Development and Evaluation of Interprofessional High-Fidelity Simulation Course on Medication Therapy Consultation for German Pharmacy and Medical Students—A Randomized Controlled Study
Abstract
1. Introduction
2. Materials and Methods
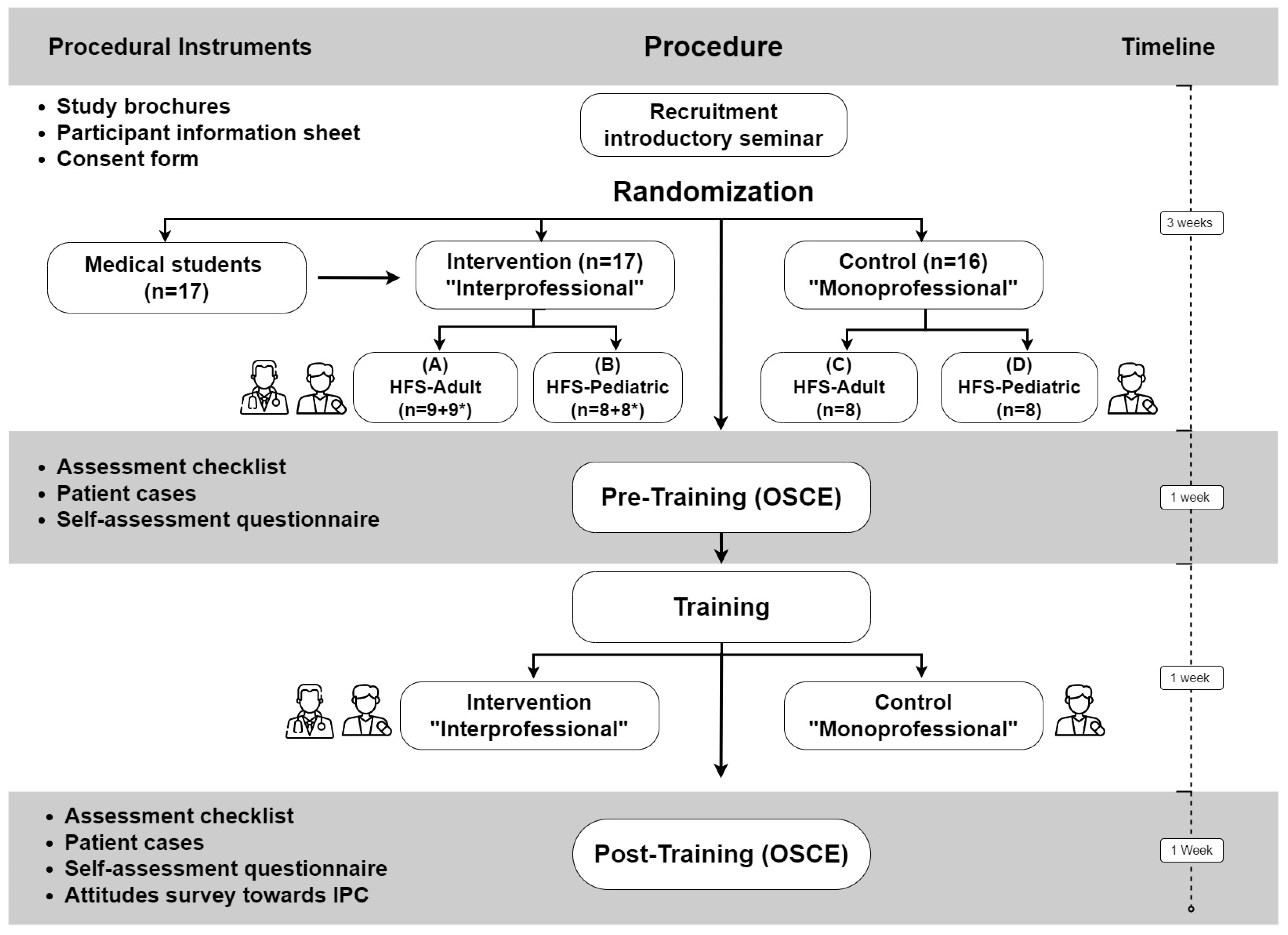
2.1. Study Design and Randomization Procedure
2.2. Study Procedure
2.3. Objective Structured Clinical Examination
2.4. Training Sessions
2.5. Instruments
2.5.1. High-Fidelity Simulators
2.5.2. Nordic RecMobile System
2.5.3. Medicheck
2.5.4. Cases for OSCEs
2.5.5. Assessment Checklist
2.5.6. Self-Assessment Questionnaire
2.5.7. Attitudes Survey toward Interprofessional Learning
2.6. Statistical Methods
3. Results
3.1. Participant Characteristics
3.2. Checklist Scores for OSCEs
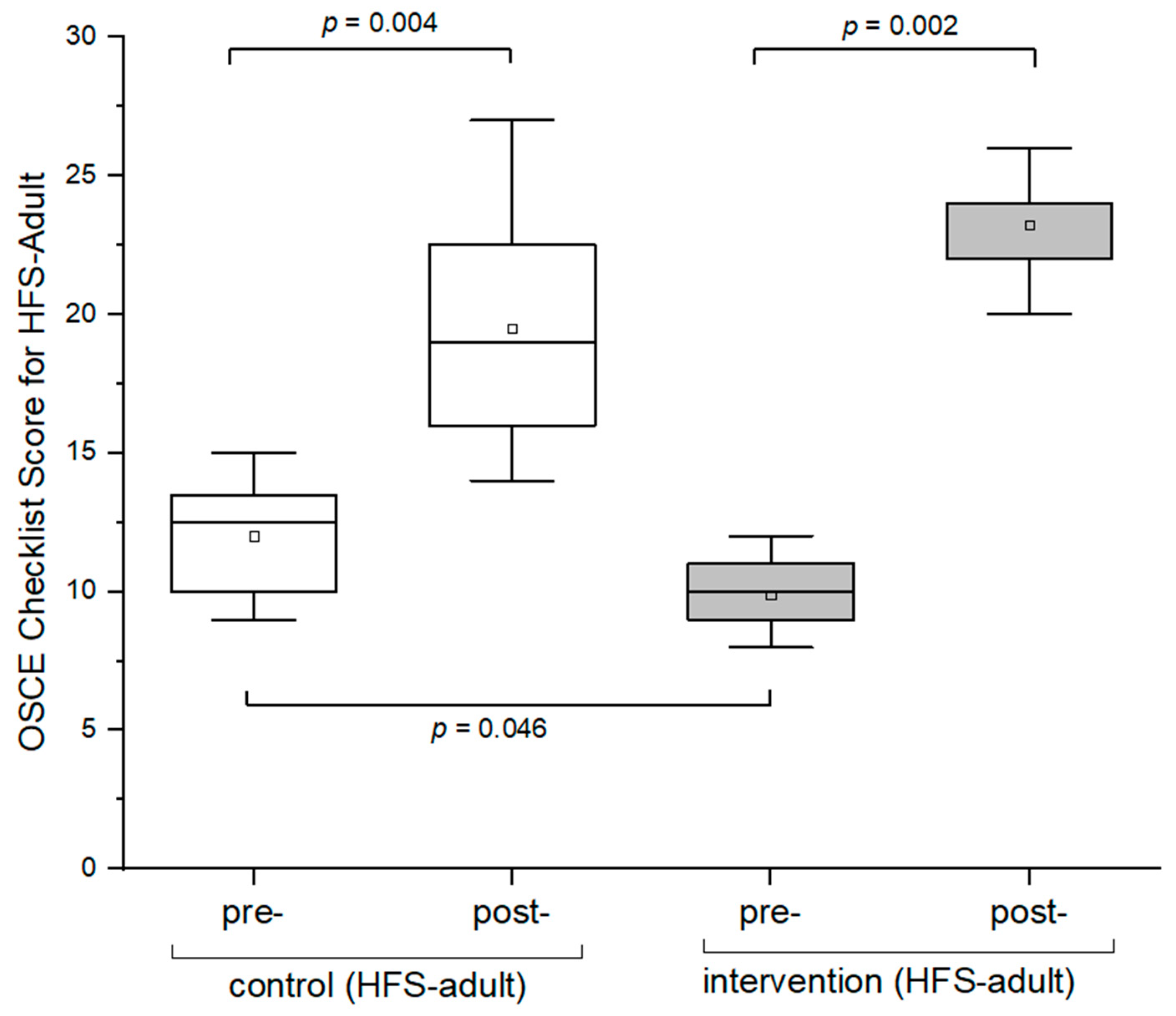
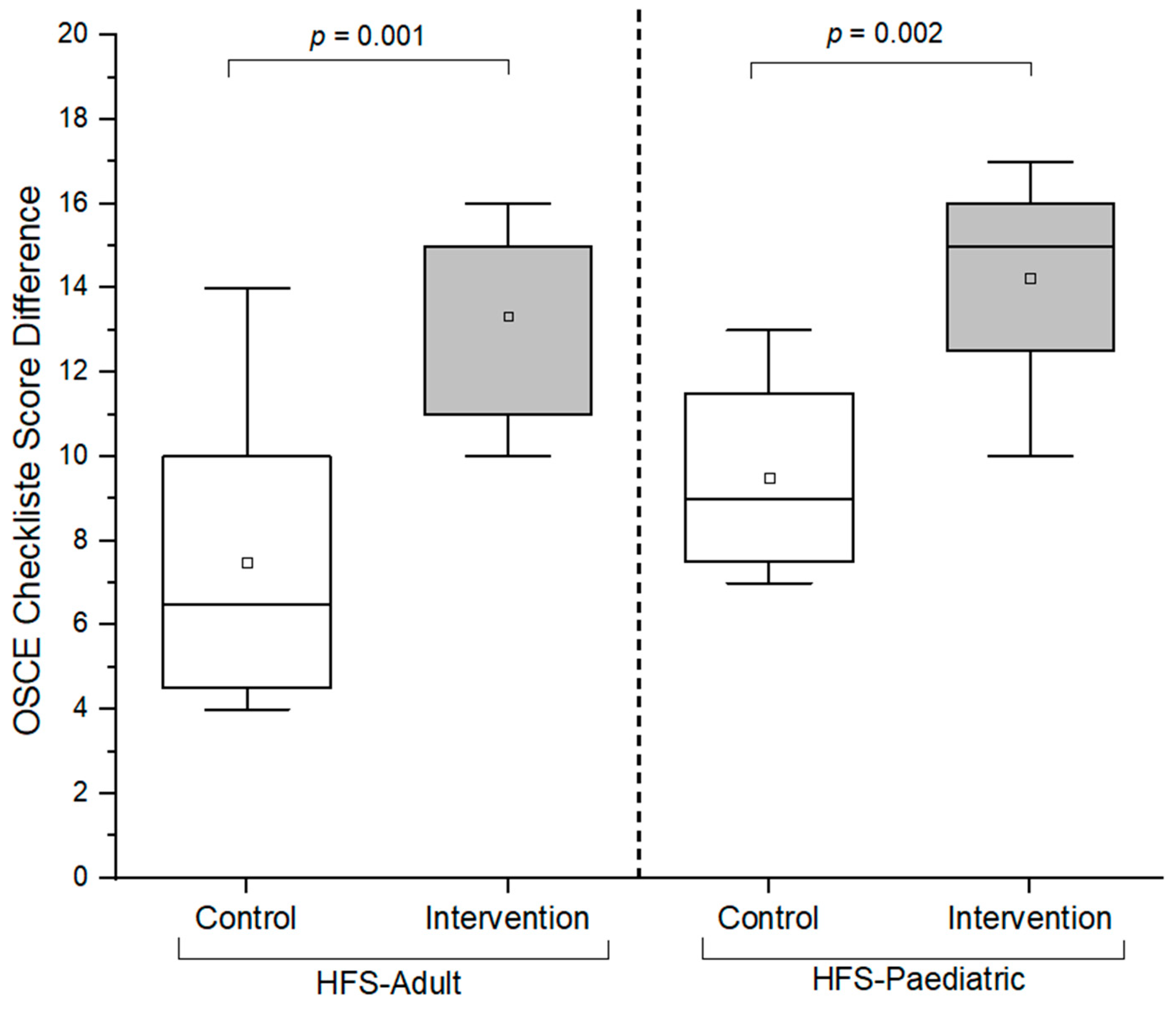
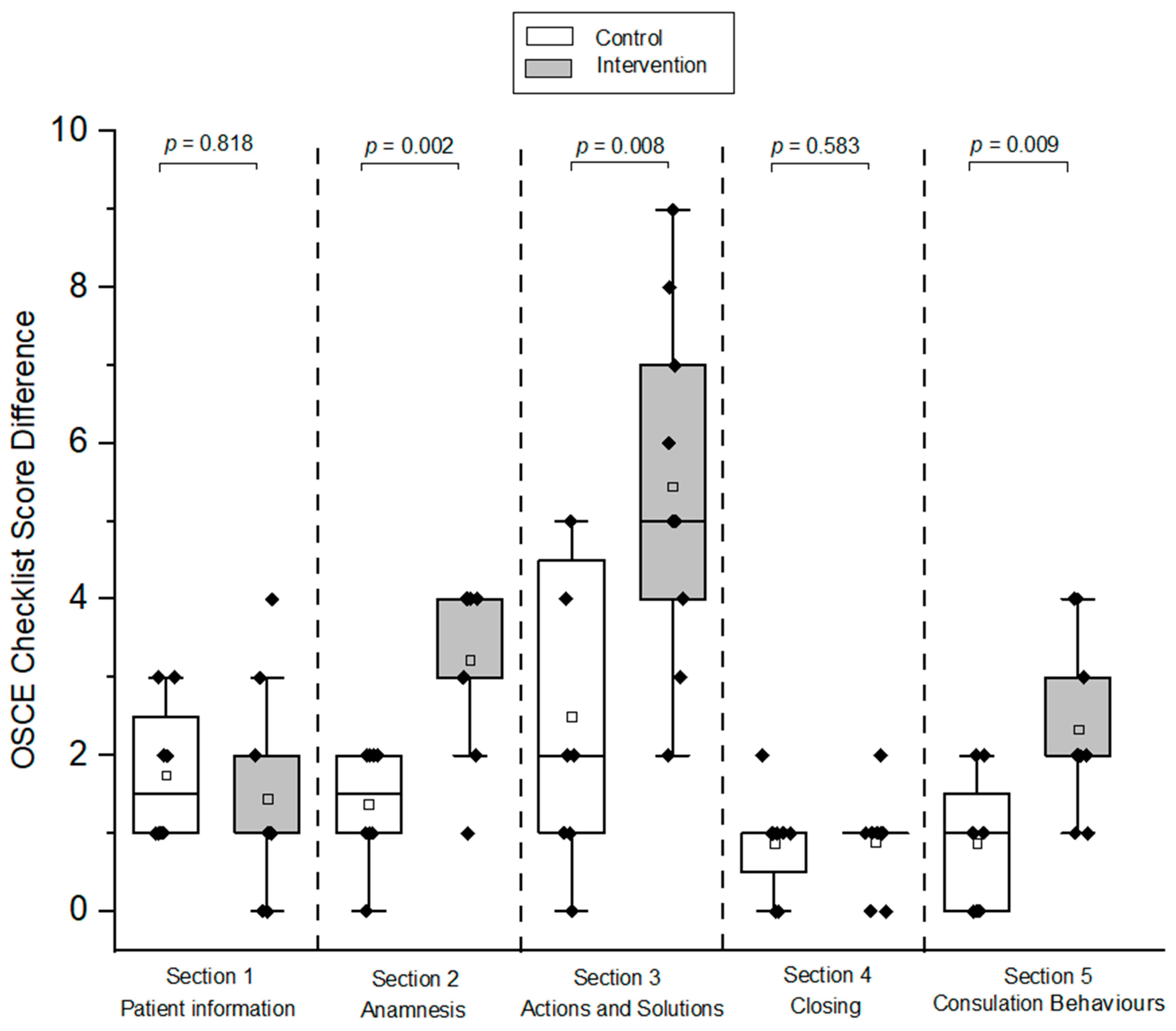
3.2.1. Checklist Scores Control and Intervention Groups (HFS-Adult)
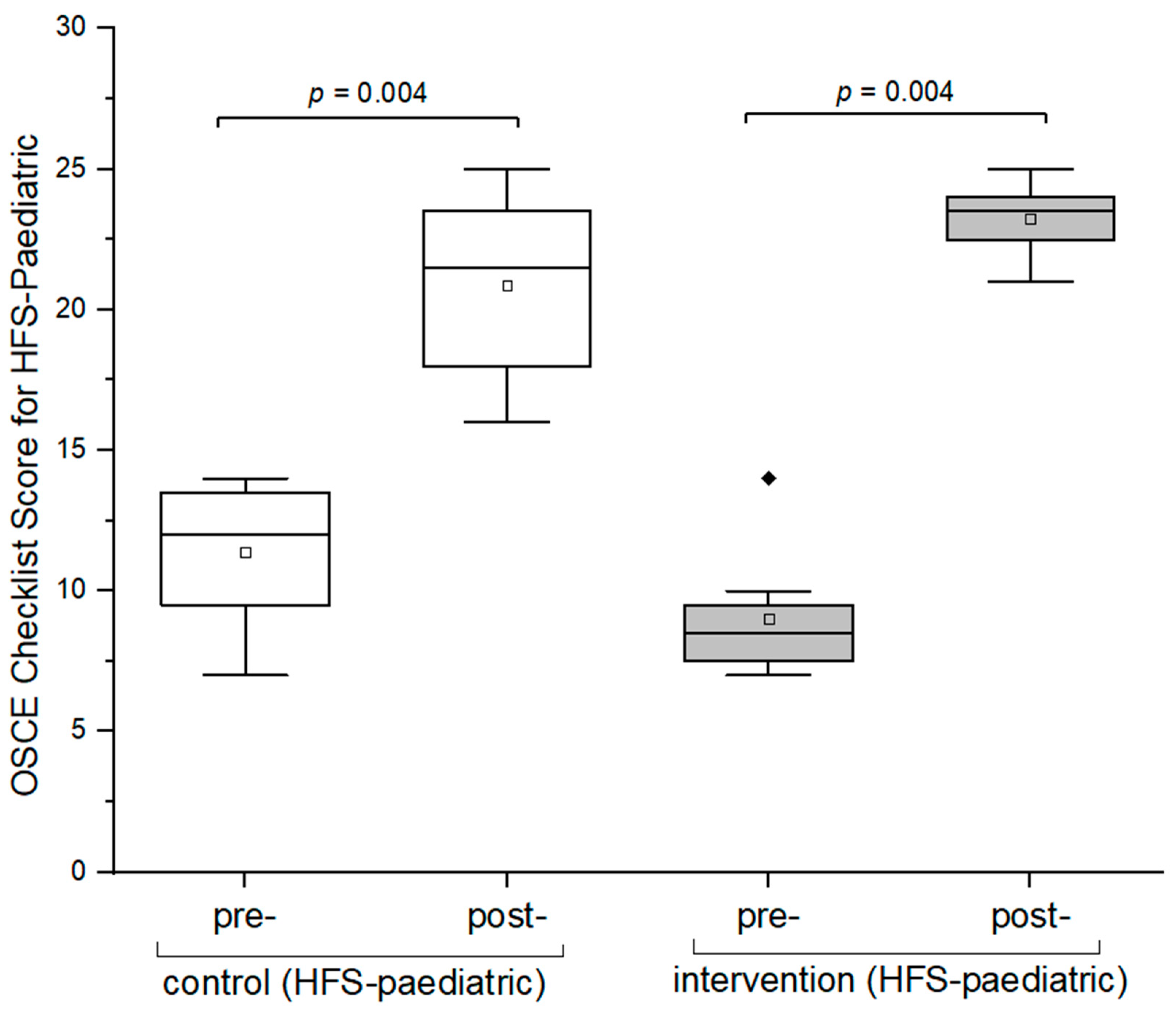
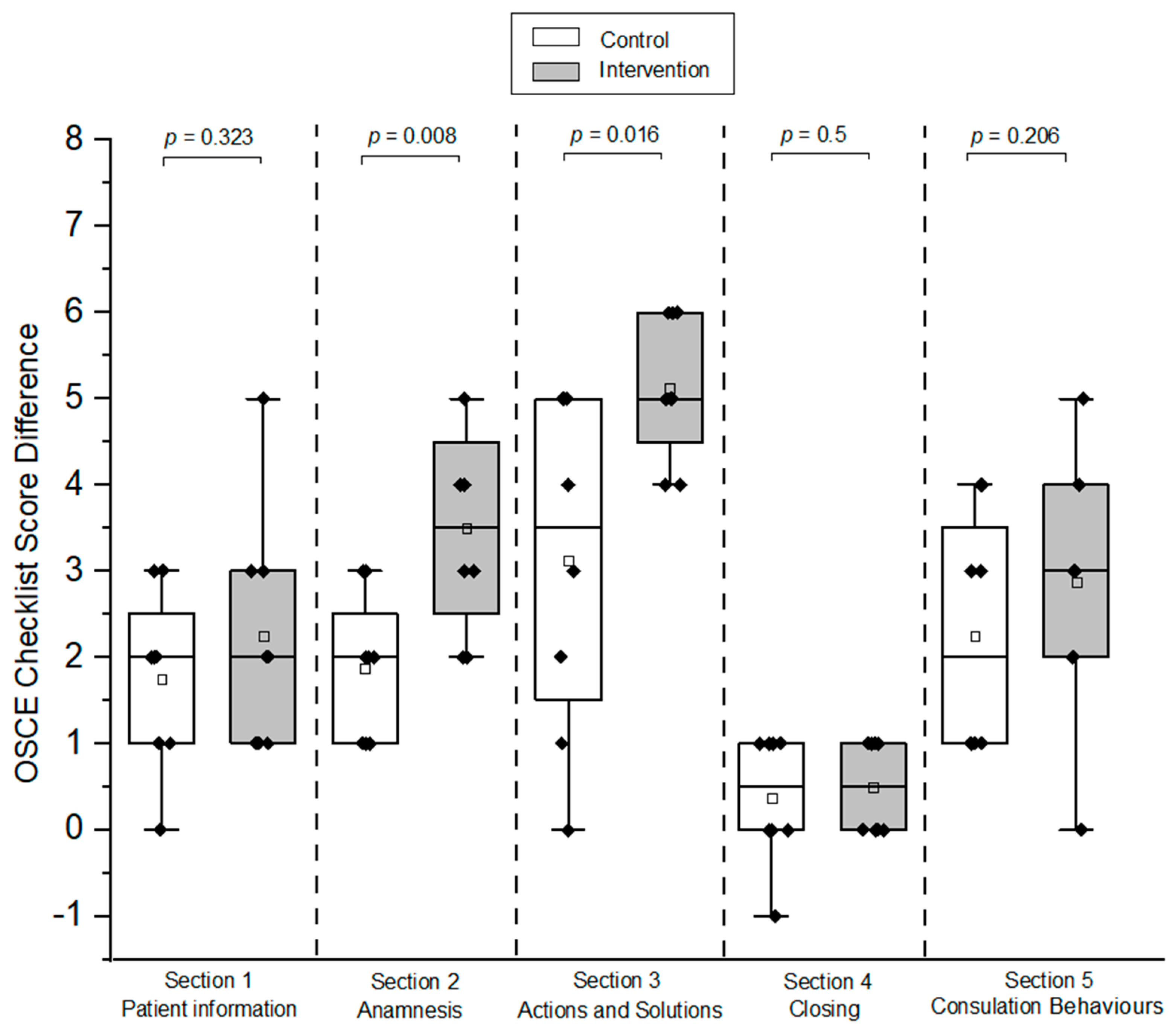
3.2.2. Checklist Scores Control and Intervention Groups (HFS-Pediatric)
4. Self-Assessment Questionnaire
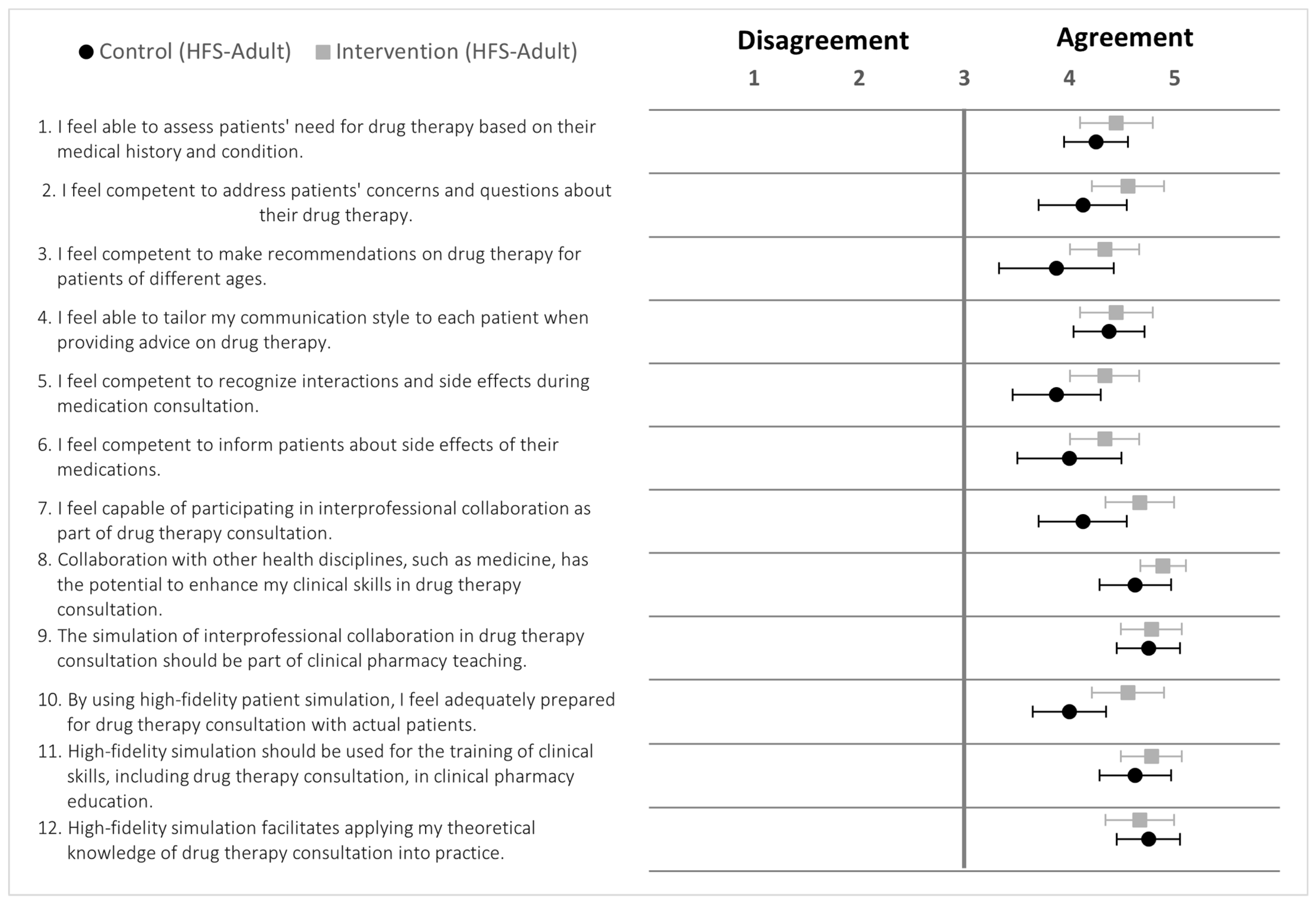
4.1. Intervention and Control Groups (HFS-Adult)
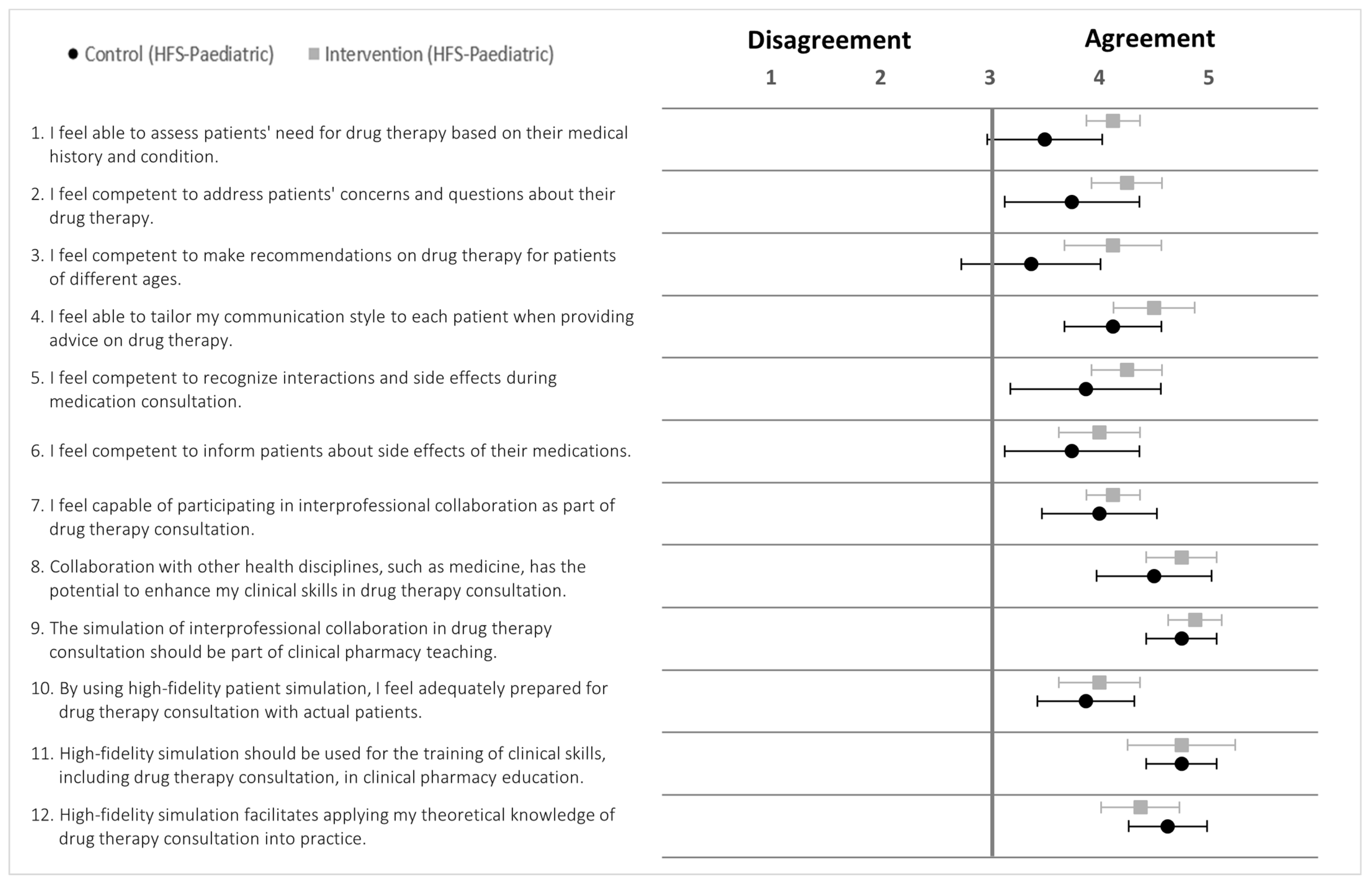
4.2. Intervention and Control Groups (HFS-Paediatric)
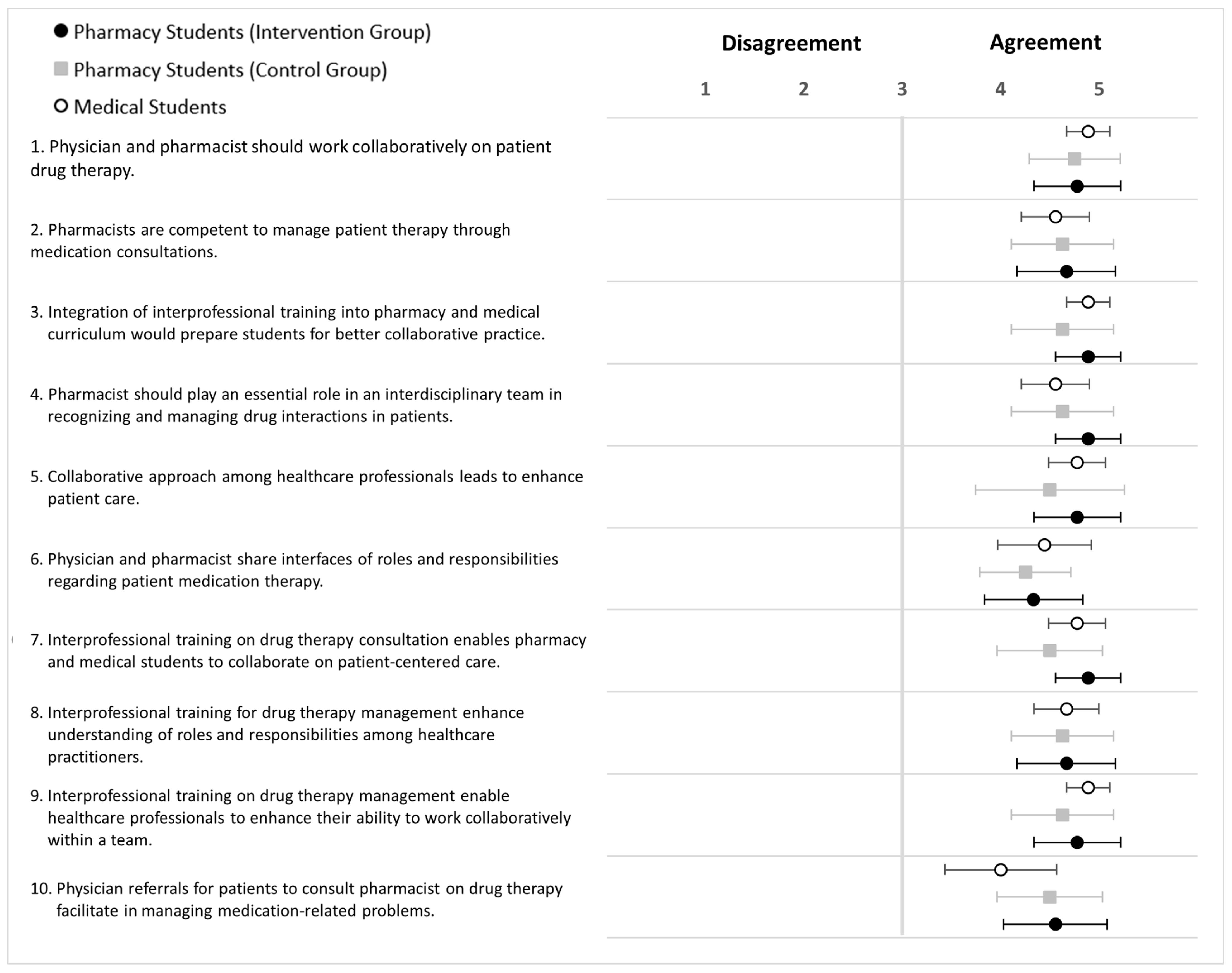
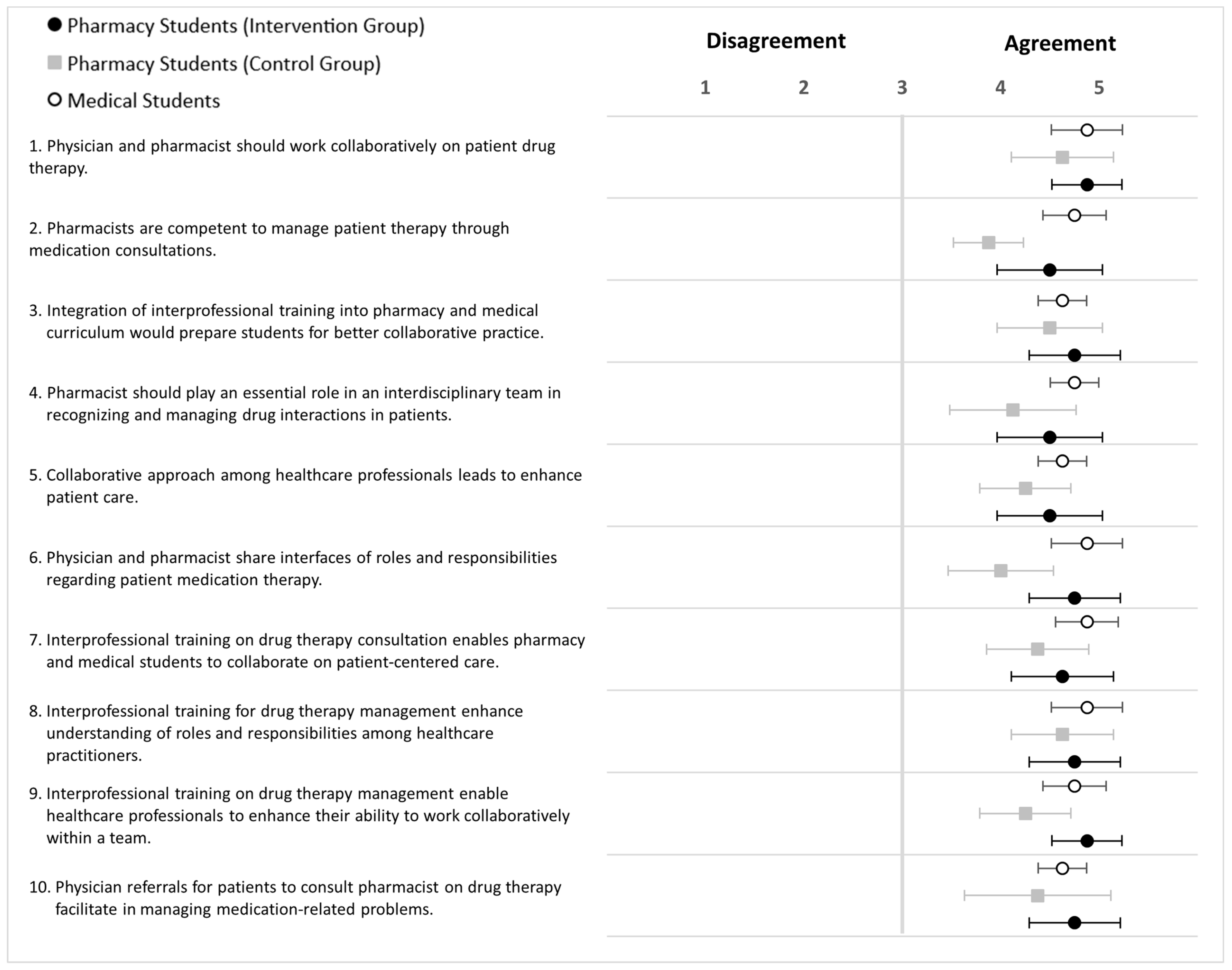
5. Attitude Survey toward Interprofessional Collaboration
5.1. Intervention and Control Groups (HFS-Adult)
5.2. Intervention and Control Groups (HFS-Paediatric)
6. Discussion
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. OSCE Checklist
 | OSCE Checklist |  | ||
| Participant code: | Date: | |||
| Comments | |||
| A.1 The participant introduces him/herself to the patient by name and role. | ||||
| A2 Confirms patient’s identity (name, date of birth) | ||||
| A2.1 The participant asks the patient to provide his/her surname and first name. | ||||
| A2.2 The participant asks the patient to provide his/her date of birth to ensure accurate identification. | ||||
