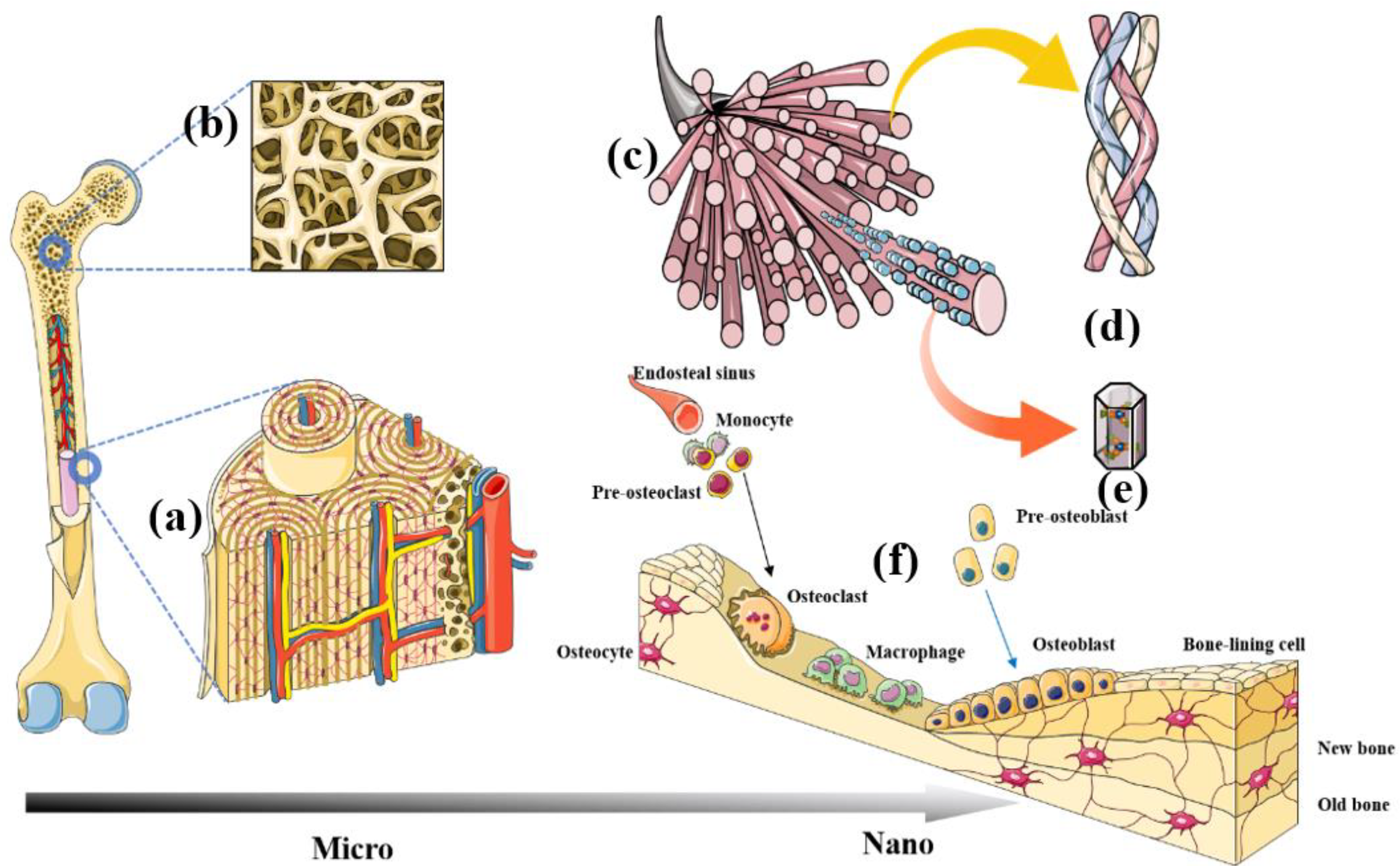
2. Macro- and Nano-Hierarchical Architecture of Natural Bone
2.1. Macroscopic Architecture
2.1.1. Cortical Bone
2.1.2. Trabecular Bone
2.2. Nano Architecture
2.2.1. Bone Biomineral Matrix
2.2.2. Bone Cells
3. Required Clinical Features of Nanoscaled Materials
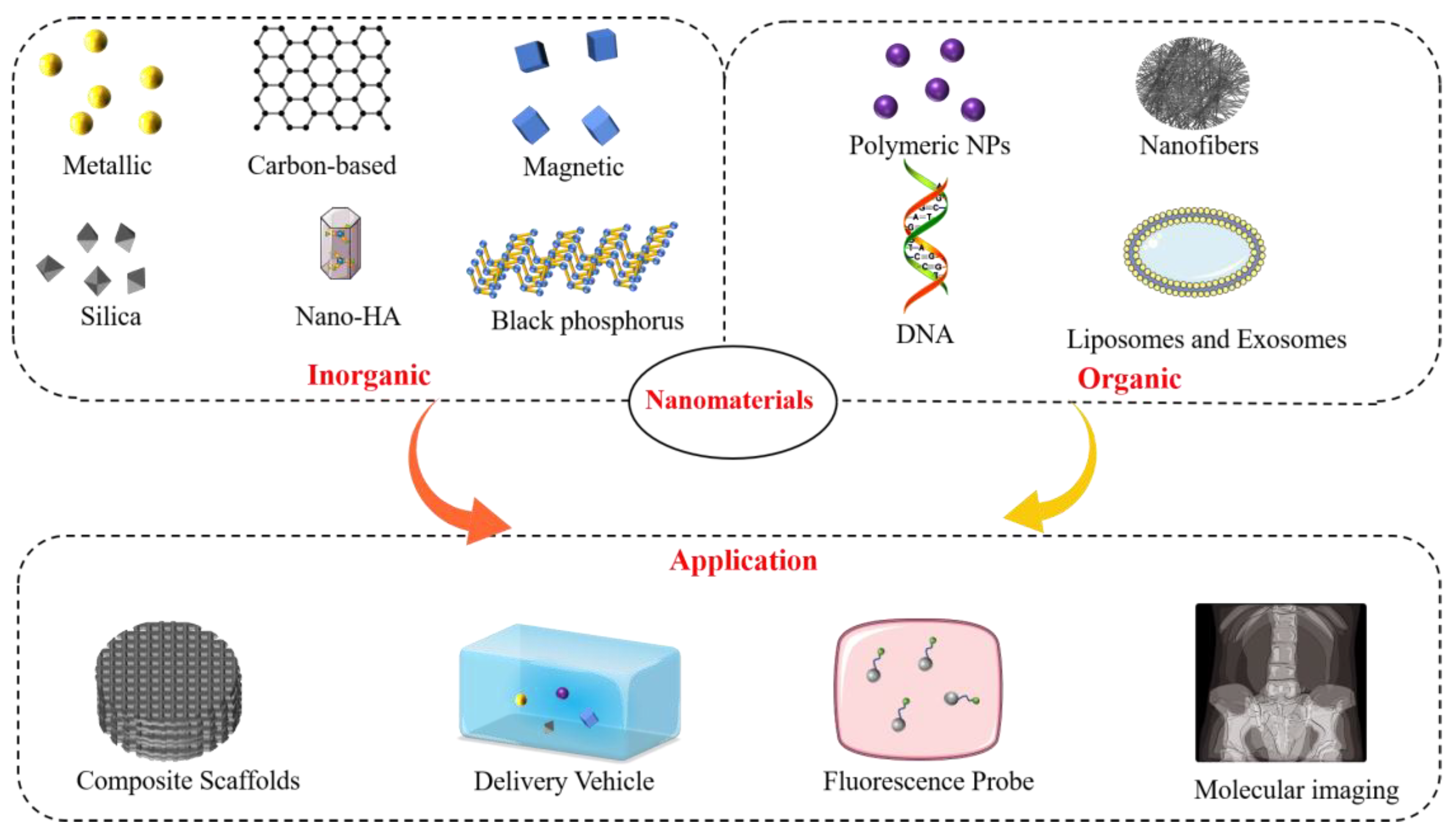
4. Nanomaterials in Bone Tissue Engineering
4.1. Inorganic Nanomaterials
4.1.1. Metallic Nanoparticles
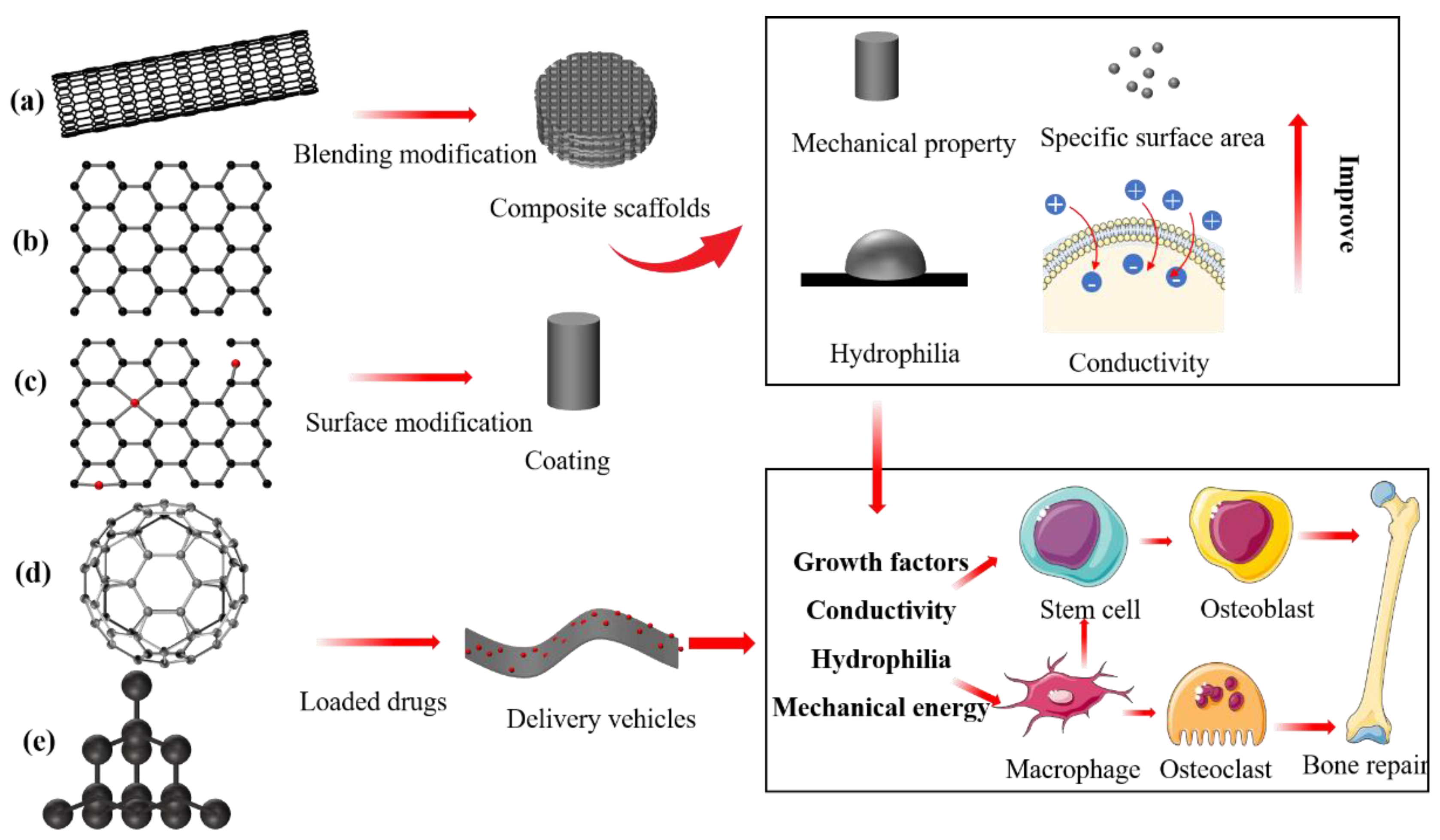
4.1.2. Carbon-Based Nanomaterials
4.1.3. Silica Nanoparticles
4.1.4. Nano-HAp and Other Bone Mineral Substitutes
4.1.5. Black Phosphorus
4.1.6. Magnetic Nanoparticles
4.1.7. Nanoclays
4.2. Organic Nanomaterials
4.2.1. Polymeric Nanoparticles
4.2.2. Polymeric Nanofibres
4.2.3. DNA Nanomaterials
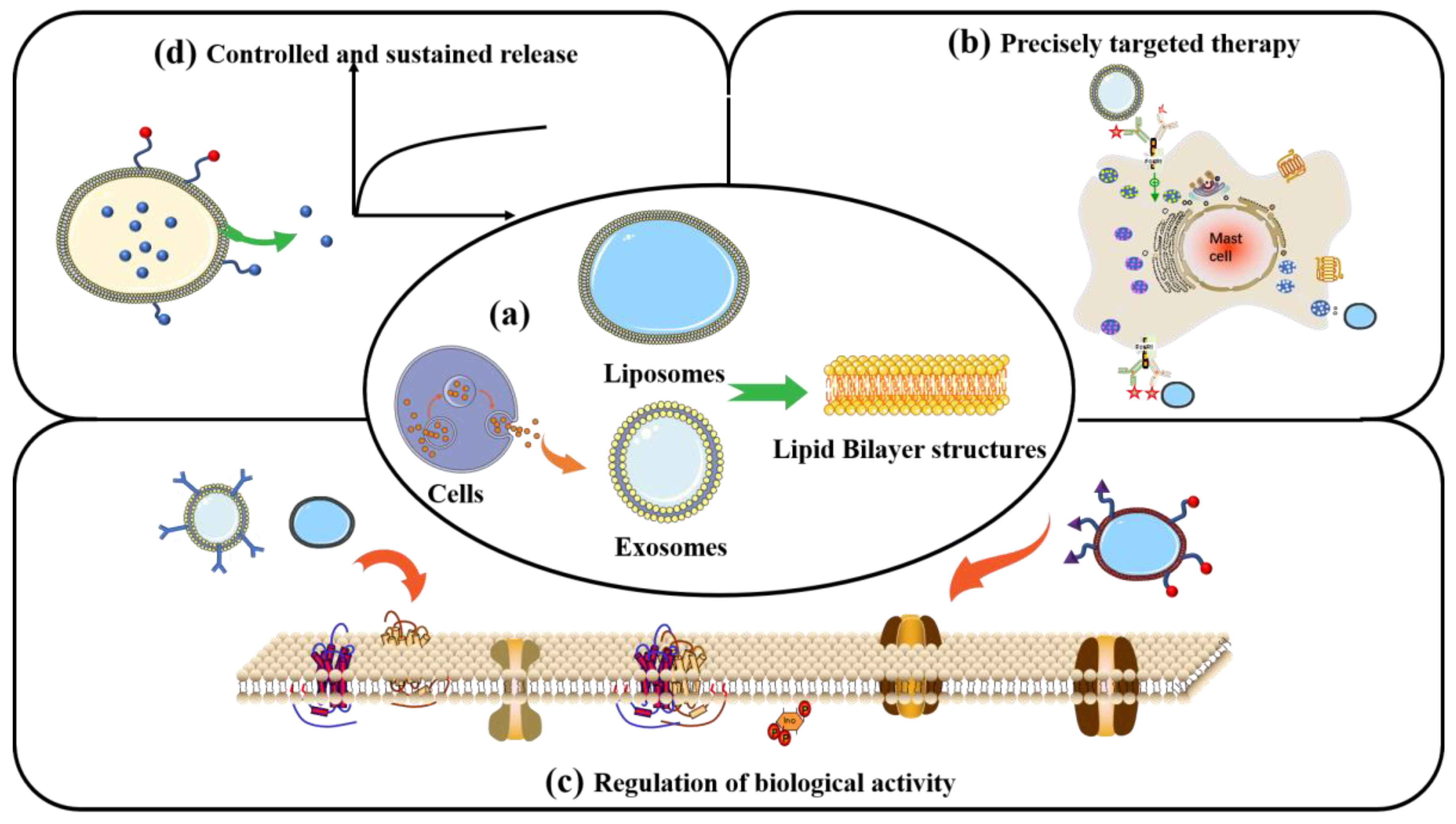
4.2.4. Liposomes and Exosomes
5. Summary and Perspectives
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Liu, Y.; Luo, D.; Wang, T. Hierarchical Structures of Bone and Bioinspired Bone Tissue Engineering. Small 2016, 12, 4611–4632. [Google Scholar] [CrossRef] [PubMed]
- Peng, Z.; Zhao, T.; Zhou, Y.; Li, S.; Li, J.; Leblanc, R.M. Bone Tissue Engineering via Carbon-Based Nanomaterials. Adv. Healthc. Mater. 2020, 9, 1901495. [Google Scholar] [CrossRef]
- Behzadi, S.; Luther, G.A.; Harris, M.B.; Farokhzad, O.C.; Mahmoudi, M. Nanomedicine for safe healing of bone trauma: Opportunities and challenges. Biomaterials 2017, 146, 168–182. [Google Scholar] [CrossRef] [PubMed]
- Wei, Y.; Zhu, G.; Zhao, Z.; Yin, C.; Zhao, Q.; Xu, H.; Wang, J.; Zhang, J.; Zhang, X.; Zhang, Y.; et al. Individualized plasticity autograft mimic with efficient bioactivity inducing osteogenesis. Int. J. Oral Sci. 2021, 13, 14. [Google Scholar] [CrossRef] [PubMed]
- Babuska, V.; Kasi, P.B.; Chocholata, P.; Wiesnerova, L.; Dvorakova, J.; Vrzakova, R.; Nekleionova, A.; Landsmann, L.; Kulda, V. Nanomaterials in Bone Regeneration. Appl. Sci. 2022, 12, 6793. [Google Scholar] [CrossRef]
- Kreyling, W.G.; Semmler-Behnke, M.; Chaudhry, Q. A complementary definition of nanomaterial. Nano Today 2010, 5, 165–168. [Google Scholar] [CrossRef]
- Xie, S.; Ai, L.; Cui, C.; Fu, T.; Cheng, X.; Qu, F.; Tan, W. Functional Aptamer-Embedded Nanomaterials for Diagnostics and Therapeutics. ACS Appl. Mater. Interfaces 2021, 13, 9542–9560. [Google Scholar] [CrossRef]
- Wang, Q.; Yan, J.; Yang, J.; Li, B. Nanomaterials promise better bone repair. Mater. Today 2016, 19, 451–463. [Google Scholar] [CrossRef]
- Micheletti, C.; Hurley, A.; Gourrier, A.; Palmquist, A.; Tang, T.; Shah, F.A.; Grandfield, K. Bone mineral organization at the mesoscale: A review of mineral ellipsoids in bone and at bone interfaces. Acta Biomater. 2022, 142, 1–13. [Google Scholar] [CrossRef]
- Hoffseth, K.; Busse, E.; Jaramillo, J.; Simkin, J.; Lacey, M.; Sammarco, M.C. Age-Dependent Changes in Bone Architecture, Patterning, and Biomechanics during Skeletal Regeneration. Front. Cell Dev. Biol. 2021, 9, 749055. [Google Scholar] [CrossRef]
- Carnelli, D.; Vena, P.; Dao, M.; Ortiz, C.; Contro, R. Orientation and size-dependent mechanical modulation within individual secondary osteons in cortical bone tissue. J. R. Soc. Interface 2013, 10, 953. [Google Scholar] [CrossRef]
- Cai, X.; Follet, H.; Peralta, L.; Gardegaront, M.; Farlay, D.; Gauthier, R.; Yu, B.; Gineyts, E.; Olivier, C.; Langer, M.; et al. Anisotropic elastic properties of human femoral cortical bone and relationships with composition and microstructure in elderly. Acta Biomater. 2019, 90, 254–266. [Google Scholar] [CrossRef] [PubMed]
- Chang, B.; Liu, X. Osteon: Structure, Turnover, and Regeneration. Tissue Eng. Part B Rev. 2022, 28, 261–278. [Google Scholar] [CrossRef] [PubMed]
- Yu, Y.E.; Hu, Y.J.; Zhou, B.; Wang, J.; Guo, X.E. Microstructure Determines Apparent-Level Mechanics Despite Tissue-Level Anisotropy and Heterogeneity of Individual Plates and Rods in Normal Human Trabecular Bone. J. Bone Miner. Res. 2021, 36, 1796–1807. [Google Scholar] [CrossRef] [PubMed]
- Wittig, N.K.; Palle, J.; Østergaard, M.; Frølich, S.; Birkbak, M.E.; Spiers, K.M.; Garrevoet, J.; Birkedal, H. Bone Biomineral Properties Vary across Human Osteonal Bone. ACS Nano 2019, 13, 12949–12956. [Google Scholar] [CrossRef] [PubMed]
- Evans, J.S. The Biomineralization Proteome: Protein Complexity for a Complex Bioceramic Assembly Process. Proteomics 2019, 19, 1900036. [Google Scholar] [CrossRef]
