Saliva Exhibits High Sensitivity and Specificity for the Detection of SARS-COV-2
Abstract
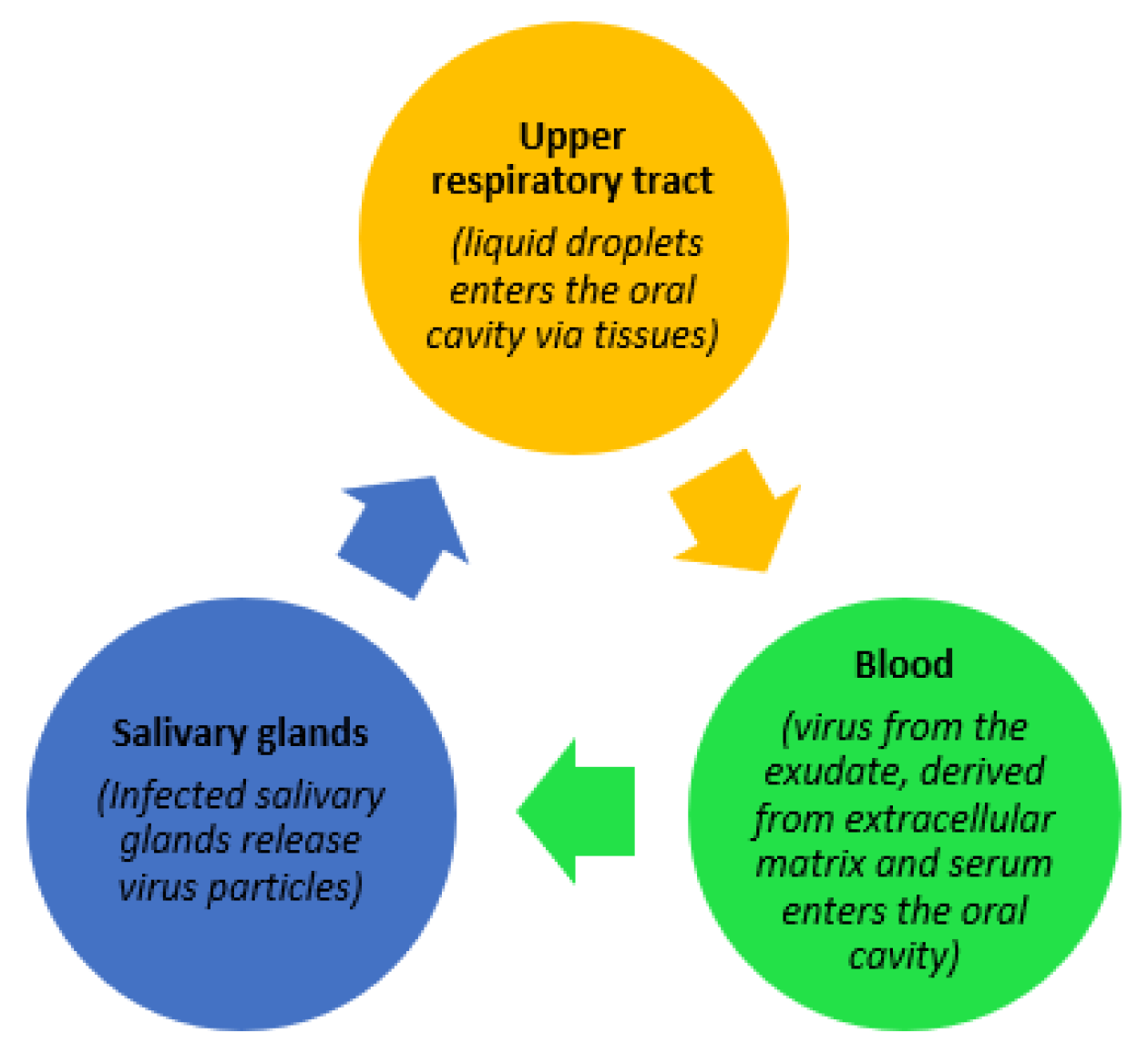
1. Introduction
2. Regulatory Framework and Introduction of Salivary Diagnostics for COVID-19
3. Review of Studies on Salivary Diagnostics
4. Sensitivity and Specificity of Salivary Diagnostics for SARS-CoV-2 Testing
4.1. Strengths and Limitations of Salivary Diagnostics
4.2. Emerging Technologies in Salivary Diagnostics for COVID-19
4.3. Direction for Future Studies
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Chen, Y.; Liu, Q.; Guo, D. Emerging coronaviruses: Genome structure, replication, and pathogenesis. J. Med. Virol. 2020, 92, 418–423. [Google Scholar] [CrossRef]
- Han, P.; Ivanovski, S. Saliva—Friend and Foe in the COVID-19 Outbreak. Diagnostics 2020, 10, 290. [Google Scholar] [CrossRef]
- Sabino-Silva, R.; Jardim, A.C.G.; Siqueira, W.L. Coronavirus COVID-19 impacts to dentistry and potential salivary diagnosis. Clin. Oral Investig. 2020, 24, 1–3. [Google Scholar] [CrossRef] [PubMed]
- Shang, J.; Wan, Y.; Luo, C.; Ye, G.; Geng, Q.; Auerbach, A.; Li, F. Cell entry mechanisms of SARS-CoV-2. Proc. Natl. Acad. Sci. USA 2020, 117, 11727–11734. [Google Scholar] [CrossRef] [PubMed]
- Zupin, L.; Pascolo, L.; Crovella, S. Is FURIN gene expression in salivary glands related to SARS-CoV-2 infectivity through saliva? J. Clin. Pathol. 2020, 74, 209–211. [Google Scholar] [CrossRef]
