Educators’ Interprofessional Collaborative Relationships: Helping Pharmacy Students Learn to Work with Other Professions
Abstract
:1. Introduction
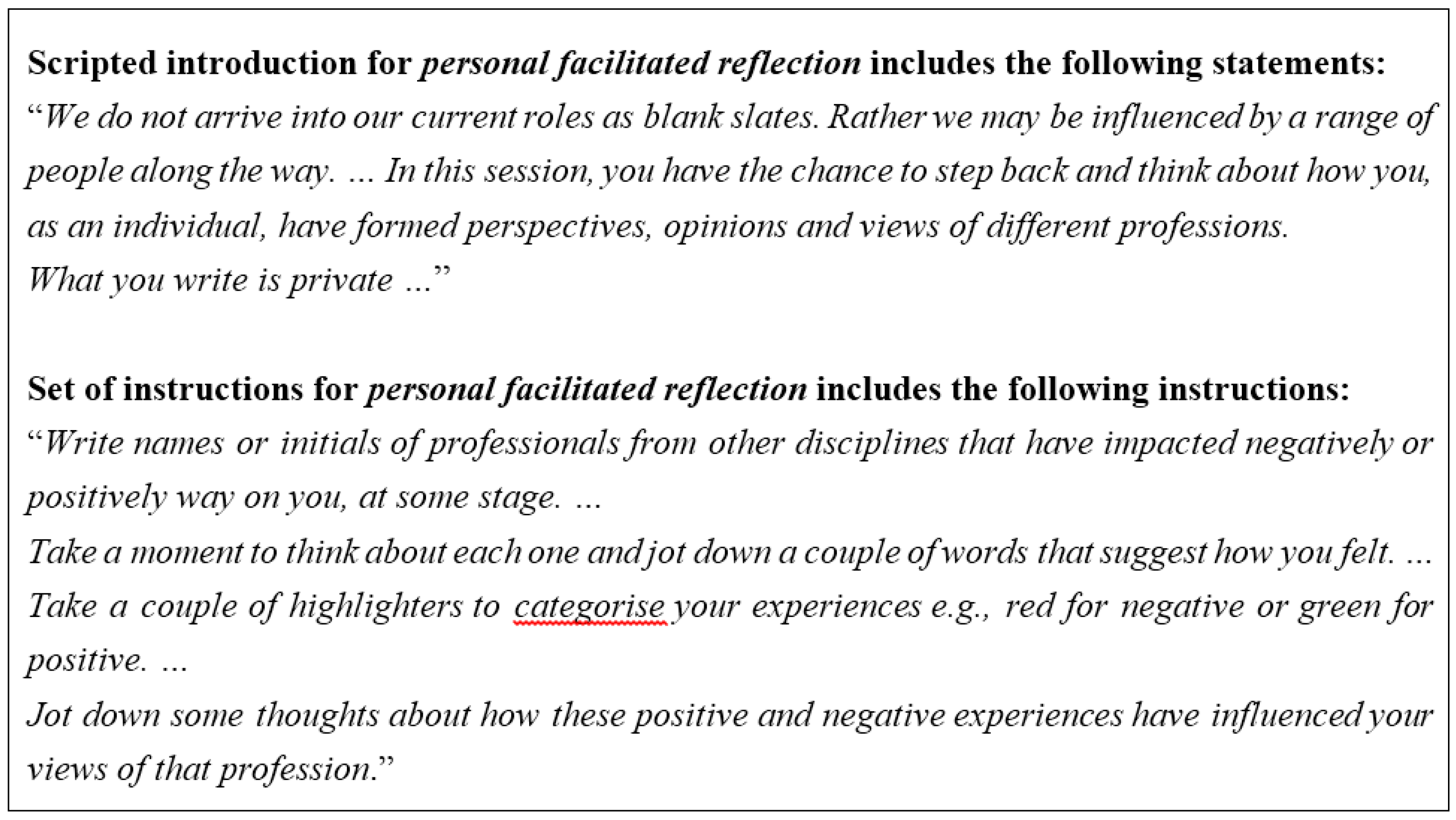
2. Method
3. Findings
3.1. Being Inclusive of Other Professions
“Well the main profession that I work with is [particular profession] so [they are] my first and probably my major contact. I don’t have a lot to do with other [professions] in my day to day duties. … I know going way back when I was at uni, we didn’t have a lot of interaction with the other disciplines, socially or in combined lectures or whatever.”(Educator N28)
“I think before I came here I was in one of those silos … I think I wasn’t aware that I was in it.”(Educator G9)
“My perspective has changed on one particular profession. … There’s more depth to what they actually do.”(Educator G9)
“I think working with the other health professions (educators) has made me teach the importance of not being so tunnelled into your own profession.”(Educator H39)
“When I see people behaving as if they own a scope of practice or a skill … I find that extremely irritating.”(Educator H8)
“Some things (about discipline territories) you can accept and some things you can’t. (But) you come at it from the patient perspective, what’s better for the patient … you need to be able to question another profession.”(Educator O18)
3.2. Developing Interpersonal Connections with Colleagues from Other Professions
“If you have preconceived ideas (about particular professions) that are negative, I’ve found that … (knowing an individual from that profession through working here) has broken down some barriers that I’ve internally had.”(Educator M15)
“I think it’s learning more about the person in order to make their profession more accessible. I think if you have a friend or know of someone socially, and they’re in a particular profession you’re going to probably know a little bit more about that profession, particularly if you’re quite friendly with that person.”(Educator G9)
“I suppose as working for [UONDRH] there’s probably an expectation to come to these social things. You don’t have to but I enjoy them.”(Educator C29)
“Because we all know each other here and we’re friendly toward each other we might sling off as a joke [about each other’s profession] but the students may not realise we’re joking.”(Educator N4)
3.3. Bringing a Sense of Own Profession in Relation to Other Professions
