The Pharmacist Prescriber: A Psychological Perspective on Complex Conversations about Medicines: Introducing Relational Prescribing and Open Dialogue in Physical Health
Abstract
:1. Introduction
“By far the most frequently used drug in general practice was the doctor himself, i.e., it was not only the bottle of medicine or the box of pills that mattered, but the way the doctor gave them to his patient—in fact the whole atmosphere in which the drug was given and taken.” [6].
2. Meaning and Medication: The Evidence Base
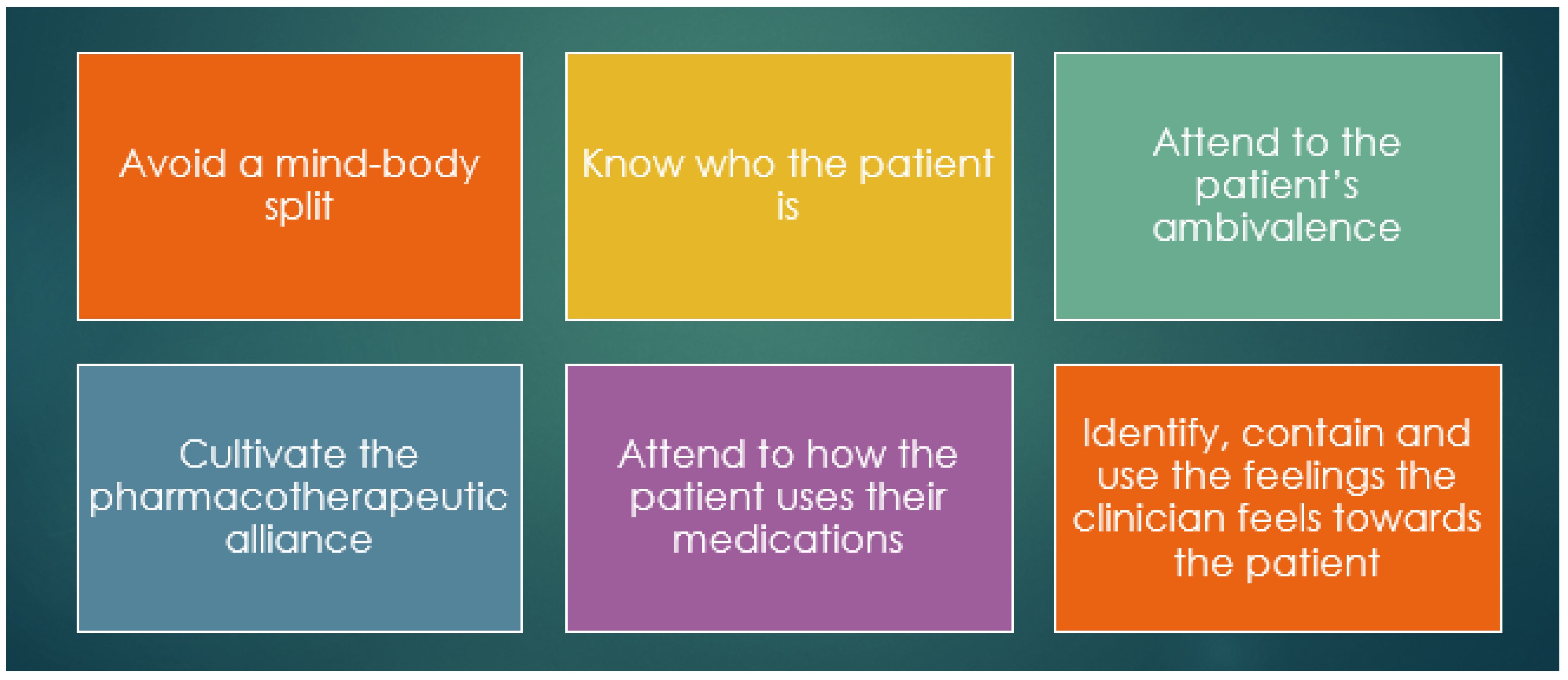
2.1. Relational Prescribing
2.1.1. Avoid Mind–Body Split
2.1.2. Know Who the Patient Is
“It is much more important to know what sort of a patient has a disease than to know what sort of a disease a patient has.” (attributed to Sir William Osler, cited in [33])
2.1.3. Attend to the Patient’s Ambivalence
2.1.4. Cultivate a Pharmacotherapeutic Alliance
2.1.5. Attend to How the Patient Uses Their Medication
2.1.6. Identify, Contain, and Use Feelings the Clinician Feels towards the Patient
- ▶
- Empathy
- ▶
- Warmth
- ▶
- Caring/Helpful/loving/competence
- ▶
- Frustration/anger
- ▶
- Helplessness/despair
- ▶
- Anxiety/sense of persecution/incompetence
- ▶
- Shame
- ▶
- Repulsion/disgust
2.2. In Summary: Relational Prescribing
3. Open Dialogue
4. Shared Decision Making and Coaching
5. Moving Forward—The Cultural and Educational Imperatives
6. Vignette
- Transactional:
- I explained that there was a limit to how much we can control our cholesterol in this way. For some people, medication is the only way to reduce it enough to make a significant difference, and he was reassured by this.
