Recent Studies on Smart Textile-Based Wearable Sweat Sensors for Medical Monitoring: A Systematic Review
Abstract
1. Introduction
- Systematic Analysis: Provides a detailed and structured examination of textile-based sweat sensors, focusing on their types, sensing mechanisms, and application areas.
- Technical Comparison: Offers a comprehensive comparison of various sensor types, highlighting their strengths, weaknesses, and potential applications.
- Integration of Advancements: Synthesizes recent developments in materials science, sensor technologies, and data analytics to present an updated overview of the field.
- Categorization of Research: Organizes existing research based on specific sweat analytes and methodologies, offering a clear and structured presentation of current knowledge.
- Practical Applications: Discusses real-world applications of smart textile-based sweat sensors in medical monitoring and sports medicine, showcasing their transformative potential.
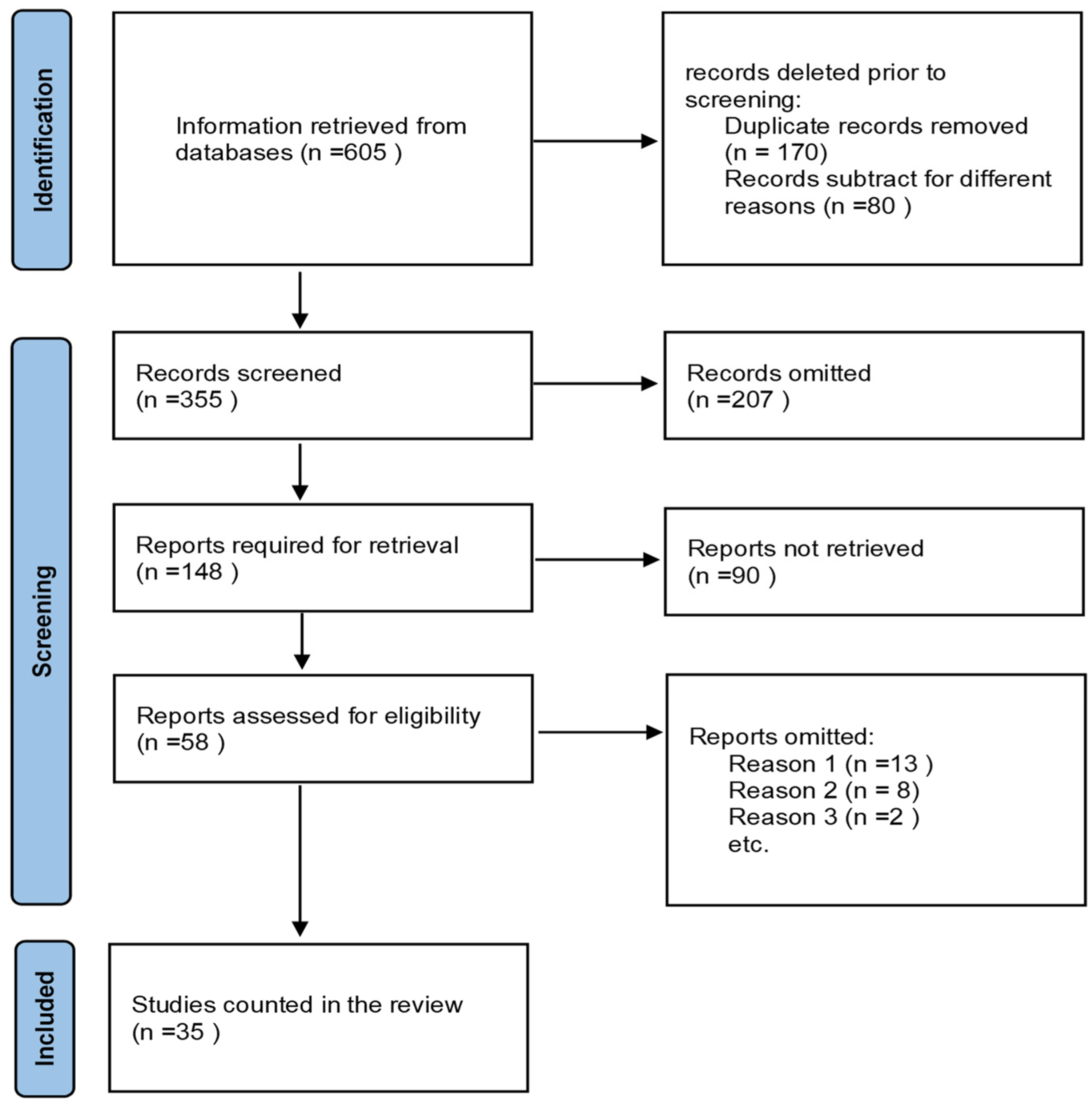
2. Materials and Methods
3. Results
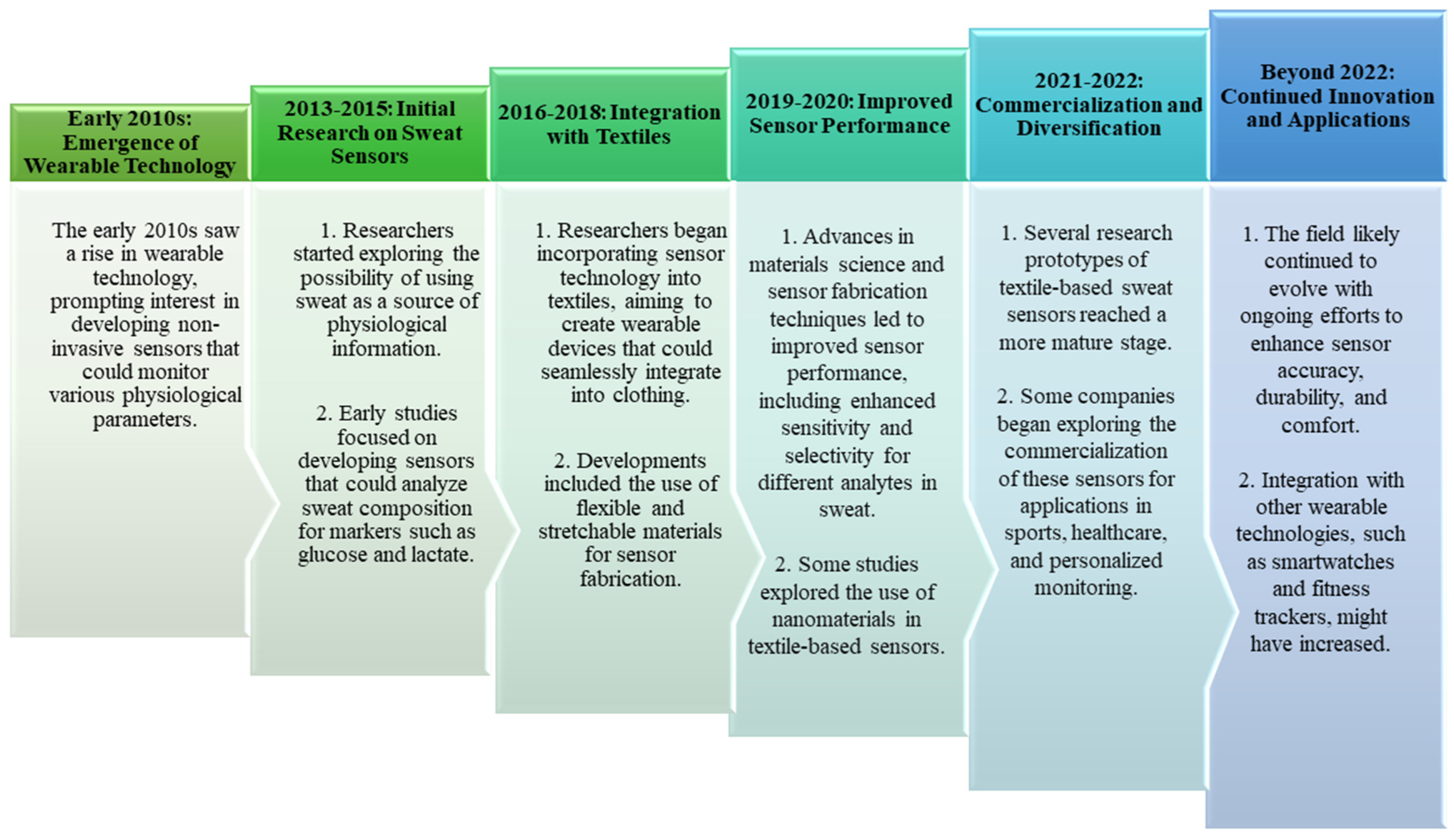
3.1. Smart Textile-Based Sweat Sensor Technology and Their Types
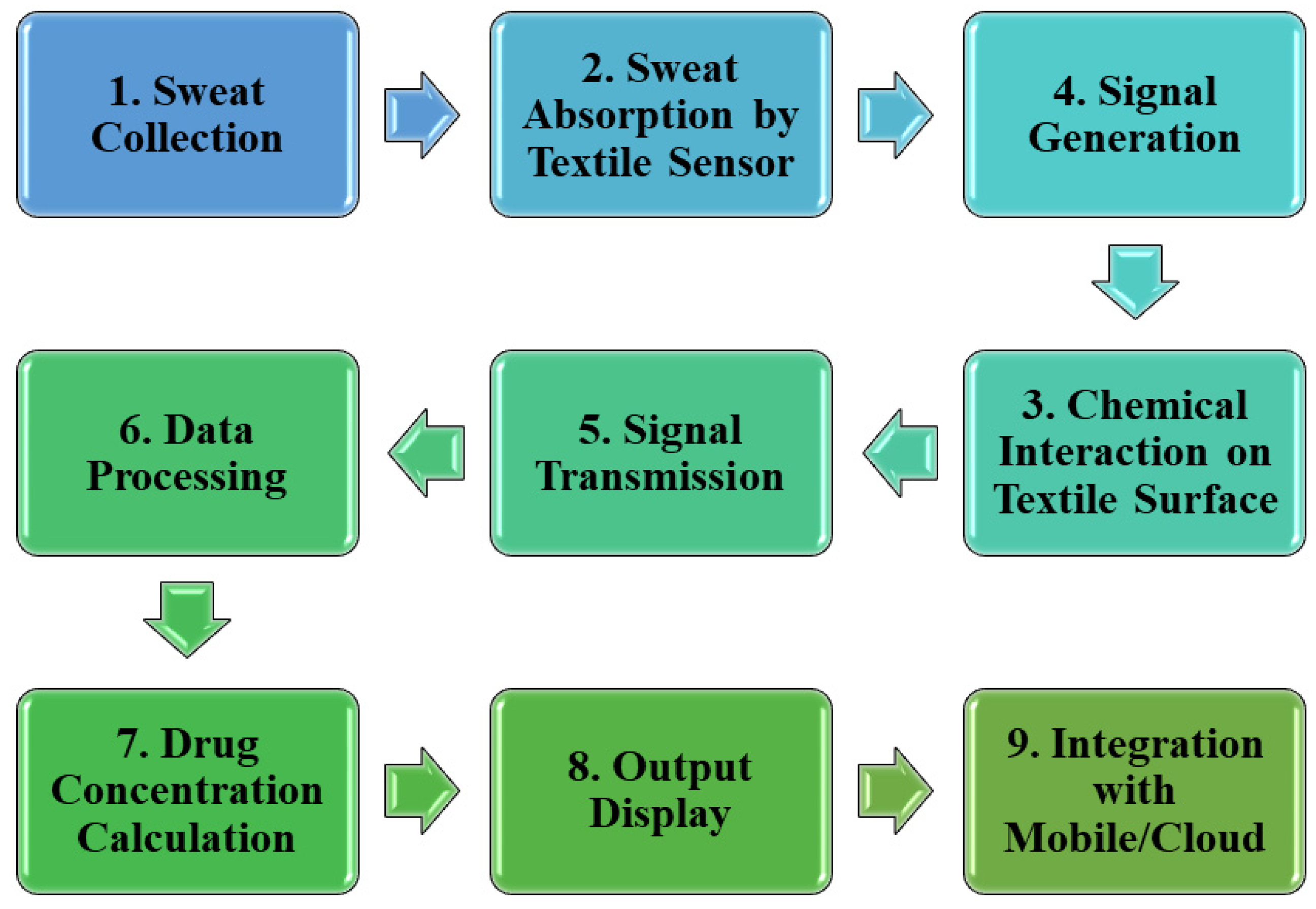
3.2. Working Procedure of Sweat Sensors
3.2.1. Sensing Mechanisms
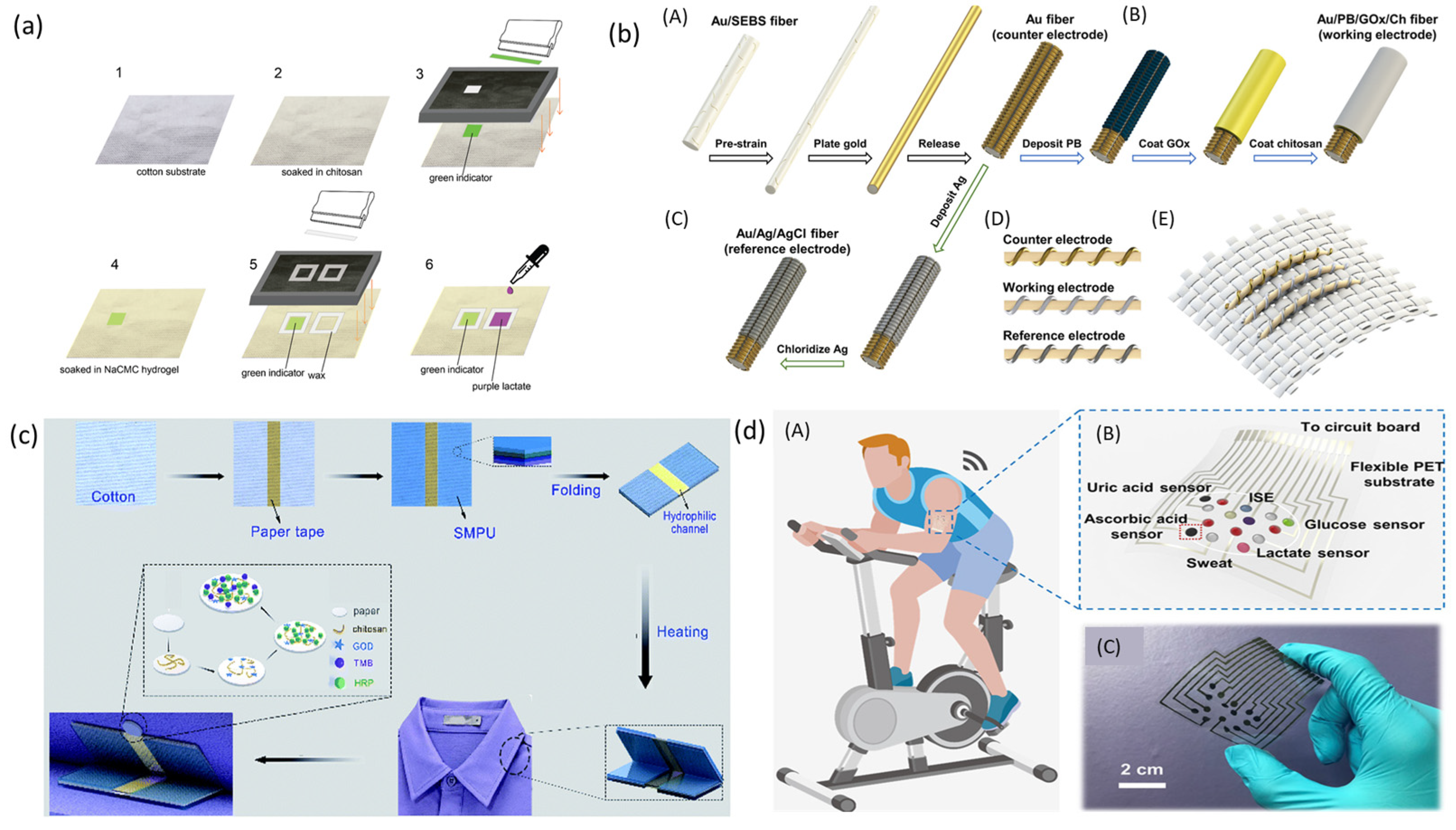
3.2.2. Materials Used in a Textile-Based Sweat Sensor
3.2.3. Miniaturization and Integration
Nanotechnology in Sweat Sensor Development
Integration of Multiple Sensors for Comprehensive Monitoring
3.3. Application
3.3.1. Disease Diagnosis and Management
Diabetes Management
Cardiac Disease Diagnosis and Management
3.3.2. Continuous Health Tracking
Physical Activity Monitoring
Mental State Monitoring
Drug Monitoring
3.3.3. Personalized Monitoring
Tailoring Treatment Plans Based on Real-Time Data
Improving Patient Outcomes through Personalized Interventions
3.3.4. Energy Harvesting
3.4. Selection and Comparative Analysis of Sensor Types
- Sensitivity: Indicates the sensor’s ability to detect minute changes in biomarker concentration.