| A3 Discusses the purpose of the consultation. | ||||
| A3.1 The participant explains the purpose of the drug therapy consultation to the patient. | ||||
| A3.2 The participant gains the patient’s consent to proceed with the drug therapy consultation. | ||||
| Comments | |||
| B1 History of Present Illness | ||||
| B1.1 The participant asks for further information about the patient’s main concern. | ||||
| B1.2 The participant asks for further information about the timing of the symptoms (onset and duration). | ||||
| B1.3 The participant asks about any associated symptoms that the patient has noticed. | ||||
| B1.4 The participant assesses the patient’s adherence to current medications. | ||||
| B1.5 The participant asks about any prescribed or over-the-counter medications that the patient is currently taking, which may not be listed in the patient sheet. | ||||
| B2 Lab Values/Vital signs Interpretation | ||||
| B2.1 The participant assesses any abnormal lab values that may indicate risk. | ||||
| B2.2 The participant assesses the patient’s vital signs. | ||||
| B3 Personal and Social History (the participant asks for further information about only one point depending on the OSCE case, other points are mentioned in the patient information sheet) | ||||
| B3.1 ask for information about tobacco. | ||||
| B3.2 ask for information about Alcohol. | ||||
| B3.3 ask for information about usual dietary practices. | ||||
| B3.4 ask for information about current physical activity. | ||||
| B3.5 ask for information about trafficability. | ||||
| Comments | |||
| C1 Drug Interactions and Side Effects | ||||
| C1.1 The participant identifies possible drug–drug interactions in the patient’s medications. | ||||
| C1.2 The participant provides optimization recommendations to possible drug–drug interactions related to point C1.1. | ||||
| C1.3 The participant recognises possible drug-related problem. | ||||
