Efficacy of Lanthanum Carbonate and Sevelamer Carbonate as Phosphate Binders in Chronic Kidney Disease—A Comparative Clinical Study
Abstract
:1. Introduction
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tbahriti, H.F.; Kaddous, A.; Bouchenak, M.; Mekki, K. Effect of different stages of chronic kidney disease and renal replacement therapies on oxidant-antioxidant balance in uremic patients. Biochem. Res. Int. 2013, 2013, 358985. [Google Scholar] [CrossRef] [PubMed]
- Fox, C.S.; Matsushita, K.; Woodward, M.; Bilo, H.J.; Chalmers, J.; Heerspink, H.J.; Lee, B.J.; Perkins, R.M.; Rossing, P.; Sairenchi, T.; et al. Associations of kidney disease measures with mortality and end-stage renal disease in individuals with and without diabetes: A meta-analysis. Lancet 2012, 380, 1662–1673. [Google Scholar] [CrossRef] [PubMed]
- Allen, A.S.; Forman, J.P.; Orav, E.J.; Bates, D.W.; Denker, B.M.; Sequist, T.D. Primary care management of chronic kidney disease. J. Gen. Intern. Med. 2011, 26, 386–392. [Google Scholar] [CrossRef] [PubMed]
- GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2020, 395, 709–733. [Google Scholar] [CrossRef]
- Liyanage, T.; Ninomiya, T.; Jha, V.; Neal, B.; Patrice, H.M.; Okpechi, I.; Zhao, M.H.; Lv, J.; Garg, A.X.; Knight, J.; et al. Worldwide access to treatment for end-stage kidney disease: A systematic review. Lancet 2015, 385, 1975–1982. [Google Scholar] [CrossRef]
- Ke, C.; Liang, J.; Liu, M.; Liu, S.; Wang, C. Burden of chronic kidney disease and its risk-attributable burden in 137 low-and middle-income countries, 1990–2019: Results from the global burden of disease study 2019. BMC Nephrol. 2022, 23, 17. [Google Scholar] [CrossRef]
- Bharati, J.; Jha, V. Global Dialysis Perspective: India. Kidney360 2020, 1, 1143–1147. [Google Scholar] [CrossRef]
- Kumar, V.; Yadav, A.K.; Sethi, J.; Ghosh, A.; Sahay, M.; Prasad, N.; Varughese, S.; Parameswaran, S.; Gopalakrishnan, N.; Kaur, P.; et al. The Indian Chronic Kidney Disease (ICKD) study: Baseline characteristics. Clin. Kidney J. 2022, 15, 60–69. [Google Scholar] [CrossRef]
- Rajapurkar, M.M.; John, G.T.; Kirpalani, A.L.; Abraham, G.; Agarwal, S.K.; Almeida, A.F.; Gang, S.; Gupta, A.; Modi, G.; Pahari, D.; et al. What do we know about chronic kidney disease in India: First report of the Indian CKD registry. BMC Nephrol. 2012, 13, 10. [Google Scholar] [CrossRef]