- Selectivity: Measures the sensor’s ability to distinguish target analytes from interfering substances.
- Response Time: Refers to the time taken by the sensor to produce a measurable signal after exposure to the analyte.
- Accuracy: Represents how closely the sensor’s measurements align with the true values of the analyte concentration.
- Durability: Indicates the number of cycles or duration the sensor can maintain its performance under typical usage conditions.
4. Discussion
4.1. Technical Challenges
4.1.1. Sensor Accuracy and Reliability
4.1.2. Power Consumption and Energy Efficiency
4.1.3. Practical Considerations of Textile-Based Sweat Sensors
- Washability:
- Strain–stress and stretch test:
- Flexibility:
4.2. User Acceptance and Privacy Concerns
4.2.1. Cultural and Social Factors Influencing Adoption
4.2.2. Data Security and Privacy in Medical Monitoring
4.3. Future Research Directions
4.3.1. Advancements in Sensor Technology
4.3.2. Collaborations between Textile and Medical Research Communities
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Ray, T.R.; Choi, J.; Bandodkar, A.J.; Krishnan, S.; Gutruf, P.; Tian, L.; Ghaffari, R.; Rogers, J.A. Bio-Integrated Wearable Systems: A Comprehensive Review. Chem. Rev. 2019, 119, 5461–5533. [Google Scholar] [CrossRef] [PubMed]
- Adeniyi, E.A.; Ogundokun, R.O.; Awotunde, J.B. IoMT-based wearable body sensors network healthcare monitoring system. In IoT in Healthcare and Ambient Assisted Living; Springer: Singapore, 2021; pp. 103–121. [Google Scholar]
- Lou, Z.; Wang, L.; Jiang, K.; Wei, Z.; Shen, G. Reviews of wearable healthcare systems: Materials, devices and system integration. Mater. Sci. Eng. R Rep. 2020, 140, 100523. [Google Scholar] [CrossRef]
- George, A.H.; Shahul, A.; George, A.S. Wearable Sensors: A New Way to Track Health and Wellness. Partn. Univers. Int. Innov. J. 2023, 1, 15–34. [Google Scholar]
- Appelboom, G.; Camacho, E.; Abraham, M.E.; Bruce, S.S.; Dumont, E.L.; Zacharia, B.E.; D’amico, R.; Slomian, J.; Reginster, J.Y.; Bruyère, O.; et al. Smart wearable body sensors for patient self-assessment and monitoring. Arch. Public Health 2014, 72, 28. [Google Scholar] [CrossRef] [PubMed]
- Spanakis, E.G.; Santana, S.; Tsiknakis, M.; Marias, K.; Sakkalis, V.; Teixeira, A.; Janssen, J.H.; de Jong, H.; Tziraki, C. Technology-Based Innovations to Foster Personalized Healthy Lifestyles and Well-Being: A Targeted Review. J. Med. Internet Res. 2016, 18, e1282016. [Google Scholar] [CrossRef]
- Kalid, N.; Zaidan, A.A.; Zaidan, B.B.; Salman, O.H.; Hashim, M.; Muzammil, H. Based Real Time Remote Health Monitoring Systems: A Review on Patients Prioritization and Related “Big Data” Using Body Sensors information and Communication Technology. J. Med Syst. 2017, 42, 30. [Google Scholar] [CrossRef]
- Mshali, H.; Lemlouma, T.; Moloney, M.; Magoni, D. A survey on health monitoring systems for health smart homes. Int. J. Ind. Ergon. 2018, 66, 26–56. [Google Scholar] [CrossRef]
- Goergen, C.J.; Tweardy, M.J.; Steinhubl, S.R.; Wegerich, S.W.; Singh, K.; Mieloszyk, R.J.; Dunn, J. Detection and Monitoring of Viral Infections via Wearable Devices and Biometric Data. Annu. Rev. Biomed. Eng. 2021, 24, 1–27. [Google Scholar] [CrossRef] [PubMed]
- Ding, X.-R.; Clifton, D.; Ji, N.; Lovell, N.H.; Bonato, P.; Chen, W.; Yu, X.; Xue, Z.; Xiang, T.; Long, X.; et al. Wearable Sensing and Telehealth Technology with Potential Applications in the Coronavirus Pandemic. IEEE Rev. Biomed. Eng. 2020, 14, 48–70. [Google Scholar] [CrossRef]
- Davis, M.; Kirwan, M.; Maclay, W.; Pappas, H. Pappas, Closing the Care Gap with Wearable Devices: Innovating Healthcare with Wearable Patient Monitoring; CRC Press: Boca Raton, FL, USA, 2022. [Google Scholar]
- Legner, C.; Kalwa, U.; Patel, V.; Chesmore, A.; Pandey, S. Sweat sensing in the smart wearables era: Towards integrative, multifunctional and body-compliant perspiration analysis. Sens. Actuators A Phys. 2019, 296, 200–221. [Google Scholar] [CrossRef]
- Yin, J.; Li, J.; Reddy, V.S.; Ji, D.; Ramakrishna, S.; Xu, L. Flexible Textile-Based Sweat Sensors for Wearable Applications. Biosensors 2023, 13, 127. [Google Scholar] [CrossRef] [PubMed]
- Sim, D.; Brothers, M.C.; Slocik, J.M.; Islam, A.E.; Maruyama, B.; Grigsby, C.C.; Kim, S.S. Biomarkers and detection Platforms for human health and performance monitoring: A Review. Adv. Sci. 2022, 9, 2104426. [Google Scholar] [CrossRef]
- Xu, J.; Fang, Y.; Chen, J. Wearable Biosensors for Non-Invasive Sweat Diagnostics. Biosensors 2021, 11, 245. [Google Scholar] [CrossRef] [PubMed]
- Heng, W.; Yang, G.; Kim, W.S.; Xu, K. Emerging wearable flexible sensors for sweat analysis. Biodes. Manuf. 2021, 5, 64–84. [Google Scholar] [CrossRef]
- Xing, Z.; Hui, J.; Lin, B.; Wu, Z.; Mao, H. Recent Advances in Wearable Sensors for the Monitoring of Sweat: A Comprehensive Tendency Summary. Chemosensors 2023, 11, 470. [Google Scholar] [CrossRef]
- Sony, S.; LaVenture, S.; Sadhu, A. A literature review of next-generation smart sensing technology in structural health monitoring. Struct. Control Health Monit. 2019, 26, e23212019. [Google Scholar] [CrossRef]
- Wang, X.; Liu, Z.; Zhang, T. Flexible Sensing Electronics for Wearable/Attachable Health Monitoring. Small 2017, 13, 1602790. [Google Scholar] [CrossRef]
- Angelucci, A.; Cavicchioli, M.; Cintorrino, I.A.; Lauricella, G.; Rossi, C.; Strati, S.; Aliverti, A. Smart Textiles and Sensorized Garments for Physiological Monitoring: A Review of Available Solutions and Techniques. Sensors 2021, 21, 814. [Google Scholar] [CrossRef] [PubMed]
- Chaudhary, M.H.; Dev, S.; Kumari, A.; Kanwal, K.; Jadav, D.N.; Rasool, S.; Mohamad, T. Holistic approaches to arrhythia management: Combining medication, ablation, and device interventions. Cureus 2023, 15, e459582023. [Google Scholar]
- Gu, Y.; Zalkikar, A.; Liu, M.; Kelly, L.; Hall, A.; Daly, K.; Ward, T. Predicting medication adherence using ensemble learning and deep learning models with large scale healthcare data. Sci. Rep. 2021, 11, 18961. [Google Scholar] [CrossRef]
- Mohan, A.V.; Rajendran, V.; Mishra, R.K.; Jayaraman, M. Recent advances and perspectives in sweat based wearable electrochemical sensors. TrAC Trends Anal. Chem. 2020, 131, 116024. [Google Scholar] [CrossRef]
- Qiao, L.; Benzigar, M.R.; Subramony, J.A.; Lovell, N.H.; Liu, G. Advances in sweat wearables: Sample extraction, real-time biosensing, and flexible platforms. ACS Appl. Mater. Interfaces 2020, 12, 34337–34361. [Google Scholar] [CrossRef] [PubMed]
- Kan, C.-W.; Lam, Y.-L. Future Trend in Wearable Electronics in the Textile Industry. Appl. Sci. 2021, 11, 3914. [Google Scholar] [CrossRef]
- Tadesse, M.G.; Loghin, C.; Dulgheriu, I.; Loghin, E. Comfort evaluation of wearable functional textiles. Materials 2021, 14, 6466. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Badea, M.; Tiwari, S.; Marty, J.L. Wearable Biosensors: An Alternative and Practical Approach in Healthcare and Disease Monitoring. Molecules 2021, 26, 748. [Google Scholar] [CrossRef] [PubMed]
- Shi, J.; Liu, S.; Zhang, L.; Yang, B.; Shu, L.; Yang, Y.; Ren, M.; Wang, Y.; Chen, J.; Chen, W.; et al. Smart Textile-Integrated Microelectronic Systems for Wearable Applications. Adv. Mater. 2019, 32, e19019582019. [Google Scholar] [CrossRef] [PubMed]
- Yokus, M.A.; Daniele, M.A. Integrated non-invasive biochemical and biophysical sensing systems for health and performance monitoring: A systems perspective. Biosens. Bioelectron. 2021, 184, 113249. [Google Scholar] [CrossRef] [PubMed]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; McKenzie, J.E. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Promphet, N.; Rattanawaleedirojn, P.; Siralertmukul, K.; Soatthiyanon, N.; Potiyaraj, P.; Thanawattano, C.; Rodthongkum, N. Non-invasive textile based colorimetric sensor for the simultaneous detection of sweat pH and lactate. Talanta 2019, 192, 424–430. [Google Scholar] [CrossRef]
- Zhao, Y.; Zhai, Q.; Dong, D.; An, T.; Gong, S.; Shi, Q.; Cheng, W. Highly Stretchable and Strain-Insensitive Fiber-Based Wearable Electrochemical Biosensor to Monitor Glucose in the Sweat. Anal. Chem. 2019, 91, 6569–6576. [Google Scholar] [CrossRef]
- He, J.; Xiao, G.; Chen, X.; Qiao, Y.; Xu, D.; Lu, Z. A thermoresponsive microfluidic system integrating a shape memory polymer-modified textile and a paper-based colorimetric sensor for the detection of glucose in human sweat. RSC Adv. 2019, 9, 23957–23963. [Google Scholar] [CrossRef] [PubMed]
- He, W.; Wang, C.; Wang, H.; Jian, M.; Lu, W.; Liang, X.; Zhang, X.; Yang, F.; Zhang, Y. Integrated textile sensor patch for real-time and multiplex sweat analysis. Sci. Adv. 2019, 5, eaax0649. [Google Scholar] [CrossRef] [PubMed]
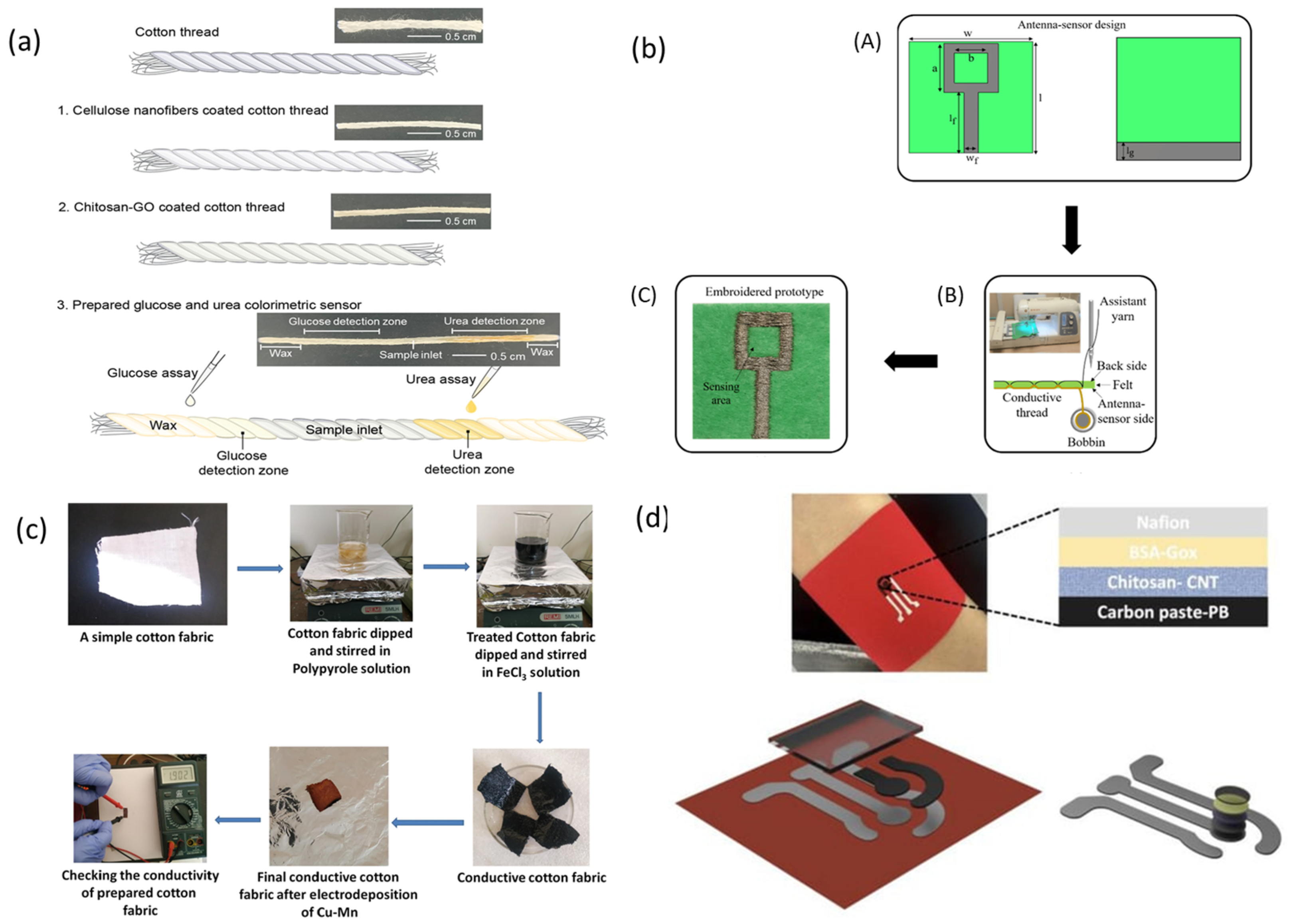
- Promphet, N.; Hinestroza, J.P.; Rattanawaleedirojn, P.; Soatthiyanon, N.; Siralertmukul, K.; Potiyaraj, P.; Rodthongkum, N. Cotton thread-based wearable sensor for non-invasive simultaneous diagnosis of diabetes and kidney failure. Sens. Actuators B Chem. 2020, 321, 128549. [Google Scholar] [CrossRef]
- El Gharbi, M.; Fernández-García, R.; Gil, I. Textile Antenna-Sensor for In Vitro Diagnostics of Diabetes. Electronics 2021, 10, 1570. [Google Scholar] [CrossRef]
- Singh, A.; Sharma, A.; Arya, S. Human sweat-based wearable glucose sensor on cotton fabric for real-time monitoring. J. Anal. Sci. Technol. 2022, 13, 11. [Google Scholar] [CrossRef]
- Khosravi, S.; Soltanian, S.; Servati, A.; Khademhosseini, A.; Zhu, Y.; Servati, P. Screen-Printed Textile-Based Electrochemical Biosensor for Noninvasive Monitoring of Glucose in Sweat. Biosensors 2023, 13, 684. [Google Scholar] [CrossRef] [PubMed]
- Xiao, G.; He, J.; Chen, X.; Qiao, Y.; Wang, F.; Xia, Q.; Yu, L.; Lu, Z. A wearable, cotton thread/paper-based microfluidic device coupled with smartphone for sweat glucose sensing. Cellulose 2019, 26, 4553–4562. [Google Scholar] [CrossRef]
- Manjakkal, L.; Pullanchiyodan, A.; Yogeswaran, N.; Hosseini, E.S.; Dahiya, R. A Wearable Supercapacitor Based on Conductive PEDOT:PSS-Coated Cloth and a Sweat Electrolyte. Adv. Mater. 2020, 32, e19072542020. [Google Scholar] [CrossRef]
- Mugo, S.M.; Lu, W.; Robertson, S. A wearable, textile-based polyacrylate imprinted electrochemical sensor for cortisol detection in sweat. Biosensors 2022, 12, 854. [Google Scholar] [CrossRef]
- Yoon, J.H.; Kim, S.-M.; Eom, Y.; Koo, J.M.; Cho, H.-W.; Lee, T.J.; Lee, K.G.; Park, H.J.; Kim, Y.K.; Yoo, H.-J.; et al. Extremely Fast Self-Healable Bio-Based Supramolecular Polymer for Wearable Real-Time Sweat-Monitoring Sensor. ACS Appl. Mater. Interfaces 2019, 11, 46165–46175. [Google Scholar] [CrossRef]
- He, X.; Yang, S.; Pei, Q.; Song, Y.; Liu, C.; Xu, T.; Zhang, X. Integrated smart janus textile bands for self-pumping sweat sampling and analysis. ACS Sens. 2020, 5, 1548–1554. [Google Scholar] [CrossRef] [PubMed]
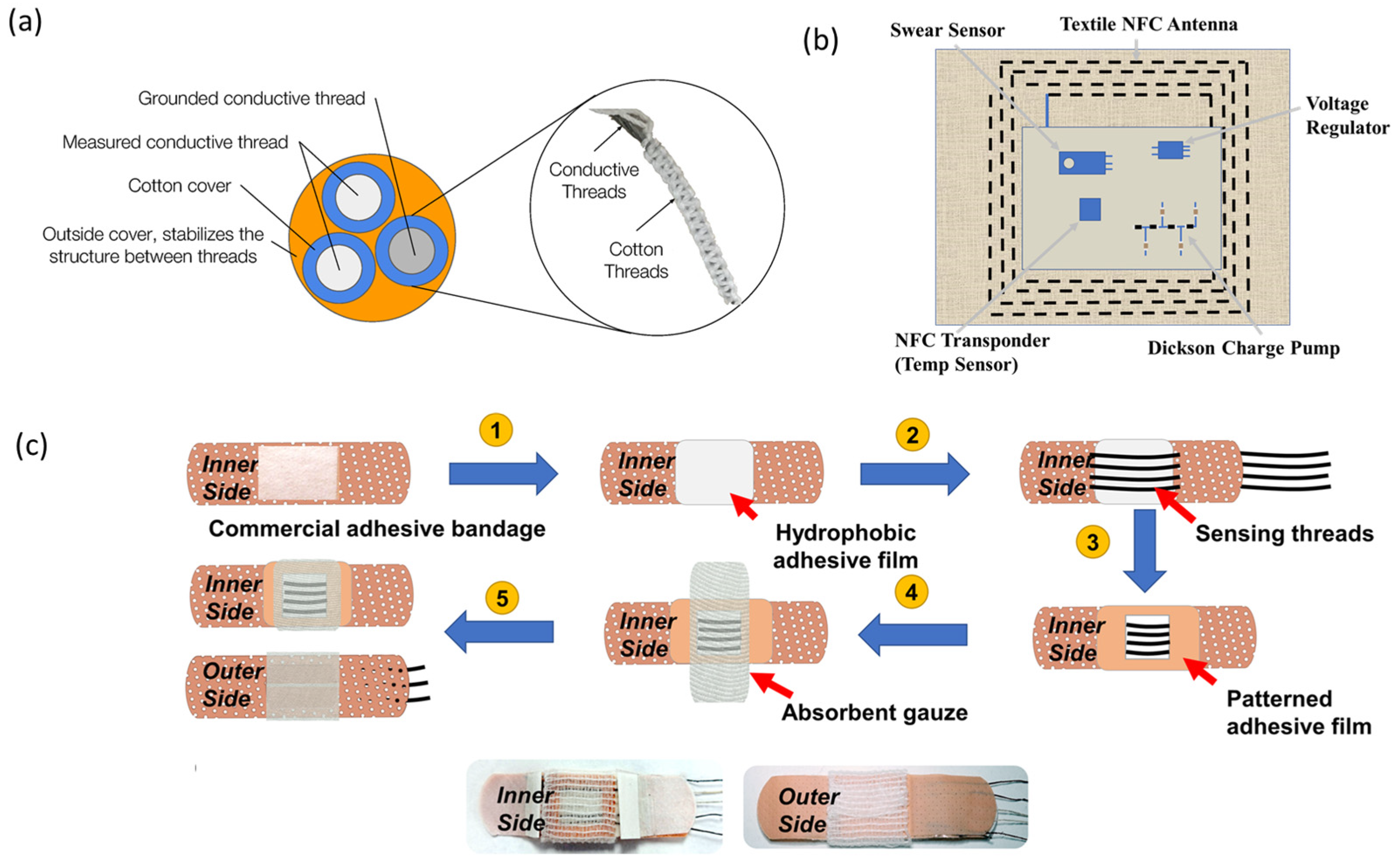
