Optimization of the Danish National Electronic Prescribing System to Improve Patient Safety: Development of a User-Friendly Prototype of the Digital Platform Shared Medication Record
Abstract
:1. Introduction
2. Methods
2.1. Shared Medication Record
2.2. Setting
2.3. Design and Participants
2.4. Semi-Structured Interview
- What is the role of the SMR in your work?
- What are your experiences with the SMR?
- Do you have any suggestions for how to improve the SMR functionality?
2.5. Iterative Design
3. Results
3.1. Themes
- 1.
- The SMR does not get updated regularly
“It is a requirement that the patients get a medical note. We can’t even print this note because the doctors technically have not approved it in SMR. This affects us and makes it difficult for us to do our jobs.”
- 2.
- It is unclear who has the responsibility to update the SMR
“I think that a part of the issue is that the responsibility is complex in some matters. I mean, you need to consider, when a patient gets prescribed medicine, it is usually not just one person, but several medical professions who is a part of this process...”
- 3.
- The system is complex, time-consuming, and unintuitive
“The thing with SMR as is that the concept works well, and it is really handy that it is available on every device. The problem with SMR is the integration with the health platform. This is horrible.”
- 4.
- Patients are often unaware that they can access the SMR, so they do not have complete insight into their medication
“Not a lot of those who use SMR have an overview over their medicine. It is rare that I experience people using it—including the younger patients.”
- 5.
- There is a need for other professional groups and/or patients to be involved in the prescribing process
“It may be linked to age and tech flair, but I think a lot of patients will benefit from more involvement... I think it could create dialogue and be easier for doctors to clean up old medicine or update the SMR.”
3.2. Prototype for an Optimized SMR
4. Discussion
4.1. Patient Safety
4.2. Workflow Efficiency
4.3. Healthcare Costs
4.4. Strength and Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Current Version of the Shared Medication Record (SMR)





Appendix B. Identified Codes and Themes
| Code | Count | Theme |
| “Updating” | 19 | The SMR does not get updated |
| “Responsibility” | 18 | Uncertainties as to who has the primary responsibility of updating the SMR |
| “The system” | 45 | The system is too complex, time-consuming, and lacks an intuitive approach |
| “Familiarity” | 25 | There is an absence of familiarity with the SMR from the patient’s side, which makes their overview of actual medicine non-efficient |
| “Involvement” | 13 | There is a need for involvement by other relevant medical professionals and/or the patients |
Appendix C. Codes and Key Citations from Interviews
| Updating | Responsibility | The System | Familiarity | Involvement |
Nurse 1:
| Pharmacist 1:
| Doctor 3:
| Patient 2:
| Doctor 2:
|
Nurse 2:
| Pharmacy technician 1:
| Nurse 1:
| Nurse 3:
| Pharmacy technician 1:
|
Doctor 1:
| Doctor 2:
| Pharmacist 1:
| Doctor 1:
| Pharmacist 2:
|
Appendix D. Prototype







References
- Stock, R.; Mahoney, E.R.; Gauthier, D.; Center, L.; Minniti, M.; Scott, J.; Pierson, M.; Nichols, L. Developing a Community-Wide Electronic Shared Medication List; Advances in Patient Safety; Agency for Healthcare Research and Quality (US): Rockville, MD, USA, 2008. [Google Scholar]
- Munck, L.K.; Hansen, K.R.; Mølbak, A.G.; Balle, H.; Kongsgren, S. The Use of Shared Medication Record as Part of Medication Reconciliation at Hospital Admission Is Feasible. Dan. Med. J. 2014, 61, 1–5. [Google Scholar]