Armed with this information and the medication, would he now be happy to start taking it? What further discussion might be of benefit?
- Relational prescribing:
- I said that it seemed like he had tried very hard to take control of his health and asked how it felt that his cholesterol was still not in the normal range. He said it had felt like a failure not to have been able to reduce his cholesterol with diet and exercise. He had tried to manage it by swimming three times a week, reducing fats in his diet, using plant-sterol spread, and taking a plant-sterol-containing drink every day. He said that he thought he could do it because he had been successful at avoiding the need for medication for his type two diabetes through diet and exercise.
6.1. Avoid Mind–Body Split
6.2. Know Who the Patient Is
6.3. Attend to the Patient’s Ambivalence
6.4. Cultivate a Pharmacotherapeutic Alliance
6.5. Attend to How the Patient Uses Their Medication
6.6. Identify, Contain, and Use Feelings the Clinician Feels towards the Patient
6.7. An Open Dialogue Approach
- Pharmacist:
- “Something in me feels that the idea of taking a statin for life may feel uncomfortable for you?”.
- Patient:
- “Yes, I feel like an old man and a failure as I really thought that my diet and exercise could sort out my cholesterol, I don’t want to take pills till I die”.
- Pharmacist to wife:
- “I know you initiated this consultation, have you got concerns you want to share?”.
- Wife:
- “Well, I know he probably needs them, but my brother died from a stroke at 53 whilst taking statins, so I feel really conflicted as the doctor said that once on them, he will never be able to stop them”.
The wife may then cry and reach out to hold her husband’s hand.
- Wife:
- “Robert may say start them but remain vigilant regarding exercise and diet”.
- Pharmacist to both:
- “The evidence is that cholesterol doesn’t always respond to lifestyle changes and often needs statins”.
- Patient to wife and pharmacist:
- “I know she [looking at wife] is concerned, and I appreciate how hard she… well we all took Robert’s death at such a young age”.
- Wife:
- “Yes, it has been and still remains hard, Robert left two teenage girls and our kids miss their uncle and they are very close to their cousins”.
- Pharmacist (with a better understanding of the context):
- “Medicines do not need to be taken with a view to never stopping, would it feel comfortable to start for twelve weeks, and then return for a review so that we can then think together again?”.
- Patient:
- “So you’d monitor me that regularly?”.
- Wife:
- “And could we all meet together again for the review?”.
- Pharmacist:
- “Yes of course, and we can then check how you are responding and do continue the exercise and diet regime”.
