Urbanization and Health Expenditure: An Empirical Investigation from Households in Vietnam
Abstract
:1. Introduction
2. Related Literature
2.1. Impacts of Urbanization on Health and Health Expenditure
2.1.1. Impacts of Urbanization on Health
2.1.2. Impacts of Urbanization on Health Expenditure
2.2. Underlying Pathways of the Effects of Urbanization on Health Expenditure
3. Sample Construction
3.1. Data Source
3.2. Variable Definitions
4. Research Methodology
4.1. Baseline Models: Fixed-Effect Regressions
4.2. Two-Stage Least Square Regressions
4.3. Plausibly Exogenous IV
5. Empirical Findings
5.1. Main Results
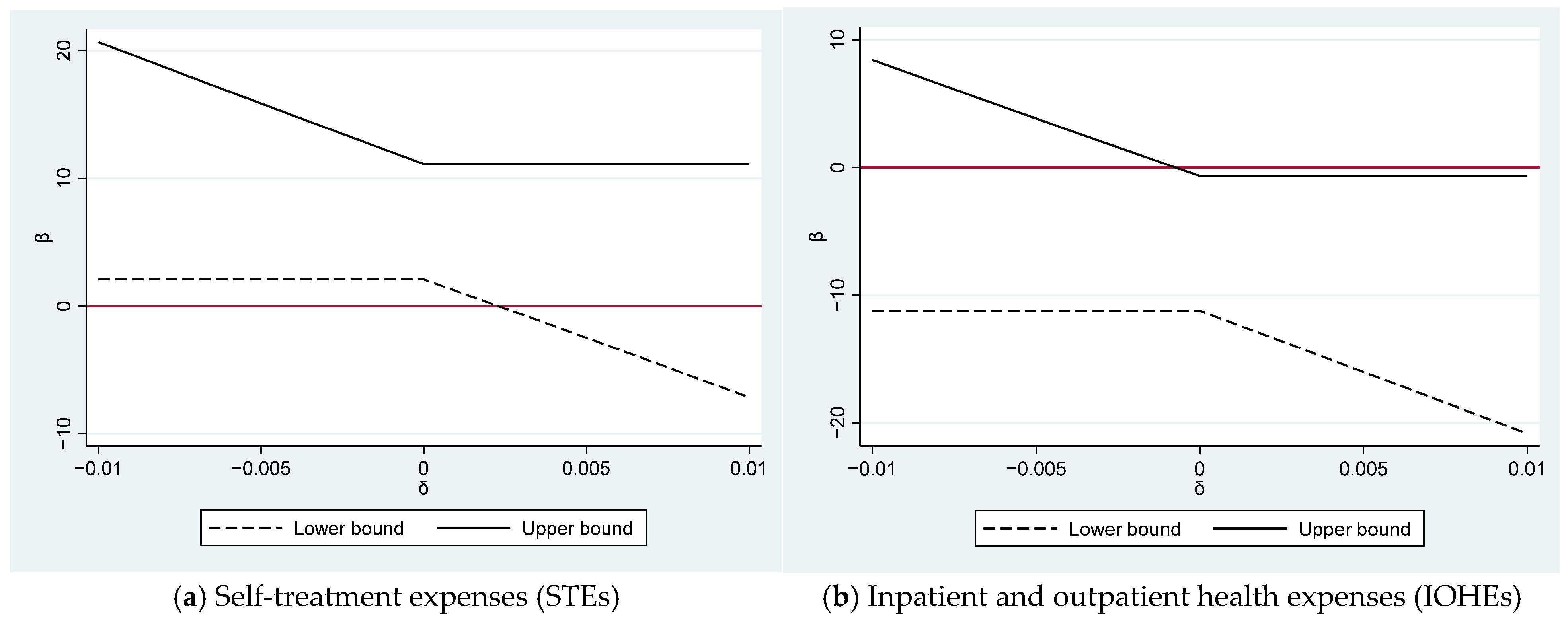
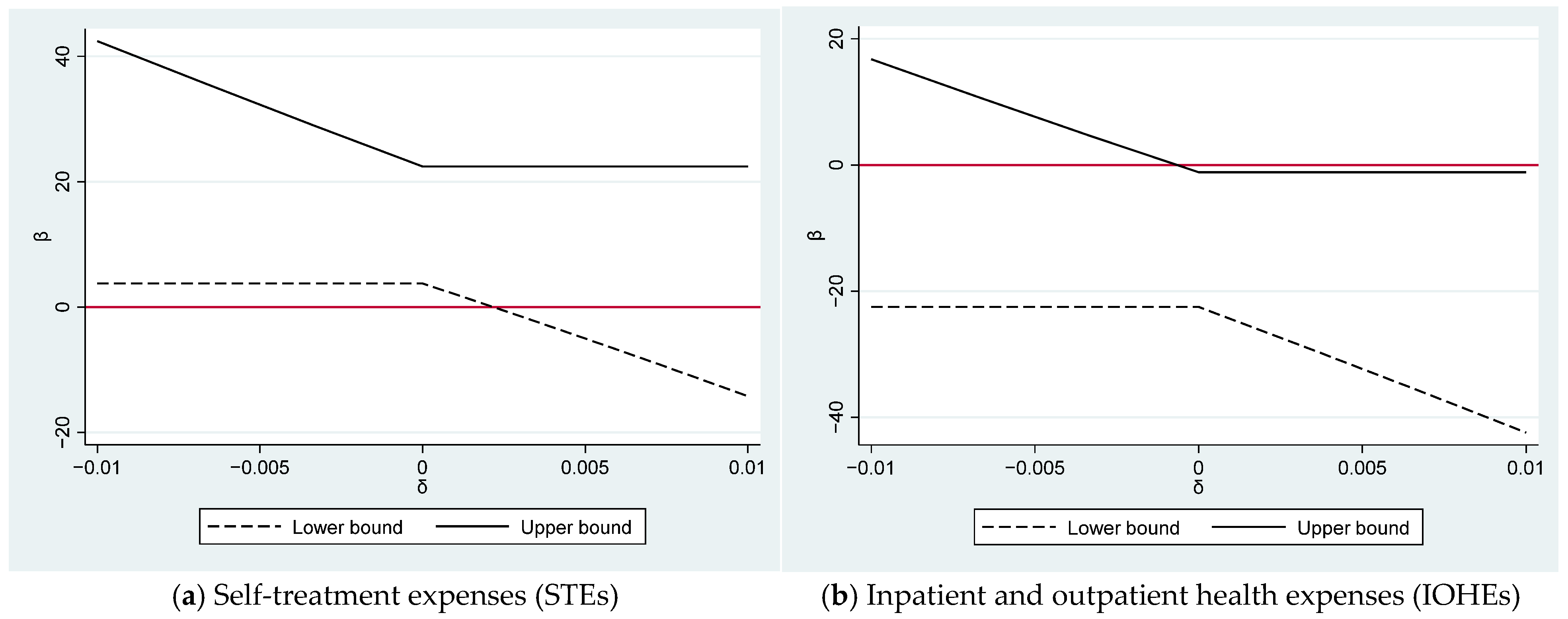
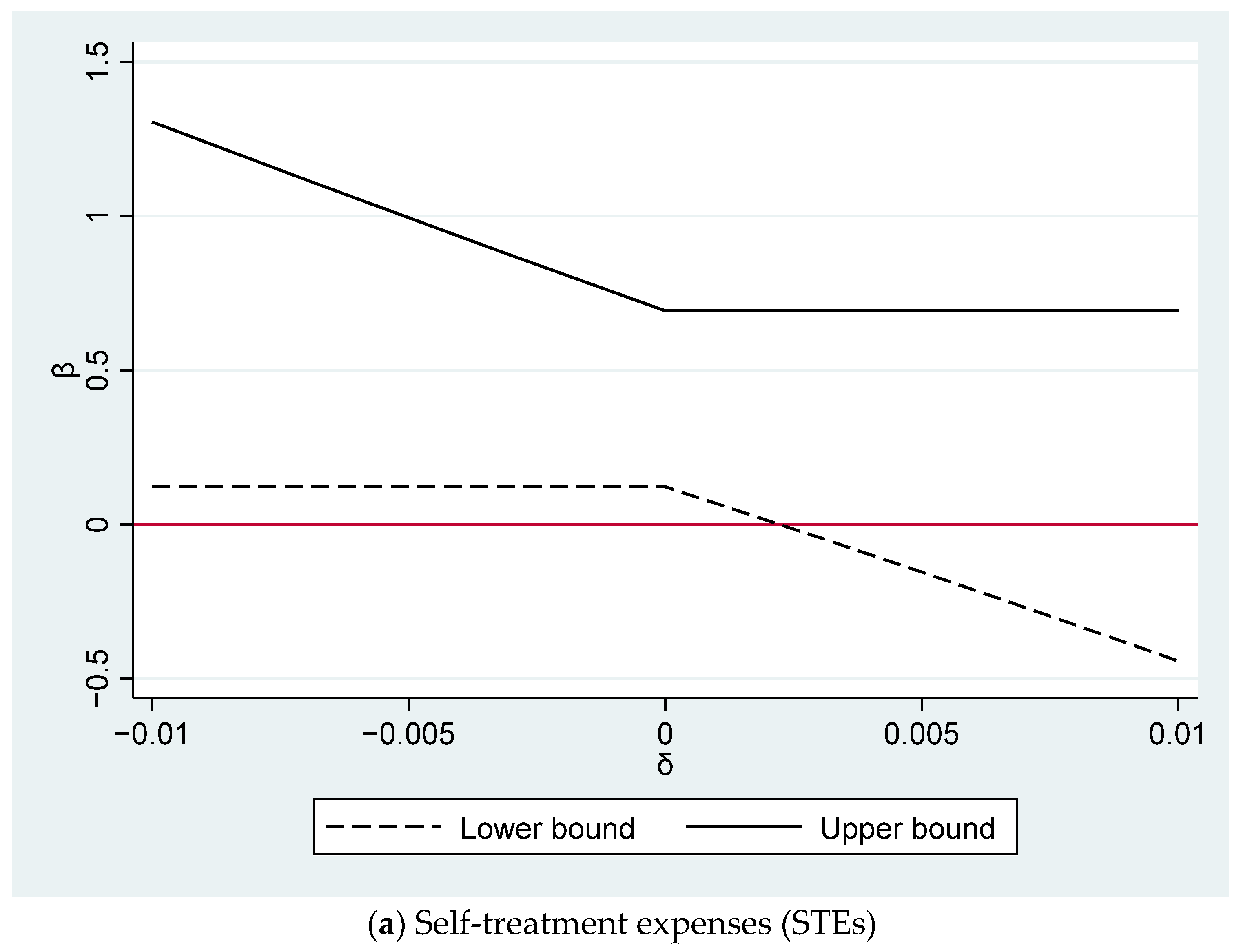
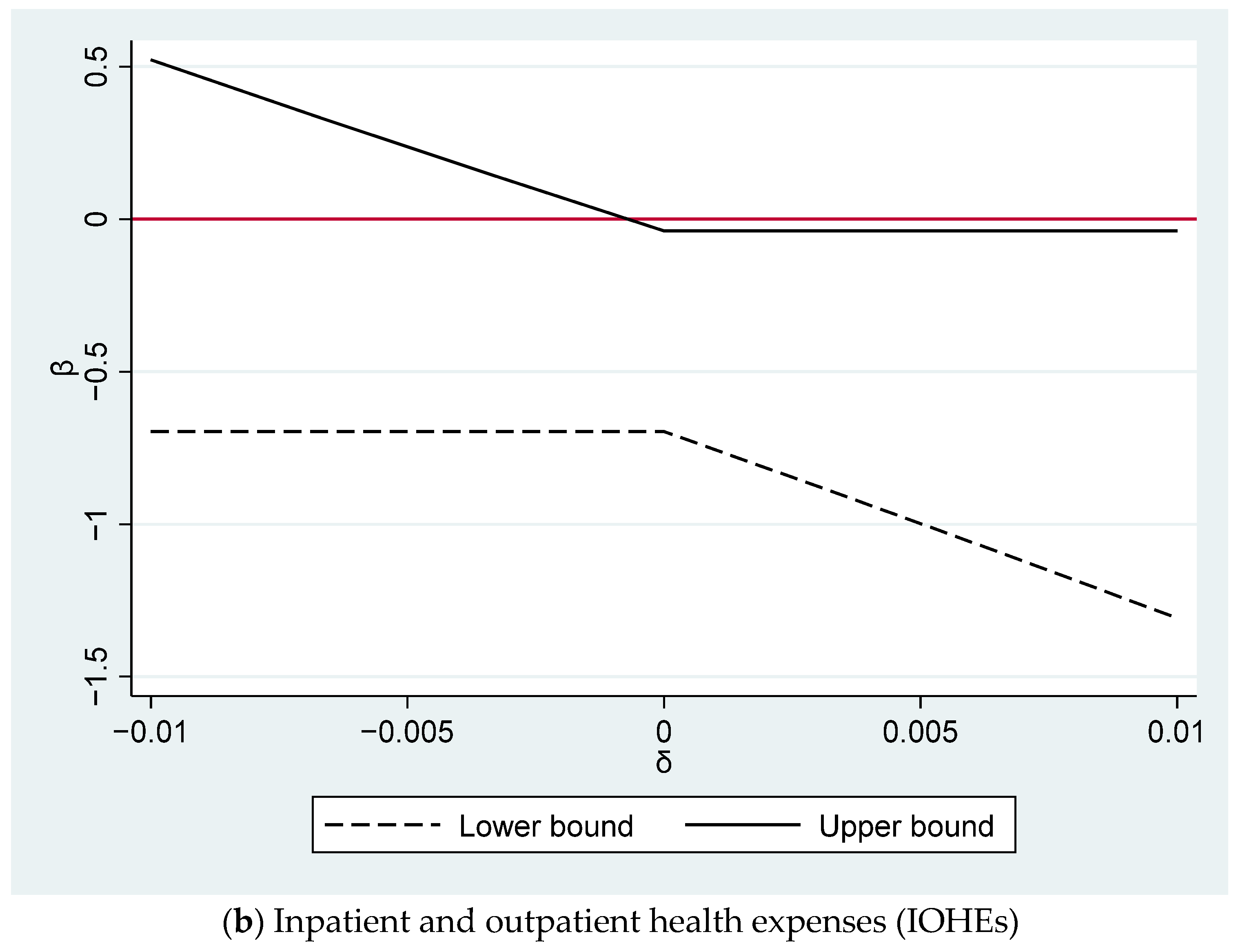
5.2. Plausible Exogeneous IV
5.3. Mechanisms
6. Conclusions and Policy Recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. Supporting Results
| In/Outpatient Health Expenses | Self-Treatment Expenses | Relative Urban Population | ICTIndex | |
|---|---|---|---|---|
| In/outpatient health expenses | 1 | |||
| Self-treatment expenses | 0.1918 | 1 | ||
| Relative urban population | 0.0418 | 0.1012 | 1 | |
| ICTIndex | 0.0939 | 0.1451 | 0.5863 | 1 |
| Observations | 16,786 | 16,786 | 16,786 | 16,786 |
| In/Outpatient Health Expenses | Self-Treatment Expenses | |
|---|---|---|
| Relative urban population | −0.364 ** | 0.344 ** |
| (0.180) | (0.154) | |
| Head of household’s age | 0.017 | 0.020 |
| (0.022) | (0.018) | |
| Age squared | −0.000 | −0.000 |
| (0.000) | (0.000) | |
| Head of household’s gender | −0.182 | −0.131 |
| (0.146) | (0.134) | |
| Head of household’s level of education | 0.053 | −0.002 |
| (0.044) | (0.037) | |
| Head of household’s marital status | 0.379 *** | 0.281 ** |
| (0.139) | (0.135) | |
| Location of residence | −1.460 | 3.016 *** |
| (1.056) | (0.888) | |
| Household size | 0.090 *** | 0.115 *** |
| (0.028) | (0.022) | |
| Dependency ratio | −0.266 | 0.150 |
| (0.196) | (0.173) | |
| Home ownership | 0.052 | −0.209 |
| (0.153) | (0.131) | |
| Log of total asset value | 0.106 *** | 0.104 *** |
| (0.035) | (0.030) | |
| Provincial unemployment rate | 0.004 | 0.035 ** |
| (0.020) | (0.017) | |
| Log of province’s revenue | 0.309 *** | −0.067 |
| (0.107) | (0.088) | |
| Observations | 16,786 | 16,786 |
| R-squared | −0.043 | −0.024 |
| Number of households | 6582 | 6582 |
| In/Outpatient Health Expenses | Self-Treatment Expenses | |
|---|---|---|
| Panel A: Standard errors are clustered at household level | ||
| Relative urban population | −0.364 ** | 0.344 ** |
| (0.179) | (0.157) | |
| Number of observations | 16,786 | 16,786 |
| R-squared | −0.043 | −0.024 |
| Number of households | 6582 | 6582 |
| Under. Id. | 72.948 | 72.948 |
| Weak id. | 71.349 | 71.349 |