| C1.4 The participant explains the reasons for occurrence of the drug-related problem related to point C1.3. | ||||
| C1.5 The participant provides optimisation recommendations related to point C1.3. | ||||
| C2 Administration Timing/Technique and Side Effects: | ||||
| C2.1 The participant asks about the patient’s understanding of the appropriate administration timing or technique for a particular medication. | ||||
| C2.2 The participant recognises inappropriate administration timing or technique related to point C2.1. | ||||
| C2.3 The participant explains the reasons for the side effects that occurred due the identified inappropriate administration timing/technique. | ||||
| C2.4 The participant provides optimisation recommendations related to inappropriate timing or technique related to point C2.1. | ||||
| C2.5 The participant provides further recommendations related to administration timing/technique depend on each case. | ||||
| Comments | |||
| D.1 The participant instructs the patient to report his/her medications (including over-the-counter products/food supplements) to the physician. | ||||
| D.2 The participant provides opportunity to the patient to ask any further questions. | ||||
| D3. The participant expresses gratitude for the patient’s collaboration and asks the patient to follow up. | ||||
| Comments | |||
| E.1 The participant listens actively and allows the patient to complete statements. | ||||
| E.2 The participant uses open and closed questions when appropriate. | ||||
| E.3 The participant responds effectively to the patient’s questions and concerns in informative and reassuring way. | ||||
| E.4 The participant shows support and respond to the patient’s feelings (angry/frustrated) and needs. | ||||
| E.5 The participant avoids scientific words (unnecessary jargon) and explain medical concepts in patient-friendly terms. | ||||
| E.6 The participant demonstrates confidence during the consultation, avoiding moments of silence and confusion. | ||||
| E.7 The participant maintains control over the drug therapy consultation and avoids irrelevant discussions. | ||||