- Jia, J.; Xu, C.; Pan, S.; Xia, S.; Wei, P.; Noh, H.Y.; Jiang, X. Conductive thread-based textile sensor for continuous perspiration level monitoring. Sensors 2018, 18, 3775. [Google Scholar] [CrossRef] [PubMed]
- Jiang, Y.; Pan, K.; Leng, T.; Hu, Z. Smart Textile Integrated Wireless Powered Near Field Communication Body Temperature and Sweat Sensing System. IEEE J. Electromagn. RF Microw. Med. Biol. 2019, 4, 164–170. [Google Scholar] [CrossRef]
- Terse-Thakoor, T.; Punjiya, M.; Matharu, Z.; Lyu, B.; Ahmad, M.; Giles, G.E.; Sonkusale, S. Thread-based multiplexed sensor patch for real-time sweat monitoring. NPJ Flex. Electron. 2020, 4, 18. [Google Scholar] [CrossRef]
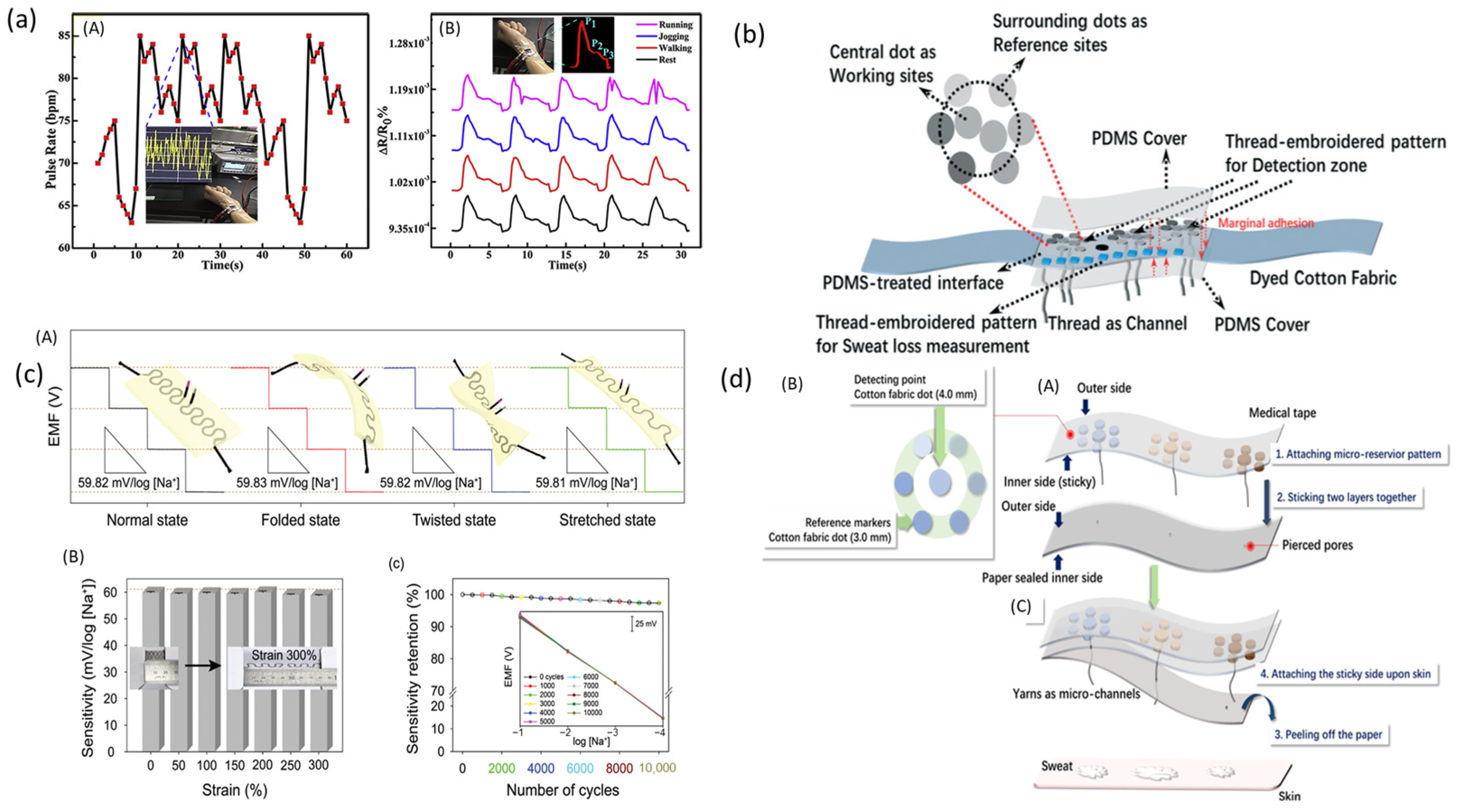
- Shathi, M.A.; Chen, M.; Khoso, N.A.; Rahman, T.; Bhattacharjee, B. Graphene coated textile based highly flexible and washable sports bra for human health monitoring. Mater. Des. 2020, 193, 108792. [Google Scholar] [CrossRef]
- Zhao, Z.; Li, Q.; Chen, L.; Zhao, Y.; Gong, J.; Li, Z.; Zhang, J. A thread/fabric-based band as a flexible and wearable microfluidic device for sweat sensing and monitoring. Lab Chip 2020, 21, 916–932. [Google Scholar] [CrossRef]
- Kim, S.J.; Kil, M.S.; Park, H.J.; Yoon, J.H.; Kim, J.; Bae, N.H.; Lee, K.G.; Choi, B.G. Highly Stretchable and Conductive Carbon Thread Incorporated into Elastic Rubber for Wearable Real-Time Monitoring of Sweat during Stretching Exercise. Adv. Mater. Technol. 2023, 8, 2201042. [Google Scholar] [CrossRef]
- Yu, W.; Li, Q.; Zhao, Z.; Gong, J.; Li, Z.; Zhang, J. A yarn/fabric-based microfluidic patch for sweat sensing and monitoring. J. Text. Inst. 2023, 1–12. [Google Scholar] [CrossRef]
- Zhao, C.; Li, X.; Wu, Q.; Liu, X. A thread-based wearable sweat nanobiosensor. Biosens. Bioelectron. 2021, 188, 113270. [Google Scholar] [CrossRef]
- Kwon, C.H.; Bin Park, Y.; Lee, J.A.; Choi, Y.-B.; Kim, H.-H.; Lima, M.D.; Baughman, R.H.; Kim, S.J. Mediator-free carbon nanotube yarn biofuel cell. RSC Adv. 2016, 6, 48346–48350. [Google Scholar] [CrossRef]
- Yin, S.; Jin, Z.; Miyake, T. Wearable high-powered biofuel cells using enzyme/carbon nanotube composite fibers on textile cloth. Biosens. Bioelectron. 2019, 141, 111471. [Google Scholar] [CrossRef]
- Lv, J.; Jeerapan, I.; Tehrani, F.; Yin, L.; Silva-Lopez, C.A.; Jang, J.-H.; Joshuia, D.; Shah, R.; Liang, Y.; Xie, L.; et al. Sweat-based wearable energy harvesting-storage hybrid textile devices. Energy Environ. Sci. 2018, 11, 3431–3442. [Google Scholar] [CrossRef]
- Huang, X.; Liu, Y.; Zhou, J.; Nejad, S.K.; Wong, T.H.; Huang, Y.; Yu, X. Garment embedded sweat-activated batteries in wearable electronics for continuous sweat monitoring. NPJ Flex. Electron. 2022, 6, 10. [Google Scholar] [CrossRef]
- Xiao, G.; Ju, J.; Li, M.; Wu, H.; Jian, Y.; Sun, W.; Wang, W.; Li, C.M.; Qiao, Y.; Lu, Z. Weavable yarn-shaped supercapacitor in sweat-activated self-charging power textile for wireless sweat biosensing. Biosens. Bioelectron. 2023, 235, 115389. [Google Scholar] [CrossRef] [PubMed]
- Jeerapan, I.; Sempionatto, J.R.; Pavinatto, A.; You, J.-M.; Wang, J. Stretchable biofuel cells as wearable textile-based self-powered sensors. J. Mater. Chem. A 2016, 4, 18342–18353. [Google Scholar] [CrossRef]
- Wang, L.; Xu, T.; Fan, C.; Zhang, X. Wearable strain sensor for real-time sweat volume monitoring. iScience 2020, 24, 102028. [Google Scholar] [CrossRef] [PubMed]
- Coppedè, N.; Giannetto, M.; Villani, M.; Lucchini, V.; Battista, E.; Careri, M.; Zappettini, A. Ion selective textile organic electrochemical transistor for wearable sweat monitoring. Org. Electron. 2019, 78, 105579. [Google Scholar] [CrossRef]
- Han, Y.; Fang, X.; Li, H.; Zha, L.; Guo, J.; Zhang, X. Sweat Sensor Based on Wearable Janus Textiles for Sweat Collection and Microstructured Optical Fiber for Surface-Enhanced Raman Scattering Analysis. ACS Sens. 2023, 8, 4774–4781. [Google Scholar] [CrossRef]
- Jang, M.; Kim, H.-D.; Koo, H.-J.; So, J.-H. Textile-Based Wearable Sensor for Skin Hydration Monitoring. Sensors 2022, 22, 6985. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Chen, G.; Cui, Y.; Ji, S.; Liu, Z.; Wan, C.; Liu, Y.; Lu, Y.; Wang, C.; Zhang, N.; et al. Highly Thermal-Wet Comfortable and Conformal Silk-Based Electrodes for On-Skin Sensors with Sweat Tolerance. ACS Nano 2021, 15, 9955–9966. [Google Scholar] [CrossRef]
- Stojanović, G.M.; Radetić, M.M.; Šaponjić, Z.V.; Radoičić, M.B.; Radovanović, M.R.; Popović, V.; Vukmirović, S.N. A Textile-Based Microfluidic Platform for the Detection of Cytostatic Drug Concentration in Sweat Samples. Appl. Sci. 2020, 10, 4392. [Google Scholar] [CrossRef]
- Chung, M.; Fortunato, G.; Radacsi, N. Wearable flexible sweat sensors for healthcare monitoring: A review. J. R. Soc. Interface 2019, 16, 20190217. [Google Scholar] [CrossRef] [PubMed]
- Wen, F.; He, T.; Liu, H.; Chen, H.Y.; Zhang, T.; Lee, C. Advances in chemical sensing tech-nology for enabling the next-generation self-sustainable integrated wearable system in the IoT era. Nano Energy 2020, 78, 105155. [Google Scholar] [CrossRef]
- Tian, H.; Ma, J.; Li, Y.; Xiao, X.; Zhang, M.; Wang, H.; Zhu, N.; Hou, C.; Ulstrup, J. Electrochemical sensing fibers for wearable health monitoring devices. Biosens. Bioelectron. 2024, 246, 115890. [Google Scholar] [CrossRef]
- Sharma, A.; Tok AI, Y.; Alagappan, P.; Liedberg, B. Point of care testing of sports bi-omarkers: Potential applications, recent advances and future outlook. TrAC Trends Anal. Chem. 2021, 142, 116327. [Google Scholar] [CrossRef]
- Feng, T.; Ling, D.; Li, C.; Zheng, W.; Zhang, S.; Li, C.; Mao, Y. Stretchable on-skin touchless screen sensor enabled by ionic hydrogel. Nano Res. 2024, 17, 4462–4470. [Google Scholar] [CrossRef]
- Kakria, P.; Tripathi, N.K.; Kitipawang, P. A Real-Time Health Monitoring System for Remote Cardiac Patients Using Smartphone and Wearable Sensors. Int. J. Telemed. Appl. 2015, 2015, 373474. [Google Scholar] [CrossRef] [PubMed]
- Kang, T.H. Textile-Embedded Sensors for Wearable Physiological Monitoring Systems; NC State University: Raleigh, NC, USA, 2007. [Google Scholar]
- Promphet, N.; Ummartyotin, S.; Ngeontae, W.; Puthongkham, P.; Rodthongkum, N. Non-invasive wearable chemical sensors in real-life applications. Anal. Chim. Acta 2021, 1179, 338643. [Google Scholar] [CrossRef] [PubMed]
- Khan, A.; Haque, N.; Kabiraz, D.C.; Yeasin, A.; Al Rashid, H.; Sarker, A.C.; Hossain, G. A review on advanced nanocomposites materials based smart textile biosensor for healthcare monitoring from human sweat. Sens. Actuators A Phys. 2023, 350, 114093. [Google Scholar] [CrossRef]
- Liu, Y.; Pharr, M.; Salvatore, G.A. Lab-on-skin: A review of flexible and stretchable electronics for wearable health monitoring. ACS Nano 2017, 11, 9614–9635. [Google Scholar] [CrossRef]
- Cao, X.; Halder, A.; Tang, Y.; Hou, C.; Wang, H.; Duus, J.; Chi, Q. Engineering two-dimensional layered nanomaterials for wearable biomedical sensors and power devices. Mater. Chem. Front. 2018, 2, 1944–1986. [Google Scholar] [CrossRef]
- Jo, S.; Sung, D.; Kim, S.; Koo, J. A review of wearable biosensors for sweat analysis. Biomed. Eng. Lett. 2021, 11, 117–129. [Google Scholar] [CrossRef] [PubMed]
- Haleem, A.; Javaid, M.; Singh, R.P.; Suman, R.; Rab, S. Biosensors applications in medical field: A brief review. Sens. Int. 2021, 2, 100100. [Google Scholar] [CrossRef]
- Chang, Y.; Zuo, J.; Zhang, H.; Duan, X. State-of-the-art and recent developments in micro/nanoscale pressure sensors for smart wearable devices and health monitoring systems. Nanotechnol. Precis. Eng. (NPE) 2020, 3, 43–52. [Google Scholar] [CrossRef]
- Villena Gonzales, W.; Mobashsher, A.T.; Abbosh, A. The progress of glucose monitoring—A review of invasive to minimally and non-invasive techniques, devices and sensors. Sensors 2019, 19, 800. [Google Scholar] [CrossRef] [PubMed]
- Zhong, B.; Jiang, K.; Wang, L.; Shen, G. Wearable Sweat Loss Measuring Devices: From the Role of Sweat Loss to Advanced Mechanisms and Designs. Adv. Sci. 2021, 9, 2103257. [Google Scholar] [CrossRef] [PubMed]
- Spychalska, K.; Zając, D.; Baluta, S.; Halicka, K.; Cabaj, J. Functional Polymers Structures for (Bio)Sensing Application—A Review. Polymers 2020, 12, 1154. [Google Scholar] [CrossRef]
- Clark, K.M.; Ray, T.R. Recent Advances in Skin-Interfaced Wearable Sweat Sensors: Opportunities for Equitable Personalized Medicine and Global Health Diagnostics. ACS Sens. 2023, 8, 3606–3622. [Google Scholar] [CrossRef]
- Saha, T.; Mukherjee, S.; Dickey, M.D.; Velev, O.D. Harvesting and manipulating sweat and interstitial fluid in microfluidic devices. Lab Chip 2024, 24, 1244–1265. [Google Scholar] [CrossRef]
- Saha, T.; Del Caño, R.; De la Paz, E.; Sandhu, S.S.; Wang, J. Access and Management of Sweat for Non-Invasive Biomarker Monitoring: A Comprehensive Review. Small 2022, 19, e22060642022. [Google Scholar] [CrossRef]
- Ramachandran, B.; Liao, Y.-C. Microfluidic wearable electrochemical sweat sensors for health monitoring. Biomicrofluidics 2022, 16, 051501. [Google Scholar] [CrossRef]
- Fan, R.; Andrew, T.L. Perspective—Challenges in Developing Wearable Electrochemical Sensors for Longitudinal Health Monitoring. J. Electrochem. Soc. 2020, 167, 037542. [Google Scholar] [CrossRef]
- Liu, Y.; Li, J.; Xiao, S.; Liu, Y.; Bai, M.; Gong, L.; Chen, D. Revolutionizing precision medicine: Exploring wearable sensors for therapeutic drug monitoring and personalized therapy. Biosensors 2023, 13, 726. [Google Scholar] [CrossRef]
- Bennet, D.; Khorsandian, Y.; Pelusi, J.; Mirabella, A.; Pirrotte, P.; Zenhausern, F. Molecular and physical technologies for monitoring fluid and electrolyte imbalance: A focus on cancer population. Clin. Transl. Med. 2021, 11, e4612021. [Google Scholar] [CrossRef] [PubMed]
- Holzer, R.; Bloch, W.; Brinkmann, C. Minimally Invasive Electrochemical Patch-Based Sensor System for Monitoring Glucose and Lactate in the Human Body—A Survey-Based Analysis of the End-User’s Perspective. Sensors 2020, 20, 5761. [Google Scholar] [CrossRef]
- Mahato, K.; Wang, J. Electrochemical sensors: From the bench to the skin. Sens. Actuators B Chem. 2021, 344, 130178. [Google Scholar] [CrossRef]
- Ye, S.; Feng, S.; Huang, L.; Bian, S. Recent Progress in Wearable Biosensors: From Healthcare Monitoring to Sports Analytics. Biosensors 2020, 10, 205. [Google Scholar] [CrossRef]
- Bhatia, D.; Paul, S.; Acharjee, T.; Ramachairy, S.S. Biosensors and their widespread impact on human health. Sens. Int. 2024, 5, 100257. [Google Scholar] [CrossRef]
- Ji, W.; Zhu, J.; Wu, W.; Wang, N.; Wang, J.; Wu, J.; Wu, Q.; Wang, X.; Yu, C.; Wei, G.; et al. Wearable Sweat Biosensors Refresh Personalized Health/Medical Diagnostics. Research 2021, 2021, 9757126. [Google Scholar] [CrossRef]
- Tu, J.; Torrente-Rodríguez, R.M.; Wang, M.; Gao, W. The Era of Digital Health: A Review of Portable and Wearable Affinity Biosensors. Adv. Funct. Mater. 2019, 30, 1906713. [Google Scholar] [CrossRef]
- Shokrekhodaei, M.; Cistola, D.P.; Roberts, R.C.; Quinones, S. Non-invasive glucose moni-toring using optical sensor and machine learning techniques for diabetes applications. IEEE Access 2021, 9, 73029–73045. [Google Scholar] [CrossRef] [PubMed]