- McCullough, P.A. Phosphate Control: The Next Frontier in Dialysis Cardiovascular Mortality. Cardiorenal. Med. 2021, 11, 123–132. [Google Scholar] [CrossRef]
- Taniguchi, M.; Fukagawa, M.; Fujii, N.; Hamano, T.; Shoji, T.; Yokoyama, K.; Nakai, S.; Shigematsu, T.; Iseki, K.; Tsubakihara, Y.; et al. Serum phosphate and calcium should be primarily and consistently controlled in prevalent hemodialysis patients. Ther. Apher. Dial. 2013, 17, 221–228. [Google Scholar] [CrossRef]
- Locatelli, F.; Del Vecchio, L.; Violo, L.; Pontoriero, G. Phosphate binders for the treatment of hyperphosphatemia in chronic kidney disease patients on dialysis: A comparison of safety profiles. Expert Opin. Drug. Saf. 2014, 13, 551–561. [Google Scholar] [CrossRef]
- Covic, A.; Kothawala, P.; Bernal, M.; Robbins, S.; Chalian, A.; Goldsmith, D. Systematic review of the evidence underlying the association between mineral metabolism disturbances and risk of all-cause mortality, cardiovascular mortality and cardiovascular events in chronic kidney disease. Nephrol. Dial. Transplant. 2009, 24, 1506–1523. [Google Scholar] [CrossRef]
- Doshi, S.M.; Wish, J.B. Past, Present, and Future of Phosphate Management. Kidney Int. Rep. 2022, 7, 688–698. [Google Scholar] [CrossRef]
- Sprague, S.M.; Martin, K.J.; Coyne, D.W. Phosphate Balance and CKD-Mineral Bone Disease. Kidney Int. Rep. 2021, 6, 2049–2058. [Google Scholar] [CrossRef]
- Lloret, M.J.; Ruiz-Garcia, C.; Dasilva, I.; Furlano, M.; Barreiro, Y.; Ballarin, J.; Bover, J. Lanthanum carbonate for the control of hyperphosphatemia in chronic renal failure patients: A new oral powder formulation—Safety, efficacy, and patient adherence. Patient Prefer. Adherence 2013, 7, 1147–1156. [Google Scholar] [CrossRef]
- Stevens, P.E.; Levin, A. Kidney Disease: Improving Global Outcomes Chronic Kidney Disease Guideline Development Work Group, M. Evaluation and management of chronic kidney disease: Synopsis of the kidney disease: Improving global outcomes 2012 clinical practice guideline. Ann. Intern Med. 2013, 158, 825–830. [Google Scholar] [CrossRef]
- Coresh, J.; Astor, B.C.; Greene, T.; Eknoyan, G.; Levey, A.S. Prevalence of chronic kidney disease and decreased kidney function in the adult US population: Third National Health and Nutrition Examination Survey. Am. J. Kidney Dis. 2003, 41, 1–12. [Google Scholar] [CrossRef]