- Hammar, T.; Ekedahl, A.; Petersson, G. Implementation of a Shared Medication List: Physicians’ Views on Availability, Accuracy and Confidentiality. Int. J. Clin. Pharm. 2014, 36, 933–942. [Google Scholar] [CrossRef]
- Jøsendal, A.V.; Bergmo, T.S. How Discrepancies in Medication Records Affect the Creation and Trust in a Shared Electronic Medication List in Norway. In Proceedings of the 17th Scandinavian Conference on Health ce on Health Informatics, Oslo, Norway, 12–13 November 2019. [Google Scholar]
- Simonson, W. Polypharmacy, MRPs, PIMs and Deprescribing. Geriatr. Nur. (Lond.) 2015, 36, 467–468. [Google Scholar] [CrossRef]
- Ruiter, R.; Visser, L.E.; Rodenburg, E.M.; Trifiró, G.; Ziere, G.; Stricker, B.H. Adverse Drug Reaction-Related Hospitalizations in Persons Aged 55 Years and Over. Drugs Aging 2012, 29, 225–232. [Google Scholar] [CrossRef]
- Saedder, E.A.; Lisby, M.; Nielsen, L.P.; Bonnerup, D.K.; Brock, B. Number of Drugs Most Frequently Found to Be Independent Risk Factors for Serious Adverse Reactions: A Systematic Literature Review. Br. J. Clin. Pharmacol. 2015, 80, 808–817. [Google Scholar] [CrossRef] [Green Version]
- Fushiki, Y.; Kinoshita, K.; Tokuda, Y. Polypharmacy and Adverse Drug Events Leading to Acute Care Hospitalization in Japanese Elderly. Gen. Med. 2014, 15, 110–116. [Google Scholar] [CrossRef] [Green Version]
- Bülow, C.; Noergaard, J.D.S.V.; Færch, K.U.; Pontoppidan, C.; Unkerskov, J.; Johansson, K.S.; Kornholt, J.; Christensen, M.B. Causes of Discrepancies between Medications Listed in the National Electronic Prescribing System and Patients’ Actual Use of Medications. J. Am. Geriatr. Soc. 2021, 129, 221–231. [Google Scholar] [CrossRef]
- Bülow, C.; Flagstad Bech, C.; Ullitz Faerch, K.; Trærup Andersen, J.; Byg Armandi, H.; Treldal, C. Discrepancies Between the Medication List in Electronic Prescribing Systems and Patients’ Actual Use of Medicines. Sr. Care Pharm. 2019, 34, 317–324. [Google Scholar] [CrossRef]
- Andersen, T.S.; Gemmer, M.N.; Sejberg, H.R.C.; Jørgensen, L.M.; Kallemose, T.; Andersen, O.; Iversen, E.; Houlind, M.B. Medicines Reconciliation in the Emergency Department: Important Prescribing Discrepancies between the Shared Medication Record and Patients’ Actual Use of Medication. Pharm. Basel Switz. 2022, 15, 142. [Google Scholar] [CrossRef]
- Beretning Til Statsrevisorerne Om Problemerne Med at Udvikle Og Implementere Fælles Medicinkort. Available online: https://rigsrevisionen.dk/Media/B/A/problemerne-med-at-udvikle-og-implementere-faelles-medicinkort.pdf (accessed on 24 October 2021).
- Fælles Medicinkort (FMK). Available online: https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-faelles-medicinkort (accessed on 30 September 2020).
- Vejledning FMK-Online. Available online: https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-faelles-medicinkort/fmk-sundhedsprofessionelle?fbclid=IwAR08M0lyzU2VSjUkw3f7pC2XXg3-xu5x8sRePt5pHVu9UFEK4mSZE16ZPDY (accessed on 25 September 2021).
- Fælles Medicinkort Øger Sikkerheden. Available online: https://systematic.com/da-dk/healthcare/news/2016/faelles-medicinkort-oeger-sikkerheden/ (accessed on 30 September 2020).
- Statistik for Ajorføring Af FMK. Available online: https://sundhedsdatastyrelsen.dk/da/registre-og-services/om-faelles-medicinkort/baggrund-og-organisering/status-og-overblik-fmk (accessed on 23 October 2021).
- Dansk Patientsikkerhedsdatabase: Årsberetning 2019. Copenhagen: Styrelsen for Patientsikkerhed. Available online: https://stps.dk/da/udgivelser/2020/aarsberetning-for-dansk-patientsikkerhedsdatabase-2019/~/media/01707469F7F9446FB3D3FD4EAB99CD6E (accessed on 30 October 2021).
- Utilsigtede Hændelse. Available online: https://stps.dk/da/laering/utilsigtede-haendelser/# (accessed on 25 November 2021).