- He, K.; Sawczyk, M.; Liu, C.; Yuan, Y.; Song, B.; Deivanayagam, R.; Nie, A.; Hu, X.; Dravid, V.P.; Lu, J.; et al. Revealing nanoscale mineralization pathways of hydroxyapatite using in situ liquid cell transmission electron microscopy. Sci. Adv. 2020, 6, eaaz7524. [Google Scholar] [CrossRef]
- Du, M.; Chen, J.; Liu, K.; Xing, H.; Song, C. Recent advances in biomedical engineering of nano-hydroxyapatite including dentistry, cancer treatment and bone repair. Compos. Part B-Eng. 2021, 215, 108790. [Google Scholar] [CrossRef]
- Zhang, D.; Wu, X.; Chen, J.; Lin, K. The development of collagen based composite scaffolds for bone regeneration. Bioact. Mater. 2018, 3, 129–138. [Google Scholar] [CrossRef]
- Tang, G.; Liu, Z.; Liu, Y.; Yu, J.; Wang, X.; Tan, Z.; Ye, X. Recent Trends in the Development of Bone Regenerative Biomaterials. Front. Cell Dev. Biol. 2021, 9, 665813. [Google Scholar] [CrossRef]
- Capulli, M.; Paone, R.; Rucci, N. Osteoblast and osteocyte: Games without frontiers. Arch. Biochem. Biophys. 2014, 561, 3–12. [Google Scholar] [CrossRef] [PubMed]
- Trejo, I.; Kojouharov, H.V. Understanding the Fundamental Molecular Mechanism of Osteogenic Differentiation from Mesenchymal Stem Cells. Appl. Appl. Math. 2019, 14, 687–698. [Google Scholar]
- Florencio-Silva, R.; da Silva Sasso, G.R.; Sasso-Cerri, E.; Simões, M.J.; Cerri, P.S. Biology of Bone Tissue: Structure, Function, and Factors That Influence Bone Cells. Biomed Res. Int. 2015, 2015, 421746. [Google Scholar] [CrossRef]
- Sims, N.A.; Martin, T.J. Osteoclasts Provide Coupling Signals to Osteoblast Lineage Cells Through Multiple Mechanisms. Annu. Rev. Physiol. 2020, 82, 507–529. [Google Scholar] [CrossRef]
- Schaffler, M.B.; Cheung, W.-Y.; Majeska, R.; Kennedy, O. Osteocytes: Master Orchestrators of Bone. Calcif. Tissue Int. 2014, 94, 5–24. [Google Scholar] [CrossRef] [PubMed]
- Shah, F.A.; Thomsen, P.; Palmquist, A. A Review of the Impact of Implant Biomaterials on Osteocytes. J. Dent. Res. 2018, 97, 977–986. [Google Scholar] [CrossRef] [PubMed]
- Park, Y.; Cheong, E.; Kwak, J.-G.; Carpenter, R.; Shim, J.-H.; Lee, J. Trabecular bone organoid model for studying the regulation of localized bone remodeling. Sci. Adv. 2021, 7, eabd6495. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.-Y.; Jeon, H.H.; Alshabab, A.; Lee, Y.J.; Chung, C.-H.; Graves, D.T. RANKL deletion in periodontal ligament and bone lining cells blocks orthodontic tooth movement. Int. J. Oral Sci. 2018, 10, 3. [Google Scholar] [CrossRef]
- Clarke, B. Normal Bone Anatomy and Physiology. Clin. J. Am. Soc. Nephrol. 2008, 3, S131–S139. [Google Scholar] [CrossRef]
- Veis, D.J.; O’Brien, C.A. Osteoclasts, Master Sculptors of Bone. Annu. Rev. Pathol. 2023, 18, 257–281. [Google Scholar] [CrossRef]
- Chun, Y.S.; Lee, D.H.; Won, T.G.; Kim, Y.; Shetty, A.A.; Kim, S.J. Current Modalities for Fracture Healing Enhancement. Tissue Eng. Regen. Med. 2022, 19, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Wu, D.; Wang, Z.; Wang, J.; Geng, Y.; Zhang, Z.; Li, Y.; Li, Q.; Zheng, Z.; Cao, Y.; Zhang, Z.-Y. Development of a micro-tissue-mediated injectable bone tissue engineering strategy for large segmental bone defect treatment. Stem Cell Res. Ther. 2018, 9, 331. [Google Scholar] [CrossRef] [PubMed]
- Wiss, D.A.; Garlich, J.M. Healing the Index Humeral Shaft Nonunion: Risk Factors for Development of a Recalcitrant Nonunion in 125 Patients. J. Bone Jt. Surg. 2020, 102, 375–380. [Google Scholar] [CrossRef]
- Asmatulu, E.; Andalib, M.N.; Subeshan, B.; Abedin, F. Impact of nanomaterials on human health: A review. Environ. Chem. Lett. 2022, 20, 2509–2529. [Google Scholar] [CrossRef]
- Ren, S.; Zhou, Y.; Zheng, K.; Xu, X.; Yang, J.; Wang, X.; Miao, L.; Wei, H.; Xu, Y. Cerium oxide nanoparticles loaded nanofibrous membranes promote bone regeneration for periodontal tissue engineering. Bioact. Mater. 2022, 7, 242–253. [Google Scholar] [CrossRef] [PubMed]
- Bianchi, E.; Vigani, B.; Viseras, C.; Ferrari, F.; Rossi, S.; Sandri, G. Inorganic Nanomaterials in Tissue Engineering. Pharmaceutics 2022, 14, 1127. [Google Scholar] [CrossRef]
- Gandhi, S.; Shende, P. Cyclodextrins-modified metallic nanoparticles for effective cancer therapy. J. Control. Release 2021, 339, 41–50. [Google Scholar] [CrossRef]