- Hong, W.; Lee, W.G. Wearable sensors for continuous oral cavity and dietary monitoring toward personalized healthcare and digital medicine. Analyst 2020, 145, 7796–7808. [Google Scholar] [CrossRef] [PubMed]
- Kazanskiy, N.L.; Butt, M.A.; Khonina, S.N. Recent Advances in Wearable Optical Sensor Automation Powered by Battery versus Skin-like Battery-Free Devices for Personal Healthcare—A Review. Nanomaterials 2022, 12, 334. [Google Scholar] [CrossRef] [PubMed]
- Pour SR, S.; Calabria, D.; Emamiamin, A.; Lazzarini, E.; Pace, A.; Guardigli, M.; Mirasoli, M. Microfluidic-Based Non-Invasive Wearable Biosensors for Real-Time Monitoring of Sweat Biomarkers. Biosensors 2024, 14, 29. [Google Scholar] [CrossRef] [PubMed]
- Zhao, W.-S.; Wang, B.-X.; Wang, D.-W.; You, B.; Liu, Q.; Wang, G. Swarm intelligence algorithm-based optimal design of microwave microfluidic sensors. IEEE Trans. Ind. Electron. 2021, 69, 2077–2087. [Google Scholar] [CrossRef]
- Zhang, S.; Tan, R.; Xu, X.; Iqbal, S.; Hu, J. Fibers/Textiles-Based Flexible Sweat Sensors: A Review. ACS Mater. Lett. 2023, 5, 1420–1440. [Google Scholar] [CrossRef]
- Chen, Y.-C.; Shan, S.-S.; Liao, Y.-T.; Liao, Y.-C. Bio-inspired fractal textile device for rapid sweat collection and monitoring. Lab Chip 2021, 21, 2524–2533. [Google Scholar] [CrossRef] [PubMed]
- Cho, I.-H.; Kim, D.H.; Park, S. Electrochemical biosensors: Perspective on functional nanomaterials for on-site analysis. Biomater. Res. 2020, 24, 1–12. [Google Scholar] [CrossRef] [PubMed]
- Zafar, H.; Channa, A.; Jeoti, V.; Stojanović, G.M. Comprehensive Review on Wearable Sweat-Glucose Sensors for Continuous Glucose Monitoring. Sensors 2022, 22, 638. [Google Scholar] [CrossRef]
- Sun, J.; Lu, Y.; He, L.; Pang, J.; Yang, F.; Liu, Y. Colorimetric sensor array based on gold nanoparticles: Design principles and recent advances. TrAC Trends Anal. Chem. 2020, 122, 115754. [Google Scholar] [CrossRef]
- Shao, Y.; Ying, Y.; Ping, J. Recent advances in solid-contact ion-selective electrodes: Functional materials, transduction mechanisms, and development trends. Chem. Soc. Rev. 2020, 49, 4405–4465. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Cheng, H.; Wang, X. Skin-interfaced colorimetric microfluidic devices for on-demand sweat analysis. NPJ Flex. Electron. 2023, 7, 43. [Google Scholar] [CrossRef]
- Zhai, Q.; Yap, L.W.; Wang, R.; Gong, S.; Guo, Z.; Liu, Y.; Lyu, Q.; Wang, J.; Simon, G.P.; Cheng, W. Vertically Aligned Gold Nanowires as Stretchable and Wearable Epidermal Ion-Selective Electrode for Noninvasive Multiplexed Sweat Analysis. Anal. Chem. 2020, 92, 4647–4655. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.-R.; Lee, S.M.; Mahmood, M.; Kwon, S.; Kim, Y.-S.; Lee, Y.; Yeo, W.-H. Development of Flexible Ion-Selective Electrodes for Saliva Sodium Detection. Sensors 2021, 21, 1642. [Google Scholar] [CrossRef] [PubMed]
- Ma, M.; Kim, S.; Chorkendorff, I.; Seger, B. Role of ion-selective membranes in the carbon balance for CO2 electroreduction via gas diffusion electrode reactor designs. Chem. Sci. 2020, 11, 8854–8861. [Google Scholar] [CrossRef] [PubMed]
- Kucherenko, I.S.; Sanborn, D.; Chen, B.; Garland, N.; Serhan, M.; Forzani, E.; Gomes, C.; Claussen, J.C. Ion-Selective Sensors Based on Laser-Induced Graphene for Evaluating Human Hydration Levels Using Urine Samples. Adv. Mater. Technol. 2020, 5, 1901037. [Google Scholar] [CrossRef]
- Gao, Y.; Huang, Y.; Ge, J.; Sun, L.; Zhou, A.; Feng, S.; Xu, Y.; Ning, X. An interrelated CataFlower enzyme system for sensitively monitoring sweat glucose. Talanta 2021, 235, 122799. [Google Scholar] [CrossRef] [PubMed]
- Yokus, M.A.; Songkakul, T.; Pozdin, V.A.; Bozkurt, A.; Daniele, M.A. Wearable multiplexed biosensor system toward continuous monitoring of metabolites. Biosens. Bioelectron. 2020, 153, 112038. [Google Scholar] [CrossRef]
- Bhardwaj, S.; Sharma, D.; Singh, S.; Ramamurthy, P.C.; Verma, T.; Pujari, M.; Singh, J.; Kapoor, D.; Prasad, R. Physiological and molecular insights into the role of silicon in improving plant performance under abiotic stresses. Plant Soil 2022, 486, 25–43. [Google Scholar] [CrossRef]
- Li, G.; Wen, D. Wearable biochemical sensors for human health monitoring: Sensing mate-rials and manufacturing technologies. J. Mater. Chem. B 2020, 8, 3423–3436. [Google Scholar] [CrossRef]
- Zhang, J.; Hurren, C.; Lu, Z.; Wang, D. Nanofiber-based colorimetric platform for point-of-care detection of E. coli. Chem. Eng. J. 2023, 463, 142357. [Google Scholar] [CrossRef]
- Brink, W.v.D.; Bloem, R.; Ananth, A.; Kanagasabapathi, T.; Amelink, A.; Bouwman, J.; Gelinck, G.; van Veen, S.; Boorsma, A.; Wopereis, S. Digital Resilience Biomarkers for Personalized Health Maintenance and Disease Prevention. Front. Digit. Health 2021, 2, 614670. [Google Scholar] [CrossRef]
- Patel, V.; Mardolkar, A.; Shelar, A.; Tiwari, R.; Srivastava, R. Wearable sweat chloride sensors: Materials, fabrication and its applications. Anal. Methods 2024, 16, 1439–1453. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; Lee, B.; Reeder, J.T.; Seo, S.H.; Lee, S.-U.; Hourlier-Fargette, A.; Shin, J.; Sekine, Y.; Jeong, H.; Oh, Y.S.; et al. Soft, skin-interfaced microfluidic systems with integrated immunoassays, fluorometric sensors, and impedance measurement capabilities. Proc. Natl. Acad. Sci. USA 2020, 117, 27906–27915. [Google Scholar] [CrossRef] [PubMed]
- Huifeng, W.; Kadry, S.N.; Raj, E.D. Continuous health monitoring of sportsperson using IoT devices based wearable technology. Comput. Commun. 2020, 160, 588–595. [Google Scholar] [CrossRef]
- Libanori, A.; Chen, G.; Zhao, X.; Zhou, Y.; Chen, J. Smart textiles for personalized healthcare. Nat. Electron. 2022, 5, 142–156. [Google Scholar] [CrossRef]
- Hassan Akhtar, M.; Azhar Hayat Nawaz, M.; Abbas, M.; Liu, N.; Han, W.; Lv, Y.; Yu, C. Advances in pH Sensing: From Traditional Approaches to Next-Generation Sensors in Biological Contexts. Chem. Rec. 2024, e202300369. [Google Scholar] [CrossRef] [PubMed]
- Justino, C.I.L.; Freitas, A.C.; Pereira, R.; Duarte, A.C.; Santos, T.A.P.R. Recent developments in recognition elements for chemical sensors and biosensors. TrAC Trends Anal. Chem. 2015, 68, 2–17. [Google Scholar] [CrossRef]
- Liu, M.; Wang, S.; Xiong, Z.; Zheng, Z.; Ma, N.; Li, L.; Gao, Q.; Ge, C.; Wang, Y.; Zhang, T. Perspiration permeable, textile embeddable microfluidic sweat sensor. Biosens. Bioelectron. 2023, 237, 115504. [Google Scholar] [CrossRef]
- Min, J.; Tu, J.; Xu, C.; Lukas, H.; Shin, S.; Yang, Y.; Solomon, S.A.; Mukasa, D.; Gao, W. Skin-Interfaced Wearable Sweat Sensors for Precision Medicine. Chem. Rev. 2023, 123, 5049–5138. [Google Scholar] [CrossRef]
- Liu, Y.; Li, J.; Xu, D.; Su, Z.; Ge, C.; Chen, Z.; Xu, W.; Liu, K. Facile and Scalable Fabrication of Hydrophilic/Hydrophobic Janus Fabric for Personal Sweat Monitoring and Perspiration Management. Adv. Mater. Technol. 2023, 8, 2300543. [Google Scholar] [CrossRef]
- Possanzini, L.; Decataldo, F.; Mariani, F.; Gualandi, I.; Tessarolo, M.; Scavetta, E.; Fraboni, B. Textile sensors platform for the selective and simultaneous detection of chloride ion and pH in sweat. Sci. Rep. 2020, 10, 17180. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.; Sato, Y.; Guo, Y. Microelectronic fibers for multiplexed sweat sensing. Anal. Bioanal. Chem. 2023, 415, 4307–4318. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Lu, J.; Li, Q.; Li, L.; He, E.; Jiao, Y.; Ye, T.; Zhang, Y. A Core–Sheath Sensing Yarn-Based Electrochemical Fabric System for Powerful Sweat Capture and Stable Sensing. Adv. Funct. Mater. 2022, 32, 2200922. [Google Scholar] [CrossRef]
- Morris, D.; Coyle, S.; Wu, Y.; Lau, K.T.; Wallace, G.; Diamond, D. Bio-sensing textile based patch with integrated optical detection system for sweat monitoring. Sens. Actuators B Chem. 2009, 139, 231–236. [Google Scholar] [CrossRef]
- Bariya, M.; Nyein, H.Y.Y.; Javey, A. Wearable sweat sensors. Nat. Electron. 2018, 1, 160–171. [Google Scholar] [CrossRef]
- Yang, T.; Xie, D.; Li, Z.; Zhu, H. Recent advances in wearable tactile sensors: Materials, sensing mechanisms, and device performance. Mater. Sci. Eng. R Rep. 2017, 115, 1–37. [Google Scholar] [CrossRef]
- Wang, B.; Facchetti, A. Mechanically Flexible Conductors for Stretchable and Wearable E-Skin and E-Textile Devices. Adv. Mater. 2019, 31, e19014082019. [Google Scholar] [CrossRef] [PubMed]
- Kralikova, I.; Babusiak, B.; Labuda, M. Textile Electrodes for Bioelectrical Signal Measurement. In Proceedings of the 2022 ELEKTRO (ELEKTRO), Krakow, Poland, 23–26 May 2022; pp. 1–5. [Google Scholar]
- Ibrahim, N.F.A.; Sabani, N.; Johari, S.; Manaf, A.A.; Wahab, A.A.; Zakaria, Z.; Noor, A.M. A Comprehensive Review of the Recent Developments in Wearable Sweat-Sensing Devices. Sensors 2022, 22, 7670. [Google Scholar] [CrossRef]
- Liu, Y.; Li, X.; Yang, H.; Zhang, P.; Wang, P.; Sun, Y.; Yang, F.; Liu, W.; Li, Y.; Tian, Y.; et al. Skin-Interfaced Superhydrophobic Insensible Sweat Sensors for Evaluating Body Thermoregulation and Skin Barrier Functions. ACS Nano 2023, 17, 5588–5599. [Google Scholar] [CrossRef]
- Napier, B.S.; Matzeu, G.; Presti, M.L.; Omenetto, F.G. Dry Spun, Bulk-Functionalized rGO Fibers for Textile Integrated Potentiometric Sensors. Adv. Mater. Technol. 2022, 7, 2101508. [Google Scholar] [CrossRef]
- Ma, H.; Li, J.; Zhou, J.; Luo, Q.; Wu, W.; Mao, Z.; Ma, W. Screen-Printed Carbon Black/Recycled Sericin@Fabrics for Wearable Sensors to Monitor Sweat Loss. ACS Appl. Mater. Interfaces 2022, 14, 11813–11819. [Google Scholar] [CrossRef] [PubMed]
- Kalasin, S.; Sangnuang, P.; Surareungchai, W. Satellite-Based Sensor for Environmental Heat-Stress Sweat Creatinine Monitoring: The Remote Artificial Intelligence-Assisted Epidermal Wearable Sensing for Health Evaluation. ACS Biomater. Sci. Eng. 2020, 7, 322–334. [Google Scholar] [CrossRef] [PubMed]
- Choudhry, N.A.; Arnold, L.; Rasheed, A.; Khan, I.A.; Wang, L. Textronics—A review of textile-based wearable electronics. Adv. Eng. Mater. 2021, 23, 2100469. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhang, T.; Huang, Z.; Yang, J. A New Class of Electronic Devices Based on Flexible Porous Substrates. Adv. Sci. 2022, 9, 2105084. [Google Scholar] [CrossRef]
- Ma, C.; Wang, M.; Uzabakiriho, P.C.; Zhao, G. High sensitivity, broad working range, comfortable, and biofriendly wearable strain sensor for electronic skin. Adv. Mater. Technol. 2022, 7, 2200106. [Google Scholar] [CrossRef]
- Fu, Q.; Cui, C.; Meng, L.; Hao, S.; Dai, R.; Yang, J. Emerging cellulose-derived materials: A promising platform for the design of flexible wearable sensors toward health and environment monitoring. Mater. Chem. Front. 2020, 5, 2051–2091. [Google Scholar] [CrossRef]
- Prakash, N.J.; Mane, P.P.; George, S.M.; Kandasubramanian, B. Silk fibroin as an immobilization matrix for sensing applications. ACS Biomater. Sci. Eng. 2021, 7, 2015–2042. [Google Scholar] [CrossRef] [PubMed]