| Panel B: Standard errors are clustered at commune level | ||
| Relative urban population | −0.364 ** | 0.344 ** |
| (0.169) | (0.165) | |
| Number of observations | 16,786 | 16,786 |
| R-squared | −0.043 | −0.024 |
| Number of households | 6582 | 6582 |
| Under. Id. | 16.037 | 16.037 |
| Weak id. | 30.468 | 30.468 |
| Panel C: Standard errors are clustered at district level | ||
| Relative urban population | −0.364 * | 0.344 * |
| (0.169) | (0.165) | |
| Number of observations | 16,786 | 16,786 |
| R-squared | −0.043 | −0.024 |
| Number of households | 6582 | 6582 |
| Under. Id. | 27.321 | 27.321 |
| Weak id. | 26.611 | 26.611 |
Appendix B. Additional Results for Conley’s Methods
| Variables | IOHEs | STEs | ||||
|---|---|---|---|---|---|---|
| Coef | Ro_std | 95% CI | Coef | Ro_std | 95% CI | |
| Panel A. Effect of relative urban population on IOHEs and STEs | ||||||
| Relative urban population | −0.368 ** | 0.177 | [−0.715; −0.020] | 0.408 *** | 0.156 | [0.101; 0.714] |
| Control variables | Yes | Yes | ||||
| Yes | Yes | |||||
| Observations | 16,786 | 16,786 | ||||
| Panel B. Effect of log of urban population on IOHEs and STEs | ||||||
| Log of urban population | −5.951 ** | 2.848 | [−11.533; −0.369] | 6.598 *** | 2.484 | [1.730; 11.466] |
| Control variables | Yes | Yes | ||||
| Yes | Yes | |||||
| Observations | 16,786 | 16,786 | ||||
| Panel C. Effect of log of population density on IOHEs and STEs | ||||||
| Log of population density | −11.822 ** | 5.747 | [−23.085; −0.559] | 13.108 ** | 5.094 | [3.124; 23.091] |
| Control variables | Yes | Yes | ||||
| Yes | Yes | |||||
| Observations | 16,786 | 16,786 | ||||
| 1 | It is worth mentioning that urbanization significantly impacts the socioeconomic dynamics of households. The process of urbanization offers numerous advantages, including improved infrastructure, expanded employment prospects, broader markets, and enhanced allocation of resources (Obi-Ani and Isiani 2020). Nonetheless, urbanization can heighten income inequality, widening the gap between affluent and impoverished households (Chen et al. 2016). |
| 2 | The in situ urbanization policy is often referred to as the process of converting villages into urban neighborhoods, which is closely connected to the commonly used term “reclassification”. This involves changing the nature of settlements from rural to urban areas. |
| 3 | It is worth noting that we perform the Hausman specification test as a means to compare the fixed-effect regression with the random-effect counterpart. The associated chi-square statistics are equal to 78.66 and 129.48 for IOHEs and STEs, respectively. Accordingly, the null hypothesis is rejected at the 1% significance level for both IOHEs and STEs. This result demonstrates that when assessing the influences of urbanization on health expenditure, the fixed-effect regression emerges as the most suitable empirical methodology. |