7. Summary
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Barnett, N.L.; Varia, S.; Jubraj, B. Adherence: Are you asking the right questions and taking the best approach? Pharm. J. 2013, 291, 153. [Google Scholar]
- Halpern, J. What is clinical empathy? J. Gen. Intern. Med. 2003, 18, 670–674. [Google Scholar] [PubMed]
- Konstantinidou, H.; Chartonas, D.; Rogalski, D.; Lee, T. Will this tablet make me happy again? The contribution of relational prescribing in providing a pragmatic and psychodynamic framework for prescribers. BJPsych Adv. 2022, 1–9. [Google Scholar] [CrossRef]
- Wolf, M.H.; Putnam, S.M.; James, S.A.; Stiles, W.B. The medical interview satisfaction scale: Development of a scale to measure patient perceptions of physician behavior. J. Behav. Med. 1978, 1, 391–401. [Google Scholar] [PubMed]
- Jubraj, B.; Barnett, N.L.; Grimes, L.; Varia, S.; Chater, A.; Auyeung, V. Why we should understand the patient experience: Clinical empathy and medicines optimisation. Int. J. Pharm. Pr. 2016, 24, 367–370. [Google Scholar] [CrossRef] [Green Version]
- Balint, M. The doctor, his patient and the Illness. Lancet 1955, 2, 683–688. [Google Scholar]
- Mintz, D.L.; Flynn, D.F. How (not what) to prescribe: Nonpharmacologic aspects of psychopharmacology. Psychiatr. Clin. N. Am. 2012, 35, 143–163. [Google Scholar]
- Mintz, D. Meaning and medication in the care of treatment-resistant patients. Am. J. Psychother. 2002, 56, 322–337. [Google Scholar] [CrossRef] [Green Version]
- Stewart, M.A. Effective physician-patient communication and health outcomes: A review. Can. Med. Assoc. J. 1995, 152, 1423–1433. [Google Scholar]
- Haigh, R.; Benefield, N. Towards a unified model of human development. Ment. Health Rev. J. 2019, 24, 124–132. [Google Scholar]
- World Health Organization (WHO). People-Centered Health Care: A Policy Framework. 2007. Available online: https://www.who.int/publications/i/item/9789290613176 (accessed on 2 November 2022).
- NHS England. Pharmaceutical Waste Reduction in the NHS; NHS: London, UK, 2015. Available online: https://www.england.nhs.uk/publication/pharmaceutical-waste-reduction-in-the-nhs/ (accessed on 2 November 2022).
- NICE, Medicines Optimization: The Safe and Effective Use of Medicines to Enable the Best Possible Outcomes NICE Guideline [NG5]. 2015. Available online: www.nice.org.uk/guidance/ng5 (accessed on 2 November 2022).
- NICE, Medicines Adherence: Involving Patients in Decisions about Prescribed Medicines and Supporting Adherence Clinical Guideline [CG76]. 2009. Available online: www.nice.org.uk/guidance/cg76 (accessed on 2 November 2022).
- Zolnierek, K.B.H.; Dimatteo, M.R. Physician communication and patient adherence to treatment: A meta-analysis. Med. Care 2009, 47, 826–834. [Google Scholar] [CrossRef] [Green Version]
- Ward, M.M.; Sundaramurthy, S.; Lotstein, D.; Bush, T.M.; Neuwelt, C.M.; Street, R.L., Jr. Participatory patient–physician communication and morbidity in patients with systemic lupus erythematosus. Arthritis Rheum. 2003, 49, 810–818. [Google Scholar]
- Street, R.L., Jr.; Voigt, B. Patient participation in deciding breast cancer treatment and subsequent quality of life. Med. Decis Making 1997, 17, 298–306. [Google Scholar]
- Tongue, J.R.; Epps, H.R.; Forese, L.L. Communication skills for patient centered care: Research-based, easily learned techniques for medical interviews that benefit orthopaedic surgeons and their patients. J. Bone Joint Surg. Am. 2005, 87, 652–658. [Google Scholar]
- Duffy, F.D.; Gordon, G.H.; Whelan, G.; Cole-Kelly, K.; Frankel, R. Assessing Competence in Communication and Interpersonal Skills: The Kalamazoo II Report. Acad. Med. 2004, 79, 495–507. [Google Scholar] [PubMed] [Green Version]
- Kaplan, S.H.; Greenfield, S.; Gandek, B.; Rogers, W.H.; Ware, J.E. Characteristics of physicians with participatory decision-making styles. Ann. Intern. Med. 1996, 124, 497–504. [Google Scholar] [PubMed]
- Davidoff, F. Time. Ann. Intern. Med. 1997, 127, 483–485. [Google Scholar] [PubMed]
- Ha, J.F.; Longnecker, N. Doctor-Patient Communication: A Review. Ochsner J. Mar. 2010, 10, 38–43. [Google Scholar]
- Skea, Z.; Harry, V.; Bhattacharya, S.; Entwistle, V.; Williams, B.; MacLennan, G.; Templeton, A. Women’s perceptions of decision-making about hysterectomy. BJOG 2004, 111, 133–142. [Google Scholar]
- Kaplan, S.H.; Greenfield, S.; Ware, J.E., Jr. Assessing the effects of physician-patient interactions on the outcomes of chronic disease. Med. Care 1989, 27 (Suppl. S3), S110–S127. [Google Scholar]