- Ha, J.H.; Jeong, Y.; Ahn, J.; Hwang, S.; Jeon, S.; Kim, D.; Ko, J.; Kang, B.; Jung, Y.; Choi, J.; et al. A wearable colorimetric sweat pH sensor-based smart textile for health state diagnosis. Mater. Horiz. 2023, 10, 4163–4171. [Google Scholar] [CrossRef]
- Li, L.; Li, D.; Sun, B.; Zhou, Y.; Ma, J.; Chen, S.; Jiang, L.; Zhou, F.-L. Styrene-ethylene-butadiene-styrene copolymer/carbon nanotubes composite fiber based strain sensor with wide sensing range and high linearity for human motion detection. J. Ind. Text. 2022, 52, 15280837221121972. [Google Scholar] [CrossRef]
- Ma, X.; Wang, P.; Huang, L.; Ding, R.; Zhou, K.; Shi, Y.; Chen, F.; Zhuang, Q.; Huang, Q.; Lin, Y.; et al. A monolithically integrated in-textile wristband for wireless epidermal biosensing. Sci. Adv. 2023, 9, eadj2763. [Google Scholar] [CrossRef] [PubMed]
- Xu, Z.; Song, J.; Liu, B.; Lv, S.; Gao, F.; Luo, X.; Wang, P. A conducting polymer PEDOT:PSS hydrogel based wearable sensor for accurate uric acid detection in human sweat. Sens. Actuators B Chem. 2021, 348, 130674. [Google Scholar] [CrossRef]
- Mazzara, F.; Patella, B.; D’agostino, C.; Bruno, M.G.; Carbone, S.; Lopresti, F.; Aiello, G.; Torino, C.; Vilasi, A.; O’riordan, A.; et al. PANI-Based Wearable Electrochemical Sensor for pH Sweat Monitoring. Chemosensors 2021, 9, 169. [Google Scholar] [CrossRef]
- Madhu, S.; Anthuuvan, A.J.; Ramasamy, S.; Manickam, P.; Bhansali, S.; Nagamony, P.; Chinnuswamy, V. ZnO Nanorod Integrated Flexible Carbon Fibers for Sweat Cortisol Detection. ACS Appl. Electron. Mater. 2020, 2, 499–509. [Google Scholar] [CrossRef]
- Nekoueian, K.; Amiri, M.; Sillanpää, M.; Marken, F.; Boukherroub, R.; Szunerits, S. Car-bon-based quantum particles: An electroanalytical and biomedical perspective. Chem. Soc. Rev. 2019, 48, 4281–4316. [Google Scholar] [CrossRef] [PubMed]
- Yao, S.; Yang, J.; Poblete, F.R.; Hu, X.; Zhu, Y. Multifunctional Electronic Textiles Using Silver Nanowire Composites. ACS Appl. Mater. Interfaces 2019, 11, 31028–31037. [Google Scholar] [CrossRef]
- Liu, Y.-L.; Liu, R.; Qin, Y.; Qiu, Q.-F.; Chen, Z.; Cheng, S.-B.; Huang, W.-H. Flexible Electrochemical Urea Sensor Based on Surface Molecularly Imprinted Nanotubes for Detection of Human Sweat. Anal. Chem. 2018, 90, 13081–13087. [Google Scholar] [CrossRef] [PubMed]
- Lim, H.; Kim, H.S.; Qazi, R.; Kwon, Y.; Jeong, J.; Yeo, W. Advanced soft materials, sensor integrations, and applications of wearable flexible hybrid electronics in healthcare, energy, and environment. Adv. Mater. 2020, 32, 1901924. [Google Scholar] [CrossRef] [PubMed]
- Raza, T.; Qu, L.; Khokhar, W.A.; Andrews, B.; Ali, A.; Tian, M. Progress of Wearable and Flexible Electrochemical Biosensors With the Aid of Conductive Nanomaterials. Front. Bioeng. Biotechnol. 2021, 9, 761020. [Google Scholar] [CrossRef]
- Mansuriya, B.D.; Altintas, Z. Applications of graphene quantum dots in biomedical sensors. Sensors 2020, 20, 1072. [Google Scholar] [CrossRef]
- Dastjerdi, R.; Montazer, M. A review on the application of inorganic nano-structured materials in the modification of textiles: Focus on anti-microbial properties. Colloids Surf. B Biointerfaces 2010, 79, 5–18. [Google Scholar] [CrossRef] [PubMed]
- Chen, G.; Xiao, X.; Zhao, X.; Tat, T.; Bick, M.; Chen, J. Electronic Textiles for Wearable Point-of-Care Systems. Chem. Rev. 2021, 122, 3259–3291. [Google Scholar] [CrossRef] [PubMed]
- Al Mamun, M.A.; Yuce, M.R. Recent progress in nanomaterial enabled chemical sensors for wearable environmental monitoring applications. Adv. Funct. Mater. 2020, 30, 2005703. [Google Scholar] [CrossRef]
- Ke, Y.; Zhang, J.; Peng, X.; Zhang, Z.; Wang, X.; Qi, W.; Wang, M. A facile strategy to construct MOF-based nanocatalyst with enhanced activity and selectivity in oxytetracycline degradation. Nano Res. 2024, 17, 5863–5871. [Google Scholar] [CrossRef]
- Yao, S.; Ren, P.; Song, R.; Liu, Y.; Huang, Q.; Dong, J.; O’Connor, B.T.; Zhu, Y. Nanomaterial-enabled flexible and stretchable sensing systems: Processing, integration, and applications. Adv. Mater. 2020, 32, 1902343. [Google Scholar] [CrossRef] [PubMed]
- Shah, M.A.; Pirzada, B.M.; Price, G.; Shibiru, A.L.; Qurashi, A. Applications of nanotechnology in smart textile industry: A critical review. J. Adv. Res. 2022, 38, 55–75. [Google Scholar] [CrossRef] [PubMed]
- Greyling, C.F.; Ganguly, A.; Sardesai, A.U.; Churcher, N.K.; Lin, K.C.; Muthukumar, S.; Prasad, S. Passive sweat wearable: A new paradigm in the wearable landscape to-ward enabling ‘detect to treat’ opportunities. Wiley Interdiscip Rev. Nanomed. Nanobiotechnol. 2024, 16, e19122024. [Google Scholar] [CrossRef] [PubMed]
- Ho, H.; Kuvaas, B. Human resource management systems, employee well-being, and firm performance from the mutual gains and critical perspectives: The well-being paradox. Hum. Resour. Manag. 2020, 59, 235–253. [Google Scholar] [CrossRef]
- Seshadri, D.R.; Li, R.T.; Voos, J.E.; Rowbottom, J.R.; Alfes, C.M.; Zorman, C.A.; Drummond, C.K. Wearable sensors for monitoring the physiological and biochemical pro-file of the athlete. NPJ Digit. Med. 2019, 2, 72. [Google Scholar] [CrossRef]
- Yang, G.; Pang, G.; Pang, Z.; Gu, Y.; Mantysalo, M.; Yang, H. Non-Invasive Flexible and Stretchable Wearable Sensors with Nano-Based Enhancement for Chronic Disease Care. IEEE Rev. Biomed. Eng. 2018, 12, 34–71. [Google Scholar] [CrossRef]
- Bandodkar, A.J.; Jeang, W.J.; Ghaffari, R.; Rogers, J.A. Wearable Sensors for Biochemical Sweat Analysis. Annu. Rev. Anal. Chem. 2019, 12, 1–22. [Google Scholar] [CrossRef]
- Gualandi, I.; Tessarolo, M.; Mariani, F.; Possanzini, L.; Scavetta, E.; Fraboni, B. Textile Chemical Sensors Based on Conductive Polymers for the Analysis of Sweat. Polymers 2021, 13, 894. [Google Scholar] [CrossRef] [PubMed]
- Kazanskiy, N.L.; Khonina, S.N.; Butt, M.A. A review on flexible wearables-Recent developments in non-invasive continuous health monitoring. Sens. Actuators A Phys. 2024, 366, 114993. [Google Scholar] [CrossRef]
- Sun, W.; Guo, Z.; Yang, Z.; Wu, Y.; Lan, W.; Liao, Y.; Wu, X.; Liu, Y. A Review of Recent Advances in Vital Signals Monitoring of Sports and Health via Flexible Wearable Sensors. Sensors 2022, 22, 7784. [Google Scholar] [CrossRef] [PubMed]
- Wazwaz, A.; Amin, K.; Semary, N.; Ghanem, T. Dynamic and Distributed Intelligence over Smart Devices, Internet of Things Edges, and Cloud Computing for Human Activity Recognition Using Wearable Sensors. J. Sens. Actuator Netw. 2024, 13, 5. [Google Scholar] [CrossRef]
- Leape, C.; Fong, A.; Ratwani, R.M. Heuristic Usability Evaluation of Wearable Mental State Monitoring Sensors for Healthcare Environments. Proc. Hum. Factors Ergon. Soc. Annu. Meet. 2016, 60, 583–587. [Google Scholar] [CrossRef]
- Mohr, D.C.; Zhang, M.; Schueller, S.M. Personal Sensing: Understanding Mental Health Using Ubiquitous Sensors and Machine Learning. Annu. Rev. Clin. Psychol. 2017, 13, 23–47. [Google Scholar] [CrossRef] [PubMed]
- Roy, R.N.; Charbonnier, S.; Campagne, A.; Bonnet, S. Efficient mental workload estimation using task-independent EEG features. J. Neural Eng. 2016, 13, 026019. [Google Scholar] [CrossRef] [PubMed]
- Zhang, D.; Cao, D.; Chen, H. Deep learning decoding of mental state in non-invasive brain computer interface. In Proceedings of the International Conference on Artificial Intelligence, Information Processing and Cloud Computing, Sanya, China, 19 December 2019; pp. 1–5. [Google Scholar]
- Nyein, H.Y.; Bariya, M.; Kivimäki, L.; Uusitalo, S.; Liaw, T.S.; Jansson, E.; Ahn, C.H.; Hangasky, J.A.; Zhao, J.; Lin, Y.; et al. Regional and correlative sweat analysis using high-throughput micro-fluidic sensing patches toward decoding sweat. Sci. Adv. 2019, 5, eaaw9906. [Google Scholar] [CrossRef]
- Torous, J.; Chan, S.R.; Tan, S.Y.; Behrens, J.; Mathew, I.; Conrad, E.J.; Hinton, L.; Yellowlees, P.; Keshavan, M. Patient smartphone ownership and interest in mobile apps to monitor symptoms of mental health conditions: A survey in four geographically distinct psychiatric clinics. JMIR Ment. Health 2014, 1, e40042014. [Google Scholar] [CrossRef]
- Lopes, L.; Rodrigues, A.; Cabral, D.; Campos, P. From Monitoring to Assisting: A Systematic Review towards Healthier Workplaces. Int. J. Environ. Res. Public Health 2022, 19, 16197. [Google Scholar] [CrossRef] [PubMed]
- Meng, K.; Zhao, S.; Zhou, Y.; Wu, Y.; Zhang, S.; He, Q.; Wang, X.; Zhou, Z.; Fan, W.; Tan, X.; et al. A Wireless Textile-Based Sensor System for Self-Powered Personalized Health Care. Matter 2020, 2, 896–907. [Google Scholar] [CrossRef]
- Lipovka, A.; Fatkullin, M.; Shchadenko, S.; Petrov, I.; Chernova, A.; Plotnikov, E.; Menzelintsev, V.; Li, S.; Qiu, L.; Cheng, C.; et al. Textile Electronics with Laser-Induced Graphene/Polymer Hybrid Fibers. ACS Appl. Mater. Interfaces 2023, 15, 38946–38955. [Google Scholar] [CrossRef]
- Kulkarni, M.B.; Rajagopal, S.; Prieto-Simón, B.; Pogue, B.W. Recent advances in smart wearable sensors for continuous human health monitoring. Talanta 2024, 272, 125817. [Google Scholar] [CrossRef]
- Bhide, A.; Ganguly, A.; Parupudi, T.; Ramasamy, M.; Muthukumar, S.; Prasad, S. Next-Generation Continuous Metabolite Sensing toward Emerging Sensor Needs. ACS Omega 2021, 6, 6031–6040. [Google Scholar] [CrossRef] [PubMed]
- Kumari, Y.; Bai, P.; Waqar, F.; Asif, A.T.; Irshad, B.; Raj, S.; Varagantiwar, V.; Kumar, M.; Neha, F.N.; Chand, S.; et al. Advancements in the management of endocrine system disorders and arrhythmias: A comprehensive narrative review. Cureus 2023, 15, e46484. [Google Scholar] [CrossRef]
- Gai, K.; Lu, Z.; Qiu, M.; Zhu, L. Toward Smart Treatment Management for Personalized Healthcare. IEEE Netw. 2019, 33, 30–36. [Google Scholar] [CrossRef]
- Hsueh, P.-Y.S.; Chang, H.; Ramakrishnan, S. Next generation wellness: A technology model for personalizing healthcare. Healthc. Inf. Manag. Syst. Cases Strateg. Solut. 2016, 355–374. [Google Scholar]
- Sachdeva, P.; Kaur, K.; Fatima, S.; Mahak, F.N.; Noman, M.; Siddenthi, S.M.; Surksha, M.A.; Munir, M.; Fatima, F.N.; Sultana, S.S.; et al. Advancements in myocardial infarction management: Exploring novel approaches and strategies. Cureus 2023, 15, e45578. [Google Scholar] [CrossRef]
- Sugandh, F.N.; Chandio, M.; Raveena, F.N.; Kumar, L.; Karishma, F.N.; Khuwaja, S.; Memon, U.A.; Bai, K.; Kashif, M.; Varrassi, G.; et al. Advances in the management of diabetes mellitus: A focus on personalized medicine. Cureus 2023, 15, e43697. [Google Scholar] [CrossRef]
- Manjakkal, L.; Yin, L.; Nathan, A.; Wang, J.; Dahiya, R. Energy autonomous sweat-based wearable systems. Adv. Mater. 2021, 33, 2100899. [Google Scholar] [CrossRef] [PubMed]
- Nozariasbmarz, A.; Collins, H.; Dsouza, K.; Polash, M.H.; Hosseini, M.; Hyland, M.; Liu, J.; Malhotra, A.; Ortiz, F.M.; Mohaddes, F.; et al. Review of wearable thermoelectric energy harvesting: From body temperature to electronic systems. Appl. Energy 2019, 258, 114069. [Google Scholar] [CrossRef]