- Johns Hopkins Coronavirus Resource Center. COVID-19 Map. Available online: https://coronavirus.jhu.edu/map.html (accessed on 26 March 2021).
- Hamid, H.; Khurshid, Z.; Adanir, N.; Zafar, M.S.; Zohaib, S. Covid-19 pandemic and role of human saliva as a testing biofluid in point-of-care technology. Eur. J. Dent. 2020, 14, S123–S129. [Google Scholar] [CrossRef]
- Khurshid, Z.; Zohaib, S.; Najeeb, S.; Zafar, M.; Slowey, P.; Almas, K. Human Saliva Collection Devices for Proteomics: An Update. Int. J. Mol. Sci. 2016, 17, 846. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC) Updated Information about the Emergency Use Authorization for the CDC 2019-nCoV RT-PCR Diagnostic Panel. Available online: https://www.cdc.gov/csels/dls/locs/2020/updated_information_about_the_emergency_use_authorization_for_the_cdc_2019-ncov_rt-pcr_diagnostic_panel.html (accessed on 29 April 2021).
- FDA. U.S. Food and Drug Administration Emergency Use Authorizations; FDA: Muntinlupa, PH, USA, 2021. Available online: https://www.fda.gov/emergency-preparedness-and-response/mcm-legal-regulatory-and-policy-framework/emergency-use-authorization (accessed on 26 March 2021).
- Rutgers Clinical Genomics Laboratory. TaqPath SARS-CoV-2 Assay EUA Summary Accelerated Emergency Use Authorization (EUA) Summary Sars-CoV-2 Assay. 13 April 2020. Available online: https://www.rutgers.edu/news/new-rutgers-saliva-test-coronavirus-gets-fda-approval (accessed on 26 March 2021).