- Nechifor, G.; Eftimie Totu, E.; Nechifor, A.C.; Isildak, I.; Oprea, O.; Cristache, C.M. Non-Resorbable Nanocomposite Membranes for Guided Bone Regeneration Based on Polysulfone-Quartz Fiber Grafted with Nano-TiO2. Nanomaterials 2019, 9, 985. [Google Scholar] [CrossRef]
- Kim, H.J.; Lee, S.; Park, J.M.; Cho, H.B.; Park, J.-I.; Park, J.S.; Park, K.-H. Development of a three-layer consecutive gene delivery system for enhanced bone regeneration. Biomaterials 2021, 277, 121104. [Google Scholar] [CrossRef]
- Mastrogiacomo, S.; Dou, W.; Koshkina, O.; Boerman, O.C.; Jansen, J.A.; Heerschap, A.; Srinivas, M.; Walboomers, X.F. Perfluorocarbon/Gold Loading for Noninvasive in Vivo Assessment of Bone Fillers Using 19F Magnetic Resonance Imaging and Computed Tomography. ACS Appl. Mater. Interfaces 2017, 9, 22149–22159. [Google Scholar] [CrossRef]
- Stabryla, L.M.; Johnston, K.A.; Diemler, N.A.; Cooper, V.S.; Millstone, J.E.; Haig, S.-J.; Gilbertson, L.M. Role of bacterial motility in differential resistance mechanisms of silver nanoparticles and silver ions. Nat. Nanotechnol. 2021, 16, 996–1003. [Google Scholar] [CrossRef]
- Abdelaziz, D.; Hefnawy, A.; Al-Wakeel, E.; El-Fallal, A.; El-Sherbiny, I.M. New biodegradable nanoparticles-in-nanofibers based membranes for guided periodontal tissue and bone regeneration with enhanced antibacterial activity. J. Adv. Res. 2021, 28, 51–62. [Google Scholar] [CrossRef]
- Shuai, C.; Liu, G.; Yang, Y.; Qi, F.; Peng, S.; Yang, W.; He, C.; Wang, G.; Qian, G. A strawberry-like Ag-decorated barium titanate enhances piezoelectric and antibacterial activities of polymer scaffold. Nano Energy 2020, 74, 104825. [Google Scholar] [CrossRef]
- Li, Z.; Wang, L.; Li, Y.; Feng, Y.; Feng, W. Carbon-based functional nanomaterials: Preparation, properties and applications. Compos. Sci. Technol. 2019, 179, 10–40. [Google Scholar] [CrossRef]
- Liu, H.; Chen, J.; Qiao, S.; Zhang, W. Carbon-Based Nanomaterials for Bone and Cartilage Regeneration: A Review. ACS Biomater. Sci. Eng. 2021, 7, 4718–4735. [Google Scholar] [CrossRef] [PubMed]
- Xin, Q.; Shah, H.; Nawaz, A.; Xie, W.; Akram, M.Z.; Batool, A.; Tian, L.; Jan, S.U.; Boddula, R.; Guo, B.; et al. Antibacterial Carbon-Based Nanomaterials. Adv. Mater. 2019, 31, 1804838. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Jiang, X.; Li, Y.; Jin, W.; Huang, X. Construction of halogenated graphenes by halogenation of hydrogenated graphene. Compos. Commun. 2021, 25, 100771. [Google Scholar] [CrossRef]
- Yildiz, G.; Bolton-Warberg, M.; Awaja, F. Graphene and graphene oxide for bio-sensing: General properties and the effects of graphene ripples. Acta Biomater. 2021, 131, 62–79. [Google Scholar] [CrossRef] [PubMed]
- Shuai, C.; Feng, P.; Wu, P.; Liu, Y.; Liu, X.; Lai, D.; Gao, C.; Peng, S. A combined nanostructure constructed by graphene and boron nitride nanotubes reinforces ceramic scaffolds. Chem. Eng. J. 2017, 313, 487–497. [Google Scholar] [CrossRef]
- Li, Y.; Yang, L.; Hou, Y.; Zhang, Z.; Chen, M.; Wang, M.; Liu, J.; Wang, J.; Zhao, Z.; Xie, C.; et al. Polydopamine-mediated graphene oxide and nanohydroxyapatite-incorporated conductive scaffold with an immunomodulatory ability accelerates periodontal bone regeneration in diabetes. Bioact. Mater. 2022, 18, 213–227. [Google Scholar] [CrossRef]
- Cheng, Z.; Landish, B.; Chi, Z.; Nannan, C.; Jingyu, D.; Sen, L.; Xiangjin, L. 3D printing hydrogel with graphene oxide is functional in cartilage protection by influencing the signal pathway of Rank/Rankl/OPG. Mater. Sci. Eng. C 2018, 82, 244–252. [Google Scholar] [CrossRef] [PubMed]
- Mahanta, A.K.; Patel, D.K.; Maiti, P. Nanohybrid Scaffold of Chitosan and Functionalized Graphene Oxide for Controlled Drug Delivery and Bone Regeneration. ACS Biomater. Sci. Eng. 2019, 5, 5139–5149. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.; Kim, W.J. Photothermally Controlled Gene Delivery by Reduced Graphene Oxide-Polyethylenimine Nanocomposite. Small 2014, 10, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Liu, F.; Xue, L.; Xu, L.; Liu, J.; Xie, C.; Chen, C.; Liu, Y. Preparation and characterization of bovine serum albumin nanoparticles modified by Poly-l-lysine functionalized graphene oxide for BMP-2 delivery. Mater. Des. 2022, 215, 110479. [Google Scholar] [CrossRef]
- Wei, N.; Tian, Y.; Liao, Y.; Komatsu, N.; Gao, W.; Lyuleeva-Husemann, A.; Zhang, Q.; Hussain, A.; Ding, E.; Yao, F.; et al. Colors of Single-Wall Carbon Nanotubes. Adv. Mater. 2021, 33, 2006395. [Google Scholar] [CrossRef]