- Zou, Y.; Raveendran, V.; Chen, J. Wearable triboelectric nanogenerators for biomechanical energy harvesting. Nano Energy 2020, 77, 105303. [Google Scholar] [CrossRef]
- Dong, K.; Deng, J.; Zi, Y.; Wang, Y.; Xu, C.; Zou, H.; Ding, W.; Dai, Y.; Gu, B.; Sun, B.; et al. 3D Orthogonal Woven Triboelectric Nanogenerator for Effective Biomechanical Energy Harvesting and as Self-Powered Active Motion Sensors. Adv. Mater. 2017, 29, 1702648. [Google Scholar] [CrossRef]
- Yin, L.; Kim, K.N.; Lv, J.; Tehrani, F.; Lin, M.; Lin, Z.; Moon, J.-M.; Ma, J.; Yu, J.; Xu, S.; et al. A self-sustainable wearable multi-modular E-textile bioenergy microgrid system. Nat. Commun. 2021, 12, 1542. [Google Scholar] [CrossRef] [PubMed]
- Dong, K.; Wang, Z.L. Self-charging power textiles integrating energy harvesting triboe-lectric nanogenerators with energy storage batteries/supercapacitors. J. Semicond. 2021, 42, 101601. [Google Scholar] [CrossRef]
- Yin, L. Energy Autonomous Microgrids for Wearable Sensors and Fully Integrated Wearable Systems; University of California: San Diego, CA, USA, 2022. [Google Scholar]
- Yin, L.; Kim, K.N.; Trifonov, A.; Podhajny, T.; Wang, J. Designing wearable microgrids: To-wards autonomous sustainable on-body energy management. Energy Environ. Sci. 2022, 15, 82–101. [Google Scholar] [CrossRef]
- Ali, M.I.; Karim, N.; Afroj, S. 2D Material-Based Wearable Energy Harvesting Textiles: A Review. Small Struct 2024, 5, 2300282. [Google Scholar] [CrossRef]
- Dong, K.; Peng, X.; Cheng, R.; Ning, C.; Jiang, Y.; Zhang, Y.; Wang, Z.L. Advances in High-Performance Autonomous Energy and Self-Powered Sensing Textiles with Novel 3D Fabric Structures. Adv. Mater. 2022, 34, 2109355. [Google Scholar] [CrossRef]
- Gong, M.; Zhang, L.; Wan, P. Polymer nanocomposite meshes for flexible electronic devices. Prog. Polym. Sci 2020, 107, 101279. [Google Scholar] [CrossRef]
- Cheng, R.; Dong, K.; Liu, L.; Ning, C.; Chen, P.; Peng, X.; Liu, D.; Wang, Z.L. Flame-Retardant Textile-Based Triboelectric Nanogenerators for Fire Protection Applications. ACS Nano 2020, 14, 15853–15863. [Google Scholar] [CrossRef] [PubMed]
- Iyer, S.V.; George, J.; Sathiyamoorthy, S.; Palanisamy, R.; Majumdar, A.; Veluswamy, P. Pertinence of textile-based energy harvesting system for biomedical applications. J. Nanomater. 2022, 2022, 7921479. [Google Scholar] [CrossRef]
- Luo, Z.; Wang, Y.; Kou, B.; Liu, C.; Zhang, W.; Chen, L. ‘Sweat-chargeable’ on-skin supercapacitors for practical wearable energy applications. Energy Storage Mater. 2021, 38, 9–16. [Google Scholar] [CrossRef]
- Gao, Y.; Rezaie, M.; Choi, S. A wearable, disposable paper-based self-charging power system integrating sweat-driven microbial energy harvesting and energy storage devices. Nano Energy 2022, 104, 107923. [Google Scholar] [CrossRef]
- Trung, T.Q.; Lee, N. Flexible and Stretchable Physical Sensor Integrated Platforms for Wearable Human-Activity Monitoringand Personal Healthcare. Adv. Mater. 2016, 28, 4338–4372. [Google Scholar] [CrossRef] [PubMed]
- Persson, N.; Martinez, J.G.; Zhong, Y.; Maziz, A.; Jager, E.W.H. Actuating Textiles: Next Generation of Smart Textiles. Adv. Mater. Technol. 2018, 3, 1700397. [Google Scholar] [CrossRef]
- Júnior, H.L.O.; Neves, R.M.; Monticeli, F.M.; Agnol, L.D. Smart Fabric Textiles: Recent Advances and Challenges. Textiles 2022, 2, 582–605. [Google Scholar] [CrossRef]
- Luo, Y.; Abidian, M.R.; Ahn, J.-H.; Akinwande, D.; Andrews, A.M.; Antonietti, M.; Bao, Z.; Berggren, M.; Berkey, C.A.; Bettinger, C.J.; et al. Technology Roadmap for Flexible Sensors. ACS Nano 2023, 17, 5211–5295. [Google Scholar] [CrossRef] [PubMed]
- Gungor, V.C.; Hancke, G.P. Industrial wireless sensor networks: Challenges, design principles, and technical approaches. IEEE Trans. Ind. Electron. 2009, 56, 4258–4265. [Google Scholar] [CrossRef]
- Wang, L.; Fu, X.; He, J.; Shi, X.; Chen, T.; Chen, P.; Wang, B.; Peng, H. Application Challenges in Fiber and Textile Electronics. Adv. Mater. 2019, 32, e19019712019. [Google Scholar] [CrossRef]
- Gao, W.; Emaminejad, S.; Nyein, H.Y.Y.; Challa, S.; Chen, K.; Peck, A.; Fahad, H.M.; Ota, H.; Shiraki, H.; Kiriya, D.; et al. Fully integrated wearable sensor arrays for multiplexed in situ perspiration analysis. Nature 2016, 529, 509–514. [Google Scholar] [CrossRef] [PubMed]
- Tabor, J.A. Textile-Based Soft Sensors for Prosthetic Environment Monitoring; North Carolina State University: Raleigh, NC, USA, 2021. [Google Scholar]
- Xue, E.; Liu, L.; Wu, W.; Wang, B. Soft Fiber/Textile Actuators: From Design Strategies to Diverse Applications. ACS Nano 2023, 18, 89–118. [Google Scholar] [CrossRef] [PubMed]
- Yeung, K.K.; Huang, T.; Hua, Y.; Zhang, K.; Yuen, M.M.F.; Gao, Z. Recent advances in electrochemical sensors for wearable sweat monitoring: A review. IEEE Sens. J. 2021, 21, 14522–14539. [Google Scholar] [CrossRef]
- Andreu-Perez, J.; Leff, D.R.; Ip, H.M.D.; Yang, G.-Z. From wearable sensors to smart im-plants-toward pervasive and personalized healthcare. IEEE Trans. Biomed. Eng. 2015, 62, 2750–2762. [Google Scholar] [CrossRef] [PubMed]
- Ali, I.; Asif, M.; Shehzad, K.; Rehman, M.R.; Kim, D.G.; Rikan, B.S.; Pu, Y.; Yoo, S.S.; Lee, K.Y. A highly accurate, polynomial-based digital temperature compensation for pie-zoresistive pressure sensor in 180 nm CMOS technology. Sensors 2020, 20, 5256. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Chiang, L. Monitoring Chemical Processes Using Judicious Fusion of Multi-Rate Sensor Data. Sensors 2019, 19, 2240. [Google Scholar] [CrossRef] [PubMed]
- Saha, A.; Sedaghat, S.; Gopalakrishnan, S.; Waimin, J.; Yermembetova, A.; Glassmaker, N.; Mousoulis, C.; Shakouri, A.; Wei, A.; Rahimi, R.; et al. A new paradigm of reliable sensing with field-deployed electrochemical sensors integrating data redundancy and source credibility. Sci. Rep. 2023, 13, 3101. [Google Scholar] [CrossRef] [PubMed]
- Clifford, A.; Das, J.; Yousefi, H.; Mahmud, A.; Chen, J.B.; Kelley, S.O. Strategies for bio-molecular analysis and continuous physiological monitoring. J. Am. Chem. Soc. 2021, 143, 5281–5294. [Google Scholar] [CrossRef] [PubMed]
- Nezakati, T.; Seifalian, A.; Tan, A.; Seifalian, A.M. Conductive polymers: Opportunities and challenges in biomedical applications. Chem. Rev. 2018, 118, 6766–6843. [Google Scholar] [CrossRef]
- Xu, J.; Zhang, Z.; Gan, S.; Gao, H.; Kong, H.; Song, Z.; Ge, X.; Bao, Y.; Niu, L. Highly stretchable fiber-based potentiometric ion sensors for multichannel re-al-time analysis of human sweat. ACS Sens. 2020, 5, 2834–2842. [Google Scholar] [CrossRef]
- Kim, S.; Park, S.; Choi, J.; Hwang, W.; Kim, S.; Choi, I.S.; Yi, H.; Kwak, R. An epifluidic electronic patch with spiking sweat clearance for event-driven perspiration monitoring. Nat. Commun. 2022, 13, 6705. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Li, M.; Fan, Q.; Qi, X.; Qu, L.; Tian, M. Smart-Fabric-Based Supercapacitor with Long-Term Durability and Waterproof Properties toward Wearable Applications. ACS Appl. Mater. Interfaces 2021, 13, 14778–14785. [Google Scholar] [CrossRef] [PubMed]
- Xu, R.; She, M.; Liu, J.; Zhao, S.; Liu, H.; Qu, L.; Tian, M. Breathable Kirigami-Shaped Ionotronic e-Textile with Touch/Strain Sensing for Friendly Epidermal Electronics. Adv. Fiber Mater. 2022, 4, 1525–1534. [Google Scholar] [CrossRef]
- Ju, J.; Xiao, G.; Jian, Y.; Wu, L.; Sun, W.; Wang, W.; Li, C.M.; Qiao, Y.; Lu, Z. Scalable, high-performance, yarn-shaped batteries activated by an ultralow volume of sweat for self-powered sensing textiles. Nano Energy 2023, 109, 108304. [Google Scholar] [CrossRef]
- Zhao, Z.; Li, Q.; Dong, Y.; Gong, J.; Li, Z.; Zhang, J. Washable Patches with Gold Nanowires/Textiles in Wearable Sensors for Health Monitoring. ACS Appl. Mater. Interfaces 2022, 14, 18884–18900. [Google Scholar] [CrossRef] [PubMed]
- Teyeme, Y.; Malengier, B.; Tesfaye, T.; Van Langenhove, L. A Fabric-Based Textile Stretch Sensor for Optimized Measurement of Strain in Clothing. Sensors 2020, 20, 7323. [Google Scholar] [CrossRef] [PubMed]
- Li, M.; Li, Z.; Ye, X.; Zhang, X.; Qu, L.; Tian, M. Tendril-Inspired 900% Ultrastretching Fiber-Based Zn-Ion Batteries for Wearable Energy Textiles. ACS Appl. Mater. Interfaces 2021, 13, 17110–17117. [Google Scholar] [CrossRef] [PubMed]
- Kil, M.S.; Kim, S.J.; Park, H.J.; Yoon, J.H.; Jeong, J.-M.; Choi, B.G. Highly Stretchable Sensor Based on Fluid Dynamics-Assisted Graphene Inks for Real-Time Monitoring of Sweat. ACS Appl. Mater. Interfaces 2022, 14, 48072–48080. [Google Scholar] [CrossRef]
- Zhang, K.; Zhang, J.; Wang, F.; Kong, D. Stretchable and Superwettable Colorimetric Sensing Patch for Epidermal Collection and Analysis of Sweat. ACS Sens. 2021, 6, 2261–2269. [Google Scholar] [CrossRef]
- Li, M.; Li, Z.; Qu, L.; Chen, F.; Tian, M. Recent Progress of the Active Materials with Various Micro-structures for Flexible Textile-Based Supercapacitors. Adv. Fiber Mater. 2022, 4, 1005–1026. [Google Scholar] [CrossRef]
- Wang, Z.; Shin, J.; Park, J.; Lee, H.; Kim, D.; Liu, H. Engineering materials for electrochemical sweat sensing. Adv. Funct. Mater. 2021, 31, 2008130. [Google Scholar] [CrossRef]
- Van Tran, V.; Lee, S.; Lee, D.; Le, T.-H. Recent developments and implementations of con-ductive polymer-based flexible devices in sensing applications. Polymers 2022, 14, 3730. [Google Scholar] [CrossRef] [PubMed]
- Baima, M.; Andrew, T.L. Fluoropolymer-Wrapped Conductive Threads for Textile Touch Sensors Operating via the Triboelectric Effect. Fibers 2018, 6, 41. [Google Scholar] [CrossRef]
- Mishra, N.; Garland, N.T.; Hewett, K.A.; Shamsi, M.; Dickey, M.D.; Bandodkar, A.J. A Soft Wearable Microfluidic Patch with Finger-Actuated Pumps and Valves for On-Demand, Lon-gitudinal, and Multianalyte Sweat Sensing. ACS Sens. 2022, 7, 3169–3180. [Google Scholar] [CrossRef] [PubMed]
- Srite, M.; Karahanna, E. The role of espoused national cultural values in technology acceptance. MIS Q. 2006, 679–704. [Google Scholar] [CrossRef]
- Baum, C.M.; Gross, C. Sustainability policy as if people mattered: Developing a frame-work for environmentally significant behavioral change. J. Bioecon. 2017, 19, 53–95. [Google Scholar] [CrossRef]
- Gay, G. Culturally Responsive Teaching: Theory, Research, and Practice; Teachers College Press: New York, NY, USA, 2018. [Google Scholar]
- Leidner, D.E.; Kayworth, T. A Review of Culture in Information Systems Research: Toward a Theory of Information Technology Culture Conflict. MIS Q. 2006, 30, 357. [Google Scholar] [CrossRef]
- Acikgoz, F.; Elwalda, A.; De Oliveira, M.J. Curiosity on Cutting-Edge Technology via Theory of Planned Behavior and Diffusion of Innovation Theory. Int. J. Inf. Manag. Data Insights 2023, 3, 100152. [Google Scholar] [CrossRef]
- Kavga, A.; Thomopoulos, V.; Barouchas, P.; Stefanakis, N.; Liopa-Tsakalidi, A. Research on innovative training on smart greenhouse technologies for economic and environmental sustainability. Sustainability 2021, 13, 10536. [Google Scholar] [CrossRef]
