Pharmacist Segments Identified from 2009, 2014, and 2019 National Pharmacist Workforce Surveys: Implications for Pharmacy Organizations and Personnel
Abstract
1. Introduction
2. Study Objectives
- Identify segments of pharmacists based upon time spent in medication providing and patient care services.
- Describe segments according to demographic characteristics.
- Describe segments according to work contributions.
- Describe segments by work setting.
- Describe segments according to work activities.
- Describe year of licensure cohorts to identify trends that might impact future pharmacist capacity for contributing to the U.S. health care system.
- Compare the findings from the 2019 data with findings from the 2009 and 2014 data.
- Interpret the findings within the context of future scope of practice changes that could affect roles filled by pharmacists and pharmacy workforce support personnel.
3. Methods
- Medication providing: professional services associated with preparing, distributing, and administering medication products, including associated consultation, interacting with patients about the selection and use of over-the-counter products, and interactions with other professionals during the medication dispensing process.
- Patient care services: professional services not associated with medication dispensing for assessing and evaluating patient medication-related needs, monitoring and adjusting patients’ treatments to attain desired outcomes, and other services designed for patient care.
- Business/organization management: managing personnel, finances, and operations.
- Research/scholarship: discovery, development, and evaluation of products, services, and/or ideas.
- Education: teaching, precepting, and mentoring of students/trainees/technicians.
- Other: any activities not described in the above categories.
4. Results
- Medication providing: professional services associated with preparing, distributing, and administering medication products, including associated consultation, interacting with patients about the selection and use of over-the-counter products, and interactions with other professionals during the medication dispensing process.
- Patient care services: professional services not associated with medication dispensing for assessing and evaluating patient medication-related needs, monitoring and adjusting patients’ treatments to attain desired outcomes, and other services designed for patient care.
4.1. Medication Providers
4.2. Medication Providers Who also Provide Patient Care
4.3. Other Activity Pharmacists
4.4. Patient Care Providers Who also Provide Medication
4.5. Patient Care Providers
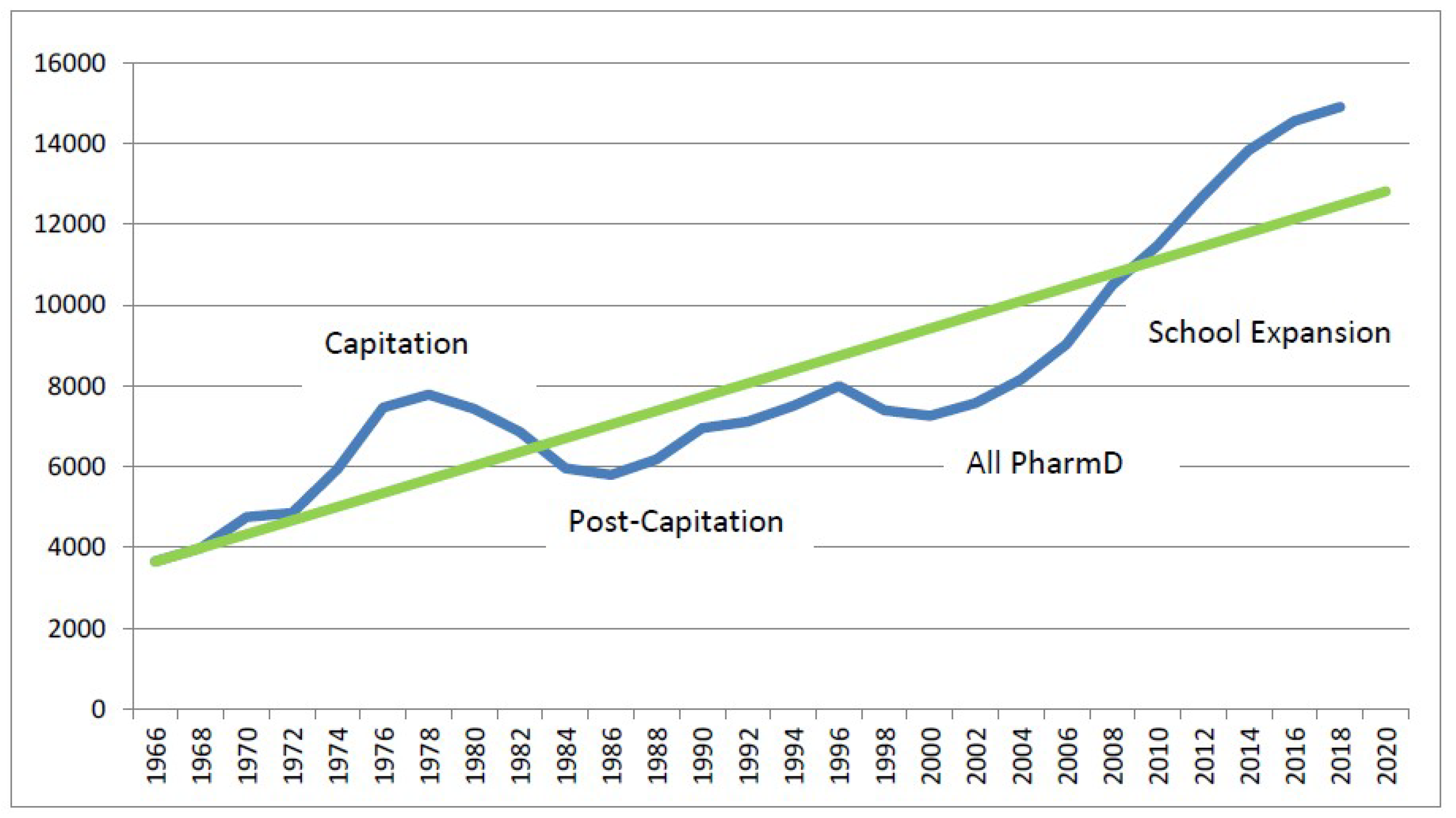
4.6. Year of Licensure Cohorts
5. Discussion
6. Limitations
7. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Schommer, J.C.; Planas, L.; Johnson, K.A.; Doucette, W.R.; Gaither, C.A.; Kreling, D.H.; Mott, D.A. Pharmacist Contributions to the U.S. Health Care System. Innov. Pharm. 2010, 1, 16. [Google Scholar] [CrossRef]
- Schommer, J.C.; Gaither, C.A.; Doucette, W.R.; Kreling, D.H.; Mott, D.A. Pharmacist Contributions to the U.S. Health Care System Reported in the 2009 and 2014 National Pharmacist Workforce Surveys. Innov. Pharm. 2015, 6, 14. [Google Scholar] [CrossRef]
- 2017–2018 Profile of Pharmacy Students—AACP, American Association of Colleges of Pharmacy. Available online: www.aacp.org (accessed on 10 October 2019).
- Maine, L.L. It Really Isn’t That Simple. Am. J. Pharm. Educ. 2019, 83, 7593. [Google Scholar]
- Lebovitz, L.; Eddington, N.D. Trends in the Pharmacist Workforce and Pharmacy Education. Am. J. Pharm. Educ. 2019, 83, 7051. [Google Scholar] [PubMed]
- Baines, D.; Bates, I.; Bader, L.; Hale, C.; Schneider, P. Conceptualising production, productivity and technology in pharmacy practice: A novel framework for policy, education and research. Hum. Resour. Health 2018, 16, 51. [Google Scholar] [CrossRef] [PubMed]
- Frogner, B.K.; Fraher, E.P.; Spetz, J.; Pittman, P.; Moore, J.; Beck, A.J.; Buerhaus, P.I. Modernizing Scope-of-Practice Regulations—Time to Prioritize Patients. N. Engl. J. Med. 2020, 382, 591–593. [Google Scholar] [CrossRef]
- Olson, A.W.; Schommer, J.C.; Hadsall, R.S. A 15 Year Ecological Comparison for the Market Dynamics of Minnesota Community Pharmacies from 2002 to 2017. Pharmacy 2018, 6, 50. [Google Scholar] [CrossRef]
- Schommer, J.C.; Olson, A.W.; Isetts, B.J. Transforming community-based pharmacy practice through financially sustainable centers for health and personal care. J. Am. Pharm. Assoc. 2019, 59, 306–309. [Google Scholar] [CrossRef] [PubMed]
- Schommer, J.C.; Doucette, W.R.; Johnson, K.A.; Planas, L. Positioning and integrating medication therapy management. J. Am. Pharm. Assoc. 2012, 52, 12–24. [Google Scholar] [CrossRef] [PubMed]
- Schommer, J.C.; Doucette, W.R.; Planas, L. Establishing pathways for access to pharmacist-provided patient care. J. Am. Pharm. Assoc. 2015, 55, 664–668. [Google Scholar] [CrossRef] [PubMed]
- Knapp, K.K.; Olson, A.W.; Schommer, J.C.; Gaither, C.A.; Mott, D.A.; Doucette, W.R. Retail Clinics Co-Located with Pharmacies: A Delphi Study of Pharmacist Impacts and Recommendations for Optimization. J. Am. Pharm. Assoc. 2019. [Google Scholar] [CrossRef]
- Pedersen, C.A.; Schneider, P.J.; Ganio, M.C.; Scheckelhoff, D.J. ASHP National Survey of Pharmacy Practice in Hospital Settings: Monitoring and Patient Education—2018. Am. J. Health Syst. Pharm. 2019, 76, 1038–1058. [Google Scholar] [CrossRef]
- Healthcare Financial Management Association. Acquisition and Affiliation Strategies; Healthcare Financial Management Association: Westchester, IL, USA, 2014; Available online: https://www.hfma.org/DownloadAsset.aspx?id=23451 (accessed on 4 September 2018).