- Azzi, L.; Carcano, G.; Gianfagna, F.; Grossi, P.; Gasperina, D.D.; Genoni, A.; Fasano, M.; Sessa, F.; Tettamanti, L.; Carinci, F.; et al. Saliva is a reliable tool to detect Sars-CoV-2. J. Infect. 2020, 81, e45–e50. [Google Scholar] [CrossRef] [PubMed]
- Azzi, L.; Carcano, G.; Dalla Gasperina, D.; Sessa, F.; Maurino, V.; Baj, A. Two cases of COVID-19 with positive salivary and negative pharyngeal or respiratory swabs at hospital discharge: A rising concern. Oral Dis. 2020, 27, 707–709. [Google Scholar] [CrossRef]
- Chen, L.; Zhao, J.; Peng, J.; Li, X.; Deng, X.; Geng, Z.; Shen, Z.; Guo, F.; Zhang, Q.; Jin, Y.; et al. Detection of 2019-nCoV in Saliva and Characterization of Oral Symptoms in COVID-19 Patients. SSRN Electron. J. 2020, 53, e12923. [Google Scholar] [CrossRef]
- Mi Seon, H.; Moon-Woo, S.; Eun Young, H.; Ji Hong, P.; Namhee, K.; Sue, S.; Sung Im, C.; Sung Sup, P.; Eun Hwa, C. Sequential Analysis of Viral Load in a Neonate and Her Mother Infected With Severe Acute Respiratory Syndrome Coronavirus 2|Clinical Infectious Diseases|Oxford Academic. Clin. Infect. Dis. 2020, 71, 2236–2239. [Google Scholar]
- To, K.K.W.; Tsang, O.T.Y.; Yip, C.C.Y.; Chan, K.H.; Wu, T.C.; Chan, J.M.C.; Leung, W.S.; Chik, T.S.H.; Choi, C.Y.C.; Kandamby, D.H.; et al. Consistent Detection of 2019 Novel Coronavirus in Saliva | Clinical Infectious Diseases|Oxford Academic. Clin. Infect. Dis. 2020, 71, 841–843. [Google Scholar] [CrossRef] [PubMed]
- To, K.K.W.; Tsang, O.T.Y.; Leung, W.S.; Tam, A.R.; Wu, T.C.; Lung, D.C.; Yip, C.C.Y.; Cai, J.P.; Chan, J.M.C.; Chik, T.S.H.; et al. Temporal profiles of viral load in posterior oropharyngeal saliva samples and serum antibody responses during infection by SARS-CoV-2: An observational cohort study. Lancet Infect. Dis. 2020, 20, 565–574. [Google Scholar] [CrossRef]
- Wyllie, A.L.; Fournier, J.; Casanovas-Massana, A.; Campbell, M.; Tokuyama, M.; Vijayakumar, P.; Geng, B.; Muenker, M.C.; Moore, A.J.; Vogels, C.B.F.; et al. Saliva is more sensitive for SARS-CoV-2 detection in COVID-19 patients than nasopharyngeal swabs. medRxiv 2020, 383, 1283–1286. [Google Scholar] [CrossRef]
- Zheng, S.; Fan, J.; Yu, F.; Feng, B.; Lou, B.; Zou, Q.; Xie, G.; Lin, S.; Wang, R.; Yang, X.; et al. Viral load dynamics and disease severity in patients infected with SARS-CoV-2 in Zhejiang province, China, January-March 2020: Retrospective cohort study. BMJ 2020, 369. [Google Scholar] [CrossRef]
- Zhang, W.; Du, R.H.; Li, B.; Zheng, X.S.; Yang, X.L.; Hu, B.; Wang, Y.Y.; Xiao, G.F.; Yan, B.; Shi, Z.L.; et al. Molecular and serological investigation of 2019-nCoV infected patients: Implication of multiple shedding routes. Emerg. Microbes Infect. 2020, 9, 386–389. [Google Scholar] [CrossRef] [PubMed]