- Asl, M.A.; Karbasi, S.; Beigi-Boroujeni, S.; Benisi, S.Z.; Saeed, M. Polyhydroxybutyrate-starch/carbon nanotube electrospun nanocomposite: A highly potential scaffold for bone tissue engineering applications. Int. J. Biol. Macromol. 2022, 223, 524–542. [Google Scholar] [CrossRef]
- Rodrigues, B.V.M.; Razzino, C.A.; Oliveira, F.D.C.; Marciano, F.R.; Lobo, A.O. On the design and properties of scaffolds based on vertically aligned carbon nanotubes transferred onto electrospun poly (lactic acid) fibers. Mater. Des. 2017, 127, 183–192. [Google Scholar] [CrossRef]
- Nazeri, N.; Derakhshan, M.A.; Faridi-Majidi, R.; Ghanbari, H. Novel electro-conductive nanocomposites based on electrospun PLGA/CNT for biomedical applications. J. Mater. Sci. Mater. Med. 2018, 29, 168. [Google Scholar] [CrossRef]
- Wang, Y.; Mei, Y.; Wang, Q.; Wei, W.; Huang, F.; Li, Y.; Li, J.Y.; Zhou, Z.W. Improved fracture toughness and ductility of PLA composites by incorporating a small amount of surface-modified helical carbon nanotubes. Compos. Part B Eng. 2019, 162, 54–61. [Google Scholar] [CrossRef]
- Janjua, T.I.; Cao, Y.; Yu, C.; Popat, A. Clinical translation of silica nanoparticles. Nat. Rev. Mater. 2021, 6, 1072–1074. [Google Scholar] [CrossRef] [PubMed]
- Bagheri, E.; Ansari, L.; Abnous, K.; Taghdisi, S.M.; Charbgoo, F.; Ramezani, M.; Alibolandi, M. Silica based hybrid materials for drug delivery and bioimaging. J. Control. Release 2018, 277, 57–76. [Google Scholar] [CrossRef] [PubMed]
- Xu, X.; Sun, M.; Wang, D.; Bu, W.; Wang, Z.; Shen, Y.; Zhang, K.; Zhou, D.; Yang, B.; Sun, H. Bone formation promoted by bone morphogenetic protein-2 plasmid-loaded porous silica nanoparticles with the involvement of autophagy. Nanoscale 2019, 11, 21953–21963. [Google Scholar] [CrossRef]
- Cheng, Y.; Cheng, G.; Xie, C.; Yin, C.; Dong, X.; Li, Z.; Zhou, X.; Wang, Q.; Deng, H.; Li, Z. Biomimetic Silk Fibroin Hydrogels Strengthened by Silica Nanoparticles Distributed Nanofibers Facilitate Bone Repair. Adv. Healthc. Mater. 2021, 10, 2001646. [Google Scholar] [CrossRef]
- Shen, M.; Wang, L.; Feng, L.; Gao, Y.; Li, S.; Wu, Y.; Xu, C.; Pei, G. bFGF-Loaded Mesoporous Silica Nanoparticles Promote Bone Regeneration Through the Wnt/β-Catenin Signalling Pathway. Int. J. Nanomed. 2022, 17, 2593–2608. [Google Scholar] [CrossRef]
- Martín-Moldes, Z.; Barreiro, D.L.; Buehler, M.J.; Kaplan, D.L. Effect of the silica nanoparticle size on the osteoinduction of biomineralized silk-silica nanocomposites. Acta Biomater. 2021, 120, 203–212. [Google Scholar] [CrossRef]
- Sutthavas, P.; Birgani, Z.T.; Habibovic, P.; van Rijt, S. Calcium Phosphate-Coated and Strontium-Incorporated Mesoporous Silica Nanoparticles Can Effectively Induce Osteogenic Stem Cell Differentiation. Adv. Healthc. Mater. 2022, 11, 2101588. [Google Scholar] [CrossRef]
- Arcos, D.; Vallet-Regí, M. Substituted hydroxyapatite coatings of bone implants. J. Mater. Chem. B 2020, 8, 1781–1800. [Google Scholar] [CrossRef]
- Murugan, R.; Ramakrishna, S. Bioresorbable composite bone paste using polysaccharide based nano hydroxyapatite. Biomaterials 2004, 25, 3829–3835. [Google Scholar] [CrossRef]
- Bas, M.; Daglilar, S.; Kuskonmaz, N.; Kalkandelen, C.; Erdemir, G.; Kuruca, S.E.; Tulyaganov, D.; Yoshioka, T.; Gunduz, O.; Ficai, D.; et al. Mechanical and Biocompatibility Properties of Calcium Phosphate Bioceramics Derived from Salmon Fish Bone Wastes. Int. J. Mol. Sci. 2020, 21, 8082. [Google Scholar] [CrossRef]
- Busuioc, C.; Isopencu, G.; Banciu, A.; Banciu, D.-D.; Oprea, O.; Mocanu, A.; Deleanu, I.; Zăuleţ, M.; Popescu, L.; Tănăsuică, R.; et al. Bacterial Cellulose Hybrid Composites with Calcium Phosphate for Bone Tissue Regeneration. Int. J. Mol. Sci. 2022, 23, 16180. [Google Scholar] [CrossRef]
- Ardelean, I.L.; Gudovan, D.; Ficai, D.; Ficai, A.; Andronescu, E.; Albu-Kaya, M.G.; Neacsu, P.; Ion, R.N.; Cimpean, A.; Mitran, V. Collagen/hydroxyapatite bone grafts manufactured by homogeneous/heterogeneous 3D printing. Mater. Lett. 2018, 231, 179–182. [Google Scholar] [CrossRef]
- Hu, Y.; Cao, S.; Chen, J.; Zhao, Y.; He, F.; Li, Q.; Zou, L.; Shi, C. Biomimetic fabrication of icariin loaded nano hydroxyapatite reinforced bioactive porous scaffolds for bone regeneration. Chem. Eng. J. 2020, 394, 124895. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, J.; Gao, R.; Liu, X.; Feng, Z.; Zhang, C.; Huang, P.; Dong, A.; Kong, D.; Wang, W. Biomimetic glycopeptide hydrogel coated PCL/nHA scaffold for enhanced cranial bone regeneration via macrophage M2 polarization-induced osteo-immunomodulation. Biomaterials 2022, 285, 121538. [Google Scholar] [CrossRef]