| 4 | The xttest3 command in Stata is utilized for assessing heteroskedasticity, and the results reveal the presence of heteroskedasticity within our sample. |
| 5 | The expansion in health insurance coverage is in line with the efforts of the Vietnamese government to expand health insurance coverage across the whole country, primarily through the national health insurance program. |
References
- Al-Hanawi, Mohammed Khaled, Martin Limbikani Mwale, and Tony Mwenda Kamninga. 2020. The effects of health insurance on health-seeking behaviour: Evidence from the kingdom of Saudi Arabia. Risk Management and Healthcare Policy 13: 595–607. [Google Scholar] [CrossRef] [PubMed]
- Anderson, Michael, Carlos Dobkin, and Tal Gross. 2012. The effect of health insurance coverage on the use of medical services. American Economic Journal: Economic Policy 4: 1–27. [Google Scholar] [CrossRef]
- Attard, S. M., A. H. Herring, E. J. Mayer-Davis, B. M. Popkin, James Benjamin Meigs, and P. Gordon-Larsen. 2012. Multilevel examination of diabetes in modernising China: What elements of urbanisation are most associated with diabetes? Diabetologia 55: 3182–92. [Google Scholar] [CrossRef] [PubMed]
- Chen, Guo, Amy K. Glasmeier, Min Zhang, and Yang Shao. 2016. Urbanization and income inequality in post-reform China: A causal analysis based on time series data. PLoS ONE 11: e0158826. [Google Scholar] [CrossRef] [PubMed]
- Clarke, Damian, and Benjamín Matta. 2018. Practical considerations for questionable IVs. The Stata Journal 18: 663–91. [Google Scholar] [CrossRef]
- Conley, Timothy G., Christian B. Hansen, and Peter E. Rossi. 2012. Plausibly exogenous. Review of Economics and Statistics 94: 260–72. [Google Scholar] [CrossRef]
- Çetin, Mümin Atalay, and İbrahim Bakırtaş. 2019. Does urbanization induce the health expenditures? A dynamic macro-panel analysis for developing countries. Dumlupınar Üniversitesi Sosyal Bilimler Dergisi 61: 208–22. Available online: https://dergipark.org.tr/en/download/article-file/762975 (accessed on 2 April 2024).
- Danaei, Goodarz, Gitanjali M. Singh, Christopher J. Paciorek, John K. Lin, Melanie J. Cowan, Mariel M. Finucane, Farshad Farzadfar, Gretchen A. Stevens, Leanne M. Riley, Yuan Lu, and et al. 2013. The global cardiovascular risk transition: Associations of four metabolic risk factors with national income, urbanization, and Western diet in 1980 and 2008. Circulation 127: 1493–502. [Google Scholar] [CrossRef] [PubMed]
- Dang, Thang. 2018. Do the more educated utilize more health care services? Evidence from Vietnam using a regression discontinuity design. International Journal of Health Economics and Management 18: 277–99. [Google Scholar] [CrossRef]
