Interventional, Quasi-Experimental Study of a Chronic Obstructive Pulmonary Disease Education Care Plan for Hospital Discharge
Abstract
:1. Introduction
2. Materials and Methods
2.1. Study Design
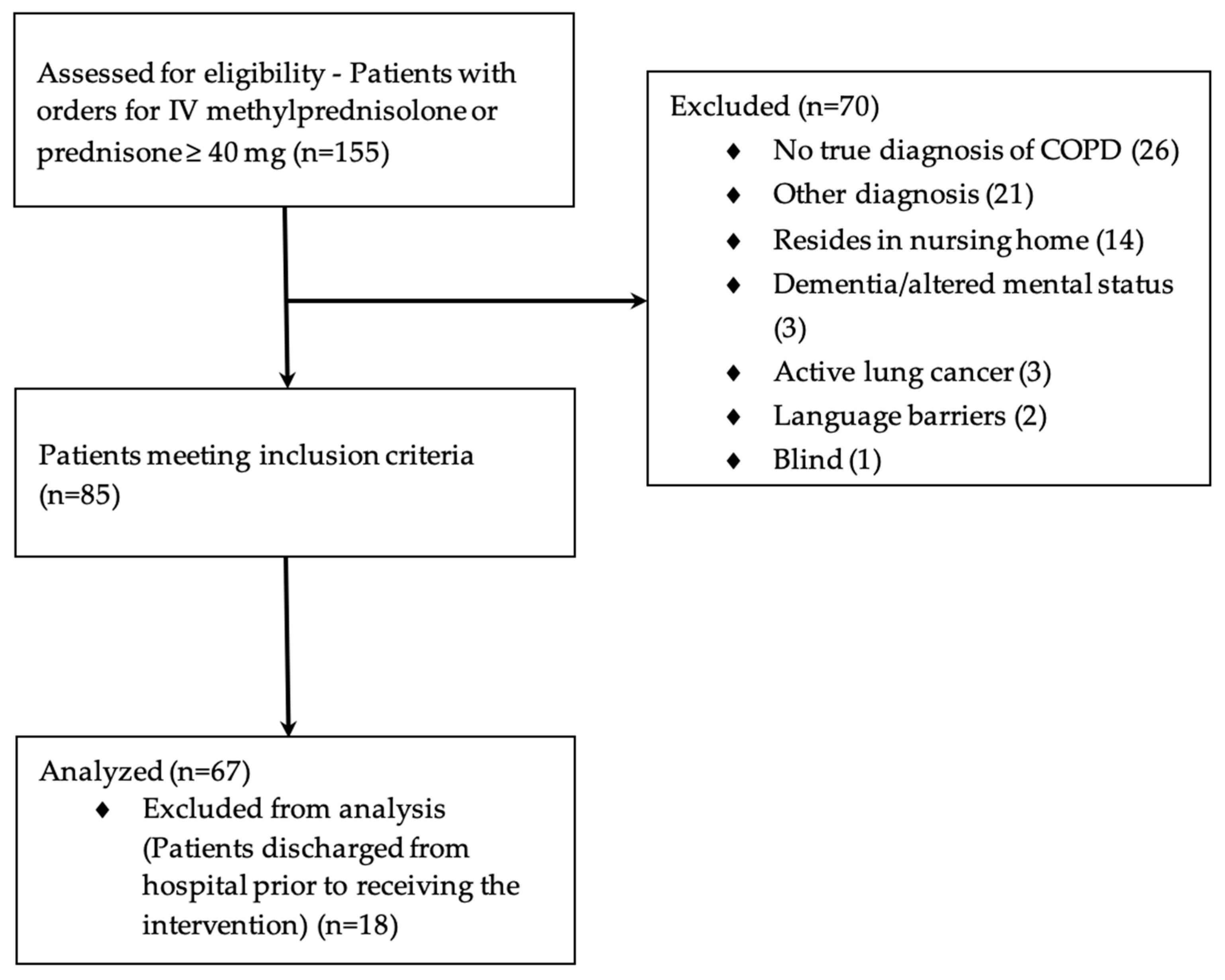
2.2. Participants
2.3. Intervention
2.4. Outcomes
2.5. Data Collection
2.6. Statistical Methods
3. Results
3.1. Participants
3.2. Primary Outcomes
3.3. Secondary Outcomes
4. Discussion
4.1. Primary Outcomes
4.2. Secondary Outcomes
4.3. Strengths
4.4. Limitations
4.5. Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Acknowledgments
Conflicts of Interest
Appendix A. Inhaler Device Checklists
| Step | Before | After |
| Understands what disease the inhaler is used for | ||
| Understands difference between short-acting and long-acting inhaler |
| Step Number | Step | Before | After |
| 1 | Remove cap | ||
| 2 | Check dose counter (understands purpose) | ||
| 3 | Hold inhaler upright and shake well | ||
| 4 | Breathe out gently, away from the inhaler | ||
| 5 | Put mouthpiece between teeth without biting and close lips to form good seal | ||
| 6 | Breathe in slowly through mouth while pressing down firmly on canister | ||
| 7 | Hold breath for about 5–10 s or as long as comfortable | ||
| 8 | While holding breath, remove inhaler from mouth | ||
| 9 | Breathe out gently, away from the inhaler | ||
| 10 | Repeat steps (2 to 10) for additional dose if needed | ||
| 11 | Replace cap when finished |
| Step | Before | After |
| Understands what disease the inhaler is used for | ||
| Understands difference between short-acting and long-acting inhaler |
| Step Number | Step | Before | After |
| 1 | Check dose counter (understands purpose) | ||
| 2 | Hold inhaler upright with the cap closed | ||
| 3 | Turn base in direction of arrows until it clicks | ||
| 4 | Open the cap until it snaps fully open | ||
| 5 | Breathe out gently, away from inhaler | ||
| 6 | Close lips around mouthpiece to form a good seal; do not cover air vents | ||
| 7 | Breathe in slowly and deeply while pressing down firmly on the dose button | ||
| 8 | Hold breath for 5–10 s or as long as comfortable | ||
| 9 | Breathe out gently, away from inhaler | ||
| 10 | Repeat steps to get the full dose of two inhalations (if needed) | ||
| 11 | Click cap shut when finished |
| Step | Before | After |
| Understands what disease the inhaler is used for | ||
| Understands difference between short-acting and long-acting inhaler |
| Step Number | Step | Before | After |
| 1 | Open cap | ||
| 2 | Flip open mouthpiece | ||
| 3 | Remove capsule from blister and place in chamber | ||