- Tamburaci, S.; Tihminlioglu, F. Development of Si doped nano hydroxyapatite reinforced bilayer chitosan nanocomposite barrier membranes for guided bone regeneration. Mater. Sci. Eng. C 2021, 128, 112298. [Google Scholar] [CrossRef] [PubMed]
- Garbo, C.; Locs, J.; D’Este, M.; Demazeau, G.; Mocanu, A.; Roman, C.; Horovitz, O.; Tomoaia-Cotisel, M. Advanced Mg, Zn, Sr, Si Multi-Substituted Hydroxyapatites for Bone Regeneration. Int. J. Nanomed. 2020, 15, 1037–1058. [Google Scholar] [CrossRef]
- Park, J.-W.; Hwang, J.-U.; Back, J.-H.; Jang, S.-W.; Kim, H.-J.; Kim, P.-S.; Shin, S.; Kim, T. High strength PLGA/Hydroxyapatite composites with tunable surface structure using PLGA direct grafting method for orthopedic implants. Compos. Part B-Eng. 2019, 178, 107449. [Google Scholar] [CrossRef]
- Wei, J.; Yan, Y.; Gao, J.; Li, Y.; Wang, R.; Wang, J.; Zou, Q.; Zuo, Y.; Zhu, M.; Li, J. 3D-printed hydroxyapatite microspheres reinforced PLGA scaffolds for bone regeneration. Biomater. Adv. 2022, 133, 112618. [Google Scholar] [CrossRef]
- Chen, S.; Guo, R.; Xie, C.; Liang, Q.; Xiao, X. Biomimetic mineralization of nanocrystalline hydroxyapatites on aminated modified polylactic acid microspheres to develop a novel drug delivery system for alendronate. Mater. Sci. Eng. C 2020, 110, 110655. [Google Scholar] [CrossRef]
- Zhao, D.-W.; Fan, X.-C.; Zhao, Y.-X.; Zhao, W.; Zhang, Y.-Q.; Zhang, R.-H.; Cheng, L. Biocompatible Nano-Hydroxyapatites Regulate Macrophage Polarization. Materials 2022, 15, 6986. [Google Scholar] [CrossRef]
- Qing, Y.; Li, R.; Li, S.; Li, Y.; Wang, X.; Qin, Y. Advanced Black Phosphorus Nanomaterials for Bone Regeneration. Int. J. Nanomed. 2020, 15, 2045–2058. [Google Scholar] [CrossRef]
- Tan, L.; Li, M.; Luo, Z.; Cai, K.; Hu, Y. Black phosphorus biomaterials for photo-controlled bone tissue engineering. Compos. Part B-Eng. 2022, 246, 110245. [Google Scholar] [CrossRef]
- Huang, K.; Wu, J.; Gu, Z. Black Phosphorus Hydrogel Scaffolds Enhance Bone Regeneration via a Sustained Supply of Calcium-Free Phosphorus. ACS Appl. Mater. Interfaces 2019, 11, 2908–2916. [Google Scholar] [CrossRef]
- Venuthurumilli, P.K.; Ye, P.D.; Xu, X. Plasmonic Resonance Enhanced Polarization-Sensitive Photodetection by Black Phosphorus in Near Infrared. ACS Nano 2018, 12, 4861–4867. [Google Scholar] [CrossRef]
- Chen, W.; Ouyang, J.; Liu, H.; Chen, M.; Zeng, K.; Sheng, J.; Liu, Z.; Han, Y.; Wang, L.; Li, J.; et al. Black Phosphorus Nanosheet-Based Drug Delivery System for Synergistic Photodynamic/Photothermal/Chemotherapy of Cancer. Adv. Mater. 2017, 29, 1603864. [Google Scholar] [CrossRef] [PubMed]
- Cheng, L.; Chen, Z.; Cai, Z.; Zhao, J.; Lu, M.; Liang, J.; Wang, F.; Qi, J.; Cui, W.; Deng, L. Bioinspired Functional Black Phosphorus Electrospun Fibers Achieving Recruitment and Biomineralization for Staged Bone Regeneration. Small 2020, 16, 2005433. [Google Scholar] [CrossRef] [PubMed]
- Dong, W.; Wang, H.; Liu, H.; Zhou, C.; Zhang, X.; Wang, S.; He, L. Potential of Black Phosphorus in Immune-Based Therapeutic Strategies. Bioinorg. Chem. Appl. 2022, 2022, 3790097. [Google Scholar] [CrossRef]
- Wang, X.; Shao, J.; Abd El Raouf, M.; Xie, H.; Huang, H.; Wang, H.; Chu, P.K.; Yu, X.-F.; Yang, Y.; AbdEl-Aal, A.M.; et al. Near-infrared light-triggered drug delivery system based on black phosphorus for in vivo bone regeneration. Biomaterials 2018, 179, 164–174. [Google Scholar] [CrossRef]
- Ma, W.; Lu, J.; Wan, B.; Peng, D.; Xu, Q.; Hu, G.; Peng, Y.; Pan, C.; Wang, Z.L. Piezoelectricity in Multilayer Black Phosphorus for Piezotronics and Nanogenerators. Adv. Mater. 2020, 32, 1905795. [Google Scholar] [CrossRef]
- Guo, T.; Lin, M.; Huang, J.; Zhou, C.; Tian, W.; Yu, H.; Jiang, X.; Ye, J.; Shi, Y.; Xiao, Y.; et al. The Recent Advances of Magnetic Nanoparticles in Medicine. J. Nanomater. 2018, 2018, 7805147. [Google Scholar] [CrossRef]
- Xia, Y.; Sun, J.; Zhao, L.; Zhang, F.; Liang, X.-J.; Guo, Y.; Weir, M.D.; Reynolds, M.A.; Gu, N.; Xu, H.H.K. Magnetic field and nano-scaffolds with stem cells to enhance bone regeneration. Biomaterials 2018, 183, 151–170. [Google Scholar] [CrossRef]