- Duc Thanh, Nguyen, Bui Thi My Anh, Phung Thanh Hung, Pham Quynh Anh, and Chu Huyen Xiem. 2021. Impact of public health insurance on out-of-pocket health expenditures of the near-poor in Vietnam. Health Services Insights 14: 11786329211017411. [Google Scholar] [CrossRef]
- Dye, Christopher. 2008. Health and urban living. Science 319: 766–69. [Google Scholar] [CrossRef] [PubMed]
- Ettner, Susan L. 1996. New evidence on the relationship between income and health. Journal of Health Economics 15: 67–85. [Google Scholar] [CrossRef] [PubMed]
- Frijters, Paul, John P. Haisken-DeNew, and Michael A. Shields. 2005. The causal effect of income on health: Evidence from German reunification. Journal of Health Economics 24: 997–1017. [Google Scholar] [CrossRef] [PubMed]
- Fu, Qiang, and Kenneth C. Land. 2017. Does urbanisation matter? A temporal analysis of the socio-demographic gradient in the rising adulthood overweight epidemic in China, 1989–2009. Population, Space and Place 23: e1970. [Google Scholar] [CrossRef]
- Gollin, Douglas, Remi Jedwab, and Dietrich Vollrath. 2016. Urbanization with and without industrialization. Journal of Economic Growth 21: 35–70. [Google Scholar] [CrossRef]
- Gong, Peng, Song Liang, Elizabeth J. Carlton, Qingwu Jiang, Jianyong Wu, Lei Wang, and Justin V. Remais. 2012. Urbanisation and health in China. The Lancet 379: 843–52. [Google Scholar] [CrossRef] [PubMed]
- Guo, Shiqi. 2020. The legacy effect of unexploded bombs on educational attainment in Laos. Journal of Development Economics 147: 102527. [Google Scholar] [CrossRef]
- Harmon, Colm, and Brian Nolan. 2001. Health insurance and health services utilization in Ireland. Health Economics 10: 135–45. [Google Scholar] [CrossRef]
- Ifeagwu, Susan C., Justin C. Yang, Rosalind Parkes-Ratanshi, and Carol Brayne. 2021. Health financing for universal health coverage in Sub-Saharan Africa: A systematic review. Global Health Research and Policy 6: 8. [Google Scholar] [CrossRef]
- Jowett, Matthew, Anil Deolalikar, and Peter Martinsson. 2004. Health insurance and treatment seeking behaviour: Evidence from a low-income country. Health Economics 13: 845–57. [Google Scholar] [CrossRef]
- Levine, David, Rachel Polimeni, and Ian Ramage. 2016. Insuring health or insuring wealth? An experimental evaluation of health insurance in rural Cambodia. Journal of Development Economics 119: 1–15. [Google Scholar] [CrossRef]
- Li, Xinhu, Cuiping Wang, Guoqin Zhang, Lishan Xiao, and Jane Dixon. 2012. Urbanisation and human health in China: Spatial features and a systemic perspective. Environmental Science and Pollution Research 19: 1375–84. [Google Scholar] [CrossRef] [PubMed]