- Hossain, M.T.; Shahid, M.A.; Limon, M.G.M.; Hossain, I.; Mahmud, N. Techniques, applications, and challenges in textiles for sustainable future. J. Open Innov. Technol. Mark. Complexit 2024, 54, 100230. [Google Scholar] [CrossRef]
- Chan, M.; Estève, D.; Fourniols, J.-Y.; Escriba, C.; Campo, E. Smart wearable systems: Cur-rent status and future challenges. Artif. Intell. Med. 2012, 56, 137–156. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, R.; Yang, D.S.; Kim, J.; Mansour, A.; Wright Jr, J.A.; Model, J.B.; Wright, D.E.; Rogers, J.A.; Ray, T.R. State of sweat: Emerging wearable systems for real-time, noninvasive sweat sensing and analytics. ACS Sens. 2021, 6, 2787–2801. [Google Scholar] [CrossRef] [PubMed]
- Khan, S.; Ali, S.; Bermak, A. Recent developments in printing flexible and wearable sensing electronics for healthcare applications. Sensors 2019, 19, 1230. [Google Scholar] [CrossRef]
- Wang, H.; Li, S.; Lu, H.; Zhu, M.; Liang, H.; Wu, X.; Zhang, Y. Carbon-Based Flexible Devices for Comprehensive Health Monitoring. Small Methods 2023, 7, 2201340. [Google Scholar] [CrossRef]
- Luo, J.; Gao, S.; Luo, H.; Wang, L.; Huang, X.; Guo, Z.; Lai, X.; Lin, L.; Li, R.K.Y.; Gao, J. Superhydrophobic and breathable smart MXene-based textile for multifunctional wearable sensing electronics. Chem. Eng. J. 2021, 406, 126898. [Google Scholar] [CrossRef]
- Muneeswari, G.; Varun, S.S.; Hegde, R.; Priya, S.S.; Shermila, P.J.; Prasanth, A. Self-diagnosis platform via IOT-based privacy preserving medical data. Meas. Sens. 2023, 25, 100636. [Google Scholar] [CrossRef]
- Wang, H.; Li, K.; Ota, K.; Shen, J. Remote Data Integrity Checking and Sharing in Cloud-Based Health Internet of Things. IEICE Trans. Inf. Syst. 2016, 99, 1966–1973. [Google Scholar] [CrossRef]
- Yeh, L.-Y.; Chiang, P.-Y.; Tsai, Y.-L.; Huang, J.-L. Cloud-based fine-grained health information access control framework for lightweightiot devices with dynamic auditing andattribute revocation. IEEE Trans. Cloud Comput. 2015, 6, 532–544. [Google Scholar] [CrossRef]
- Liman, M.L.R.; Islam, M.T.; Hossain, M.M. Mapping the progress in flexible electrodes for wearable electronic textiles: Materials, durability, and applications. Adv. Electron. Mater. 2022, 8, 2100578. [Google Scholar] [CrossRef]
- Yu, R.; Zhu, C.; Wan, J.; Li, Y.; Hong, X. Review of graphene-based textile strain sensors, with emphasis on structure activity relationship. Polymers 2021, 13, 151. [Google Scholar] [CrossRef]
- Kong, M.; Yang, M.; Li, R.; Long, Y.Z.; Zhang, J.; Huang, X.; Cui, X.; Zhang, Y.; Said, Z.; Li, C. Graphene-based flexible wearable sensors: Mechanisms, challenges, and future directions. Int. J. Adv. Manuf. Technol. 2024, 131, 3205–3237. [Google Scholar] [CrossRef]
- Zhao, H.; Su, R.; Teng, L.; Tian, Q.; Han, F.; Li, H.; Cao, Z.; Xie, R.; Li, G.; Liu, X.; et al. Recent advances in flexible and wearable sensors for monitoring chemical molecules. Nanoscale 2021, 14, 1653–1669. [Google Scholar] [CrossRef] [PubMed]
- Garland, N.T.; Kaveti, R.; Bandodkar, A.J. Biofluid-Activated Biofuel Cells, Batteries, and Supercapacitors: A Comprehensive Review. Adv. Mater. 2023, 35, e23031972023. [Google Scholar] [CrossRef] [PubMed]
- Hansora, D.P.; Shimpi, N.G.; Mishra, S. Performance of hybrid nanostructured conduc-tive cotton materials as wearable devices: An overview of materials, fabrication, properties and applications. RSC Adv. 2015, 5, 107716–107770. [Google Scholar] [CrossRef]
- Teymourian, H.; Parrilla, M.; Sempionatto, J.R.; Montiel, N.F.; Barfidokht, A.; Van Echelpoel, R.; De Wael, K.; Wang, J. Wearable Electrochemical Sensors for the Monitoring and Screening of Drugs. ACS Sens. 2020, 5, 2679–2700. [Google Scholar] [CrossRef] [PubMed]
- Luo, D.; Sun, H.; Li, Q.; Niu, X.; He, Y.; Liu, H. Flexible Sweat Sensors: From Films to Textiles. ACS Sens. 2023, 8, 465–481. [Google Scholar] [CrossRef] [PubMed]
- Heikenfeld, J.; Jajack, A.; Rogers, J.; Gutruf, P.; Tian, L.; Pan, T.; Li, R.; Khine, M.; Kim, J.; Wang, J. Wearable sensors: Modalities, challenges, and prospects. Lab Chip 2018, 18, 217–248. [Google Scholar] [CrossRef]
- Chenani, H.; Saeidi, M.; Rastkhiz, M.A.; Bolghanabadi, N.; Aghaii, A.H.; Orouji, M.; Hatamie, A.; Simchi, A. Challenges and Advances of Hydrogel-Based Wearable Electrochemical Biosensors for Real-Time Monitoring of Biofluids: From Lab to Market. A Review. Anal Chem. 2024, 96, 8160–8183. [Google Scholar] [CrossRef] [PubMed]
- Heo, J.S.; Hossain, M.F.; Kim, I. Challenges in design and fabrication of flexi-ble/stretchable carbon-and textile-based wearable sensors for health monitoring: A critical review. Sensors 2020, 20, 3927. [Google Scholar] [CrossRef]
- El Gharbi, M.; Fernández-García, R.; Ahyoud, S.; Gil, I. A review of flexible wearable antenna sensors: Design, fabrication methods, and applications. Materials 2020, 13, 3781. [Google Scholar] [CrossRef]
- Sekar, M.; Sriramprabha, R.; Sekhar, P.K.; Bhansali, S.; Ponpandian, N.; Pandiaraj, M.; Viswanathan, C. Towards wearable sensor platforms for the electrochemical detection of cortisol. J. Electrochem. Soc. 2020, 167, 067508. [Google Scholar] [CrossRef]
- Hong, X.; Wu, H.; Wang, C.; Zhang, X.; Wei, C.; Xu, Z.; Chen, D.; Huang, X. Hybrid Janus Membrane with Dual-Asymmetry Integration of Wettability and Conductivity for Ultra-Low-Volume Sweat Sensing. ACS Appl. Mater. Interfaces 2022, 14, 9644–9654. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Gao, W. Wearable and flexible electronics for continuous molecular monitoring. Chem. Soc. Rev. 2019, 48, 1465–1491. [Google Scholar] [CrossRef]
- Coyle, S.; Lau, K.T.; Moyna, N.; O’Gorman, D.; Diamond, D.; Di Francesco, F.; Costanzo, D.; Salvo, P.; Trivella, M.G.; De Rossi, D.E.; et al. BIOTEX—Biosensing Textiles for Personalised Healthcare Management. IEEE Trans. Inf. Technol. Biomed. 2010, 14, 364–370. [Google Scholar] [CrossRef] [PubMed]


| Sweat Sensors | Type of the Sweat Sensor | Sensing Mechanisms | Key Features | Application | References |
|---|---|---|---|---|---|
| Non-invasive sweat sensor detection of sweat pH and lactate | Electrochemical sweat sensor | colorimetric sensing | Detects sweat pH and lactate simultaneously, uses cotton as a substrate | Diabetes management | [31] |
| Highly Stretchable and Strain-Insensitive sweat sensor | Electrochemical Biosensor | enzyme-based non-invasive sensing | Highly stretchy, strain-insensitive fiber, detects glucose, sensitivity of 11.7 μA mM−1 cm−2 | [32] | |
| Thermoresponsive sweat sensor | Optical sensor | colorimetric sensing | Shape memory polymer-modified fabric with a paper-based colorimetric sensor | [33] | |
| Noninvasive flexible sweat sensor | Ion-Selective Electrodes (ISEs) | multiplex sweat analysis | Uses SilkNCT as working electrodes, detects glucose, AA, lactate, UA, K+, and Na+ | [34] | |
| Non-invasive simultaneous sweat sensor | Optical sensor | colorimetric sensing | Non-invasive diagnosis of diabetes and renal failure, colorimetric approach | [35] | |
| In Vitro Diagnostics sweat sensor | Microwave sensors | resonance frequency shift of the reflection response of the antenna-based sensor | Textile-embroidered monopole antenna-based sensor, functions at 2.4 GHz | [36] | |
| Non-invasive sweat-based wearable sensor | Electrochemical Sensor | non-invasive cotton-based electrochemical sensing | Fabricated at room temperature, simple immersion method | [37] | |
| Screen-Printed Textile-Based Sweat sensor | Electrochemical Sensor | multiplexed sensing | Fully integrated enzymatic electrochemical sensor, high sensitivity and selectivity for glucose | [38] | |
| Cotton thread/paper-based microfluidic device for sweat glucose sensing | Microfluidic Sensors | non-invasive colorimetric sensing of glucose | Disposable, low-cost | [39] | |
| A sweat-based flexible supercapacitor (SC) | Electrochemical Sensor | chemiresistive sensing | Flexible, energy storage capabilities | Cardiovascular monitoring | [40] |
| Textile-Based Polyacrylate Imprinted sweat Sensor | Electrochemical Sensor | cortisol sensing | Wearable, stress monitoring | [41] | |
| Extremely Fast Self-Healable sweat sensor | Electrochemical Sensor | ion-selective electrode (ISE) mechanism | Self-healing capability, durable | [42] | |
| Integrated Smart Janus Textile sweat sensor | Noninvasive Electrochemical Sensor | multiple biomarkers including glucose, lactate, K+, and Na+ sensing | Self-pumping, multi-analyte sensing | [43] | |
| Conductive Thread-Based Textile sweat Sensor | Non-intrusive electrochemical sensor | sensing resistance between conductive threads, which changes according to the amount of sweat absorbed by the cotton braids between the threads | Sweat monitoring, low cost | Physical Activity Monitoring | [44] |
| Smart Textile Integrated Wireless sweat sensor | Electrochemical Sensor | sensing system with temperature and sweat sensors embedded into and powered by a smart textile NFC antenna | Battery-free, real-time monitoring | [45] | |
| Thread-based multiplexed sweat sensor patch | Electrochemical Selective potentiometric Sensor | ion-selective electrode (ISE) sensing | Real-time metabolic tracking | [46] | |
| Graphene-coated textile-based sweat sensor | Electrochemical Sensor developed with nanocomposites | sensing conductivity | Improved skin contact, washable | [47] | |
| A thread/fabric-based band as sweat sensor | Microfluidic sensor | epidermal sweat sensing and detection through a wearable microfluidic thread/fabric-based analytical device | Sweat collection, colorimetric analysis | [48] | |
| Highly Stretchable and Conductive Carbon Thread sweat sensor | Electrochemical Sensor | target biomarkers, sodium ion detecting electrochemical sensing | Stable, sodium ion detection | [49] | |
| A yarn/fabric-based microfluidic patch for sweat sensor | Microfluidic sensor | colorimetric analysis and quantitative analysis of sweat sensing | Flexible, real-time monitoring | [50] | |
| Wearable glucose sensor on cotton fabric for real-time monitoring | Electrochemical Sensor | electrochemical and pH sensing | Real-time glucose monitoring | [37] | |
| A thread-based wearable sweat nanobiosensor | Electrochemical Sensor | ion-selective sensing | High sensitivity, real-time monitoring | [51] | |
| Mediator-free carbon nanotube yarn for sweat sensing | Electrochemical Sensor | enzymatic biofuel cell for direct electron transfer | Energy harvesting, sustainable | Energy Harvesting | [52] |
| Wearable high-powered biofuel cells for sweat sensing | Electrochemical Sensor | a series connection by tying the enzyme fibers with batik-based ionic isolation to boost the net output voltage and power | High-power output | [53] | |
| Sweat-based wearable energy harvesting-storage sensor | Electrochemical Sensor | relies on lactate, which is oxidized enzymatically to generate electricity | Energy harvesting and storage | [54] | |