- Farzin, A.; Hassan, S.; Emadi, R.; Etesami, S.A.; Ai, J. Comparative evaluation of magnetic hyperthermia performance and biocompatibility of magnetite and novel Fe-doped hardystonite nanoparticles for potential bone cancer therapy. Mater. Sci. Eng. C 2019, 98, 930–938. [Google Scholar] [CrossRef] [PubMed]
- Shuai, C.; Yang, W.; He, C.; Peng, S.; Gao, C.; Yang, Y.; Qi, F.; Feng, P. A magnetic micro-environment in scaffolds for stimulating bone regeneration. Mater. Des. 2020, 185, 108275. [Google Scholar] [CrossRef]
- Li, Y.; Huang, L.; Tai, G.; Yan, F.; Cai, L.; Xin, C.; Al Islam, S. Graphene Oxide-loaded magnetic nanoparticles within 3D hydrogel form High-performance scaffolds for bone regeneration and tumour treatment. Compos. Part A Appl. Sci. Manuf. 2022, 152, 106672. [Google Scholar] [CrossRef]
- Strbak, O.; Antal, I.; Khmara, I.; Koneracka, M.; Kubovcikova, M.; Zavisova, V.; Molcan, M.; Jurikova, A.; Hnilicova, P.; Gombos, J.; et al. Influence of Dextran Molecular Weight on the Physical Properties of Magnetic Nanoparticles for Hyperthermia and MRI Applications. Nanomaterials 2020, 10, 2468. [Google Scholar] [CrossRef] [PubMed]
- Campodoni, E.; Velez, M.; Fragogeorgi, E.; Morales, I.; de la Presa, P.; Stanicki, D.; Dozio, S.M.; Xanthopoulos, S.; Bouziotis, P.; Dermisiadou, E.; et al. Magnetic and radio-labeled bio-hybrid scaffolds to promote and track in vivo the progress of bone regeneration. Biomater. Sci. 2021, 9, 7575–7590. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.-S.; Hwang, H.S.; Kim, S.; Fan, J.; Aghaloo, T.; Lee, M. Inspired by Nature: Facile Design of Nanoclay–Organic Hydrogel Bone Sealant with Multifunctional Properties for Robust Bone Regeneration. Adv. Funct. Mater. 2020, 30, 2003717. [Google Scholar] [CrossRef]
- Long, M.; Zhang, Y.; Huang, P.; Chang, S.; Hu, Y.; Yang, Q.; Mao, L.; Yang, H. Emerging Nanoclay Composite for Effective Hemostasis. Adv. Funct. Mater. 2018, 28, 1704452. [Google Scholar] [CrossRef]
- Wu, M.; Chen, F.; Wu, P.; Yang, Z.; Zhang, S.; Xiao, L.; Deng, Z.; Zhang, C.; Chen, Y.; Cai, L. Nanoclay mineral-reinforced macroporous nanocomposite scaffolds for in situ bone regeneration: In vitro and in vivo studies. Mater. Des. 2021, 205, 109734. [Google Scholar] [CrossRef]
- Zhang, X.; Fan, J.; Lee, C.-S.; Kim, S.; Chen, C.; Lee, M. Supramolecular Hydrogels Based on Nanoclay and Guanidine-Rich Chitosan: Injectable and Moldable Osteoinductive Carriers. ACS Appl. Mater. Interfaces 2020, 12, 16088–16096. [Google Scholar] [CrossRef]
- Liao, J.; Wang, H.; Liu, N.; Yang, H. Functionally modified halloysite nanotubes for personalized bioapplications. Adv. Colloid Interface Sci. 2023, 311, 102812. [Google Scholar] [CrossRef]
- Erezuma, I.; Eufrasio-da-Silva, T.; Golafshan, N.; Deo, K.; Mishra, Y.K.; Castilho, M.; Gaharwar, A.K.; Leeuwenburgh, S.; Dolatshahi-Pirouz, A.; Orive, G. Nanoclay Reinforced Biomaterials for Mending Musculoskeletal Tissue Disorders. Adv. Healthc. Mater. 2021, 10, 2100217. [Google Scholar] [CrossRef]
- Hu, J.; Miszuk, J.M.; Stein, K.M.; Sun, H. Nanoclay promotes mouse cranial bone regeneration mainly through modulating drug binding and sustained release. Appl. Mater. Today 2020, 21, 100860. [Google Scholar] [CrossRef]
- Ji, J.; Wang, C.; Xiong, Z.; Pang, Y.; Sun, W. 3D-printed scaffold with halloysite nanotubes laden as a sequential drug delivery system regulates vascularized bone tissue healing. Mater. Today Adv. 2022, 15, 100259. [Google Scholar] [CrossRef]
- Kazemi-Aghdam, F.; Jahed, V.; Dehghan-Niri, M.; Ganji, F.; Vasheghani-Farahani, E. Injectable chitosan hydrogel embedding modified halloysite nanotubes for bone tissue engineering. Carbohydr. Polym. 2021, 269, 118311. [Google Scholar] [CrossRef] [PubMed]
- Meyer, R.A.; Green, J.J. Shaping the future of nanomedicine: Anisotropy in polymeric nanoparticle design. WIREs Nanomed. Nanobiotechnol. 2016, 8, 191–207. [Google Scholar] [CrossRef]
- Sun, M.; Lee, J.; Chen, Y.; Hoshino, K. Studies of nanoparticle delivery with in vitro bio-engineered microtissues. Bioact. Mater. 2020, 5, 924–937. [Google Scholar] [CrossRef] [PubMed]
- Washington, M.A.; Balmert, S.C.; Fedorchak, M.V.; Little, S.R.; Watkins, S.C.; Meyer, T.Y. Monomer sequence in PLGA microparticles: Effects on acidic microclimates and in vivo inflammatory response. Acta Biomater. 2018, 65, 259–271. [Google Scholar] [CrossRef]