- Iseki, K.; Iseki, C.; Ikemiya, Y.; Fukiyama, K. Risk of developing end-stage renal disease in a cohort of mass screening. Kidney Int. 1996, 49, 800–805. [Google Scholar] [CrossRef]
- Shaman, A.M.; Kowalski, S.R. Hyperphosphatemia Management in Patients with Chronic Kidney Disease. Saudi Pharm. J. 2016, 24, 494–505. [Google Scholar] [CrossRef] [Green Version]
- Sun, M.; Wu, X.; Yu, Y.; Wang, L.; Xie, D.; Zhang, Z.; Chen, L.; Lu, A.; Zhang, G.; Li, F. Disorders of Calcium and Phosphorus Metabolism and the Proteomics/Metabolomics-Based Research. Front Cell Dev. Biol. 2020, 8, 576110. [Google Scholar] [CrossRef] [PubMed]
- Prasad, N.; Bhadauria, D. Renal phosphate handling: Physiology. Indian J. Endocrinol. Metab. 2013, 17, 620–627. [Google Scholar] [CrossRef] [PubMed]
- Malluche, H.H.; Mawad, H. Management of hyperphosphataemia of chronic kidney disease: Lessons from the past and future directions. Nephrol. Dial. Transplant. 2002, 17, 1170–1175. [Google Scholar] [CrossRef] [PubMed]
- Floege, J. Phosphate binders in chronic kidney disease: An updated narrative review of recent data. J. Nephrol. 2020, 33, 497–508. [Google Scholar] [CrossRef]
- Babitt, J.L.; Lin, H.Y. Mechanisms of anemia in CKD. J. Am. Soc. Nephrol. 2012, 23, 1631–1634. [Google Scholar] [CrossRef]
- Atkinson, M.A.; Warady, B.A. Anemia in chronic kidney disease. Pediatr. Nephrol. 2018, 33, 227–238. [Google Scholar] [CrossRef]
- Hanna, R.M.; Streja, E.; Kalantar-Zadeh, K. Burden of Anemia in Chronic Kidney Disease: Beyond Erythropoietin. Adv. Ther. 2021, 38, 52–75. [Google Scholar] [CrossRef]
- Hutchison, A.J.; Barnett, M.E.; Krause, R.; Kwan, J.T.; Siami, G.A.; Group, S.P.D.L.S. Long-term efficacy and safety profile of lanthanum carbonate: Results for up to 6 years of treatment. Nephron. Clin. Pract. 2008, 110, c15–c23. [Google Scholar] [CrossRef]
- Covic, A.; Rastogi, A. Hyperphosphatemia in patients with ESRD: Assessing the current evidence linking outcomes with treatment adherence. BMC Nephrol. 2013, 14, 153. [Google Scholar] [CrossRef]