- Greaney, T.L.; Richman, B.D. Consolidation in Provider and Insurer Markets: Enforcement Issues and Priorities; American Antitrust Institute: Washington, DC, USA, 2018; Available online: https://www.antitrustinstitute.org/sites/default/files/AAI_Healthcare%20WP%20Part%20I_6.12.18.pdf (accessed on 4 September 2018).
- Greaney, T.L.; Richman, B.D. Promoting Competition in Healthcare Enforcement and Policy: Framing an Active Competition Agenda; American Antitrust Institute: Washington, DC, USA, 2018; Available online: https://www.antitrustinstitute.org/sites/default/files/AAI_Healthcare%20WP%20Part%20II_6.18.18.pdf (accessed on 4 September 2018).
- Madara, J.L. The Acquisition of Aetna, Inc. by CVS Health Corporation; Position Paper; American Medical Association: Chicago, IL, USA, 2018; Available online: https://searchlf.ama-assn.org/undefined/documentDownload?uri=%2Funstructured%2Fbinary%2Fletter%2FLETTERS%2F2018-8-7-Letter-to-Delrahim-CVS-Aetna-Merger.pdf (accessed on 4 September 2018).
- Urick, B.Y.; Meggs, E.V. Towards a Greater Professional Standing: Evolution of Pharmacy Practice and Education, 1920–2020. Pharmacy 2019, 7, 98. [Google Scholar] [CrossRef]
- Ascione, F. Preparing Pharmacists for Collaborative/Integrated Health Settings. Pharmacy 2019, 7, 47. [Google Scholar] [CrossRef]
- Goode, J.-V.K.R.; Owen, J.A.; Page, A.; Gatewood, S. Community-Based Pharmacy Practice Innovation and the Role of the Community-Based Pharmacist Practitioner in the United States. Pharmacy 2019, 7, 106. [Google Scholar] [CrossRef]
- Doucette, W.R. Innovative Collaboration between a Medical Clinic and a Community Pharmacy: A Case Report. Pharmacy 2019, 7, 62. [Google Scholar] [CrossRef]
- Knapp, K.; Yoshizuka, K.; Sasaki-Hill, D.; Caygill-Walsh, R. Co-located Retail Clinics and Pharmacies: An Opportunity to Provide More Primary Care. Pharmacy 2019, 7, 74. [Google Scholar] [CrossRef]
- Neves, C.D.M.; Nascimento, M.M.G.D.; Silva, D.; Álvares, M.; Ramalho-De-Oliveira, D. Clinical Results of Comprehensive Medication Management Services in Primary Care in Belo Horizonte. Pharmacy 2019, 7, 58. [Google Scholar]
- Twigg, G.; David, T.; Taylor, J. An Improved Comprehensive Medication Review Process to Assess Healthcare Outcomes in a Rural Independent Community Pharmacy. Pharmacy 2019, 7, 66. [Google Scholar] [CrossRef]
- Took, R.L.; Liu, Y.; Kuehl, P.G. A Study to Identify Medication-Related Problems and Associated Cost Avoidance by Community Pharmacists during a Comprehensive Medication Review in Patients One Week Post Hospitalization. Pharmacy 2019, 7, 51. [Google Scholar] [CrossRef]
- Schullo-Feulner, A.; Krohn, L.; Knutson, A. Reducing Medication Therapy Problems in the Transition from Hospital to Home: A Pre- & Post-Discharge Pharmacist Collaboration. Pharmacy 2019, 7, 86. [Google Scholar]
- Liu, Y.; Guthrie, K.D.; May, J.R.; DiDonato, K.L. Community Pharmacist-Provided Wellness and Monitoring Services in an Employee Wellness Program: A Four-Year Summary. Pharmacy 2019, 7, 80. [Google Scholar] [CrossRef] [PubMed]
- Abraham, O.; Morris, A. Opportunities for Outpatient Pharmacy Services for Patients with Cystic Fibrosis: Perceptions of Healthcare Team Members. Pharmacy 2019, 7, 34. [Google Scholar] [CrossRef] [PubMed]