- del Castillo-Santaella, T.; Ortega-Oller, I.; Padial-Molina, M.; O’Valle, F.; Galindo-Moreno, P.; Jódar-Reyes, A.B.; Peula-García, J.M. Formulation, Colloidal Characterization, and In Vitro Biological Effect of BMP-2 Loaded PLGA Nanoparticles for Bone Regeneration. Pharmaceutics 2019, 11, 388. [Google Scholar] [CrossRef]
- Swy, E.R.; Schwartz-Duval, A.S.; Shuboni, D.D.; Latourette, M.T.; Mallet, C.L.; Parys, M.; Cormode, D.P.; Shapiro, E.M. Dual-modality, fluorescent, PLGA encapsulated bismuth nanoparticles for molecular and cellular fluorescence imaging and computed tomography. Nanoscale 2014, 6, 13104–13112. [Google Scholar] [CrossRef] [PubMed]
- Chen, D.; Liu, Y.; Zhang, Z.; Liu, Z.; Fang, X.; He, S.; Wu, C. NIR-II Fluorescence Imaging Reveals Bone Marrow Retention of Small Polymer Nanoparticles. Nano Lett. 2021, 21, 798–805. [Google Scholar] [CrossRef] [PubMed]
- Fu, L.; Feng, Q.; Chen, Y.; Fu, J.; Zhou, X.; He, C. Nanofibers for the Immunoregulation in Biomedical Applications. Adv. Fiber Mater. 2022, 4, 1334–1356. [Google Scholar] [CrossRef]
- Wu, T.; Ding, M.; Shi, C.; Qiao, Y.; Wang, P.; Qiao, R.; Wang, X.; Zhong, J. Resorbable polymer electrospun nanofibers: History, shapes and application for tissue engineering. Chin. Chem. Lett. 2020, 31, 617–625. [Google Scholar] [CrossRef]
- Lian, M.; Sun, B.; Qiao, Z.; Zhao, K.; Zhou, X.; Zhang, Q.; Zou, D.; He, C.; Zhang, X. Bi-layered electrospun nanofibrous membrane with osteogenic and antibacterial properties for guided bone regeneration. Colloids Surf. B Biointerfaces 2019, 176, 219–229. [Google Scholar] [CrossRef]
- Dhand, C.; Ong, S.T.; Dwivedi, N.; Diaz, S.M.; Venugopal, J.R.; Navaneethan, B.; Fazil, M.H.U.T.; Liu, S.P.; Seitz, V.; Wintermantel, E.; et al. Bio-inspired in situ crosslinking and mineralization of electrospun collagen scaffolds for bone tissue engineering. Biomaterials 2016, 104, 323–338. [Google Scholar] [CrossRef]
- Gu, J.-T.; Jiao, K.; Li, J.; Yan, J.-F.; Wang, K.-Y.; Wang, F.; Liu, Y.; Tay, F.R.; Chen, J.-H.; Niu, L.-N. Polyphosphate-crosslinked collagen scaffolds for hemostasis and alveolar bone regeneration after tooth extraction. Bioact. Mater. 2022, 15, 68–81. [Google Scholar] [CrossRef]
- Pinho, E.D.; Martins, A.; Araujo, J.V.; Reis, R.L.; Neves, N.M. Degradable particulate composite reinforced with nanofibres for biomedical applications. Acta Biomater. 2009, 5, 1104–1114. [Google Scholar] [CrossRef] [PubMed]
- Shaikh, S.; Younis, M.; Yuan, L. Functionalized DNA nanostructures for bioimaging. Coord. Chem. Rev. 2022, 469, 214648. [Google Scholar] [CrossRef]
- Guo, Y.; Tang, J.; Yao, C.; Yang, D. Multimodules integrated functional DNA nanomaterials for intelligent drug delivery. WIREs Nanomed. Nanobiotechnol. 2022, 14, e1753. [Google Scholar] [CrossRef]
- Huang, M.; Zhang, X.; Li, J.; Li, Y.; Wang, Q.; Teng, W. Comparison of osteogenic differentiation induced by siNoggin and pBMP-2 delivered by lipopolysaccharide-amine nanopolymersomes and underlying molecular mechanisms. Int. J. Nanomed. 2019, 14, 4229–4245. [Google Scholar] [CrossRef]
- Kim, T.-H.; Singh, R.K.; Kang, M.S.; Kim, J.-H.; Kim, H.-W. Gene delivery nanocarriers of bioactive glass with unique potential to load BMP2 plasmid DNA and to internalize into mesenchymal stem cells for osteogenesis and bone regeneration. Nanoscale 2016, 8, 8300–8311. [Google Scholar] [CrossRef]
- Lei, Y.; Rahim, M.; Ng, Q.; Segura, T. Hyaluronic acid and fibrin hydrogels with concentrated DNA/PEI polyplexes for local gene delivery. J. Control. Release 2011, 153, 255–261. [Google Scholar] [CrossRef]
- Shafiei, M.; Ansari, M.N.M.; Razak, S.I.A.; Khan, M.U.A. A Comprehensive Review on the Applications of Exosomes and Liposomes in Regenerative Medicine and Tissue Engineering. Polymers 2021, 13, 2529. [Google Scholar] [CrossRef]
- Yu, J.R.; Janssen, M.; Liang, B.J.; Huang, H.-C.; Fisher, J.P. A liposome/gelatin methacrylate nanocomposite hydrogel system for delivery of stromal cell-derived factor-1α and stimulation of cell migration. Acta Biomater. 2020, 108, 67–76. [Google Scholar] [CrossRef]
- Mohammadi, M.; Alibolandi, M.; Abnous, K.; Salmasi, Z.; Jaafari, M.R.; Ramezani, M. Fabrication of hybrid scaffold based on hydroxyapatite-biodegradable nanofibers incorporated with liposomal formulation of BMP-2 peptide for bone tissue engineering. Nanomed. Nanotechnol. Biol. Med. 2018, 14, 1987–1997. [Google Scholar] [CrossRef] [PubMed]