- Pasomsub, E.; Watcharananan, S.P.; Boonyawat, K.; Janchompoo, P.; Wongtabtim, G.; Suksuwan, W.; Sungkanuparph, S.; Phuphuakrat, A. Saliva sample as a non-invasive specimen for the diagnosis of coronavirus disease-2019 (COVID-19): A cross-sectional study. Clin. Microbiol. Infect. 2020, 27, 285.e1–285.e4. [Google Scholar] [CrossRef]
- Sirikhetkon, S.; Shrestha, M.; Okada, P.A.; Prasert, K. Diagnostic Accuracy of Saliva for SARS-CoV-2 Detection in State-sponsored Quarantine in Thailand. Outbreak Surveill. Investig. Response J. 2021, 14, 12–19. [Google Scholar]
- Basso, D.; Aita, A.; Padoan, A.; Cosma, C.; Navaglia, F.; Moz, S.; Contran, N.; Zambon, C.F.; Maria Cattelan, A.; Plebani, M. Salivary SARS-CoV-2 antigen rapid detection: A prospective cohort study. Clin. Chim. Acta 2021, 517, 54–59. [Google Scholar] [CrossRef]
- To, K.K.; Tsang, O.T.Y.; Chik-Yan Yip, C. Consistent detection of novel coronavirus in saliva. Clin. Infect. Dis 2019, 71, 841–843. [Google Scholar] [CrossRef] [PubMed]
- Azzi, L.; Baj, A.; Alberio, T.; Lualdi, M.; Veronesi, G.; Carcano, G.; Ageno, W.; Gambarini, C.; Maffioli, L.; Di Saverio, S. Rapid Salivary Test suitable for a mass screening program to detect SARS-CoV-2: A diagnostic accuracy study. J. Infect. 2020, 81, e75–e78. [Google Scholar] [CrossRef] [PubMed]
- Cheng, V.C.C.; Wong, S.-C.; Chen, J.H.K.; Yip, C.C.Y.; Chuang, V.W.M.; Tsang, O.T.Y.; Sridhar, S.; Chan, J.F.W.; Ho, P.-L.; Yuen, K.-Y. Escalating infection control response to the rapidly evolving epidemiology of the Coronavirus disease 2019 (COVID-19) due to SARS-CoV-2 in Hong Kong. Infect. Control Hosp. Epidemiol. 2020, 41, 493–498. [Google Scholar] [CrossRef] [PubMed]
- Han, M.S.; Seong, M.-W.; Kim, N.; Shin, S.; Cho, S.I.; Park, H.; Kim, T.S.; Park, S.S.; Choi, E.H. Viral RNA load in mildly symptomatic and asymptomatic children with COVID-19, Seoul, South Korea. Emerg. Infect. Dis. 2020, 26, 2497–2499. [Google Scholar] [CrossRef]
- Han, M.S.; Seong, M.-W.; Heo, E.Y.; Park, J.H.; Kim, N.; Shin, S.; Cho, S.I.; Park, S.S.; Choi, E.H. Sequential analysis of viral load in a neonate and her mother infected with SARS-CoV-2. Clin. Infect. Dis. 2020, 71, 2236–2239. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, S.; Fujisawa, S.; Nakakubo, S.; Kamada, K.; Yamashita, Y.; Fukumoto, T.; Sato, K.; Oguri, S.; Taki, K.; Senjo, H. Comparison of SARS-CoV-2 detection in nasopharyngeal swab and saliva. J. Infect. 2020, 81, e145–e147. [Google Scholar] [CrossRef]
- To, K.K.-W.; Tsang, O.T.-Y.; Yip, C.C.-Y.; Chan, K.-H.; Wu, T.-C.; Chan, J.M.-C.; Leung, W.-S.; Chik, T.S.-H.; Choi, C.Y.-C.; Kandamby, D.H. Consistent detection of 2019 novel coronavirus in saliva. Clin. Infect. Dis. 2020, 71, 841–843. [Google Scholar] [CrossRef] [PubMed]
- Yoon, J.G.; Yoon, J.; Song, J.Y.; Yoon, S.-Y.; Lim, C.S.; Seong, H.; Noh, J.Y.; Cheong, H.J.; Kim, W.J. Clinical Significance of a High SARS-CoV-2 Viral Load in the Saliva. J. Korean Med. Sci. 2020, 35, e195. [Google Scholar] [CrossRef]