| 4 | Close mouthpiece until it clicks | ||
| 5 | Press green piercing button in once and release (do not shake) | ||
| 6 | Breathe out gently, away from inhaler | ||
| 7 | Place mouthpiece between teeth without biting and close lips to form a good seal | ||
| 8 | Breathe in slowly and deeply, so capsule vibrates | ||
| 9 | Keep breathing in as long as comfortable | ||
| 10 | While holding breath, remove inhaler from mouth | ||
| 11 | Breathe out gently, away from inhaler | ||
| 12 | Repeat steps (7–11) to take the full dose | ||
| 13 | Open mouthpiece and remove capsule | ||
| 14 | Close mouthpiece and cap when finished |
| Step | Before | After |
| Understands what disease the inhaler is used for | ||
| Understands difference between short-acting and long-acting inhaler |
| Step Number | Step | Before | After |
| 1 | Check dose counter (understands purpose) | ||
| 2 | Slide the cover down until it clicks to activate dose (do not shake) | ||
| 3 | Breathe out gently, away from the inhaler | ||
| 4 | Close lips around mouthpiece to form a good seal; do not cover air vents | ||
| 5 | Breathe in steadily and deeply | ||
| 6 | Hold breath for 5–10 s or as long as comfortable | ||
| 7 | While holding breath, remove inhaler from mouth | ||
| 8 | Breathe out gently, away from the inhaler | ||
| 9 | Slide the cover upwards to cover the mouthpiece when finished |
| Step | Before | After |
| Understands what disease the inhaler is used for | ||
| Understands difference between short-acting and long-acting inhaler |
| Step Number | Step | Before | After |
| 1 | Check dose counter (understands purpose) | ||
| 2 | Open cover using thumb grip | ||
| 3 | Hold horizontally, load dose by sliding lever until it clicks | ||
| 4 | Breathe out gently, away from the inhaler | ||
| 5 | Place mouthpiece in mouth and close lips to form a good seal, keep inhaler horizontal | ||
| 6 | Breathe in steadily and deeply | ||
| 7 | Hold breath for about 5–10 s or as long as comfortable | ||
| 8 | While holding breath, remove inhaler from mouth | ||
| 9 | Breathe out gently, away from the inhaler | ||
| 10 | Repeat inhalation to ensure dose is complete | ||
| 11 | Close cover to click shut when finished |
| Step | Before | After |
| Understands what disease the inhaler is used for | ||
| Understands difference between short-acting and long-acting inhaler |
| Step Number | Step | Before | After |
| 1 | Check dose counter (understands purpose) | ||
| 2 | Remove cap all the way down until you hear the click | ||
| 3 | Breathe out gently, away from the inhaler | ||