- Damment, S.; Secker, R.; Shen, V.; Lorenzo, V.; Rodriguez, M. Long-term treatment with lanthanum carbonate reduces mineral and bone abnormalities in rats with chronic renal failure. Nephrol. Dial. Transplant. 2011, 26, 1803–1812. [Google Scholar] [CrossRef] [Green Version]
- Hutchison, A.J.; Wilson, R.J.; Garafola, S.; Copley, J.B. Lanthanum carbonate: Safety data after 10 years. Nephrology 2016, 21, 987–994. [Google Scholar] [CrossRef]
- Rodriguez-Osorio, L.; Zambrano, D.P.; Gracia-Iguacel, C.; Rojas-Rivera, J.; Ortiz, A.; Egido, J.; Gonzalez Parra, E. Use of sevelamer in chronic kidney disease: Beyond phosphorus control. Nefrologia 2015, 35, 207–217. [Google Scholar] [CrossRef]
- Toussaint, N.D.; Lau, K.K.; Polkinghorne, K.R.; Kerr, P.G. Attenuation of aortic calcification with lanthanum carbonate versus calcium-based phosphate binders in haemodialysis: A pilot randomized controlled trial. Nephrology 2011, 16, 290–298. [Google Scholar] [CrossRef]
- Sprague, S.M.; Abboud, H.; Qiu, P.; Dauphin, M.; Zhang, P.; Finn, W. Lanthanum carbonate reduces phosphorus burden in patients with CKD stages 3 and 4: A randomized trial. Clin. J. Am. Soc. Nephrol. 2009, 4, 178–185. [Google Scholar] [CrossRef]
- Chau, Y.Y.; Kumar, J. Vitamin D in chronic kidney disease. Indian J. Pediatr. 2012, 79, 1062–1068. [Google Scholar] [CrossRef]
- Freemont, A.J.; Hoyland, J.A.; Denton, J.; Lanthanum Carbonate SPD405-303 Study Group. The effects of lanthanum carbonate and calcium carbonate on bone abnormalities in patients with end-stage renal disease. Clin. Nephrol. 2005, 64, 428–437. [Google Scholar]
- Makowka, A.; Nowicki, M. Different Effect of Lanthanum Carbonate and Sevelamer Hydrochloride on Calcium Balance in Patients with Moderate to Advanced Chronic Kidney Disease. Ther. Clin. Risk Manag. 2021, 17, 1145–1151. [Google Scholar] [CrossRef]
- Bulbul, M.C.; Dagel, T.; Afsar, B.; Ulusu, N.N.; Kuwabara, M.; Covic, A.; Kanbay, M. Disorders of Lipid Metabolism in Chronic Kidney Disease. Blood Purif. 2018, 46, 144–152. [Google Scholar] [CrossRef]
- Trevisan, R.; Dodesini, A.R.; Lepore, G. Lipids and renal disease. J. Am. Soc. Nephrol. 2006, 17, S145–S147. [Google Scholar] [CrossRef]
- Pan, X. Cholesterol Metabolism in Chronic Kidney Disease: Physiology, Pathologic Mechanisms, and Treatment. Adv. Exp. Med. Biol. 2022, 1372, 119–143. [Google Scholar] [CrossRef]