| E.8 The participant employs effective non-verbal communication including appropriate gestures and friendly facial expressions. | ||||
| E.9 The participant manages the OSCE time effectively and ensures that the drug therapy consultation remains within the designated time frame. | ||||
| Name of examiner: | Date: | |||
| Signature of examiner: | ||||
Appendix B
| HFS-Adult | HFS-Pediatric | |||
|---|---|---|---|---|
| Intervention Mean (SD) | Control Mean (SD) | Intervention Mean (SD) | Control Mean (SD) | |
| Section 1 | ||||
| Pre-OSCE Score | 0.44 (0.53) | 0.13 (0.35) | 1.00 (0.53) | 1.50 (0.53) |
| Post-OSCE Score | 1.89 (1.27) | 1.88 (0.83) | 3.25 (1.16) | 3.25 (0.71) |
| Score Difference | 1.44 (1.33) | 1.75 (0.89) | 2.25 (1.39) | 1.75 (1.04) |
| p-Value | 0.818 | 0.323 | ||
| Section 2 | ||||
| Pre-OSCE Score | 1.56 (0.73) | 2.00 (1.07) | 1.38 (1.19) | 2.25 (0.89) |
| Post-OSCE Score | 4.78 (0.97) | 3.38 (0.92) | 4.88 (0.83) | 4.13 (1.25) |
| Score Difference | 3.22 (1.09) | 1.38 (0.74) | 3.50 (1.20) | 1.88 (0.83) |
| p-Value | 0.002 | 0.008 | ||
| Section 3 | ||||
| Pre-OSCE Score | 1.00 (0.87) | 2.88 (1.13) | 1.00 (0.76) | 1.25 (1.04) |
| Post-OSCE Score | 6.44 (2.13) | 5.38 (2.07) | 6.13 (1.25) | 4.38 (1.51) |
| Score Difference | 5.44 (2.30) | 2.50 (1.93) | 5.13 (0.83) | 3.13 (1.96) |
| p-Value | 0.008 | 0.016 | ||
| Section 4 | ||||
| Pre-OSCE Score | 1.11 (0.60) | 0.75 (0.71) | 0.75 (0.46) | 1.00 (0.53) |
| Post-OSCE Score | 2.00 (0.71) | 1.63 (0.74) | 1.25 (0.46) | 1.38 (0.74) |
| Score Difference | 0.89 (0.60) | 0.88 (0.64) | 0.50 (0.53) | 0.38 (0.74) |
| p-Value | 0.583 | 0.5 | ||
| Section 5 | ||||
| Pre-OSCE Score | 5.78 (0.97) | 6.25 (1.04) | 4.88 (1.73) | 5.38 (1.41) |
| Post-OSCE Score | 8.11 (0.60) | 7.25 (1.49) | 7.75 (0.46) | 7.75 (0.46) |
| Score Difference | 2.33 (1.12) | 0.88 (0.83) | 2.88 (1.55) | 2.25 (1.39) |
| p-Value | 0.009 | 0.206 | ||
| Total | ||||
| Pre-OSCE Score | 9.89 (1.27) | 12.00 (2.20) | 9.00 (2.27) | 11.38 (2.56) |