| Garment embedded sweat-activated batteries in wearable electronics | Electrochemical Sensor | garment-based microelectronics powered by sweat-activated batteries (SABs) and applications of powering biosensors and microelectronic systems for real time sweat monitoring | Continuous sweat monitoring | [55] | |
| Weavable yarn-shaped supercapacitor in sweat-activated self-charging sweat sensor | Electrochemical Sensor | pH-sensing system | Self-charging, wearable | [56] | |
| Stretchable biofuel cells as wearable textile-based self-powered sensors | Electrochemical Sensor | power output sensing | Stretchable, self-powered | [57] | |
| Wearable strain sweat sensor | Microfluidic Sensors | strain sensing by volume of sweat | Real-time monitoring | Physiological health conditions monitoring | [58] |
| Ion-selective textile organic sweat transistor | Electrochemical Sensor | ion-selective sensing | High selectivity, wearable | [59] | |
| Wearable Janus Textiles for Sweat sensor | Microfluidic Sensors | ion-selective sensing | Personalized diagnosis | Personalized diagnosis | [60] |
| Polyacrylate Imprinted Electrochemical Sensor for Cortisol detection | Electrochemical Sensor | conductivity sensing | Stress monitoring | [41] | |
| Sensor for Skin Hydration Monitoring | Electrochemical Sensor | impedance sensing | Skin hydration monitoring | Skin Hydration Monitoring | [61] |
| Highly Thermal-Wet Comfortable Sweat sensor | Electrochemical Sensor | conductivity and high water-vapor transmission rate sensing | Comfortable, high sweat tolerance | Electrocardiography signal monitoring | [62] |
| Microfluidic Platform for the Detection of Cytostatic Drug Concentration by sweat sensing | Microfluidic Sensor | conductivity sensing | Drug concentration monitoring | Drug concentration sensing | [63] |
| Sensor Type | Description | Key Technologies and Materials | Methodology | Applications and Advancements |
|---|---|---|---|---|
| Electrochemical Sensors | Highly innovative sensors providing non-invasive, real-time information about a person’s physiological state through the unique composition of sweat | - Conductive polymers | Utilize electrochemical reactions | Health monitoring [85] |
| - Flexible substrates | Incorporate flexible substrates, conductive polymers, and nanomaterials | Personalized medicine [86] | ||
| - Nanomaterials | Detect biomarkers in sweat (electrolytes, metabolites, specific ions) | Monitoring hydration levels and electrolyte balance in athletes [87] | ||
| Tracking glucose and lactate concentrations for diabetes and intense physical activities [88] | ||||
| Continuous health monitoring and personalized diagnostics [89] | ||||
| Biosensors | Provide important information about an individual’s performance and overall health by identifying different proteins and ions in sweat | - Conductive polymers | Employ diverse materials such as conductive polymers, enzymes, nanoparticles, and advanced nanomaterials | Non-invasive health monitoring [90] |
| - Enzymes | Real-time insights into health and performance [91] | |||
| - Nanoparticles | Detect biomolecules and ions in sweat | Applications in sports science, healthcare, and personalized medicine [92] | ||
| - Sophisticated nanomaterials | ||||
| Wearable integration enhances utility for continuous monitoring and early detection of health conditions [93] | ||||
| Optical Sensors | Employ cutting-edge technologies like nanotechnology and microfabrication to produce compact devices for non-invasive, real-time monitoring | - Functionalized substrates | Utilize light-based principles | Non-invasive monitoring capabilities [94] |
| - Nanomaterials | Employ microfabrication and nanotechnology | Applications in disease diagnosis, fitness monitoring, and personalized medicine [95] | ||
| - Biocompatible polymers | Detect and quantify changes in target parameters | Revolutionizing tracking and understanding of human health [96] | ||
| Microfluidic Sensors | Enable precise and controlled manipulation of small amounts of sweat using microfluidic channels, allowing for non-invasive, real-time monitoring of sweat biomarkers | - Biocompatible polymers | Utilize microfluidic channels | Non-invasive, real-time monitoring of biomarkers in sweat [97] |
| - State-of-the-art microfabrication techniques | Manipulate small volumes of sweat | Applications in fitness tracking, disease diagnosis, and performance optimization [98] | ||
| Use biocompatible polymers and advanced microfabrication techniques | Potential to revolutionize healthcare through continuous and convenient monitoring of relevant biomarkers in sweat [81] |
| Sensing Mechanism | Materials Used | Applications and Advantages |
|---|---|---|
| Ion-Selective Electrodes | Materials reactive to specific ions | Selective response to specific ions in sweat [106] |
| Non-invasive, continuous monitoring of ion concentrations [107] | ||
| Valuable insights into electrolyte balance [108] | ||
| Monitoring hydration levels [109] | ||
| Enzymatic Reactions | Enzymes immobilized on textile substrate | Catalysis of specific molecules in sweat [110] |
| Non-invasive, continuous monitoring of metabolites [111] | ||
| Provides insights into specific physiological processes [112] | ||
| Potential for personalized health monitoring [113] | ||
| Colorimetric/Fluorometric Changes | Chemical indicators reacting with sweat components | Induction of measurable changes in color or fluorescence [114] |
| Non-invasive, continuous monitoring of biomolecules [115] | ||
| Real-time insights into changes in sweat composition [116] | ||
| Versatile application in health and performance tracking [117] | ||
| Integration into Textile-based Sensors | Flexible substrates | Non-invasive monitoring of physiological parameters [29] |
| Conductive materials | Continuous tracking of health and performance [118] | |
| Materials reactive to target analytes | Wearable technology for convenience and ease of use [28] | |
| Real-time data for personalized health insights [119] |
| Material Type | Application | Characteristics |
|---|---|---|
| Natural Materials | Sweat collection and transport | Comfortable, breathable, flexible, unharmful, sustainable, e.g., cellulose, silk fibroin (SF), chitosan (CS) [13] |
| Flexible Substrates | Base substrate for sweat sensors | Compatible with human skin and perform well during daily activities, such as poly(styrene–ethylene–butadiene–styrene) (SEBS) and polyurethane (PU) [152] |
| Conventional Conductive Materials | Electrodes | High conductivity materials include carbon, metals (Au, Cu, Ag), metallic oxides (ZnO), poly(3,4-ethylenedioxythiophene) (PEDOT), and polyaniline (PANI) [153] |
| Microstructural Forms (QDs, NPs, NWs, NRs, NTs) | Electrodes | Larger specific surface area, improved sensitivity, e.g., carbon quantum dots (CQDs), graphene (Gr)-based materials, metal NRs [154] |
| Metallic Microstructural Materials (Au, Ag, ZnO, etc.) | Integration into textiles | High electrical conductivity and antibacterial properties, e.g., Au nanodendrites, ZnO nanorods [155] |
| Publication Year | Researchers | Sensor Type | Key Features | Applications | Reference |
|---|---|---|---|---|---|
| 2018 | Jia, Ji, et al. | Conductive thread | Sweat monitoring, low-cost | Activity monitoring, healthcare | [43] |
| 2019 | Jiang, Yutong, et al. | NFC-enabled textile | Battery-free, real-time monitoring | Systemic hyperthermia, wound healing | [44] |
| 2020 | Terse-Thakoor, Trupti, et al. | Thread-based multiplexed | Real-time metabolic tracking | Athletic assessment, clinical diagnosis | [45] |
| 2020 | Shathi, Mahmuda Akter, et al. | Graphene-coated bra | Improved skin contact, washable | Detecting arrhythmia | [46] |
| 2020 | Zhao, Zhiqi, et al. | Thread/fabric microfluidic | Sweat collection, colorimetric analysis | Point-of-care diagnostics | [47] |
| 2022 | Kim et al. | Stretchable carbon threads | Stable, sodium ion detection | Activity monitoring | [48] |
| 2023 | Yu, Wenze, et al. | Yarn/fabric microfluidic | Real-time sweat sensing | Cystic fibrosis, diabetes monitoring | [178] |
| Sensor Type | Sensitivity (Units) | Selectivity (%) | Response Time (s) | Accuracy (%) | Durability (Cycles) | Applications |
|---|---|---|---|---|---|---|
| Conductive Threads | High | Medium | Low | Medium | High | Physical activity monitoring, healthcare |
| NFC-enabled Textiles | Medium | High | Very Low | High | Medium | Systemic hyperthermia, wound healing |
| Thread-based Microfluidics | High | High | Medium | High | High | Point-of-care diagnostics, health monitoring |
| Graphene-coated Textiles | High | High | Medium | High | High | Arrhythmia detection, long-term monitoring |
| Carbon Fiber-based Sensors | High | High | Low | High | High | Real-time sodium ion detection, sports monitoring |
| Yarn/Fabric-based Microfluidics | High | High | Medium | High | High | Continuous health monitoring, disease management |
| Sensor Type | Strengths | Weaknesses | Potential Applications |
|---|---|---|---|
| Conductive Thread | Flexibility, low cost | Limited sensitivity, durability | Activity monitoring, healthcare |
| NFC-enabled Textile | Battery-free, real-time monitoring | Range limitation, cost | Systemic hyperthermia, wound healing |
| Thread-based Multiplexed | Real-time metabolic tracking | Limited biomarker panel, integration | Athletic assessment, clinical diagnosis |
| Graphene-coated Textile | Improved skin contact, washable | High cost, complex fabrication | Detecting arrhythmia |
| Thread/Fabric Microfluidic | Sweat collection, colorimetric analysis | Integration complexity, calibration | Point-of-care diagnostics |
| Stretchable Carbon Threads | Stable, sodium ion detection | Fabrication complexity, cost | Activity monitoring |
| Yarn/Fabric Microfluidic | Real-time sweat sensing | Sensor integration, scalability | Cystic fibrosis, diabetes monitoring |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Akter, A.; Apu, M.M.H.; Veeranki, Y.R.; Baroud, T.N.; Posada-Quintero, H.F. Recent Studies on Smart Textile-Based Wearable Sweat Sensors for Medical Monitoring: A Systematic Review. J. Sens. Actuator Netw. 2024, 13, 40. https://doi.org/10.3390/jsan13040040
Akter A, Apu MMH, Veeranki YR, Baroud TN, Posada-Quintero HF. Recent Studies on Smart Textile-Based Wearable Sweat Sensors for Medical Monitoring: A Systematic Review. Journal of Sensor and Actuator Networks. 2024; 13(4):40. https://doi.org/10.3390/jsan13040040
Chicago/Turabian StyleAkter, Asma, Md Mehedi Hasan Apu, Yedukondala Rao Veeranki, Turki Nabieh Baroud, and Hugo F. Posada-Quintero. 2024. "Recent Studies on Smart Textile-Based Wearable Sweat Sensors for Medical Monitoring: A Systematic Review" Journal of Sensor and Actuator Networks 13, no. 4: 40. https://doi.org/10.3390/jsan13040040
APA StyleAkter, A., Apu, M. M. H., Veeranki, Y. R., Baroud, T. N., & Posada-Quintero, H. F. (2024). Recent Studies on Smart Textile-Based Wearable Sweat Sensors for Medical Monitoring: A Systematic Review. Journal of Sensor and Actuator Networks, 13(4), 40. https://doi.org/10.3390/jsan13040040