- Lim, Ming Yao, Hanin Farhana Kamaruzaman, Olivia Wu, and Claudia Geue. 2023. Health financing challenges in Southeast Asian countries for universal health coverage: A systematic review. Archives of Public Health 81: 148. [Google Scholar] [CrossRef]
- Marmot, Michael. 2002. The influence of income on health: Views of an epidemiologist. Health Affairs 21: 31–46. [Google Scholar] [CrossRef] [PubMed]
- Meierrieks, Daniel, and Laura Renner. 2023. Islamist terrorism and the status of women. European Journal of Political Economy 78: 102364. [Google Scholar] [CrossRef]
- Miao, Jia, and Xiaogang Wu. 2016. Urbanization, socioeconomic status and health disparity in China. Health & Place 42: 87–95. [Google Scholar]
- Nguyen-Phung, Hang Thu, and Hai Le. 2024. Energy Poverty and Health Expenditure: Empirical Evidence from Vietnam. Social Sciences 13: 253. [Google Scholar] [CrossRef]
- Obi-Ani, Ngozika Anthonia, and Mathias Chukwudi Isiani. 2020. Urbanization in Nigeria: The onitsha experience. Cities 104: 102744. [Google Scholar] [CrossRef]
- Raza, Wameq A., Ellen Van de Poel, Arjun Bedi, and Frans Rutten. 2016. Impact of community-based health insurance on access and financial protection: Evidence from three randomized control trials in rural India. Health Economics 25: 675–87. [Google Scholar] [CrossRef]
- Shao, Qi, Ran Tao, and Magda Mihaela Luca. 2022. The effect of urbanization on health care expenditure: Evidence from China. Frontiers in Public Health 10: 207. [Google Scholar] [CrossRef]
- Shen, Yu, and Wenkai Sun. 2023. From Villages to Urban Neighborhoods: Urbanization and Health. China & World Economy 31: 37–158. [Google Scholar]
- Sparrow, Robert, Asep Suryahadi, and Wenefrida Widyanti. 2013. Social health insurance for the poor: Targeting and impact of Indonesia’s Askeskin programme. Social Science & Medicine 96: 264–71. [Google Scholar]
- Thanh, Nguyen Duc, Bui Thi My Anh, Chu Huyen Xiem, and Hoang Van Minh. 2019. Out-of-pocket health expenditures among insured and uninsured patients in Vietnam. Asia Pacific Journal of Public Health 31: 210–18. [Google Scholar] [CrossRef] [PubMed]
- Thornton, James A., and Jennifer L. Rice. 2008. Determinants of healthcare spending: A state level analysis. Applied Economics 40: 2873–89. [Google Scholar] [CrossRef]
- Van de Poel, Ellen, Owen O’Donnell, and Eddy Van Doorslaer. 2012. Is there a health penalty of China’s rapid urbanization? Health Economics 21: 367–85. [Google Scholar] [CrossRef] [PubMed]
- Wagstaff, Adam, and Magnus Lindelow. 2008. Can insurance increase financial risk?: The curious case of health insurance in China. Journal of Health Economics 27: 990–1005. [Google Scholar] [CrossRef]
- Wang, Jiankang, and Zetao Xu. 2023. Analysis of the effect of heterogeneous human capital on new urbanization in China. Economic Research-Ekonomska Istraživanja 36: 2180649. [Google Scholar] [CrossRef]