| Post-OSCE Score | 23.22 (2.22) | 19.50 (4.41) | 23.25 (1.28) | 20.88 (3.27) |
| Score Difference | 13.33 (2.40) | 7.38 (3.29) | 14.25 (2.38) | 9.38 (2.20) |
| p-Value | 0.001 | 0.002 | ||
Appendix C
| Group | Pre-Training | Post-Training |
|---|---|---|
| Mean | Mean | |
| (CI) | (CI) | |
| Intervention | 41.22 | 54.78 |
| (n = 9) | (3.18) | (1.38) |
| Control | 46.38 | 51.38 |
| (n = 8) | (3.68) | (2.77) |
| Group | Pre-Training | Post-Training |
|---|---|---|
| Mean | Mean | |
| (CI) | (CI) | |
| Intervention | 43.38 | 52.13 |
| (n = 8) | (2.64) | (2.38) |
| Control | 40.63 | 48.88 |
| (n = 8) | (3.87) | (3.00) |
| Group | Intervention (Pharmacy Students) (n = 9) | Intervention (Medical Students) (n = 9) | Control (Pharmacy Students) (n = 8) |
|---|---|---|---|
| Mean | 47.22 | 46.44 | 45.63 |
| (CI) | (1.75) | (1.39) | (2.09) |
| Group | Intervention (Pharmacy Students) (n = 8) | Intervention (Medical Students) (n = 8) | Control (Pharmacy Students) (n = 8) |
|---|---|---|---|
| Mean | 47.00 | 48.00 | 43.38 |
| (CI) | (2.19) | (1.57) | (2.67) |
References
- Interprofessional Education Collaborative. IPEC Core Competencies for Interprofessional Collaborative Practice: Version 3; Interprofessional Education Collaborative: Washington, DC, USA, 2023. [Google Scholar]
- Romme, S.; Bosveld, M.H.; Van Bokhoven, M.A.; De Nooijer, J.; Van den Besselaar, H.; Van Dongen, J.J. Patient involvement in interprofessional education: A qualitative study yielding recommendations on incorporating the patient’s perspective. Health Expect. 2020, 23, 943–957. Available online: https://pubmed.ncbi.nlm.nih.gov/32496648/ (accessed on 8 May 2024). [CrossRef]
- Monkeytree Creative Inc. Framework for Action on Interprofessional Education & Collaborative Practice Health Professions Networks Nursing & Midwifery Human Resources for Health; WHO Press: Geneva, Switzerland, 2010; Available online: https://iris.who.int/bitstream/handle/10665/70185/WHO_HRH_HPN_10.3_eng.pdf (accessed on 8 May 2024).