- Zhu, J.; Guo, J.; Xu, Y.; Chen, X. Viral dynamics of SARS-CoV-2 in saliva from infected patients. J. Infect. 2020, 81, e48–e50. [Google Scholar] [CrossRef] [PubMed]
- Jamal, A.J.; Mohammad, M.; Coomes, E.; Powis, J.; Li, A.; Paterson, A.; Anceva-Sami, S.; Barati, S.; Crowl, G.; Faheem, A. Sensitivity of nasopharyngeal swabs and saliva for the detection of severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). medRxiv 2020, 72, 1064–1066. [Google Scholar]
- Leung, E.C.; Chow, V.C.; Lee, M.K.; Lai, R.W. Deep throat saliva as an alternative diagnostic specimen type for the detection of SARS-CoV-2. J. Med. Virol. 2020, 93, 533–536. [Google Scholar] [CrossRef]
- Nagura-Ikeda, M.; Imai, K.; Tabata, S.; Miyoshi, K.; Murahara, N.; Mizuno, T.; Horiuchi, M.; Kato, K.; Imoto, Y.; Iwata, M. Clinical evaluation of self-collected saliva by RT-qPCR, direct RT-qPCR, RT-LAMP, and a rapid antigen test to diagnose COVID-19. J. Clin. Microbiol. 2020, 58, e01438-20. [Google Scholar] [CrossRef] [PubMed]
- Tajima, Y.; Suda, Y.; Yano, K. A case report of SARS-CoV-2 confirmed in saliva specimens up to 37 days after onset: Proposal of saliva specimens for COVID-19 diagnosis and virus monitoring. J. Infect. Chemother. 2020, 26, 1086–1089. [Google Scholar] [CrossRef] [PubMed]
- Williams, E.; Bond, K.; Zhang, B.; Putland, M.; Williamson, D.A. Saliva as a non-invasive specimen for detection of SARS-CoV-2. J. Clin. Microbiol. 2020, 58, e00776-20. [Google Scholar] [CrossRef] [PubMed]
- Otto, M.P.; Darles, C.; Valero, E.; Benner, P.; Dutasta, F.; Janvier, F. Posterior oropharyngeal salivafor the detection of SARS-CoV-2. Clin. Infect. Dis. 2020, 71, 2939–2946. [Google Scholar] [CrossRef]
- McCormick-Baw, C.; Morgan, K.; Gaffney, D.; Cazares, Y.; Jaworski, K.; Byrd, A.; Molberg, K.; Cavuoti, D. Saliva as an alternate specimen source for detection of SARS-CoV-2 in symptomatic patients using Cepheid Xpert Xpress SARS-CoV-2. J. Clin. Microbiol. 2020, 58. [Google Scholar] [CrossRef]
- Chen, J.H.-K.; Yip, C.C.-Y.; Poon, R.W.-S.; Chan, K.-H.; Cheng, V.C.-C.; Hung, I.F.-N.; Chan, J.F.-W.; Yuen, K.-Y.; To, K.K.-W. Evaluating the use of posterior oropharyngeal saliva in a point-of-care assay for the detection of SARS-CoV-2. Emerg. Microbes Infect. 2020, 9, 1–14. [Google Scholar] [CrossRef]
- Mak, G.C.K.; Cheng, P.K.C.; Lau, S.S.Y.; Wong, K.K.Y.; Lau, C.S.; Lam, E.T.K.; Chan, R.C.W.; Tsang, D.N.C. Evaluation of rapid antigen test for detection of SARS-CoV-2 virus. J. Clin. Virol. 2020, 129, 104500. [Google Scholar] [CrossRef]
- Bosworth, A.; Whalley, C.; Poxon, C.; Wanigasooriya, K.; Pickles, O.; Aldera, E.L.; Papakonstantinou, D.; Morley, G.L.; Walker, E.M.; Zielinska, A.E. Rapid implementation and validation of a cold-chain free SARS-CoV-2 diagnostic testing workflow to support surge capacity. J. Clin. Virol. 2020, 128, 104469. [Google Scholar] [CrossRef]