- Safitrih, L.; Perwitasari, D.A.; Ndoen, N.; Lestari, K. Health Workers’ Perceptions and Expectations of the Role of the Pharmacist in Emergency Units: A Qualitative Study in Kupang, Indonesia. Pharmacy 2019, 7, 31. [Google Scholar] [CrossRef]
- Maes, K.A.; Ruppanner, J.A.; Imfeld-Isenegger, T.L.; Hersberger, K.E.; Lampert, M.L.; Boeni, F. Dispensing of Prescribed Medicines in Swiss Community Pharmacies-Observed Counselling Activities. Pharmacy 2018, 7, 1. [Google Scholar] [CrossRef]
- Kaae, S.; Nørgaard, L.S.; Sporrong, S.K.; Almarsdottir, A.B.; Kofoed, M.; Daysh, R.F.; Jowkar, N. Patients’, Pharmacy Staff Members’, and Pharmacy Researchers’ Perceptions of Central Elements in Prescription Encounters at the Pharmacy Counter. Pharmacy 2019, 7, 84. [Google Scholar] [CrossRef]
- Schindel, T.J.; Breault, R.R.; Hughes, C.A. “It Made a Difference to Me”: A Comparative Case Study of Community Pharmacists’ Care Planning Services in Primary Health Care. Pharmacy 2019, 7, 90. [Google Scholar] [CrossRef]
- Redmond, S.; Paterson, N.; Shoemaker, S.J.; Ramalho-De-Oliveira, D. Development, Testing and Results of a Patient Medication Experience Documentation Tool for Use in Comprehensive Medication Management Services. Pharmacy 2019, 7, 71. [Google Scholar] [CrossRef]
- Frost, T.P.; Adams, A.J. Pharmacist and Technician Perceptions of Tech-Check-Tech in Community Pharmacy Practice Settings. J. Pharm. Pract. 2017, 31, 190–194. [Google Scholar] [CrossRef]
- Miller, R.F.; Cesarz, J.; Rough, S. Evaluation of community pharmacy tech-check-tech as a strategy for practice advancement. J. Am. Pharm. Assoc. 2018, 58, 652–658. [Google Scholar] [CrossRef]
- Andreski, M.; Myers, M.; Gainer, K.; Pudlo, A. The Iowa new practice model: Advancing technician roles to increase pharmacists’ time to provide patient care services. J. Am. Pharm. Assoc. 2018, 58, 268–274.e1. [Google Scholar] [CrossRef] [PubMed]
- Loria, K. A Look Ahead: What to Expect from the Pharmacy Landscape in 2020. Drug Topics. 2020. Available online: https://www.drugtopics.com/latest/look-ahead-what-expect-pharmacy-landscape-2020 (accessed on 29 January 2020).
- Doucette, W.R.; Matthew, J.W.; Vibhuti Arya, B.K.; Bakken, C.A.; Gaither, D.H.; Kreling, D.A.; Schommer, J.C. 2019 National Pharmacist Workforce Survey; Pharmacy Workforce Center: Washington, DC, USA, 2019; Available online: https://www.aacp.org/article/national-pharmacist-workforce-studies (accessed on 10 January 2020).
- Schommer, C.J.; Doucette, W.R.; Gaither, C.A.; Kreling, D.H.; Mott, D.A. Final Report of the 2009 National Pharmacist Workforce Survey; Pharmacy Manpower Project, Inc.: Alexandria, VA, USA, 2009; Available online: https://www.aacp.org/article/2009-national-pharmacist-workforce-study (accessed on 2 November 2009).
- Gaither, A.C.; Schommer, J.C.; Doucette, W.R.; Kreling, D.H.; Mott, D.A. 2014 National Pharmacist Workforce Survey; Pharmacy Workforce Center: Washington, DC, USA, 2014; Available online: https://www.aacp.org/article/2014-national-pharmacist-workforce-study (accessed on 31 January 2015).