- Albassam, A.; Almohammed, H.; Alhujaili, M.; Koshy, S.; Awad, A. Perspectives of primary care physicians and pharmacists on interprofessional collaboration in Kuwait: A quantitative study. PLoS ONE 2020, 15, e0236114. [Google Scholar] [CrossRef] [PubMed]
- Sudeshika, T.; Naunton, M.; Peterson, G.M.; Deeks, L.S.; Guénette, L.; Sharma, R.; Freeman, C.; Niyonsenga, T.; Kosari, S. Interprofessional Collaboration and Team Effectiveness of Pharmacists in General Practice: A Cross-National Survey. Int. J. Environ. Res. Public Health 2023, 20, 394. [Google Scholar] [CrossRef] [PubMed]
- Dahlke, S.; Hunter, K.F.; Reshef Kalogirou, M.; Negrin, K.; Fox, M.; Wagg, A. Perspectives about Interprofessional Collaboration and Patient-Centred Care. Can. J. Aging 2020, 39, 443–455. Available online: https://www.cambridge.org/core/journals/canadian-journal-on-aging-la-revue-canadienne-du-vieillissement/article/perspectives-about-interprofessional-collaboration-and-patientcentred-care/E7F90B2F9FD39101379DE7A6CA538DA1 (accessed on 8 May 2024). [CrossRef] [PubMed]
- Breckner, A.; Glassen, K.; Schulze, J.; Lühmann, D.; Schaefer, I.; Szecsenyi, J.; Scherer, M.; Wensing, M. Original research: Experiences of patients with multimorbidity with primary care and the association with patient activation: A cross-sectional study in Germany. BMJ Open 2022, 12, 59100. [Google Scholar] [CrossRef]
- Gehrke-Beck, S.; Petersen, M.; Herrmann, W.J.; Zimmermann, N.; Daub, E.; Seeger, J.; Schulz, J.; Czimmeck, C.; Lauterbach, N.; Peters, H.; et al. Development of a project for interprofessional collaboration between medical and pharmacy students to improve medication safety in polypharmacy (PILLE). GMS J. Med. Educ. 2023, 40, Doc3. [Google Scholar]
- Stausberg, J.; Hasford, J. Drug-related admissions and hospital-acquired adverse drug events in Germany: A longitudinal analysis from 2003 to 2007 of ICD-10-coded routine data. BMC Health Serv. Res. 2011, 11, 134. [Google Scholar] [CrossRef]
- Abe, F. The Importance of Medication Management: Ensuring Safe and Effective Treatment. Int. Res. J. Pharm. Pharmacol. 2023, 11, 1–3. [Google Scholar]
- Waszyk-Nowaczyk, M.; Guzenda, W.; Kamasa, K.; Pawlak, K.; Bałtruszewicz, N.; Artyszuk, K.; Białoszewski, A.; Merks, P. Cooperation between Pharmacists and Physicians—Whether It Was before and is It Still Ongoing during the Pandemic? J. Multidiscip. Healthc. 2021, 14, 2101. [Google Scholar] [CrossRef]
- van Diggele, C.; Roberts, C.; Burgess, A.; Mellis, C. Interprofessional education: Tips for design and implementation. BMC Med. Educ. 2020, 20, 455. Available online: https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-020-02286-z (accessed on 8 May 2024). [CrossRef]
- Grymonpre, R.E.; Bainbridge, L.; Nasmith, L.; Baker, C. Development of accreditation standards for interprofessional education: A Canadian Case Study. Hum. Resour. Health 2021, 19, 12. Available online: https://human-resources-health.biomedcentral.com/articles/10.1186/s12960-020-00551-2 (accessed on 1 June 2024). [CrossRef] [PubMed]
- Walkenhorst, U.; Mahler, C.; Aistleithner, R.; Hahn, E.G.; Kaap-Fröhlich, S.; Karstens, S.; Reiber, K.; Stock-Schröer, B.; Sottas, B. Position statement GMA Comittee—“Interprofessional Education for the Health Care Professions”. GMS Z. Med. Ausbild. 2015, 32, Doc22. [Google Scholar] [PubMed]
- Kaap-Fröhlich, S.; Ulrich, G.; Wershofen, B.; Ahles, J.; Behrend, R.; Handgraaf, M.; Herinek, D.; Mitzkat, A.; Oberhauser, H.; Scherer, T.; et al. Position paper of the GMA Committee Interprofessional Education in the Health Professions—Current status and outlook. GMS J. Med. Educ. 2022, 39, Doc17. [Google Scholar]
- Depasquale, C.; Cunningham, S.; Jacob, S.A.; Boyter, A.; Portlock, J.; Power, A.; Addison, B. A cross-sectional study examining the nature and extent of interprofessional education in schools of pharmacy in the United Kingdom. Int. J. Clin. Pharm. 2024, 46, 122–130. [Google Scholar] [CrossRef]
- Patel, N.; Begum, S.; Kayyali, R. Interprofessional Education (IPE) and Pharmacy in the UK. A study on IPE Activities across Different Schools of Pharmacy. Pharmacy 2016, 4, 28. [Google Scholar] [CrossRef]
- Machado, A.C.; Czock, A.; Boone, J.; Anderson, C.; Leite, S.N. How interprofessional education is offered to pharmacists and pharmacy students: A scoping review. J. Interprof. Educ. Pract. 2022, 29, 100563. [Google Scholar] [CrossRef]
- Shah, K.R.; McKeefer, H.J.M.; Wieters, M.D.; Babalola, R.O.; Hodge, C.K. Stop, collaborate, and listen: Encouraging interprofessional education through critical care simulations for pharmacy students. J. Am. Coll. Clin. Pharm. 2023, 6, 918–924. Available online: https://onlinelibrary.wiley.com/doi/full/10.1002/jac5.1826 (accessed on 8 May 2024). [CrossRef]
- Madden, M.; Stewart, D.; Mills, T.; McCambridge, J. Original research: Consultation skills development in general practice: Findings from a qualitative study of newly recruited and more experienced clinical pharmacists during the COVID-19 pandemic. BMJ Open 2023, 13, 69017. [Google Scholar] [CrossRef]
- Green, B.N.; Johnson, C.D. Interprofessional collaboration in research, education, and clinical practice: Working together for a better future. J. Chiropr. Educ. 2015, 29, 1–10. [Google Scholar] [CrossRef]
- El-Awaisi, A.; Wilby, K.J.; Wilbur, K.; El Hajj, M.S.; Awaisu, A.; Paravattil, B. A Middle Eastern journey of integrating Interprofessional Education into the healthcare curriculum: A SWOC analysis. BMC Med. Educ. 2017, 17, 15. Available online: https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-016-0852-5 (accessed on 8 May 2024). [CrossRef]
- Wilbur, K.; Pelletier, T. Training for Collaborative Care: How Hospital Team Members View Pharmacy Students. Can. J. Hosp. Pharm. 2023, 76, 228. [Google Scholar] [CrossRef]
- Schuster, B.G.; Faisal, S.; Gagnon, C.L. A new curricular framework for an interprofessional approach to deprescribing: Why and how pharmacists should lead the way. Can. Pharm. J. 2024, 157, 101–103. Available online: https://orcid.org/0009-0006-2456-9594 (accessed on 8 August 2024). [CrossRef] [PubMed]
- Abdelhakim, H.E.; Brown, L.; Mills, L.; Ahmad, A.; Hammell, J.; McKechnie, D.G.; Ng, T.W.; Lever, R.; Whittlesea, C.; Rosenthal, J.; et al. Medical and pharmacy students’ perspectives of remote synchronous interprofessional education sessions. BMC Med. Educ. 2022, 22, 611. Available online: https://bmcmededuc.biomedcentral.com/articles/10.1186/s12909-022-03675-2 (accessed on 8 May 2024). [CrossRef] [PubMed]
- Nock, L. Interprofessional teaching and learning in the health care professions: A qualitative evaluation of the Robert Bosch Foundation’s grant program “Operation Team”. GMS J. Med. Educ. 2016, 33, Doc16. [Google Scholar]
- Verordnung zur Neuregelung der Ärztlichen Ausbildung. Available online: https://www.bundesgesundheitsministerium.de/service/gesetze-und-verordnungen/detail/verordnung-zur-neuregelung-der-aerztlichen-ausbildung.html (accessed on 8 May 2024).