- Hamida, F.B.; Fatma, L.B.; Barbouch, S.; Kaaroud, H.; Helal, I.; Hedri, H.; Abdallah, T.B.; Maiz, H.B.; Kheder, A. Effect of sevelamer on mineral and lipid abnormalities in hemodialysis patients. Saudi J. Kidney Dis. Transpl. 2008, 19, 183–188. [Google Scholar] [PubMed]
- Yamada, K.; Fujimoto, S.; Tokura, T.; Fukudome, K.; Ochiai, H.; Komatsu, H.; Sato, Y.; Hara, S.; Eto, T. Effect of sevelamer on dyslipidemia and chronic inflammation in maintenance hemodialysis patients. Ren. Fail. 2005, 27, 361–365. [Google Scholar] [CrossRef] [PubMed]
- Braunlin, W.; Zhorov, E.; Guo, A.; Apruzzese, W.; Xu, Q.; Hook, P.; Smisek, D.L.; Mandeville, W.H.; Holmes-Farley, S.R. Bile acid binding to sevelamer HCl. Kidney Int. 2002, 62, 611–619. [Google Scholar] [CrossRef] [PubMed]
- Isaka, Y.; Hamano, T.; Fujii, H.; Tsujimoto, Y.; Koiwa, F.; Sakaguchi, Y.; Tanaka, R.; Tomiyama, N.; Tatsugami, F.; Teramukai, S. Optimal Phosphate Control Related to Coronary Artery Calcification in Dialysis Patients. J. Am. Soc. Nephrol. 2021, 32, 723–735. [Google Scholar] [CrossRef]



| Gender (Sex) | Group 1 n (%) | Group 2 n (%) |
|---|---|---|
| Male | 41 (54%) | 43 (57%) |
| Female | 34 (46%) | 32 (43%) |
| Age | ||
| 21–35 | 13 (17%) | 11 (15%) |
| 36–50 | 22 (29%) | 22 (29%) |
| 51–60 | 40 (54%) | 42 (56%) |
| Area | ||
| Rural | 39 (52%) | 42 (56%) |
| Urban | 36 (48%) | 33 (44%) |
| Stages of CKD | ||
| Stage 3 | 28 (37%) | 24 (32%) |
| Stage 4 | 39 (52%) | 40 (54%) |
| Stage 5 | 8 (11%) | 11 (14%) |
| Laboratory Parameters | Group 1 | Group 2 | ||
|---|---|---|---|---|
| On 1st Visit | After 6 Months | On 1st Visit | After 6 Months | |
| Hemoglobin (g/dL) | 8.91 ± 0.39 | 10.93 ± 0.42 | 9.06 ± 0.80 | 10.74 ± 0.50 |
| Total Leukocyte Count (/cumm) | 9.16 ± 0.53 | 9.79 ± 0.36 | 10.1 ± 0.66 | 12.11 ± 0.47 |
| Platelet Count (/cumm) | 188 ± 13 | 218 ± 14 | 198 ± 19 | 220 ± 20 |
| LFT | Laboratory Parameters | Group 1 (n = 75) | Group 2 (n = 75) | ||
| On 1st Visit | After 6 Months | On 1st Visit | After 6 Months | ||
| Alkaline Phosphatase (U/L) | 155.16 ± 12.93 | 109.86 ± 10.69 | 187.16 ± 34.21 | 170.8 ± 25.39 | |
| SGOT (U/L) | 50.03 ± 13.31 | 42.25 ± 7.25 | 41.25 ± 10.71 | 35.17 ± 4.7 | |
| SGPT (U/L) | 40.97 ± 4.10 | 36.97 ± 4.28 | 35.58 ± 8.16 | 32.92 ± 4.76 | |
| Total Protein (g/dL) | 6.87 ± 0.17 | 7.11 ± 0.17 | 6.48 ± 0.37 | 6.73 ± 0.16 | |