- Yim, O.; Ramdeen, K.T. Hierarchical Cluster Analysis: Comparison of Three Linkage Measures and Application to Psychological Data. Quant. Methods Psychol. 2015, 11, 8–21. [Google Scholar] [CrossRef]
- Gernant, S.A.; Nguyen, M.-O.; Siddiqui, S.; Schneller, M. Use of pharmacy technicians in elements of medication therapy management delivery: A systematic review. Res. Soc. Adm. Pharm. 2017, 14, 883–890. [Google Scholar] [CrossRef] [PubMed]
- Doucette, W.R.; Schommer, J.C. Pharmacy Technicians’ Willingness to Perform Emerging Tasks in Community Practice. Pharmacy 2018, 6, 113. [Google Scholar] [CrossRef]
- Koehler, T.; Brown, A. A global picture of pharmacy technician and other pharmacy support workforce cadres. Res. Soc. Adm. Pharm. 2017, 13, 271–279. [Google Scholar] [CrossRef]
- Zellmer, W.A.; McAllister, E.B.; Silvester, J.A.; Vlasses, P.H. Toward uniform standards for pharmacy technicians: Summary of the 2017 Pharmacy Technician Stakeholder Consensus Conference. Am. J. Health Pharm. 2017, 74, 1321–1332. [Google Scholar] [CrossRef]
- Schommer, J.C.; Gaither, C.; Goode, J.-V.K.R.; Owen, J.A.; Scime, G.M.; Skelton, J.B.; Cernasev, A.; Hillman, L. Pharmacist and student pharmacist views of professional and personal well-being and resilience. J. Am. Pharm. Assoc. 2019, 60, 47–56. [Google Scholar] [CrossRef]
- Desselle, S.P.; Holmes, E.R. Results of the 2015 National Certified Pharmacy Technician Workforce Survey. Am. J. Health Pharm. 2017, 74, 981–991. [Google Scholar] [CrossRef]

| Pharmacist Segment | Segment Size (% of total) | Mean Time Devoted to Medication Providing | Mean Time Devoted to Patient Care Services | ||||||
|---|---|---|---|---|---|---|---|---|---|
| 2009 | 2014 | 2019 | 2009 | 2014 | 2019 | 2009 | 2014 | 2019 | |
| 1: Medication Provider | n = 496 (41%) | n = 555 (40%) | n = 1627 (34%) | 88% | 83% | 88% | 5% | 6% | 4% |
| 2: Medication Provider who also Provides Patient Care | n = 303 (25%) | n = 301 (22%) | n = 1194 (25%) | 65% | 60% | 63% | 19% | 22% | 16% |
| 3: Other Activity Pharmacists | n = 193 (16%) | n = 247 (18%) | n = 680 (14%) | 5% | 6% | 3% | 3% | 5% | 4% |
| 4: Patient Care Provider who also Provides Medication | n = 142 (12%) | n = 184 (13%) | n = 689 (15%) | 33% | 29% | 30% | 43% | 49% | 43% |
| 5: Patient Care Provider | n = 66 (6%) | n = 99 (7%) | n = 576 (12%) | 5% | 5% | 5% | 82% | 84% | 81% |
| Total | N = 1200 | N = 1382 | N = 4766 | 58% | 52% | 51% | 17% | 20% | 22% |
| Medication Provider | Medication Provider who also Provides Patient Care | Other Activity Pharmacists | Patient Care Provider who also Provides Medication | Patient Care Provider | Overall | |
|---|---|---|---|---|---|---|
| Demographic Characteristics | ||||||
| Mean Age (years) | ||||||
| 2009 | 52.0 | 50.2 | 49.2 | 45.6 | 47.4 | 50.1 |
| 2014 | 49.5 | 47.3 | 49.5 | 44.5 | 45.8 | 48.1 |
| 2019 | 45.1 | 44.1 | 48.2 | 41.9 | 41.3 | 44.4 |
| Gender (% female) | ||||||
| 2009 | 41% | 48% | 40% | 64% | 59% | 47% |
| 2014 | 52% | 59% | 54% | 66% | 68% | 57% |
| 2019 | 67% | 62% | 60% | 65% | 74% | 65% |
| Mean Year of First Licensure | ||||||
| 2009 | 1982 | 1983 | 1984 | 1988 | 1988 | 1983 |