- Nachwuchs Macht Sich für Interprofessionalität Stark. Available online: https://www.pharmazeutische-zeitung.de/nachwuchs-macht-sich-fuer-interprofessionalitaet-stark-136732/ (accessed on 8 May 2024).
- Klinikum Braunschweig, Apothekerkammer Niedersachsen und TU Braunschweig: PJ-Akademie—Interdisziplinäres Pilotprojekt in Braunschweig. Available online: https://www.deutsche-apotheker-zeitung.de/news/artikel/2023/09/08/pj-akademie-interdisziplinaeres-pilotprojekt-in-braunschweig (accessed on 9 May 2024).
- Bode, S.; Dürkop, A.; Wilcken, H.; Peters, S.; Straub, C. Interprofessional learning during SARS-CoV-2 (COVID-19) pandemic conditions: The learning project I-reCovEr as a substitute for a rotation on an interprofessional training ward. GMS J. Med. Educ. 2021, 38, Doc13. [Google Scholar] [PubMed]
- Rose, O.; Happe, S.; Huchtemann, T.; Mönig, C.; Ohms, M.; Schwalbe, O.; Warnecke, T.; Erzkamp, S. Enhancing medication therapy in Parkinson’s disease by establishing an interprofessional network including pharmacists. Int. J. Clin. Pharm. 2021, 43, 441–448. [Google Scholar] [CrossRef]
- Dähne, A.; Costa, D.; Krass, I.; Ritter, C.A. General practitioner—Pharmacist collaboration in Germany: An explanatory model. Int. J. Clin. Pharm. 2019, 41, 939–949. [Google Scholar] [CrossRef]
- Lash, D.B.; Barnett, M.J.; Parekh, N.; Shieh, A.; Louie, M.C.; Tang, T.T.L. Perceived Benefits and Challenges of Interprofessional Education Based on a Multidisciplinary Faculty Member Survey. Am. J. Pharm. Educ. 2014, 78, 180. [Google Scholar] [CrossRef]
- West, C.; Graham, L.; Palmer, R.T.; Miller, M.F.; Thayer, E.K.; Stuber, M.L.; Awdishu, L.; Umoren, R.A.; Wamsley, M.A.; Nelson, E.A.; et al. Implementation of interprofessional education (IPE) in 16 U.S. medical schools: Common practices, barriers and facilitators. J. Interprof. Educ. Pract. 2016, 4, 41–49. Available online: https://pubmed.ncbi.nlm.nih.gov/28184380/ (accessed on 8 May 2024). [CrossRef]
- Lin, K.; Travlos, D.V.; Wadelin, J.W.; Vlasses, P.H. Simulation and Introductory Pharmacy Practice Experiences. Am. J. Pharm. Educ. 2011, 75, 209. [Google Scholar] [CrossRef]
- Davis, A.H.; Goumas, A.L.; Hebert, C.M.; Levitzky, E.; McLean, A.M.; Rusnak, S.; Gunaldo, T.P. The transfer of interprofessional learning to the clinical environment following a high-fidelity simulation experience in undergraduate nursing and medical students: A curricular resource. J. Interprof. Educ. Pract. 2022, 29, 100544. [Google Scholar] [CrossRef]
- Chen, H.W.; O’Donnell, J.M.; Chiu, Y.J.; Chen, Y.C.; Kang, Y.N.; Tuan, Y.T.; Kuo, S.Y.; Wu, J.C. Comparison of learning outcomes of interprofessional education simulation with traditional single-profession education simulation: A mixed-methods study. BMC Med. Educ. 2022, 22, 651. [Google Scholar] [CrossRef]
- Bolesta, S.; Chmil, J.V. Interprofessional Education Among Student Health Professionals Using Human Patient Simulation. Am. J. Pharm. Educ. 2014, 78, 94. [Google Scholar] [CrossRef] [PubMed]
- Kelsch, M.P.; Brynjulson, R.; Hursman, A.; Werremeyer, A.; Eukel, H.N. Impact of an Emergency Department Simulation on Pharmacy Students’ Interprofessional Team Skills and Attitudes. Innov. Pharm. 2022, 13, 1. [Google Scholar] [CrossRef] [PubMed]
- Korayem, G.B.; Alshaya, O.A.; Kurdi, S.M.; Alnajjar, L.I.; Badr, A.F.; Alfahed, A.; Cluntun, A. Simulation-Based Education Implementation in Pharmacy Curriculum: A Review of the Current Status. Adv. Med. Educ. Pract. 2022, 13, 649. [Google Scholar] [CrossRef] [PubMed]
- Zabar, S.; Adams, J.; Kurland, S.; Shaker-Brown, A.; Porter, B.; Horlick, M.; Hanley, K.; Altshuler, L.; Kalet, A.; Gillespie, C. Charting a Key Competency Domain: Understanding Resident Physician Interprofessional Collaboration (IPC) Skills. J. Gen. Intern. Med. 2016, 31, 846. [Google Scholar] [CrossRef]
- Keshmiri, F.; Najarkolai, A.R.; Motlagh, M.K.; Saljoughi, N. Inter-Professional Team Objective Structured Clinical Examination (ITOSCE): Teaching and Assessment Strategies of the Inter Professional Approach. Bali Med. J. 2016, 5, 111. [Google Scholar] [CrossRef][Green Version]
- Laven, A.; Deters, M.A.; Rose, O.; Schwender, H.; Smaranda, A.; Waltering, I.; Laeer, S. PharmAdhere: Training German community pharmacists with Objective Structured Clinical Examinations. Int. J. Clin. Pharm. 2018, 40, 1317–1327. Available online: https://link.springer.com/article/10.1007/s11096-018-0710-0 (accessed on 9 May 2024). [CrossRef]
- Dyess, A.L.; Brown, J.S.; Brown, N.D.; Flautt, K.M.; Barnes, L.J. Impact of interprofessional education on students of the health professions: A systematic review. J. Educ. Eval. Health Prof. 2019, 16, 33. [Google Scholar] [CrossRef]
- Mitzel, K.; Storjohann, T.; Herrick, A.; Davis, L.; Shamblen, C.; Bonnin, K. Interprofessional objective structured clinical examination with physician assistant and pharmacy students—A qualitative and quantitative study. Curr. Pharm. Teach. Learn. 2020, 12, 174–180. [Google Scholar] [CrossRef]
- Dabaghzadeh, F.; Zihayat, B.; Sarafzadeh, F. Influence of pharmacy students on the attitudes of medical students following an interprofessional course. Educ. Health Chang. Learn. Pract. 2017, 30, 103–107. [Google Scholar] [CrossRef] [PubMed]
- Curley, L.E.; Jensen, M.; McNabb, C.; Ram, S.; Torrie, J.; Jowsey, T.; McDonald, M. Pharmacy Students’ Perspectives on Interprofessional Learning in a Simulated Patient Care Ward Environment. Am. J. Pharm. Educ. 2019, 83, 1328–1342. [Google Scholar] [CrossRef] [PubMed]
- Darlow, B.; Coleman, K.; McKinlay, E.; Donovan, S.; Beckingsale, L.; Gray, B.; Neser, H.; Perry, M.; Stanley, J.; Pullon, S. The positive impact of interprofessional education: A controlled trial to evaluate a programme for health professional students. BMC Med. Educ. 2015, 15, 98. [Google Scholar] [CrossRef]
- Hamada, S.; Haruta, J.; Maeno, T.; Maeno, T.; Suzuki, H.; Takayashiki, A.; Inada, H.; Naito, T.; Tomita, M.; Kanou, N.; et al. Effectiveness of an interprofessional education program using team-based learning for medical students: A randomized controlled trial. J. Gen. Fam. Med. 2020, 21, 2–9. [Google Scholar] [CrossRef]
- Guraya, S.Y.; Barr, H. The effectiveness of interprofessional education in healthcare: A systematic review and meta-analysis. Kaohsiung J. Med. Sci. 2018, 34, 160–165. Available online: https://onlinelibrary.wiley.com/doi/full/10.1016/j.kjms.2017.12.009 (accessed on 10 July 2024). [CrossRef] [PubMed]
- Kostenlose Online-Tabellenkalkulationssoftware: Excel|Microsoft 365. Available online: https://www.microsoft.com/de-de/microsoft-365/excel?legRedir=true&CorrelationId=ad85ea15-a381-4157-ae9e-45b3c87fee3f&market=de (accessed on 10 July 2024).
- Untitled Diagram—Draw.io. Available online: https://app.diagrams.net/ (accessed on 2 June 2024).