- Wang, Zijun. 2009. The determinants of health expenditures: Evidence from US state-level data. Applied Economics 41: 429–35. [Google Scholar] [CrossRef]
- Waters, Hugh R., Gerard F. Anderson, and Jim Mays. 2004. Measuring financial protection in health in the United States. Health Policy 69: 339–49. [Google Scholar] [CrossRef]
- Yang, Gonghuan, Yu Wang, Yixin Zeng, George F. Gao, Xiaofeng Liang, Maigeng Zhou, Xia Wan, Shicheng Yu, Yuhong Jiang, Mohsen Naghavi, and et al. 2013. Rapid health transition in China, 1990–2010: Findings from the Global Burden of Disease Study 2010. The Lancet 381: 1987–2015. [Google Scholar] [CrossRef]
- Zhang, Zhenhua, Mingcheng Zhao, Yunpeng Zhang, and Yanchao Feng. 2023. How does urbanization affect public health? New evidence from 175 countries worldwide. Frontiers in Public Health 10: 1096964. [Google Scholar] [CrossRef] [PubMed]
- Zheng, Wei, and Patrick Paul Walsh. 2019. Economic growth, urbanization and energy consumption—A provincial level analysis of China. Energy Economics 80: 153–62. [Google Scholar] [CrossRef]
- Zheng, Xiaoting, Anqi Wu, and Xuejing Wei. 2023. The social support returns to college education in China: Evidence from online medical crowdfunding. China Economic Review 79: 101978. [Google Scholar] [CrossRef]
- Zhu, Enyan, Qiuyu Qi, Lisu Chen, and Xianhua Wu. 2022. The spatial-temporal patterns and multiple driving mechanisms of carbon emissions in the process of urbanization: A case study in Zhejiang, China. Journal of Cleaner Production 358: 131954. [Google Scholar] [CrossRef]
| Variables | Type | Description | Source |
|---|---|---|---|
| Inpatient and outpatient health expenses | Continuous | Natural log of a sum of hospitalization and outpatient costs | VHLSS |
| Self-treatment expenses | Continuous | Natural log of a sum of household’s expenditure on medicines without prescription and household’s expenditure on medical facilities | VHLSS |
| Urbanization | Continuous | Average urban population by province | Statistical Yearbook of General Statistics Offices of Vietnam |
| Relative urban intensity | Continuous | Urban population divided by total population for each province | Statistical Yearbook of General Statistics Offices of Vietnam |
| Age of the household head | Continuous | Age of the household head | VHLSS |
| Marital status | Categorical | Marital status of the household head | VHLSS |
| Level of education | Categorical | Level of education of the household head | VHLSS |
| Male | Dummy | Gender of the household head | VHLSS |
| Rural | Dummy | Location of residence: whether rural or urban | VHLSS |
| Household size | Continuous | Household size | VHLSS |
| Dependent ratio | Continuous | Ratio of dependent people (less than 6 years old and greater than 60 years old) | VHLSS |