| 2014 | 1989 | 1992 | 1989 | 1994 | 1993 | 1991 |
| 2019 | 2000 | 2001 | 1996 | 2003 | 2004 | 2001 |
| Hold PharmD (%) | ||||||
| 2009 | 17% | 17% | 42% | 40% | 53% | 26% |
| 2014 | 43% | 48% | 58% | 59% | 61% | 50% |
| 2019 | 57% | 59% | 60% | 75% | 81% | 63% |
| Residency Training (%) | ||||||
| 2009 | 3% | 4% | 19% | 25% | 26% | 9% |
| 2014 | 6% | 5% | 27% | 30% | 34% | 15% |
| 2019 | 4% | 6% | 26% | 28% | 40% | 15% |
| Both PharmD and Residency (%) | ||||||
| 2009 | 2% | 3% | 17% | 21% | 24% | 8% |
| 2014 | 4% | 3% | 22% | 26% | 33% | 12% |
| 2019 | 3% | 5% | 23% | 27% | 39% | 14% |
| Work Contributions | ||||||
| Practicing as a Pharmacist (%) | ||||||
| 2009 | 89% | 93% | 45% | 94% | 97% | 84% |
| 2014 | 90% | 95% | 59% | 94% | 93% | 86% |
| 2019 | 99% | 99% | 62% | 99% | 99% | 94% |
| Mean Hours Worked/Week | ||||||
| 2009 | 35.6 | 38.0 | 44.7 | 37.2 | 39.8 | 38.1 |
| 2014 | 37.2 | 39.5 | 46.4 | 40.3 | 40.8 | 40.0 |
| 2019 | 37.9 | 40.6 | 45.8 | 41.9 | 41.3 | 40.7 |
| Mean Hours per Week Worked from Home or Remotely | ||||||
| 2009 | - | - | - | - | - | - |
| 2014 | - | - | - | - | - | - |
| 2019 | 1.0 | 1.5 | 11.9 | 2.7 | 6.0 | 3.5 |
| For Primary Employment, Mean Number of Locations Worked at in a Typical Month | ||||||
| 2009 | - | - | - | - | - | - |
| 2014 | - | - | - | - | - | - |
| 2019 | 2.0 | 1.8 | 2.2 | 1.6 | 1.8 | 1.9 |
| Mean Number of Patients with whom you Interact as a Pharmacy Care Provider on a Typical Day | ||||||
| 2009 | - | - | - | - | - | - |
| 2014 | - | - | - | - | - | - |
| 2019 | 17.6 | 16.9 | 5.5 | 10.4 | 10.9 | 11.9 |
| Current Work Setting (Column %) | ||||||
| 2009 Community Pharmacy a | 78% | 67% | 10% | 23% | 1% | - |
| 2014 Community Pharmacy a | 68% | 58% | 15% | 13% | 1% | - |
| 2019 Community Pharmacy a | 76% | 64% | 9% | 15% | 3% | - |
| 2009 Hospital Setting | 15% | 25% | 30% | 54% | 64% | - |
| 2014 Hospital Setting | 17% | 28% | 23% | 70% | 49% | - |
| 2019 Hospital Setting | 10% | 21% | 27% | 57% | 47% | - |
| 2009 Other, Pharmacy Setting b | 7% | 7% | 15% | 16% | 27% | - |
| 2014 Other Pharmacy Setting b | 14% | 14% | 16% | 14% | 36% | |
| 2019 Other Pharmacy Setting b | 11% | 13% | 14% | 20% | 34% | |
| 2009 Other, Setting Non-Pharmacy c | <1% | 1% | 45% | 7% | 8% | - |
| 2014 Other, Setting Non-Pharmacy c | 1% | <1% | 46% | 3% | 14% | |
| 2019 Other Setting Non- Pharmacy c | 2% | 2% | 50% | 8% | 17% | |
| Current Work Setting (Row %) | ||||||
| 2009 Community Pharmacy a | 60% | 32% | 3% | 5% | <1% | - |
| 2014 Community Pharmacy a | 61% | 29% | 6% | 4% | <1% | |
| 2019 Community Pharmacy a | 57% | 35% | 3% | 5% | <1% | |
| 2009 Hospital Setting | 23% | 24% | 17% | 23% | 13% | - |
| 2014 Hospital Setting | 23% | 20% | 14% | 31% | 12% | |
| 2019 Hospital Setting | 13% | 20% | 15% | 31% | 21% | |
| 2009 Other Pharmacy Setting b | 29% | 16% | 23% | 18% | 14% | - |
| 2014 Other, Pharmacy Setting b | 36% | 18% | 18% | 12% | 16% | |
| 2019 Other, Pharmacy Setting b | 24% | 20% | 13% | 18% | 25% | |
| 2009 Other, Setting Non-Pharmacy c | 1% | 2% | 83% | 10% | 5% | - |
| 2014 Other, Setting Non-Pharmacy c | 4% | 1% | 81% | 4% | 10% | |