- Wei, L.; Chapman, S.; Li, X.; Li, X.; Li, S.; Chen, R.; Bo, N.; Chater, A.; Horne, R. Beliefs about medicines and non-adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: A cross-sectional study in China. BMJ Open 2017, 7, e017293. [Google Scholar] [CrossRef] [PubMed]
- Horne, R.; Chapman, S.; Parham, R.; Freemantle, N.; Forbes, A.; Cooper, V. Understanding Patients’ Adherence-Related Beliefs about Medicines Prescribed for Long-Term Conditions: A Meta-Analytic Review of the Necessity-Concerns Framework. PLoS ONE 2013, 8, e80633. [Google Scholar] [CrossRef]
- Jalal, Z.; Akhtar, S.; Finlay, K.; King, K.; Goel, N.; Ward, J. Perceptions of UK Community Pharmacists on Current Consultation Skills and Motivational Interviewing as a Consultation Approach: A Qualitative Study. Pharmacy 2019, 7, 52. [Google Scholar] [CrossRef] [Green Version]
- Barnett, N.L.; Leader, I.; Easthall, C. Developing person-centered consultation skills within a UK hospital pharmacy service: Evaluation of a pilot practice-based support package for pharmacy staff. Eur. J. Hosp. Pharm. 2019, 26, 93–100. [Google Scholar]
- Ilardo, M.L.; Speciale, A. The Community Pharmacist: Perceived Barriers and Patient-Centered Care Communication. Int. J. Environ. Res. Public Health 2020, 17, 536. [Google Scholar] [CrossRef] [Green Version]
- Greenhill, N.; Anderson, C.; Avery, A.; Pilnick, A. Analysis of pharmacist–patient communication using the Calgary-Cambridge guide. Patient Educ. Couns. 2011, 83, 423–431. [Google Scholar] [CrossRef] [PubMed]
- Mintz, D.L. Psychodynamic Psychopharmacology: Caring for the Treatment-Resistant Patient; American Psychiatric Association Publishing: Washington, DC, USA, 2022. [Google Scholar]
- Brower, V. Mind–body research moves towards the mainstream. EMBO Rep. 2006, 7, 358–361. [Google Scholar] [CrossRef]
- John, M. From Osler to the cone technique. HSR Proc. Intensive Care Cardiovasc. Anesth. 2013, 5, 57–58. [Google Scholar] [PubMed]
- Sabaté, E. (Ed.) Adherence to Long-Term Therapies: Evidence for Action; World Health Organization: Geneva, Switzerland, 2003. [Google Scholar]
- Cruz, M.; Roter, D.L.; Cruz, R.F.; Wieland, M.; Larson, S.; Cooper, L.A.; Pincus, H.A. Appointment length, psychiatrists’ communication behaviors and medication management appointment adherence. Psychiatr. Serv. 2013, 64, 886–892. [Google Scholar]
- Scott, I.A. Errors in clinical reasoning: Causes and remedial strategies. BMJ 2009, 338, b1860. [Google Scholar]
- Delga, C.; Megnin, Y.; Oustric, S.; Laurent, C.; Pauly, L.; Vergez, J.-P.; Charlet, J.-P.; Montastruc, J.-L.; Arlet, P. A pilot study in general practice: Pressure to prescribe. Therapie 2003, 58, 513–517. [Google Scholar] [PubMed]
- NHS England. Liberating the NHS: No Decision about Me, without Me. 2012. Available online: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/216980/Liberating-the-NHS-No-decision-about-me-without-me-Government-response.pdf (accessed on 2 November 2022).
- Von Peter, S.; Aderhold, V.; Cubellis, L.; Bergström, T.; Stastny, P.; Seikkula, J.; Puras, D. Open Dialogue as a Human Rights-Aligned Approach. Front. Psychiatry 2019, 10, 00387. [Google Scholar] [CrossRef]
- Bergström, T.; Seikkula, J.; Alakare, B.; Mäki, P.; Köngäs-Saviaro, P.; Taskila, J.J.; Tolvanen, A.; Aaltonen, J. The family-oriented open dialogue approach in the treatment of first-episode psychosis: Nineteen–year outcomes. Psychiatry Res. 2018, 270, 168–175. [Google Scholar] [CrossRef] [Green Version]
- Seikkula, J.; Alakare, B.; Aalotonen, J.; Holma, J.; Rasinkangas, A.; Lehtinen, V. Open Dialogue approach: Treatment principles and preliminary results of a two-year follow-up on first episode schizophrenia. Ethical Hum. Sci. Serv. 2003, 5, 163–182. [Google Scholar]
- Pilling, S.; Clarke, K.; Parker, G.; James, K.; Landau, S.; Weaver, T.; Razzaque, R.; Craig, T. Open Dialogue compared to treatment as usual for adults experiencing a mental health crisis: Protocol for the ODDESSI multi-site cluster randomised controlled trial. Contemp. Clin. Trials 2022, 113, 106664. [Google Scholar] [CrossRef]
- Razzaque, R.; Stockmann, T. An introduction to peer-supported open dialogue in mental healthcare. BJPsych Adv. 2016, 22, 348–356. [Google Scholar] [CrossRef] [Green Version]
- NHS England. Shared Decision Making Summary Guide; NHS: London, UK, 2019. Available online: https://www.england.nhs.uk/publication/shared-decision-making-summary-guide/ (accessed on 2 November 2022).