“[In our interprofessional learning modules] you’re your own person to shine within your area and each person has that opportunity to be that person and promote their own profession which is a fantastic opportunity really for people to recognise the whole patient pathway and not just the bit that they do.”(Educator O18)
“I think it’s trying to ascribe value to each discipline group so that they feel that they can contribute.”(Educator X27)
“I guess if you’re voicing frustrations about certain things then that’s going to impact and perhaps add to a stereotype.”(Educator K7)
3.4. Giving and Receiving Respect to Other Professions
“I think the way we get [the students to learn to work with other professions] is by being positive role models about [interactions with] other disciplines as educators and being mindful of what we say in front of the students we’re teaching whether they’re students of our own discipline or students of other disciplines.”(Educator N4)
“By the facilitators asking each other what they would do, it shows respect and an acknowledgement that we’re all part of a jigsaw and we’re all there for the patient.”(Educator X27)
“You’d hope that in the whole way we treat them [other professions] … that they [the students] would sense that we do value [other professions’] input, according to the patient’s needs.”(Educator Z1)
“I think if you respect others, then it’s not unreasonable to expect respect in return.”(Educator X27)
3.5. Being Learner-centred for Students’ Collaborative Practice
“We’re all really committed to creating these learning opportunities for the students.”(Educator R20)
“There’s that synergy between the academics. … They want to work together and all the discipline academics are always thinking about how they can work together and how they can pull that together because they can all see the considerable benefits for their students to work in an interdisciplinary fashion.”(Educator A3)
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- American Pharmacists Association Foundation and American Pharmacists Association. Consortium recommendations for advancing pharmacists’ patient care services and collaborative practice agreements. J. Am. Pharm. Assoc. 2013, 53, e132–e141. [Google Scholar]
- The Interprofessional Curriculum Renewal Consortium A. Curriculum Renewal for Interprofessional Education in Health; Commonwealth of Australia, Office for Learning and Teaching: Canberra, Australia, 2014.