| 2019 Other, Setting Non-Pharmacy c | 7% | 4% | 61% | 11% | 17% | |
| Mean % of Time Currently Spent in Work Activities | ||||||
| 2009 Medication Providing | 88% | 65% | 5% | 33% | 5% | 58% |
| 2014 Medication Providing | 83% | 60% | 6% | 29% | 5% | 52% |
| 2019 Medication Providing | 88% | 63% | 3% | 30% | 5% | 51% |
| 2009 Patient Care Services | 5% | 19% | 3% | 43% | 82% | 17% |
| 2014 Patient Care Services | 6% | 22% | 5% | 49% | 84% | 20% |
| 2019 Patient Care Services | 4% | 16% | 4% | 43% | 81% | 22% |
| 2009 Business/Org. Management | 5% | 10% | 41% | 9% | 3% | 12% |
| 2014 Business/Org. Management | 5% | 8% | 39% | 7% | 2% | 12% |
| 2019 Business/Org. Management | 4% | 10% | 39% | 8% | 3% | 11% |
| 2009 Research | <1% | 1% | 18% | 4% | 3% | 4% |
| 2014 Research | <1% | 1% | 15% | 3% | 2% | 4% |
| 2019 Research | <1% | 1% | 12% | 4% | 2% | 3% |
| 2009 Education | 2% | 4% | 8% | 8% | 6% | 4% |
| 2014 Education | 4% | 7% | 10% | 9% | 6% | 7% |
| 2019 Education | 3% | 7% | 12% | 11% | 7% | 7% |
| 2009 Other d | 1% | 1% | 25% | 5% | 2% | 5% |
| 2014 Other d | 1% | 2% | 24% | 3% | 2% | 6% |
| 2019 Other d | 1% | 2% | 29% | 3% | 1% | 6% |
| Year of Licensure Cohort (Year of First Licensure) | Female Gender | Age (years) | Hold PharmD Degree | Residency Training | Have Both PharmD and Residency | % (Medication Provider) | % (Medication Provider who also Provides Patient Care) | % (Other Activity Pharmacist) | % (Patient Care Provider who also Provides Medication) | % (Patient Care Provider) |
|---|---|---|---|---|---|---|---|---|---|---|
| 2009 Survey Data | ||||||||||
| 2005 to 2006 (n = 23) | 70% | 30.9 | 96% | 30% | 30% | 52% | 4% | 9% | 13% | 22% |
| 2000 to 2004 (n = 101) | 66% | 33.7 | 75% | 22% | 21% | 33% | 23% | 18% | 20% | 7% |
| 1995 to 1999 (n = 136) | 67% | 38.2 | 46% | 13% | 13% | 31% | 27% | 18% | 19% | 5% |
| 1990 to 1994 (n = 142) | 66% | 42.0 | 30% | 14% | 14% | 44% | 23% | 12% | 11% | 10% |
| 1985 to 1989 (n = 141) | 58% | 47.0 | 17% | 6% | 6% | 38% | 26% | 17% | 15% | 4% |
| 1980 to 1984 (n =164) | 50% | 51.2 | 20% | 7% | 6% | 35% | 29% | 21% | 9% | 6% |
| 1975 to 1979 (n = 188) | 39% | 55.6 | 12% | 6% | 3% | 47% | 23% | 16% | 9% | 5% |
| 1970 to 1974 (n = 133) | 22% | 60.7 | 7% | 3% | 0% | 39% | 30% | 17% | 8% | 6% |
| 1965 to 1969 (n = 74) | 10% | 65.4 | 5% | 7% | 3% | 47% | 24% | 18% | 10% | 1% |
| 1960 to 1964 (n = 41) | 10% | 70.0 | 8% | 3% | 3% | 71% | 20% | 7% | 2% | 0% |
| Before 1960 (n = 33) | 6% | 77.1 | 9% | 0% | 0% | 73% | 21% | 6% | 0% | 0% |
| OVERALL (N = 1176) | 47% | 51.6 | 26% | 9% | 8% | 41% | 25% | 16% | 12% | 6% |
| 2014 Survey Data | ||||||||||
| 2010 to 2013 (n = 111) | 63% | 30.5 | 96% | 28% | 28% | 37% | 23% | 8% | 21% | 11% |
| 2005 to 2009 (n = 174) | 71% | 33.9 | 95% | 22% | 22% | 35% | 24% | 15% | 17% | 9% |
| 2000 to 2004 (n = 153) | 71% | 38.3 | 85% | 27% | 26% | 34% | 24% | 17% | 16% | 9% |
| 1995 to 1999 (n = 137) | 72% | 43.7 | 52% | 16% | 14% | 39% | 23% | 21% | 12% | 5% |
| 1990 to 1994 (n = 157) | 66% | 47.5 | 31% | 13% | 11% | 41% | 19% | 20% | 15% | 5% |
| 1985 to 1989 (n = 147) | 61% | 52.1 | 28% | 8% | 6% | 40% | 21% | 22% | 11% | 7% |