| 4 | Put mouthpiece between teeth without biting and close lips to form good seal | ||
| 5 | Breathe in slowly and deeply through mouth | ||
| 6 | Hold breath for about 5–10 s or as long as comfortable | ||
| 7 | While holding breath, remove inhaler from mouth | ||
| 8 | Breathe out gently, away from the inhaler | ||
| 9 | Repeat steps (2 to 10) for additional dose if needed | ||
| 10 | Replace cap when finished |
Appendix B
| Device Type | Inhaler Type | Propellant | Comments |
| Pressurized Metered Dose Inhaler | pMDI | Yes | Variety of medication formulations |
| Respimat® | SMI | No | Variety of medication formulations |
| HandiHaler® | DPI | No | Specific to Spiriva® |
| Ellipta® | DPI | No | Variety of medication formulations |
| Diskus® | DPI | No | Variety of medication formulations |
| Respiclick® | DPI | No | Variety of medication formulations |
| Abbreviations: DPI, dry powder inhaler; pMDI, pressurized metered dose inhaler; SMI, soft mist inhaler. | |||
References
- Global Initiative for Chronic Obstructive Lung Disease. Global Strategy for the Diagnosis, Management, and Prevention of Chronic Obstructive Pulmonary Disease (Updated 2019). Available online: http://goldcopd.org/ (accessed on 23 November 2021).
- Leading Causes of Death and Numbers of Deaths, by Sex, Race, and Hispanic Origin: United States, 1980 and 2014 (Table 19). In Health, United States, 2019; National Center for Health Statistics: Hyattsville, MD, USA, 2021.
- Stein, B.D.; Charbeneau, J.T.; Lee, T.A.; Schumock, G.T.; Lindenauer, P.K.; Bautista, A.; Lauderdale, D.S.; Naureckas, E.T.; Krishnan, J.A. Hospitalizations for acute exacerbations of chronic obstructive pulmonary disease: How you count matters. COPD J. Chronic Obstr. Pulm. Dis. 2010, 7, 164–171. [Google Scholar]
- Jencks, S.F.; Williams, M.V.; Coleman, E.A. Rehospitalizations among patients in the Medicare fee-for-service program. N. Eng. J. Med. 2009, 360, 1418–1428. [Google Scholar]
- Hardin, L.; Kilian, A.; Murphy, E. Bundled payments for care improvement: Preparing for the medical diagnosis-related groups. J. Nurs. Adm. 2017, 47, 313–319. [Google Scholar]
- CMS.gov—Centers for Medicare and Medicaid Services. Readmission Reduction Program. Available online: https://www.cms.gov/Medicare/Quality-Initiatives-Patient-Assessment-Instruments/Value-Based-Programs/HRRP/Hospital-Readmission-Reduction-Program.html (accessed on 23 November 2021).
- American Association for Respiratory Care. Reducing Hospital Readmissions for COPD. Available online: http://www.aarc.org/resources/programs-projects/reducing-hospital-readmissions-for-copd/ (accessed on 23 November 2021).