| Total value of household assets | Continuous | Total value of assets in the household | VHLSS |
| Home ownership | Categorical | Household owns house or not | VHLSS |
| Government revenue | Continuous | Government revenue at provincial level | Ministry of Finance |
| Unemployment rates | Continuous | Unemployment rate at provincial level | Statistical Yearbook of General Statistics Offices of Vietnam |
| Expenditure on insurance | Continuous | Natural log of household’s expenditure on health insurance | VHLSS |
| Household’s total income | Continuous | Household’s income in the last 12 months (thousand VND) | VHLSS |
| Variables | N | Mean | SD | Min | Max |
|---|---|---|---|---|---|
| Log of in/outpatient health expenses | 16,786 | 6.781 | 2.350 | 0 | 13.12 |
| Log of self-treatment expenses | 16,786 | 5.676 | 2.097 | 0 | 17.03 |
| Relative urban population | 16,786 | 29.21 | 18.70 | 9.718 | 87.28 |
| ICT Index | 16,786 | 44.99 | 12.19 | 9.130 | 94.07 |
| Head of household’s age | 16,786 | 51.33 | 13.97 | 13 | 105 |
| Head of household’s age squared | 16,786 | 2830 | 1547 | 169 | 11,025 |
| Head of household’s male | 16,786 | 0.752 | 0.432 | 0 | 1 |
| Head of household’s level of education | 16,786 | 1.533 | 1.192 | 0 | 4 |
| Head of household’s marital status | 16,786 | 0.803 | 0.397 | 0 | 1 |
| Household size | 16,786 | 3.833 | 1.570 | 1 | 13 |
| Dependent ratio | 16,786 | 0.239 | 0.217 | 0 | 1 |
| House ownership | 16,786 | 0.964 | 0.185 | 0 | 1 |
| Location of residence | 16,786 | 0.709 | 0.454 | 0 | 1 |
| Log of total asset value | 16,786 | 9.922 | 1.305 | 3.401 | 14.85 |
| Log of province’s revenue | 16,786 | 15.60 | 1.497 | 11.47 | 19.75 |
| Provincial unemployment rate | 16,786 | 2.216 | 3.310 | 0 | 19 |
| FE | FEIV | |
|---|---|---|
| Panel A: Inpatient and outpatient health expenses (IOHEs) | (A1) | (A2) |
| Relative urban population | −0.011 | −0.364 ** |
| (0.015) | (0.180) | |
| Number of observations | 16,786 | 16,786 |
| R-squared | 0.008 | −0.043 |
| Number of households | 6582 | 6582 |
| Kleibergen–Paap rk LM statistic (Underidentification test) | 80.2 | |
| Kleibergen–Paap rk Wald F statistic (Weak identification test) | 78.565 | |
| First-stage results | ||
| ICT Index | 0.021 *** | |
| (0.002) | ||
| Panel B: Self-treatment expenses (STEs) | (B1) | (B2) |
| Relative urban population | 0.058 *** | 0.344 ** |
| (0.013) | (0.154) | |
| Number of observations | 16,786 | 16,786 |
| R-squared | 0.025 | −0.024 |
| Number of households | 6582 | 6582 |
| Kleibergen–Paap rk LM statistic (Underidentification test) | 80.2 | |
| Kleibergen–Paap rk Wald F statistic (Weak identification test) | 78.565 | |
| First-stage results | ||
| ICT Index | 0.021 *** | |
| (0.002) |