- Hung, D.L.-L.; Li, X.; Chiu, K.H.-Y.; Yip, C.C.-Y.; To, K.K.-W.; Chan, J.F.-W.; Sridhar, S.; Chung, T.W.-H.; Lung, K.-C.; Liu, R.W.-T. Early Morning Versus Spot Posterior Oropharyngeal Saliva for Diagnosis of SARS-CoV-2 Infection: Implication of Timing of Specimen Collection for Community-wide Screening. In Open Forum Infectious Diseases; Oxford University Press: Oxford, UK, June 2020. [Google Scholar]
- Khurshid, Z.; Zohaib, S.; Joshi, C.; Moin, S.F.; Zafar, M.S.; Speicher, D.J. Saliva as a non-invasive sample for the detection of SARS-CoV-2: A systematic review. medRxiv 2020. [Google Scholar] [CrossRef]
- Khurshid, Z.; Asiri, F.Y.I.; Al Wadaani, H. Human Saliva: Non-Invasive Fluid for Detecting Novel Coronavirus (2019-nCoV). Int. J. Environ. Res. Public Health 2020, 17, 2225. [Google Scholar] [CrossRef]
- World Health Organization Laboratory testing for 2019 novel coronavirus (2019-nCoV) in suspected human cases. WHO-Interim Guid. 2020, 2019, 1–7.
- Santosh, T.S.; Parmar, R.; Anand, H.; Srikanth, K.; Saritha, M. A review of salivary diagnostics and its potential implication in detection of Covid-19. Cureus 2020, 12, e7708. [Google Scholar] [CrossRef] [PubMed]
- Kojima, N.; Turner, F.; Slepnev, V.; Bacelar, A.; Deming, L.; Kodeboyina, S.; Klausner, J.D. Self-Collected Oral Fluid and Nasal Swabs Demonstrate Comparable Sensitivity to Clinician Collected Nasopharyngeal Swabs for Covid-19 Detection. medRxiv 2020. [Google Scholar] [CrossRef]
- Khurshid, Z.; Warsi, I.; Moin, S.F.; Slowey, P.D.; Latif, M.; Zohaib, S.; Zafar, M.S. Biochemical analysis of oral fluids for disease detection. In Advances in Clinical Chemistry; Academic Press Inc.: Cambridge, MA, USA, 2021; Volume 100, pp. 205–253. ISBN 9780128239223. [Google Scholar]
- Khurshid, Z.; Zafar, M.S.; Khan, R.S.; Najeeb, S.; Slowey, P.D.; Rehman, I.U. Role of Salivary Biomarkers in Oral Cancer Detection. Adv. Clin. Chem. 2018, 86, 23–70. [Google Scholar] [CrossRef]
- Saher, F.; Khurshid, Z.; Zafar, M.S.; Mohammed, F.; Khurram, S.A. Salivary Glands. In An Illustrated Guide to Oral Histology; Wiley: Hoboken, NJ, USA, 2021; pp. 147–166. [Google Scholar]
- Khurshid, Z.; Zafar, M.; Khan, E.; Mali, M.; Latif, M. Human saliva can be a diagnostic tool for Zika virus detection. J. Infect. Public Health 2019, 12, 601–604. [Google Scholar] [CrossRef] [PubMed]
- To, K.K.W.; Yip, C.C.Y.; Lai, C.Y.W.; Wong, C.K.H.; Ho, D.T.Y.; Pang, P.K.P.; Ng, A.C.K.; Leung, K.H.; Poon, R.W.S.; Chan, K.H.; et al. Saliva as a diagnostic specimen for testing respiratory virus by a point-of-care molecular assay: A diagnostic validity study. Clin. Microbiol. Infect. 2019, 25, 372–378. [Google Scholar] [CrossRef]