- Hamzah, A.; Wahid, F. Participatory Design in the Development of Healthcare Systems: A Literature Review. In Proceedings of the 2nd International Conference on Communication and Information Processing, Singapore, 26–29 November 2016. [Google Scholar]
- van der Velden, M.; Mörtberg, C. Participatory Design and Design for Values. In Handbook of Ethics, Values, and Technological Design: Sources, Theory, Values and Application Domains; van den Hoven, J.M., Vermaas, P.E., van de Poel, I., Eds.; Springer: Berlin/Heidelberg, Germany, 2014. [Google Scholar]
- Iterative Design Process—An Overview | ScienceDirect Topics. Available online: https://www-sciencedirect-com.ep.fjernadgang.kb.dk/topics/computer-science/iterative-design-process (accessed on 10 December 2021).
- Preece, J.; Rogers, Y.; Sharp, H. Interaction Design: Beyond Human-Computer Interaction, 4th ed.; Wiley & Sons Ltd.: Hoboken, NJ, USA, 2015. [Google Scholar]
- Bryman, A. Social Research Methods; Oxford University Press: Oxford, UK, 2016; Volume 5. [Google Scholar]
- Shared Medication Record. Available online: https://www.medcom.dk/medcom-in-english/national-activities/shared-medication-record (accessed on 2 October 2020).
- Medicinering-Anvendelse Af Fælles Medicinkort (FMK). Available online: https://pri.rn.dk/Sider/22261.aspx (accessed on 2 October 2020).
- DeJonckheere, M.; Vaughn, L.M. Semistructured Interviewing in Primary Care Research: A Balance of Relationship and Rigour. Fam. Med. Community Health 2019, 7, e000057. [Google Scholar] [CrossRef] [Green Version]
- Braun, V.; Clarke, V. Thematic Analysis. In APA handbook of research methods in psychology: Research designs: Quantitative, qualitative, neuropsychological, and biological; Cooper, H., Camic, P.M., Long, D.L., Panter, A.T., Rindskopf, D., Sher, K.J., Eds.; American Psychological Association.: Washington, DC, USA, 2012; Volume 2. [Google Scholar]
- Manskow, U.S.; Lind, K.F.; Bergmo, T.S. Digital Solutions for a Shared Medication List: A Narrative Literature Review. In Proceedings of the 17th Scandinavian Conference on Health Informatics, Oslo, Norway, 12–13 November 2019. [Google Scholar]
- Al-Hashar, A.; Al-Zakwani, I.; Eriksson, T.; Al Za’abi, M. Whose Responsibility Is Medication Reconciliation: Physicians, Pharmacists or Nurses? A Survey in an Academic Tertiary Care Hospital. Saudi Pharm. J. SPJ 2017, 25, 52–58. [Google Scholar] [CrossRef] [Green Version]
- Rozich, J.; Resar, R. Medication Safety: One Organization’s Approach to the Challenge. JCOM-WAYNE PA- 2001, 8, 27–34. [Google Scholar]