- Moye, P.M.; Chu, P.S.; Pounds, T.; Thurston, M.M. Impact of a pharmacy team-led intervention program on the readmission rate of elderly patients with heart failure. Am. J. Health Syst. Pharm. 2018, 75, 183–190. [Google Scholar]
- Schumacher, C.; Moaddab, G.; Colbert, M.; Kliethermes, M.A. The effect of clinical pharmacists on readmission rates of heart failure patients in the accountable care environment. J. Manag. Care Spec. Pharm. 2018, 24, 795–799. [Google Scholar]
- Shiwaku, E.; Dote, S.; Kaneko, S.; Hei, C.; Aikawa, M.; Sakai, Y.; Kawai, T.; Iwatsubo, S.; Hashimoto, M.; Tsuneishi, T. Pharmacist involvement in the inhaler choice improves lung function in patients with COPD: A prospective single-arm study. J. Pharm. Health Care Sci. 2021, 7, 28. [Google Scholar]
- Valentino, A.S.; Eddy, E.; Woods, Z.; Wilken, L. Pharmacist provided spirometry services: A scoping review. Integr. Pharm. Res. Pract. 2021, 10, 93–111. [Google Scholar]
- Petite, S.E.; Hess, M.W.; Wachtel, H. The role of the pharmacist in inhaler selection and education in chronic obstructive pulmonary disease. J. Pharm. Technol. 2021, 37, 95–106. [Google Scholar]
- Aerosol Drug Management Improvement Team (ADMIT); Sanchis, J.; Gich, I.; Pedersen, S. Systematic review of rrrors in inhaler use: Has patient technique improved over time? Chest 2016, 150, 394–406. [Google Scholar]
- Usmani, O.S.; Lavorini, F.; Marshall, J.; Dunlop, W.C.N.; Heron, L.; Farrington, E.; Dekhuiyzen, R. Critical inhaler errors in asthma and COPD: A systematic review of impact on health outcomes. Respir. Res. 2018, 19, 10. [Google Scholar]
- Ahn, J.H.; Chung, J.H.; Shin, K.C.; Jin, H.J.; Jang, J.G.; Lee, M.S.; Lee, K.H. The effects of repeated inhaler device handling education in COPD patients: A prospective cohort study. Sci. Rep. 2020, 10, 19676. [Google Scholar]
- Pothirat, C.; Chaiwong, W.; Phetsuk, N.; Pisalthanapuna, S.; Chetsadaphan, N.; Choomuang, W. Evaluating inhaler use technique in COPD patients. Int. J. Chron. Obstr. Pulm. Dis. 2015, 10, 1291–1298. [Google Scholar]
- Roggeri, A.; Micheletto, C.; Roggeri, D.P. Inhalation errors due to device switch in patients with chronic obstructive pulmonary disease and asthma: Critical health and economic issues. Int. J. Chron. Obstr. Pulm. Dis. 2016, 11, 597–602. [Google Scholar]
- Joint Commission of Pharmacy Practitioners. Pharmacists’ Patient Care Process. Available online: https://jcpp.net/wp-content/uploads/2016/03/PatientCareProcess-with-supporting-organizations.pdf (accessed on 1 December 2021).
- National Asthma Council Australia: Inhaler Technique Checklists. Available online: https://nationalasthma.org.au/resources/InhalerTechniqueChecklist (accessed on 23 November 2021).