- Post, B. Consultation Skills for Pharmacy Practice: Taking a Patient-Centred Approach a CPPE Distance Learning Programme for Pharmacy Professionals Contacting CPPE Telephone 0161 778 4000 Consultation Skills for Pharmacy Practice: Taking a Patient-Centred Approach a CPPE Distance Learning Programme for Pharmacy Professionals Educational Solutions for the NHS Pharmacy Workforce a Core Learning Programme for: Acknowledgements 2014. Available online: www.cppe.ac.uk (accessed on 8 May 2024).
- Pediatric HAL® S3005|Tetherless 5-Year Pediatric Simulator. Available online: https://www.gaumard.com/products/s3005 (accessed on 22 May 2024).
- HAL® S1000|Advanced Life Support and Emergency Care, Wireless Patient Simulator. Available online: https://www.gaumard.com/products/s1000 (accessed on 22 May 2024).
- SIMULATION RECORDING SYSTEMS|Portable Recording and Debriefing|Nordic Simulators. Available online: https://nordicsimulators.com/portable-recording-systems/ (accessed on 22 May 2024).
- Infos—Pharma4u. Available online: https://www.pharma4u.de/apotheker/medicheck/infos/ (accessed on 9 May 2024).
- Dabidian, A.; Obarcanin, E.; Ali Sherazi, B.; Schlottau, S.; Schwender, H.; Laeer, S. Impact of a Digital Tool on Pharmacy Students’ Ability to Perform Medication Reviews: A Randomized Controlled Trial. Healthcare 2023, 11, 1968. Available online: https://www.mdpi.com/2227-9032/11/13/1968/htm (accessed on 22 May 2024). [CrossRef] [PubMed]
- Abdel-Tawab, R.; James, D.H.; Fichtinger, A.; Clatworthy, J.; Horne, R.; Davies, G. Development and validation of the Medication-Related Consultation Framework (MRCF). Patient Educ. Couns. 2011, 83, 451–457. [Google Scholar] [CrossRef] [PubMed]
- Zorek, J.A.; Fike, D.S.; Eickhoff, J.C.; Engle, J.A.; MacLaughlin, E.J.; Dominguez, D.G.; Seibert, C.S. Refinement and Validation of the Student Perceptions of Physician-Pharmacist Interprofessional Clinical Education Instrument. Am. J. Pharm. Educ. 2016, 80, 47. [Google Scholar] [CrossRef]
- Van Winkle, L.J.; Fjortoft, N.; Hojat, M. Validation of an Instrument to Measure Pharmacy and Medical Students’ Attitudes Toward Physician-Pharmacist Collaboration. Am. J. Pharm. Educ. 2011, 75, 178. [Google Scholar] [CrossRef]
- Origin 2021 Feature Highlights. Available online: https://www.originlab.com/2021 (accessed on 27 May 2024).
- Tallentire, V.R.; Kerins, J.; McColgan-Smith, S.; Power, A.; Stewart, F.; Mardon, J. Exploring transformative learning for trainee pharmacists through interprofessional simulation: A constructivist interview study. Adv. Simul. 2021, 6, 31. Available online: https://advancesinsimulation.biomedcentral.com/articles/10.1186/s41077-021-00180-2 (accessed on 2 June 2024). [CrossRef]
- Kelly, A.; Nirula, L.; McDiarmid, E.; Jindani, F.; Fernando, A.; Naismith, L.; Kowalski, C. Lessons Learned: Implementing UK-Developed Interprofessional Simulation Training Courses in a Canadian Setting. Acad. Psychiatry 2018, 42, 659–663. Available online: https://link.springer.com/article/10.1007/s40596-018-0943-1 (accessed on 10 July 2024). [CrossRef]
- Robinson, J.D.; Bray, B.S.; Willson, M.N.; Weeks, D.L. Using Human Patient Simulation to Prepare Student Pharmacists to Manage Medical Emergencies in an Ambulatory Setting. Am. J. Pharm. Educ. 2011, 75, 3. [Google Scholar] [CrossRef] [PubMed]
- Tokunaga, J.; Takamura, N.; Ogata, K.; Yoshida, H.; Setoguchi, N.; Matsuoka, T.; Hirokane, T.; Yamaoka, A.; Sato, K. Vital Sign Monitoring Using Human Patient Simulators at Pharmacy Schools in Japan. Am. J. Pharm. Educ. 2010, 74, 132. [Google Scholar] [CrossRef] [PubMed]
- Won, K.J.; Tsu, L.V.; Saldivar, S.; Beuttler, R.; Walsh, A. The effect of interprofessional simulations on pharmacy and physician assistant students’ learning of advanced cardiac life support concepts. Curr. Pharm. Teach. Learn. 2023, 15, 521–527. [Google Scholar] [CrossRef] [PubMed]
- Yıldırım Sarı, H.; Özgüven Öztornacı, B.; Ardahan Akgül, E.; Karakul, A.; Doğan, Z.; Doğan, P. The Results of Simulation Training in Pediatric Nursing Students’ Education. J. Pediatr. Res. 2018, 5, 194–200. [Google Scholar] [CrossRef]
- Chin, K.L.; Yap, Y.L.; Lee, W.L.; Soh, Y.C. Comparing Effectiveness of High-Fidelity Human Patient Simulation vs Case-Based Learning in Pharmacy Education. Am. J. Pharm. Educ. 2014, 78, 153. [Google Scholar] [CrossRef]
- Carey, J.M.; Rossler, K. The How When Why of High Fidelity Simulation; StatPearls: Treasure Island, FL, USA, 2023. Available online: https://www.ncbi.nlm.nih.gov/books/NBK559313/ (accessed on 22 June 2024).
- Beichler, H.; Grandy, S.; Neumaier, S.; Lilgenau, A.; Schwarz, H.; Wagner, M. Interprofessional Paediatric High-Fidelity Simulation Training: A Mixed Methods Study of Experiences and Readiness among Nursing and Medical Students. Nurs. Rep. 2024, 14, 566–585. [Google Scholar] [CrossRef]



| Pharmacy Participants | HFS-Adult (n = 17) | HFS-Pediatric (n = 16) | |||
|---|---|---|---|---|---|
| Intervention (n = 9) | Control (n = 8) | Intervention (n = 8) | Control (n = 8) | ||
| Age | Mean (±SD) | 24 (±2.205) | 25 (±3.615) | 25 (±4.062) | 25 (±2.268) |
| Median | 23 | 23 | 23.5 | 24 | |
| Range | 21–28 | 22–32 | 22–34 | 22–29 | |
| Gender | Male, n (%) | 1 (11%) | 2 (25%) | 3 (37%) | 0 (0%) |
| Female, n (%) | 8 (89%) | 6 (75%) | 5 (63%) | 8 (100%) | |
| Experience in drug therapy consultation (e.g., outpatient or inpatient hospitals) | |||||
| Yes, n (%) | 0 (0%) | 1 (12%) | 1 (12%) | 0 (0%) | |
| No, n (%) | 9 (100%) | 7 (88%) | 7 (88%) | 8 (100%) | |
| Medical Participants | HFS-Adult (n = 9) | HFS-Pediatric (n = 8) | |
|---|---|---|---|
| Age | Mean (±SD) | 24 (±2.550) | 23 (±0.518) |
| Median | 23 | 23.5 | |
| Range | 22–29 | 22–23 | |
| Gender | Male, n (%) | 5 (56%) | 2 (25%) |
| Female, n (%) | 4 (44%) | 6 (75%) | |
| Experience in drug therapy consultation (e.g., outpatient or inpatient hospitals) | |||
| Yes, n (%) | 6 (67%) | 3 (37%) | |
| No, n (%) | 3 (33%) | 5 (63%) | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sharkas, A.R.; Ali Sherazi, B.; Sayyed, S.A.; Kinny, F.; Steichert, M.; Schwender, H.; Laeer, S. Development and Evaluation of Interprofessional High-Fidelity Simulation Course on Medication Therapy Consultation for German Pharmacy and Medical Students—A Randomized Controlled Study. Pharmacy 2024, 12, 128. https://doi.org/10.3390/pharmacy12040128
Sharkas AR, Ali Sherazi B, Sayyed SA, Kinny F, Steichert M, Schwender H, Laeer S. Development and Evaluation of Interprofessional High-Fidelity Simulation Course on Medication Therapy Consultation for German Pharmacy and Medical Students—A Randomized Controlled Study. Pharmacy. 2024; 12(4):128. https://doi.org/10.3390/pharmacy12040128
Chicago/Turabian StyleSharkas, Ahmed Reda, Bushra Ali Sherazi, Shahzad Ahmad Sayyed, Florian Kinny, Melina Steichert, Holger Schwender, and Stephanie Laeer. 2024. "Development and Evaluation of Interprofessional High-Fidelity Simulation Course on Medication Therapy Consultation for German Pharmacy and Medical Students—A Randomized Controlled Study" Pharmacy 12, no. 4: 128. https://doi.org/10.3390/pharmacy12040128
APA StyleSharkas, A. R., Ali Sherazi, B., Sayyed, S. A., Kinny, F., Steichert, M., Schwender, H., & Laeer, S. (2024). Development and Evaluation of Interprofessional High-Fidelity Simulation Course on Medication Therapy Consultation for German Pharmacy and Medical Students—A Randomized Controlled Study. Pharmacy, 12(4), 128. https://doi.org/10.3390/pharmacy12040128