- Schiøtz, M.L.; Frølich, A.; Jensen, A.K.; Reuther, L.; Perrild, H.; Petersen, T.S.; Kornholt, J.; Christensen, M.B. Polypharmacy and Medication Deprescribing: A Survey among Multimorbid Older Adults in Denmark. Pharmacol. Res. Perspect. 2018, 6, e00431. [Google Scholar] [CrossRef] [Green Version]
- Jacobsen, D.I.; Thorsvik, J. Hvordan Organisationer Fungerer: En Indføring i Organisation Og Ledelse, 3rd ed.; Hans Reitzels Forlag: Copenhagen, Denmark, 2013. [Google Scholar]
- Aharaz, A.; Rasmussen, J.H.; McNulty, H.B.Ø.; Cyron, A.; Fabricius, P.K.; Bengaard, A.K.; Sejberg, H.R.C.; Simonsen, R.R.L.; Treldal, C.; Houlind, M.B. A Collaborative Deprescribing Intervention in a Subacute Medical Outpatient Clinic: A Pilot Randomized Controlled Trial. Metabolites 2021, 11, 204. [Google Scholar] [CrossRef]
- Houlind, M.B.; Andersen, A.L.; Treldal, C.; Jørgensen, L.M.; Kannegaard, P.N.; Castillo, L.S.; Christensen, L.D.; Tavenier, J.; Rasmussen, L.J.H.; Ankarfeldt, M.Z.; et al. A Collaborative Medication Review Including Deprescribing for Older Patients in an Emergency Department: A Longitudinal Feasibility Study. J. Clin. Med. 2020, 9, 348. [Google Scholar] [CrossRef] [Green Version]
- Campanella, P.; Lovato, E.; Marone, C.; Fallacara, L.; Mancuso, A.; Ricciardi, W.; Specchia, M.L. The Impact of Electronic Health Records on Healthcare Quality: A Systematic Review and Meta-Analysis. Eur. J. Public Health 2016, 26, 60–64. [Google Scholar] [CrossRef] [Green Version]
- Bates, D.W.; Cohen, M.; Leape, L.L.; Overhage, M.J.; Shabot, M.; Sheridan, T. Reducing the Frequency of Errors in Medicine Using Information Technology. J. Am. Med. Inform. Assoc. 2001, 299–308. [Google Scholar] [CrossRef] [Green Version]


| Implementation | Description |
|---|---|
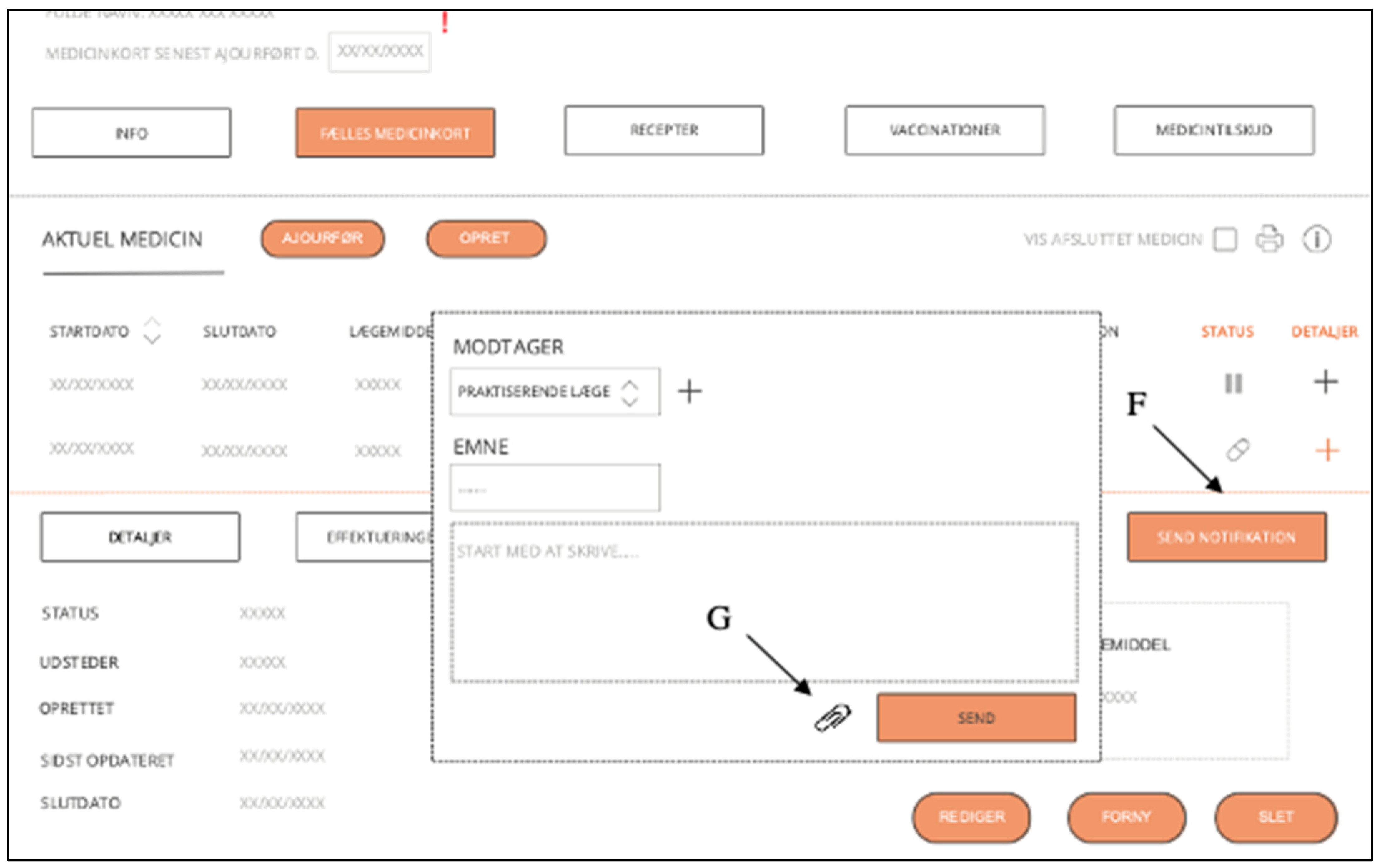
| Overall redesign | A more manageable, navigable, and straightforward interface that facilitates up-to-date, complete, and accurate medication records as well as knowledge and information sharing |
| ‘Last updated’-field (A) | States when the medication record was last updated. A notification will appear if it has not been updated for X-months |
| ‘Edit’-button (B) | Current medication can be edited so that the risk of double/incorrect prescriptions is reduced |
| ‘Renew’-button (C) | Current medication can be renewed so that the risk of double prescriptions is reduced * |
| ‘Delete’-button (D) | Current medication can be deleted so that the risk of double/incorrect prescriptions is reduced |
| ‘Note’-button (E) | It makes it possible to write notes to a specific medication (if important, it is indicated with a red exclamation mark) |