- Mahon, J.; Fitzgerald, A.; Glanville, J.; Dekhuijzen, R.; Glatte, J.; Glanemann, S.; Torvinen, S. Misuse and/or treatment delivery failure of inhalers among patients with asthma or COPD: A review and recommendations for the conduct of future research. Respir. Med. 2017, 129, 98–116. [Google Scholar]
- Wilcoxon, F. Individual comparisons by ranking methods. Biometrics 1945, 1, 80–83. [Google Scholar]
- McNemar, Q. Note on the sampling error of the difference between correlated proportions or percentages. Psychometrika 1947, 12, 153–157. [Google Scholar]
- Lindh, A.; Theander, K.; Arne, M.; Lisspers, K.; Lundh, L.; Sandelowsky, H.; Ställberg, B.; Westerdahl, E.; Zakrisson, A. Errors in inhaler use related to devices and to inhalation technique among patients with chronic obstructive pulmonary disease in primary health care. Nurs. Open 2019, 6, 1519–1527. [Google Scholar]
- Purohit, A.N.; Patel, P.P.; Gandhi, A.M.; Desai, M.K. An evaluation of impact of educational interventions on the technique of use of metered-dose inhaler by patients. Indian J. Pharmacol. 2017, 49, 194–200. [Google Scholar]
- Van Boven, J.F.; Stuurman-Bieze, A.G.; Hiddink, E.G.; Postma, M.J. Effects of targeting disease and medication management interventions towards patients with COPD. Curr. Med. Res. Opin. 2016, 32, 229–239. [Google Scholar]
- Maricoto, T.; Monteiro, L.; Gama, J.M.R.; Correia de Sousa, J.; Taborda Barata, L. Inhaler technique education and exacerbation risk in older adults with asthma or chronic obstructive pulmonary disease: A meta-analysis. J. Am. Geriatr. Soc. 2019, 67, 57–66. [Google Scholar]
- Bouros, D.; Evangeliou, M.N. Critical steps: A non-interventional, multicenter, prospective, observational study on critical handling errors with DPI use, in asthma and COPD patients. J. Pulm. Respir. Med. 2016, 6, 360. [Google Scholar]
- Stein, S.W.; Thiel, C.G. The history of therapeutic aerosols: A chronological review. J. Aerosol Med. Pulm. Drug Deliv. 2017, 30, 20–41. [Google Scholar]

| Component | Intervention |
|---|---|
| Target population | Patients with a diagnosis of acute COPD exacerbation residing on the general hospital floors prior to discharge Patients admitted to the ICU were screened once transferred to the general hospital floors Patients with prior use of the inhaler device type prior to hospital admission |
| Patient identification | Patients with active orders for intravenous methylprednisolone or prednisone 40 mg or more with an indication of COPD exacerbation identified by institution report |
| Assessment of appropriate medication regimen | Based on GOLD Guideline criteria per the patient’s GOLD status Identify medications for optimization Inform medical team prior to patient discharge for correction |
| Individualized inhaler education and discharge counseling | Assess patient understanding of inhaler administration using scored checklist for each inhaler to determine baseline education Conduct face-to-face training session: Educate patient on proper inhaler technique, timing of inhalers, and proper storage Provide educational material to aid in inhaler education Reassess patient understanding of inhaler administration using scored checklist for each inhaler after education session Medication education will be documented in patient chart |
| Demographic | n = 67 |
|---|---|
| Age (yr), mean (SD) | 68 (±11) |
| Female, n (%) | 30 (45) |
| Oxygen requirements prior to admission (L), mean (SD) | 1.1 (±1.4) |
| Presence of comorbidities, n (%) | |
| Heart failure | 21 (31) |
| Diabetes | 13 (19) |
| Coronary artery disease | 20 (30) |
| Hypertension | 44 (66) |
| Hyperlipidemia | 26 (39) |
| Obesity | 19 (28) |
| Obstructive sleep apnea | 19 (28) |
| Smoking history, n (%) | |
| Current | 27 (40) |
| Previous | 35 (52) |
| Never | 5 (8) |
| COPD exacerbations in previous year, n (%) | |
| 0 | 22 (33) |
| 1 | 17 (26) |