- Khurshid, Z. Salivary point-of-care technology. Eur. J. Dent. 2018, 12, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Sullivan, P.S.; Sailey, C.; Guest, J.L.; Guarner, J.; Siegler, A.J.; Valentine-Graves, M.; Gravens, L.; del Rio, C.; Sanchez, T.H. Detection of SARS-CoV-2 RNA and antibodies in diverse samples: Protocol to validate the sufficiency of provider-observed home-collected blood, saliva and oropharyngeal samples (Preprint). JMIR Public Health Surveill. 2020, 6, e19054. [Google Scholar] [CrossRef]
- Xu, H.; Zhong, L.; Deng, J.; Peng, J.; Dan, H.; Zeng, X.; Li, T.; Chen, Q. High expression of ACE2 receptor of 2019-nCoV on the epithelial cells of oral mucosa. Int. J. Oral Sci. 2020, 12, 1–5. [Google Scholar] [CrossRef]
- Fulgent Therapeutics, L. Fulgent COVID-19 by RT-PCR test EUA Summary 2 Device Description and Test Principle. Available online: https://www.fda.gov/media/138150/download (accessed on 23 July 2020).
| Sr. No. | Tests | Date of Approval |
|---|---|---|
| 1 | MicroGenDX Laboratories obtains FDA EUA approval for 24-h saliva test [RT-PCR] | 4 April 2020 |
| 2 | Rutgers University/Infinite Biologics gets first FDA EUA Approval for saliva high throughput method connected to Thermo Fisher RT-PCR | 13 April 2020 |
| 3 | Curative receives FDA EUA for oral fluid test | 19 April 2020 |
| 4 | FDA announces changes in registration requirements | 19 May 2020 |
| 5 | MLB adopts saliva COVID-19 Testing | 20 May 2020 |
| 6 | Chronomics [UK] Saliva COVID-19 Test Launched | 20 May 2020 |
| 7 | Phosphorus gets FDA EUA for home saliva test [collection] | 9 June 2020 |
| 8 | Sysmex Japan gets approval in Japan with BGI RT-PCR Kit | 10 June 2020 |
| 9 | Yale/Saliva Direct working with the NBA | 24 June 2020 |
| 10 | CRL/OraSure get EUA with RT-PCR | 31 July 2020 |
| 11 | Approval for Yale/Saliva Direct | 17 August 2020 |
| 12 | U of Illinois-Urbana-Champaign FDA EUA approval granted | 20 August 2020 |
| 13 | OraSure/MiraDx get EUA for RT-PCR Kit | 4 September 2020 |
| 14 | Spectrum DNA gets FDA EUA for saliva collection kit | 19 October 2020 |
| 15 | DNA Genotek’s OMNIgene·ORAL OM-505 and OME-505 saliva collection devices receive FDA EUA | 11 February 2020 |
| 16 | AZOA P23 At-Home COVID-19 Home Saliva Collection Kit available at Costco Retail outlets for $129.99–$139.99 | 11 March 2020 |
| 17 | PerkinElmer coronavirus RT-PCR assay receives CE Mark for saliva use, first for sample pooling | 17 December 2020 |
| 18 | Kleva Health’s at-home COVID-19 saliva test kit achieves EUA | 12 September 2020 |
| 19 | UAE: Scientists develop smartphone-read saliva testing method for Covid-19 | 12 October 2020 |
| 20 | KnowNow COVID-19 saliva lateral flow from Vatic [UK] launched | 19 October 2020 |