- Reeves, S.; Zwarenstein, M.; Goldman, J.; Barr, H.; Freeth, D.; Hammick, M.; Koppel, I. Interprofessional Education: Effects on Professional Practice and Health Care Outcomes. Cochrane Database Syst. Rev. 2008. [Google Scholar] [CrossRef]
- Croker, A.; Croker, J.; Grotowski, M. Changing directions in health care. In Health Practice Relationships; Higgs, J., Croker, A., Tasker, D., Hummell, J., Patton, N., Eds.; Sense Publishers: Rotterdam, The Netherlands, 2014; pp. 27–36. [Google Scholar]
- Halvorsen, K.H.; Stensland, P.; Granas, A.G. A qualitative study of physicians’ and nurses’ experiences of multidisciplinary collaboration with pharmacists participating at case conferences. Int. J. Pharm. Pract. 2011, 19, 350–357. [Google Scholar] [CrossRef] [PubMed]
- Furniss, L.; Burns, A.; Craig, K.; Scobie, S.; Cooke, J.; Faragher, B. Effects of a pharmacist’s medication review in nursing homes. Br. J. Psychiatry 2000, 176, 563–567. [Google Scholar] [CrossRef] [PubMed]
- Alderman, C.; Farmer, C. A brief analysis of clinical pharmacy interventions undertaken in an Australian teaching hospital. Int. J. Pharm. Pract. 2001, 21, 99–103. [Google Scholar] [CrossRef]
- Aslani, P. Patient empowerment and informed decision-making. Int. J. Pharm. Pract. 2013, 21, 347–348. [Google Scholar] [CrossRef] [PubMed]
- Chisholm-Burns, M.A.; Lee, J.K.; Spivey, C.A.; Slack, M.; Herrier, R.N.; Hall-Lipsy, E.; Zivin, J.G.; Abraham, I.; Palmer, J.; Martin, J.R.; et al. US pharmacists’ effect as team members on patient care. Med. Care 2010, 48, 923–933. [Google Scholar] [CrossRef] [PubMed]
- Croker, A.; Higgs, J.; Trede, F. What do we mean by collaboration, and when is a “team” not a “team”? A qualitative unbundling of terms and meanings. Qual. Res. J. 2009, 9, 28–42. [Google Scholar] [CrossRef]
- Freeth, D. Sustaining interprofessional collaboration. J. Interprof. Care 2001, 15, 37–46. [Google Scholar] [CrossRef] [PubMed]
- Dey, R.M.; de Vries, M.J.W.; Bosnic-Anticevich, S. Collaboration in chronic care: Unpacking the relationship of pharmacists and general practitioners in primary care. Int. J. Pharm. Pract. 2011, 19, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Kelly, D.; Bishop, L.; Young, S.; Hawboldt, J.; Phillips, L.; Montgomery Keough, T. Pharmacist and physician views on collaborative practice: Findings from the community pharmaceutical care project. Can. Pharm. J. 2013, 146, 218–266. [Google Scholar] [CrossRef] [PubMed]
- Tan, E.; Stewart, K.; Elliott, R.; George, J. Integration of pharmistis into general practice clinics in Australia: The views of general practitioners and pharmacists. Int. J. Pharm. Pract. 2014, 22, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Jorgenson, D.; Laubscher, T.; Lyons, B.; Palmer, R. Integrating pharmacists into primary care teams: Barriers and facilitators. Int. J. Pharm. Pract. 2014, 22, 292–299. [Google Scholar] [CrossRef] [PubMed]
- Centre for The Advancement Of Interprofessional Education (CAIPE). Defining IPE. 2002. Available online: http://www.caipe.org.uk/about-us/defining-ipe (accessed on 1 December 2014).
- Farlow, J.L.; Goodwin, C.; Sevilla, J. Interprofessional education through service-learning: Lessons from a student-led free clinic. J. Interprof. Care 2015, 29, 263–264. [Google Scholar] [CrossRef] [PubMed]
- Borrego, M.E.; Rhyne, R.; Hansbarger, L.; Geller, Z.; Edwards, P.; Griffin, B.; McClain, L. Pharmacy student participation in rural interdisciplinary education using problem based learning (PBL) case tutorials. Am. J. Pharm. Educ. 2000, 64, 355–363. [Google Scholar]
- Croker, A.; Fisher, K.; Smith, T. When students from different professions are co-located: The importance of interprofessional rapport for learning to work together. J. Interprof. Care 2015, 29, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Page, R.L.; Hume, A.L.; Trujillo, J.; Leader, W.G.; Vardeny, O.; Neuhauser, M.M.; Devra Dang, M.P.H.; Nesbit, S.; Cohen, L.J. ACCP White Paper. Interprofessional education: Principles and application. A framework for clinical pharmacy. Pharmacotherapy 2009, 29, 145e–164e. [Google Scholar] [CrossRef]
- Boyce, R.; Robilliard, J.; Duprez, K.; Cooper, J.; Rasiah, R.; Smith, T. Integrating inter-professional learning into pharmacy student placements. In Proceedings of the Interprofessional Education for Quality Use of Medicine, Newcastle, Australia, 29–30 November 2012.
- Lindqvist, S.; Reeves, S. Facilitators’ perceptions of delivering interprofessional education: A qualitative study. Med. Teach. 2007, 29, 403–405. [Google Scholar] [CrossRef] [PubMed]
- Freeth, D.; Reeves, S. Learning to work together: Using the presage, process, product (3P) model to highlight decisions and possibilities. J. Interprof. Care 2004, 18, 43–56. [Google Scholar] [CrossRef] [PubMed]
- Croker, A.; Hudson, J.N. Interprofessional education: Does recent literature from rural settings offer insights into what really matters? Med. Educ. 2015, 49, 880–887. [Google Scholar] [CrossRef] [PubMed]
- Australian Government Department of Health. Rural Health Multidisciplinary Training Program—University Departments of Rural Health (UDRH). Available online: http://www.ruralhealthaustralia.gov.au/internet/rha/publishing.nsf/Content/Multidisciplinary_Rural_Training_Network-University_Departments_of_Rural_Health (accessed on 27 October 2015).