- World Health Organization (WHO). Guidance on Community Mental Health Services: Promoting Person-Centered and Rights-Based Approaches. 2021. Available online: https://www.who.int/publications/i/item/9789240025707 (accessed on 2 November 2022).
- Centre for Pharmacy Postgraduate Education. Consultation Skills for Pharmacy Practice: Taking a Patient-Centered Approach; CPPE: Manchester, UK, 2014. [Google Scholar]
- Barnett, N.L.; Oboh, L.; Smith, K. Patient-centred management of polypharmacy: A process for practice. Eur. J. Hosp. Pharm. 2016, 23, 113–117. [Google Scholar] [CrossRef] [PubMed]
- NHS England. Good for You, Good for Us, Good for Everybody. A Plan to Reduce Overprescribing to Make Patient Care Better and Safer, Support the NHS, and Reduce Carbon Emissions; NHS: London, UK, 2021. Available online: https://www.gov.uk/government/publications/national-overprescribing-review-report (accessed on 2 November 2022).
- Pharmaceutical Services Negotiating Committee. Pharmacies in England Provide 65 Million Consultations a Year, 26th June 2022. Available online: https://psnc.org.uk/our-news/pharmacies-in-england-provide-65-million-consultations-a-year/ (accessed on 9 March 2022).
- Barnett, N.; Minshull, J.; Shah, N.; Easthall, C. Feasibility of using CollaboRATE to evaluate pharmacist-led medicines-related consultations in UK hospitals: A pilot study. Eur. J. Hosp. Pharm. 2021, 28, 170–172. [Google Scholar]
- Tan, E.C.; Stewart, K.; Elliott, R.A.; George, J. Pharmacist consultations in general practice clinics: The Pharmacists in Practice Study (PIPS). Res. Soc. Adm. Pharm. 2014, 10, 623–632. [Google Scholar] [CrossRef]
- Barnett, N.; Jubraj, B.; White, D. Supporting professional self-care for PCN pharmacists. Prescriber 2021, 32, 13–16. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rogalski, D.; Barnett, N.; Bueno de Mesquita, A.; Jubraj, B. The Pharmacist Prescriber: A Psychological Perspective on Complex Conversations about Medicines: Introducing Relational Prescribing and Open Dialogue in Physical Health. Pharmacy 2023, 11, 62. https://doi.org/10.3390/pharmacy11020062
Rogalski D, Barnett N, Bueno de Mesquita A, Jubraj B. The Pharmacist Prescriber: A Psychological Perspective on Complex Conversations about Medicines: Introducing Relational Prescribing and Open Dialogue in Physical Health. Pharmacy. 2023; 11(2):62. https://doi.org/10.3390/pharmacy11020062
Chicago/Turabian StyleRogalski, David, Nina Barnett, Amanda Bueno de Mesquita, and Barry Jubraj. 2023. "The Pharmacist Prescriber: A Psychological Perspective on Complex Conversations about Medicines: Introducing Relational Prescribing and Open Dialogue in Physical Health" Pharmacy 11, no. 2: 62. https://doi.org/10.3390/pharmacy11020062
APA StyleRogalski, D., Barnett, N., Bueno de Mesquita, A., & Jubraj, B. (2023). The Pharmacist Prescriber: A Psychological Perspective on Complex Conversations about Medicines: Introducing Relational Prescribing and Open Dialogue in Physical Health. Pharmacy, 11(2), 62. https://doi.org/10.3390/pharmacy11020062