| 2 | 14 (21) |
| 3 | 14 (20) |
| Inhaler medications prior to admission, n (%) | |
| LABA or LAMA | 4 (6) |
| LABA and LAMA | 7 (10) |
| LABA and ICS | 14 (21) |
| LABA, LAMA, and ICS | 42 (63) |
| Baseline | Follow-Up | p-Value | |
|---|---|---|---|
| Median percent score on checklist a (IQR) | 81.8 (67.5–97.0) | 100.0 (90.0–100.0) | p < 0.0001 |
| Proportion of patients correctly identifying when to use short-acting versus long-acting inhalers types b, n (%) | 49 (73.1) | 66 (98.5) | p < 0.0001 |
| Most Common Incorrect Steps | Prior to Education n (%) | After Education n (%) | p-Value a |
|---|---|---|---|
| Metered Dose Inhaler (pMDI) (n = 62) | |||
| Hold inhaler upright and shake well | 34 (55) | 12 (19) | p < 0.0001 |
| Repeat steps for additional dose if needed | 33 (53) | 12 (19) | p < 0.0001 |
| Check dose counter | 23 (37) | 4 (6) | p < 0.0001 |
| Respimat® (n = 24) | |||
| Repeat steps to get the full dose of two inhalations | 15 (63) | 8 (33) | p = 0.016 |
| Hold inhaler upright with the cap closed | 15 (63) | 2 (8) | p < 0.0001 |
| Close lips around mouthpiece; do not cover air vents | 14 (58) | 7 (29) | p = 0.016 |
| HandiHaler® (n = 18) | |||
| Repeat steps to take the full dose | 9 (50) | 2 (11) | p = 0.016 |
| Press green piercing button in once and release | 5 (28) | 0 (0) | p = 0.063 |
| Close mouthpiece until it clicks | 3 (17) | 0 (0) | |
| Ellipta® (n = 16) | |||
| Check dose counter | 7 (44) | 4 (25) | p = 0.250 |
| Slide cover down until it clicks; do not shake | 6 (38) | 2 (13) | p = 0.219 |
| Close lips around mouthpiece; do not cover air vents | 6 (38) | 1 (6) | p = 0.063 |
| Diskus® (n = 13) | |||
| Check dose counter | 3 (23) | 1 (8) | |
| Repeat inhalation to ensure dose is complete | 3 (23) | 0 (0) | |
| Hold breath for 5-10 s or as long as comfortable | 2 (15) | 0 (0) | |
| Respiclick® (n = 3) | |||
| Remove cap all the way down until you hear the click | 2 (66) | 0 (0) | |
| Breathe in slowly and deeply through mouth | 2 (66) | 0 (0) | |
| Repeat steps for additional dose if needed | 2 (66) | 2 (66) |
| Item | n = 67 |
|---|---|
| Number of patients with pharmacist interventions, n (%) | 25 (36) |
| Adjustment to medication regimen | 12 (18) |
| Refills prior to discharge | 11 (16) |
| Recommendation due to medication cost | 2 (3) |
| Additional topics reviewed during education session, n (%) | |
| Smoking cessation education | 6 (9) |
| Item | Time (min) |
|---|---|
| Patient chart review and interventions prior to education, mean (SD) | 15.9 (±2.8) |
| Baseline checklist and inhaler education, mean (SD) | 16.6 (±3.7) |
| Follow-up checklist and reinforcement of inhaler education, mean (SD) | 11.8 (±2.7) |
| Total time spent, mean (SD) | 44.3 (±6.4) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Warunek, L.N.; Cieri-Hutcherson, N.E.; Kersten, B.P.; Hassan, A.K. Interventional, Quasi-Experimental Study of a Chronic Obstructive Pulmonary Disease Education Care Plan for Hospital Discharge. Pharmacy 2021, 9, 202. https://doi.org/10.3390/pharmacy9040202
Warunek LN, Cieri-Hutcherson NE, Kersten BP, Hassan AK. Interventional, Quasi-Experimental Study of a Chronic Obstructive Pulmonary Disease Education Care Plan for Hospital Discharge. Pharmacy. 2021; 9(4):202. https://doi.org/10.3390/pharmacy9040202
Chicago/Turabian StyleWarunek, Letitia N., Nicole E. Cieri-Hutcherson, Brian P. Kersten, and Amany K. Hassan. 2021. "Interventional, Quasi-Experimental Study of a Chronic Obstructive Pulmonary Disease Education Care Plan for Hospital Discharge" Pharmacy 9, no. 4: 202. https://doi.org/10.3390/pharmacy9040202
APA StyleWarunek, L. N., Cieri-Hutcherson, N. E., Kersten, B. P., & Hassan, A. K. (2021). Interventional, Quasi-Experimental Study of a Chronic Obstructive Pulmonary Disease Education Care Plan for Hospital Discharge. Pharmacy, 9(4), 202. https://doi.org/10.3390/pharmacy9040202