- Gadamer, H. On the scope and function of hermeneutical reflection (1967). In Hans-Georg Gadamer: Philosophical Hermeneutics; Linge, D.E., Ed.; University of California Press: Berkley, MA, USA, 1976. [Google Scholar]
- Bridges, D.; McGee, S. Collaborative inquiry: Process, theory and ethics. In Researching Practice: A Discourse on Qualitative Methodologies; Higg, J., Cheery, N., Macklin, R., Ajjawi, R., Eds.; Sense: Rotterdam, The Netherlands, 2010. [Google Scholar]
- Gilbert, L. Pharmacist and nurse: A team approach towards primary health care or a convenient “therapeutic alliance”? Int. J. Nurs. Stud. 1997, 34, 367–374. [Google Scholar] [CrossRef]
- Makowsky, M.; Schindel, T.; Rosenthal, M.; Campbell, K.; Tsuyuki, R.; Madill, H. Collaboration between pharmacistis, physicians and nurse practitioners: A qualitative investigation of working relationships in the inpatient medical setting. J. Interprof. Care 2009, 23, 169–184. [Google Scholar] [CrossRef] [PubMed]
- Dobson, R.; Henry, C.; Taylor, J.; Zello, G.; Lachaine, J.; Forbes, D.; Keegan, D.L. Interprofessional health care teams: Attitudes and environmental factors associated with participation by community pharmacists. J. Interprof. Care 2006, 20, 119–132. [Google Scholar] [CrossRef] [PubMed]
- Weiss, M.; Sutton, J. The changing nature of prescribing: Pharmacists as prescribers and challenges to medical dominance. Sociol. Health Illn. 2009, 31, 406–421. [Google Scholar] [CrossRef] [PubMed]
- Fletcher, A.; Marra, F.; Kaczorowski, J. Pharmacists as vaccination providers: Friend or foe? Can. Pharm. J. Rev. Pharm. Can. 2014, 147, 141–142. [Google Scholar] [CrossRef] [PubMed]
- Australian Medical Association. AMA Questions Safety of Pharmacy Vaccinations. 2014. Available online: https://ama.com.au/gp-network-news/ama-questions-safety-pharmacy-vaccinations (accessed on 15 September 2015).
- Colleridge, S. The Rime of the Ancient Mariner. 1798. Available online: http://www.poetsgraves.co.uk/Classic%20Poems/Coleridge/the_rime_of_the_ancient_mariner.htm (accessed on 23 November 2015).
| Professional Category 1 | Photo-Elicitation Interviews 2 | Educators Contributing to Focus Groups 3 |
|---|---|---|
| Diagnostic radiography | 2 | 2 |
| Medicine | 6 | 3 |
| Nursing | 3 | 2 |
| Nutrition and dietetics | 4 | 3 |
| Occupational therapy | 2 | 2 |
| Pharmacy | 2 | 2 |
| Physiotherapy | 3 | 2 |
| Speech pathology | 2 | 1 |
| TOTAL | 24 | 19 |
© 2016 by the authors; licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons by Attribution (CC-BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Croker, A.; Smith, T.; Fisher, K.; Littlejohns, S. Educators’ Interprofessional Collaborative Relationships: Helping Pharmacy Students Learn to Work with Other Professions. Pharmacy 2016, 4, 17. https://doi.org/10.3390/pharmacy4020017
Croker A, Smith T, Fisher K, Littlejohns S. Educators’ Interprofessional Collaborative Relationships: Helping Pharmacy Students Learn to Work with Other Professions. Pharmacy. 2016; 4(2):17. https://doi.org/10.3390/pharmacy4020017
Chicago/Turabian StyleCroker, Anne, Tony Smith, Karin Fisher, and Sonja Littlejohns. 2016. "Educators’ Interprofessional Collaborative Relationships: Helping Pharmacy Students Learn to Work with Other Professions" Pharmacy 4, no. 2: 17. https://doi.org/10.3390/pharmacy4020017
APA StyleCroker, A., Smith, T., Fisher, K., & Littlejohns, S. (2016). Educators’ Interprofessional Collaborative Relationships: Helping Pharmacy Students Learn to Work with Other Professions. Pharmacy, 4(2), 17. https://doi.org/10.3390/pharmacy4020017