| In/Outpatient Health Expenses | Self-Treatment Expenses | In/Outpatient Health Expenses | Self-Treatment Expenses | |
|---|---|---|---|---|
| Log of urban population | −5.549 ** | 5.240 ** | ||
| (2.712) | (2.321) | |||
| Log of population density | −11.160 ** | 10.539 ** | ||
| (5.575) | (4.809) | |||
| Number of observations | 16,786 | 16,786 | 16,786 | 16,786 |
| R-squared | −0.023 | 0.014 | −0.123 | −0.123 |
| Number of households | 6582 | 6582 | 6582 | 6582 |
| Under. Id. | 174.424 | 174.424 | 67.768 | 67.768 |
| Weak id. | 172.159 | 172.159 | 67.463 | 67.463 |
| First-stage results | ||||
| ICT Index | 0.001 *** | 0.001 *** | 0.001 *** | 0.001 *** |
| (0.0001) | (0.0001) | (0.0001) | (0.0001) |
| Inpatient and Outpatient Health Expenses | Self-Treatment Expenses | |
|---|---|---|
| Relative urban population | −0.044 * | 0.077 *** |
| (0.025) | (0.020) | |
| Number of observations | 16,786 | 16,786 |
| R-squared | 0.007 | 0.025 |
| Number of households | 6582 | 6582 |
| Kleibergen–Paap rk LM statistic (Underidentification test) | 926.43 | 926.43 |
| Kleibergen–Paap rk Wald F statistic (Weak identification test) | 450.797 | 450.797 |
| Hansen J statistics (Overidentification test) | 3.375 | 3.114 |
| Hansen J statistics (p-value) | 0.066 | 0.078 |
| First-stage results | ||
| ICT Index | 0.014 *** | 0.014 *** |
| (0.002) | (0.002) | |
| Lag of relative urban population | 0.517 *** | 0.517 *** |
| (0.017) | (0.017) |
| (A1) | (A2) | |
|---|---|---|
| Insurance Expense | Household’s Total Income | |
| Relative urban population | 0.780 *** | 9422.991 *** |
| (0.213) | (3189.222) | |
| Number of observations | 16,786 | 12,704 |
| R-squared | −0.141 | −0.065 |
| Number of households | 6582 | 5046 |
| Kleibergen–Paap rk LM statistic (Underidentification test) | 80.2 | 56.812 |
| Kleibergen–Paap rk Wald F statistic (Weak identification test) | 78.565 | 55.614 |
| First-stage results | ||
| ICT Index | 0.021 *** | 0.02 *** |
| (0.002) | (0.003) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Nguyen-Phung, H.T.; Le, H. Urbanization and Health Expenditure: An Empirical Investigation from Households in Vietnam. Economies 2024, 12, 153. https://doi.org/10.3390/economies12060153
Nguyen-Phung HT, Le H. Urbanization and Health Expenditure: An Empirical Investigation from Households in Vietnam. Economies. 2024; 12(6):153. https://doi.org/10.3390/economies12060153
Chicago/Turabian StyleNguyen-Phung, Hang Thu, and Hai Le. 2024. "Urbanization and Health Expenditure: An Empirical Investigation from Households in Vietnam" Economies 12, no. 6: 153. https://doi.org/10.3390/economies12060153
APA StyleNguyen-Phung, H. T., & Le, H. (2024). Urbanization and Health Expenditure: An Empirical Investigation from Households in Vietnam. Economies, 12(6), 153. https://doi.org/10.3390/economies12060153