| ‘Send notification’-button (F) | It makes it possible to notify a patient’s general practitioner or other relevant parties about any changes, suggestions, notes, etc. in medication |
| ‘Attach file/document’-button (G) | It makes it possible to attach relevant files/pictures/documents in connection with the ‘send notification’ and/or ’note’-button |
| ‘End date’-field (H) | End date requirements in connection with the creation of prescriptions * |
| ‘Medication is about to expire’-function (I) | A notification will appear as the medication is about to expire. If the user does not renew the medication, it will be removed from the ‘current medication’ list and then appear on the list of ‘completed medication.’ |
| ‘Irregularities in effectuation’-function (J) | A notification will appear if there are irregularities in the effectuated medication |
| ‘Contact patient’-button (K) | It makes it possible to contact the patient directly via the SMR, either per phone or virtually (with video) |
| ‘Dropdown navigation menu’ (L) | The dropdown navigation menu for more straightforward navigation |
| ‘Add shortcut’-button (M) | Personalized frontpage that lets users select and add the most frequently used shortcuts to the frontpage |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aharaz, A.; Kejser, C.L.; Poulsen, M.W.; Jeftic, S.; Ulstrup-Hansen, A.I.; Jørgensen, L.M.; Iversen, E.; Thorhauge, A.M.; Houlind, M.B. Optimization of the Danish National Electronic Prescribing System to Improve Patient Safety: Development of a User-Friendly Prototype of the Digital Platform Shared Medication Record. Pharmacy 2023, 11, 41. https://doi.org/10.3390/pharmacy11020041
Aharaz A, Kejser CL, Poulsen MW, Jeftic S, Ulstrup-Hansen AI, Jørgensen LM, Iversen E, Thorhauge AM, Houlind MB. Optimization of the Danish National Electronic Prescribing System to Improve Patient Safety: Development of a User-Friendly Prototype of the Digital Platform Shared Medication Record. Pharmacy. 2023; 11(2):41. https://doi.org/10.3390/pharmacy11020041
Chicago/Turabian StyleAharaz, Anissa, Cecillie Louise Kejser, Mille Wilhjelm Poulsen, Sara Jeftic, Aisha Isabella Ulstrup-Hansen, Lillian Mørch Jørgensen, Esben Iversen, Anne Mette Thorhauge, and Morten Baltzer Houlind. 2023. "Optimization of the Danish National Electronic Prescribing System to Improve Patient Safety: Development of a User-Friendly Prototype of the Digital Platform Shared Medication Record" Pharmacy 11, no. 2: 41. https://doi.org/10.3390/pharmacy11020041