| 1980 to 1984 (n = 165) | 51% | 55.9 | 18% | 8% | 4% | 38% | 23% | 19% | 12% | 9% |
| 1975 to 1979 (n = 162) | 36% | 60.9 | 18% | 10% | 2% | 48% | 19% | 20% | 9% | 6% |
| 1970 to 1974 (n = 73) | 21% | 65.3 | 18% | 5% | 2% | 41% | 22% | 19% | 8% | 10% |
| 1965 to 1969 (n = 39) | 18% | 69.7 | 9% | 16% | 3% | 49% | 18% | 21% | 10% | 3% |
| 1960 to 1964 (n = 15) | 13% | 74.5 | 0% | 0% | 0% | 80% | 13% | 7% | 0% | 0% |
| Before 1960 (n = 5) | 20% | 78.0 | 0% | 0% | 0% | 40% | 0% | 40% | 0% | 20% |
| OVERALL (N = 1338) | 60% | 48.1 | 50% | 15% | 13% | 40% | 22% | 18% | 13% | 7% |
| 2019 Survey Data | ||||||||||
| 2015 to 2019 (n = 842) | 68% | 30.4 | 97% | 22% | 22% | 34% | 28% | 6% | 17% | 16% |
| 2010 to 2014 (n = 1054) | 69% | 33.6 | 98% | 22% | 22% | 32% | 25% | 11% | 18% | 14% |
| 2005 to 2009 (n = 404) | 75% | 39.0 | 95% | 23% | 23% | 31% | 21% | 16% | 17% | 16% |
| 2000 to 2004 (n = 296) | 73% | 43.4 | 80% | 11% | 11% | 33% | 25% | 17% | 13% | 12% |
| 1995 to 1999 (n = 397) | 74% | 48.6 | 43% | 9% | 9% | 39% | 26% | 12% | 14% | 9% |
| 1990 to 1994 (n = 515) | 70% | 52.1 | 28% | 8% | 6% | 35% | 24% | 19% | 12% | 10% |
| 1985 to 1989 (n = 413) | 62% | 56.2 | 22% | 7% | 5% | 34% | 26% | 20% | 10% | 10% |
| 1980 to 1984 (n = 372) | 55% | 60.5 | 15% | 10% | 5% | 35% | 24% | 19% | 12% | 10% |
| 1975 to 1979 (n = 245) | 37% | 65.0 | 18% | 5% | 4% | 40% | 19% | 25% | 8% | 8% |
| 1970 to 1974 (n = 102) | 28% | 69.9 | 18% | 10% | 5% | 38% | 24% | 20% | 11% | 9% |
| 1965 to 1969 (n = 27) | 7% | 75.1 | 11% | 4% | 0% | 37% | 22% | 19% | 11% | 11% |
| 1960 to 1964 (n = 13) | 31% | 76.5 | 8% | 0% | 0% | 62% | 23% | 8% | 8% | 0% |
| Before 1960 (n = 6) | 0% | 88.8 | 17% | 17% | 17% | 17% | 17% | 17% | 17% | 33% |
| OVERALL (N = 4686) | 65% | 44.4 | 64% | 15% | 14% | 34% | 25% | 14% | 15% | 12% |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Schommer, J.; Doucette, W.; Witry, M.; Arya, V.; Bakken, B.; Gaither, C.; Kreling, D.; Mott, D. Pharmacist Segments Identified from 2009, 2014, and 2019 National Pharmacist Workforce Surveys: Implications for Pharmacy Organizations and Personnel. Pharmacy 2020, 8, 49. https://doi.org/10.3390/pharmacy8020049
Schommer J, Doucette W, Witry M, Arya V, Bakken B, Gaither C, Kreling D, Mott D. Pharmacist Segments Identified from 2009, 2014, and 2019 National Pharmacist Workforce Surveys: Implications for Pharmacy Organizations and Personnel. Pharmacy. 2020; 8(2):49. https://doi.org/10.3390/pharmacy8020049
Chicago/Turabian StyleSchommer, Jon, William Doucette, Matthew Witry, Vibhuti Arya, Brianne Bakken, Caroline Gaither, David Kreling, and David Mott. 2020. "Pharmacist Segments Identified from 2009, 2014, and 2019 National Pharmacist Workforce Surveys: Implications for Pharmacy Organizations and Personnel" Pharmacy 8, no. 2: 49. https://doi.org/10.3390/pharmacy8020049
APA StyleSchommer, J., Doucette, W., Witry, M., Arya, V., Bakken, B., Gaither, C., Kreling, D., & Mott, D. (2020). Pharmacist Segments Identified from 2009, 2014, and 2019 National Pharmacist Workforce Surveys: Implications for Pharmacy Organizations and Personnel. Pharmacy, 8(2), 49. https://doi.org/10.3390/pharmacy8020049