| Serum Albumin (g/dL) | 2.61 ± 0.12 | 3.86 ± 0.11 | 2.98 ± 0.23 | 3.73 ± 0.18 | |
| Serum Electrolyte | Laboratory Parameters | Group 1 (n = 75) | Group 2 (n = 75) | ||
| On 1st Visit | After 6 Months | On 1st Visit | After 6 Months | ||
| Serum calcium (mg/dL) | 8.2 ± 0.2 | 9.5 ± 0.2 | 8.6 ± 0.2 | 10.7 ± 0.1 | |
| Serum sodium (mEq/L) | 135 ± 1 | 131 ± 0 | 139 ± 2 | 136 ± 1 | |
| Serum potassium (mEq/L) | 4.6 ± 0.2 | 4.8 ± 0.2 | 4.8 ± 0.3 | 4.8 ± 0.2 | |
| Serum chloride (mEq/L) | 111 ± 1 | 103 ± 1 | 109 ± 1 | 103 ± 1 | |
| Others | Laboratory Parameters | Group 1 (n = 75) | Group 2 (n = 75) | ||
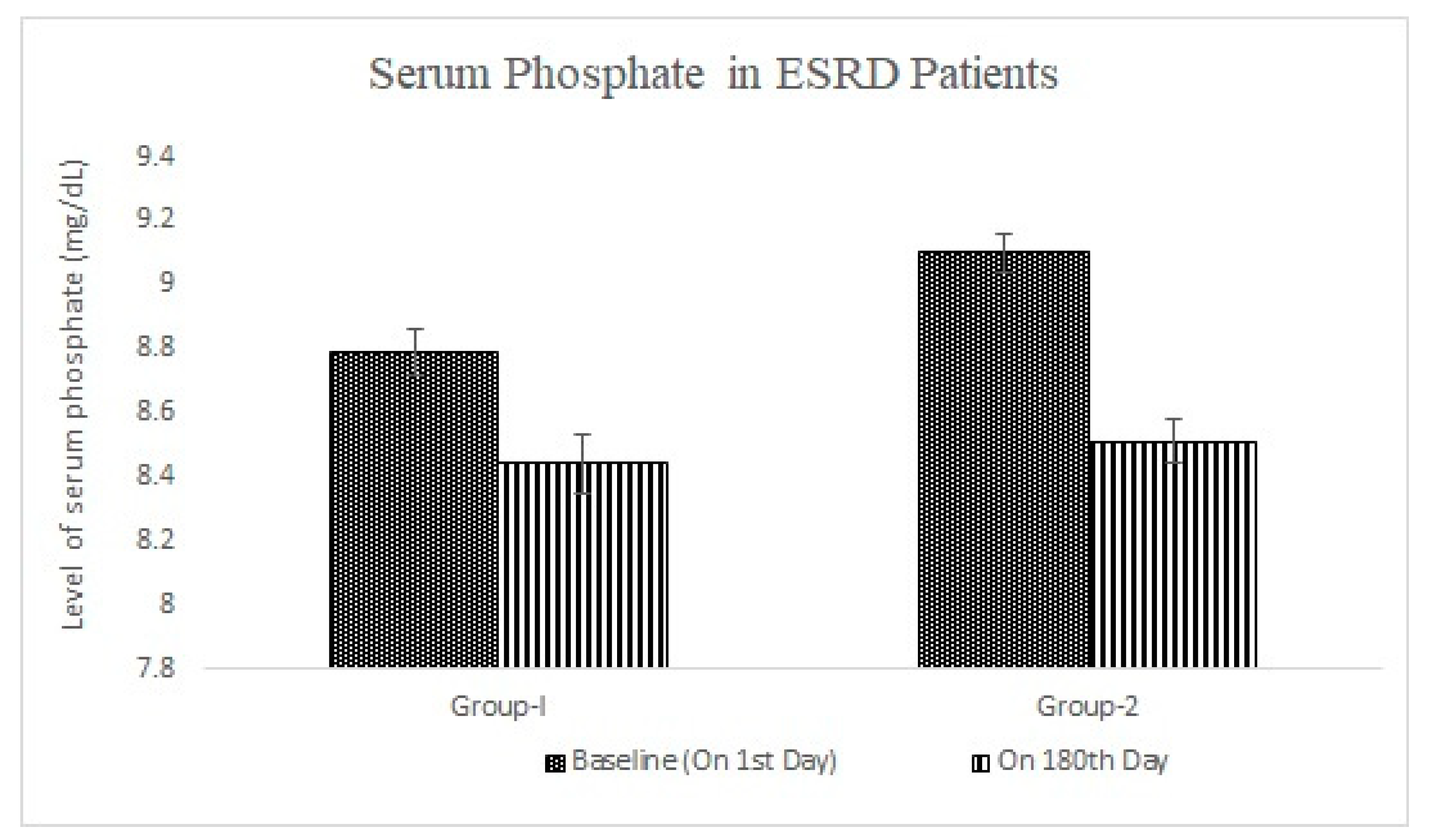
| On Baseline | After 6 Months | On Baseline | After 6 Months | ||
| Triglycerides (mg/dL) | 180 ± 18 | 166 ± 15 | 185 ± 13 | 157 ± 13 | |
| PTH (pg/mL) | 70 ± 3 | 69 ± 3 | 72 ± 5 | 68 ± 5 | |
| Vitamin D (ng/mL) | 20 ± 0 | 23 ± 1 | 21 ± 1 | 25 ± 0 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nain, P.; Nayak, N.; Maj, M.C.; Singh, R.K.; Kaur, J.; Jeong, Y.; Maity, S.; Nath, R.; Hilgers, R.H.; Nauhria, S.; et al. Efficacy of Lanthanum Carbonate and Sevelamer Carbonate as Phosphate Binders in Chronic Kidney Disease—A Comparative Clinical Study. Pharmacy 2023, 11, 27. https://doi.org/10.3390/pharmacy11010027
Nain P, Nayak N, Maj MC, Singh RK, Kaur J, Jeong Y, Maity S, Nath R, Hilgers RH, Nauhria S, et al. Efficacy of Lanthanum Carbonate and Sevelamer Carbonate as Phosphate Binders in Chronic Kidney Disease—A Comparative Clinical Study. Pharmacy. 2023; 11(1):27. https://doi.org/10.3390/pharmacy11010027
Chicago/Turabian StyleNain, Parminder, Narendra Nayak, Mary C. Maj, Rohit Kumar Singh, Jaspreet Kaur, Yujin Jeong, Sabyasachi Maity, Reetuparna Nath, Robert H. Hilgers, Shreya Nauhria, and et al. 2023. "Efficacy of Lanthanum Carbonate and Sevelamer Carbonate as Phosphate Binders in Chronic Kidney Disease—A Comparative Clinical Study" Pharmacy 11, no. 1: 27. https://doi.org/10.3390/pharmacy11010027
APA StyleNain, P., Nayak, N., Maj, M. C., Singh, R. K., Kaur, J., Jeong, Y., Maity, S., Nath, R., Hilgers, R. H., Nauhria, S., & Nauhria, S. (2023). Efficacy of Lanthanum Carbonate and Sevelamer Carbonate as Phosphate Binders in Chronic Kidney Disease—A Comparative Clinical Study. Pharmacy, 11(1), 27. https://doi.org/10.3390/pharmacy11010027