| Study | Ref | Saliva Collection Method | Swabs and Lavage for Comparison | Diagnostic Test | N | TP | FP | FN | TN | Sensitivity | Specificity | PPV | NPV |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Azzi, L et al., 2020 (Italy) | [12] | Drooling | NPS | RT-PCR | 25 | 25 | 0 | 0 | 0 | 1 | uc | 1 | uc |
| Azzi, L et al., 2020 (Italy) | [13] | Drooling | BAL | RT-PCR | 2 | 0 | 2 | 0 | 0 | uc | 0 | 0 | uc |
| Chen, Lili et al., 2020 (China) | [14] | Cotton Swabs—Saliva from orifices | OPS | RT-qPCR | 31 | 4 | 0 | 9 | 18 | 0.31 | 1 | 1 | 0.66 |
| Han, Mi Seon et al., 2020 (Korea) | [15] | Saliva | NPS, OPS | qPCR | 2 | 1 | 0 | 1 | 0 | 0.50 | uc | 1 | 0 |
| Wang, To et al., 2020 (Hong Kong, China) | [16] | Sputum/Coughed-out Saliva (self-collected) | NPS | RT-qPCR | 12 | 11 | 0 | 1 | 0 | 0.92 | uc | 1 | 0 |
| Wang, To et al., 2020 (Hong Kong, China) | [17] | Coughed-up Saliva—Posterior OroPharynx | NPS, Sputum | RT-qPCR | 23 | 20 | 0 | 3 | 0 | 0.87 | uc | 1 | 0 |
| Wyllie Anne et al., 2020 (USA) | [18] | Saliva (spitting) | NPS | rRT-PCR | 46 | 38 | 1 | 7 | 0 | 0.84 | 0 | 0.97 | 0 |
| Zheng Shufa et al., 2020 (China) | [19] | Sputum (hospitalized patients) | Stool, Serum, Urine | RT-qPCR | 96 | 96 | 0 | 0 | 0 | 1 | uc | 1 | uc |
| Zhang Wei et al., 2020 (China) | [20] | Oral Swabs (hospitalized patients—baseline) | Blood, Anal | RT-qPCR | 16 | 8 | 0 | 8 | 0 | 0.50 | uc | 1 | 0 |
| Pasomsub, E et al., 2020 (Thailand) | [21] | Saliva | NPS, TS | RT-PCR | 200 | 16 | 2 | 3 | 179 | 0.84 | 0.98 | 0.88 | 0.98 |
| Somrak et al., 2021 | [22] | Self-collected | NPS | RT-PCR | 32 | 12 | 0 | 20 | 0 | 0.37 | 1 | 1 | 0.91 |
| Basso et al., 2021 | [23] | Self-collected | NPS | RT-PCR | 84 | 67 | 0 | 17 | 0 | 0.78 | uc | 1 | 0 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Warsi, I.; Khurshid, Z.; Shazam, H.; Umer, M.F.; Imran, E.; Khan, M.O.; Slowey, P.D.; Goodson, J.M. Saliva Exhibits High Sensitivity and Specificity for the Detection of SARS-COV-2. Diseases 2021, 9, 38. https://doi.org/10.3390/diseases9020038
Warsi I, Khurshid Z, Shazam H, Umer MF, Imran E, Khan MO, Slowey PD, Goodson JM. Saliva Exhibits High Sensitivity and Specificity for the Detection of SARS-COV-2. Diseases. 2021; 9(2):38. https://doi.org/10.3390/diseases9020038
Chicago/Turabian StyleWarsi, Ibrahim, Zohaib Khurshid, Hamda Shazam, Muhammad Farooq Umer, Eisha Imran, Muhammad Owais Khan, Paul Desmond Slowey, and J. Max Goodson. 2021. "Saliva Exhibits High Sensitivity and Specificity for the Detection of SARS-COV-2" Diseases 9, no. 2: 38. https://doi.org/10.3390/diseases9020038
APA StyleWarsi, I., Khurshid, Z., Shazam, H., Umer, M. F., Imran, E., Khan, M. O., Slowey, P. D., & Goodson, J. M. (2021). Saliva Exhibits High Sensitivity and Specificity for the Detection of SARS-COV-2. Diseases, 9(2), 38. https://doi.org/10.3390/diseases9020038