- Yao, Y.; Jiang, Y.; Song, J.; Wang, R.; Li, Z.; Yang, L.; Wu, W.; Zhang, L.; Peng, Q. Exosomes as Potential Functional Nanomaterials for Tissue Engineering. Adv. Healthc. Mater. 2022, 2201989. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.; Wu, J.; Hu, H.; Mu, Y.; Zhang, L.; Zhao, Y.; Bian, X.; Jing, W.; Wei, P.; Zhao, B.; et al. Novel fusion peptides deliver exosomes to modify injectable thermo-sensitive hydrogels for bone regeneration. Mater. Today Bio 2022, 13, 100195. [Google Scholar] [CrossRef] [PubMed]

| Structure | Nanoclay Types | |
|---|---|---|
| Layered | T:O | Kaolinite, Halloysite, rectorite |
| T:O:T | Pyrophyillite, Illite, Vermiculite, Chlorite, Smectite, Montmorillonite | |
| Fibrous | Attapulgite |
| Nanomaterials | |||
|---|---|---|---|
| Inorganic | Unique Characteristics | Typical Application | |
| Metallic NPs (Au, Ag) | 1. Biocompatibility 2. Antimicrobial 3. Controllable shape and size 4. Conductivity 5. Easy to functionalise | 1. Metallic NP-based composite 2. Biological imaging 3. Diagnostic nanoprobes 4. Treating infections 5. Drug delivery | |
| Carbon-based Nanomaterials (Graphene, CNTs) | 1. Excellent conductivity 2. Reinforce mechanical performance 3. Hydrophilia 4. Large specific surface area 5. Chemical stability 6. Thermal and wear resistance | 1. Conductive composite 2. Imaging 3. Drug delivery 4. High mechanical properties implant | |
| Silica NPs | 1. Controlled mesoporous structure 2. Conjugate with wide variety of compounds 3. Large specific surface area 4. Promotes osteogenic differentiation | 1. Drug delivery systems 2. Biological imaging 3. Composite scaffold | |
| Nano-HAp | 1. Natural bone tissue components 2. Outstanding osteogenic features 3. Easy chemical grafting 4. Protein adsorption 5. Improve the mechanical properties | 1. Bone biomimetic scaffold 2. Surface modification of the bone implant 3. Loaded with biological factors 4. Artificial bone materials | |
| Black Phosphorus (BP) | 1. Conductivity and piezoelectricity 2. Degraded into nontoxic phosphates 3. Be composed of phosphorus, an inorganic component of bone 4. Near-infrared optical properties 5. Reinforce mechanical performance | 1. Conductivity scaffolds 2. NIR light-triggered drug release system 3. Photothermal therapy | |
| Magnetic NPs (Fe2O3, Fe3O4) | 1. Superparamagnetic property 2. Magnetothermal 3. Magnetic imaging 4. Regulating osteogenic activity by the inherent magnetic field | 1. Magnetic bone-repair scaffold 2. Magnetic nanoimaging technology 3. Magnetothermal therapy | |
| Nanoclays (MMT, HNTs) | 1. Enforce mechanical performance 2. Charge heterogeneity 3. Promote osteogenesis releasing Mg2+ and Ca2+ 4. Easy chemical grafting 5. Protein adsorption | 1. Drug delivery 2. As Hard polymeric scaffold reinforcers 3. As hydrogel reinforcers | |
| Organic | |||
| Polymeric NPs | 1. Nontoxic degradation products 2. Functional modification 3. Biocompatible | 1. Drug delivery 2. Fluorescence imaging | |
| Nanofibres | 1. Biomimetic structure of the ECM 2. Good tensile mechanical properties 3. Pore interconnectivity 4. High physical adsorption capacity | 1. Be applied as bone-repair scaffolds 2. Drug delivery 3. Core-shell structure endow with specific biofunction 4. Nanofibre-reinforced bone composite scaffold | |
| DNA Nanomaterials | 1. Be accurately designed, modified, and endowed with unique functions 2. Be composed of nucleobases | 1. Drug delivery 2. Targeted therapy 3. Biofunctional modification of bone-repair scaffold | |
| Liposomes, Exosomes | 1. Lipid bilayer structure 2. Easy to functionalise 3. Exosomes are extracellular vesicles that are secreted by cells and carry biomolecules | 1. Drug delivery 2. Targeted therapy 3. Biofunctional modification of bone-repair scaffold | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wan, T.; Zhang, M.; Jiang, H.-R.; Zhang, Y.-C.; Zhang, X.-M.; Wang, Y.-L.; Zhang, P.-X. Tissue-Engineered Nanomaterials Play Diverse Roles in Bone Injury Repair. Nanomaterials 2023, 13, 1449. https://doi.org/10.3390/nano13091449
Wan T, Zhang M, Jiang H-R, Zhang Y-C, Zhang X-M, Wang Y-L, Zhang P-X. Tissue-Engineered Nanomaterials Play Diverse Roles in Bone Injury Repair. Nanomaterials. 2023; 13(9):1449. https://doi.org/10.3390/nano13091449
Chicago/Turabian StyleWan, Teng, Meng Zhang, Hao-Ran Jiang, Yi-Chong Zhang, Xiao-Meng Zhang, Yi-Lin Wang, and Pei-Xun Zhang. 2023. "Tissue-Engineered Nanomaterials Play Diverse Roles in Bone Injury Repair" Nanomaterials 13, no. 9: 1449. https://doi.org/10.3390/nano13091449






