College Student Mental Health and Wellbeing Prior to and during the COVID-19 Pandemic
Abstract
:1. Introduction
2. Material and Methods
2.1. Survey Design and Procedure
2.2. Sample
Variables and Instruments
2.3. Data Analysis
3. Results
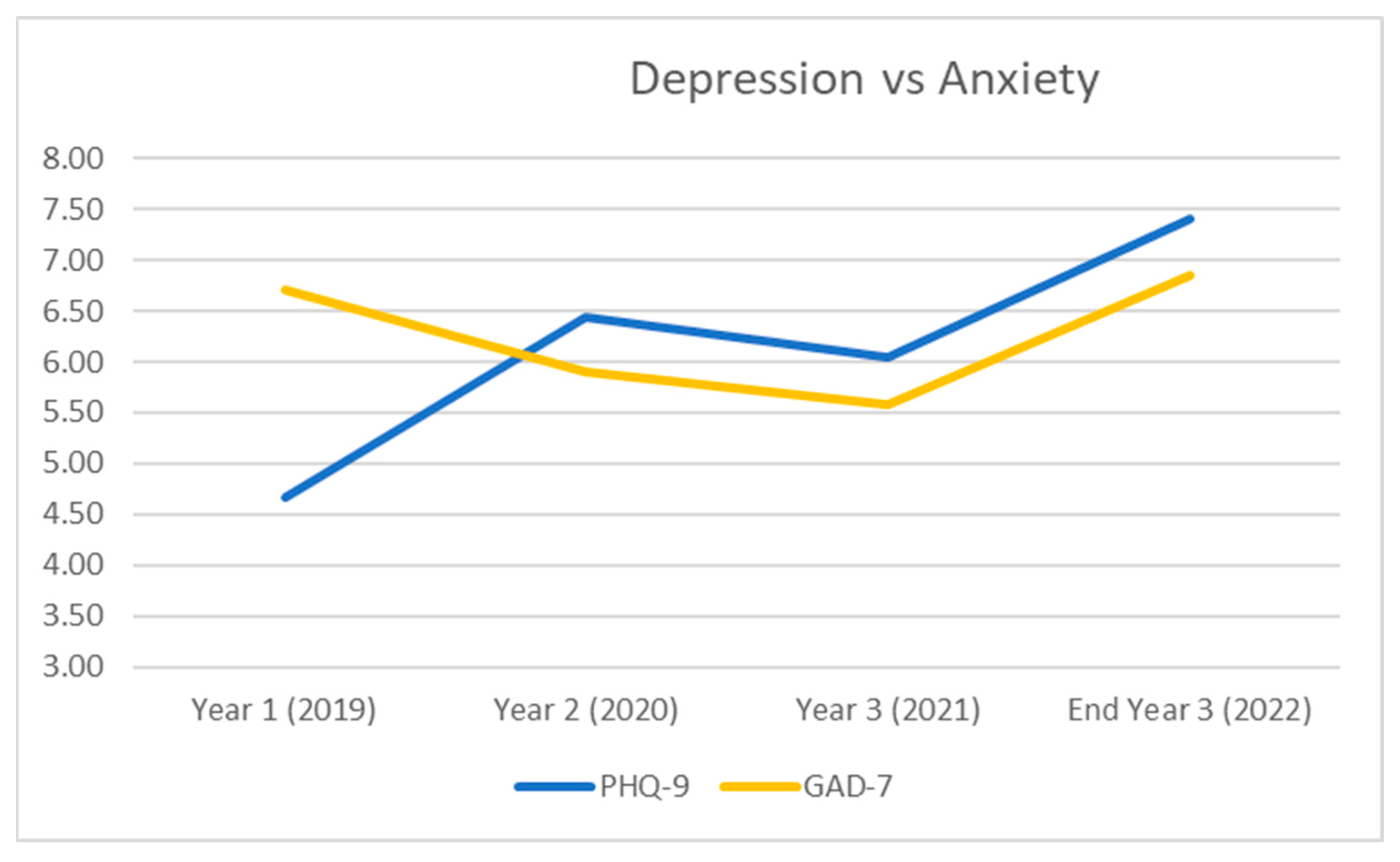
3.1. Depression (PHQ-9) Scores
3.2. Anxiety (GAD-7) Scores
3.3. Impact of Pandemic on College Experiences
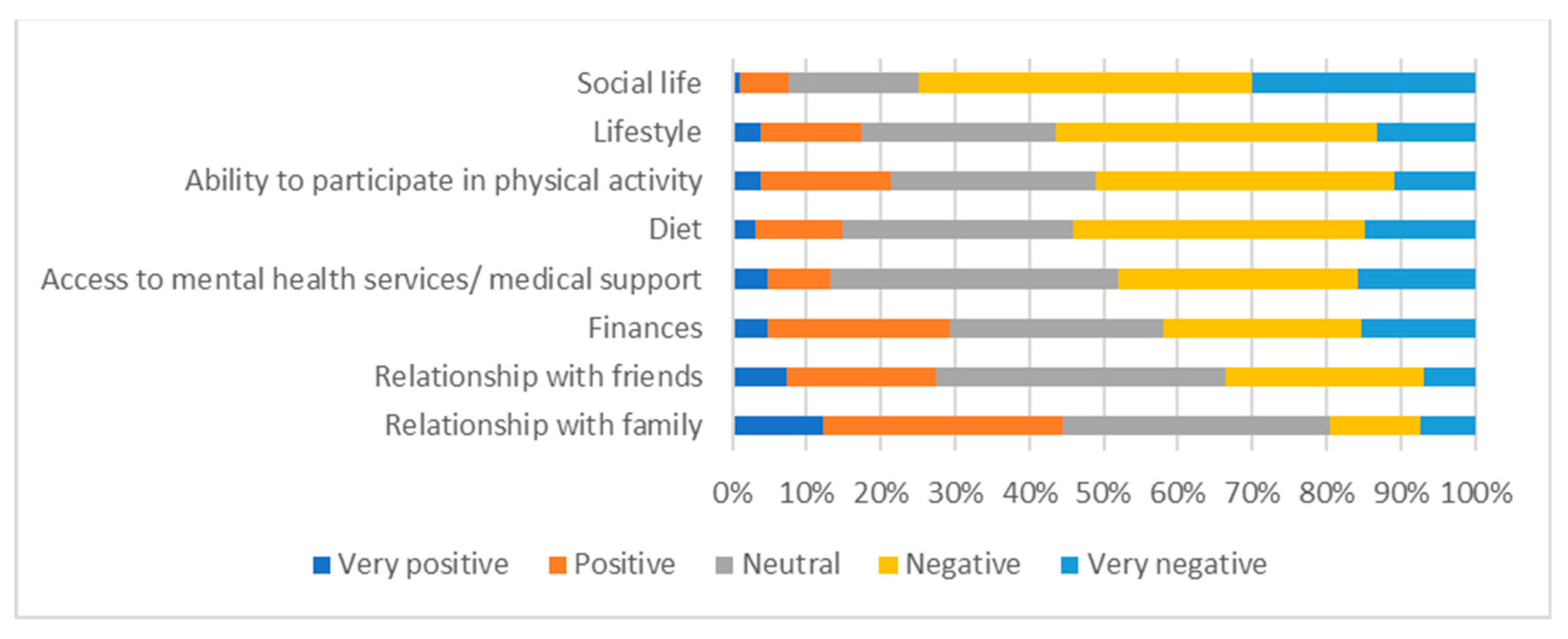
3.4. Impact of Pandemic on Other Aspects of Life
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Auerbach, R.P.; Mortier, P.; Bruffaerts, R.; Alonso, J.; Benjet, C.; Cuijpers, P.; Demyttenaere, K.; Ebert, D.D.; Green, J.G.; Hasking, P.; et al. WHO World Mental Health Surveys International College Student Project: Prevalence and distribution of mental disorders. J. Abnorm. Psychol. 2018, 127, 623–638. [Google Scholar] [CrossRef]
- McLafferty, M.; Lapsley, C.R.; Ennis, E.; Armour, C.; Murphy, S.; Bunting, B.P.; Bjourson, A.J.; Murray, E.K.; O’Neill, S.M. Mental health, behavioural problems and treatment seeking among students commencing university in Northern Ireland. PLoS ONE 2017, 12, e0188785. [Google Scholar] [CrossRef]
- O’Neill, S.; McLafferty, M.; Ennis, E.; Lapsley, C.; Bjourson, T.; Armour, C.; Murphy, S.; Bunting, B.; Murray, E. Socio-demographic, mental health and childhood adversity risk factors for self-harm and suicidal behaviour in College students in Northern Ireland. J. Affect. Disord. 2018, 239, 58–65. [Google Scholar] [CrossRef] [PubMed]
- Horgan, A.; Kelly, P.; Goodwin, J.; Behan, L. Depressive Symptoms and Suicidal Ideation among Irish Undergraduate College Students. Issues Ment. Health Nurs. 2018, 39, 575–584. [Google Scholar] [CrossRef]
- Karyotaki, E.; Klein, A.M.; Riper, H.; de Wit, L.; Krijnen, L.; Bol, E.; Bolinski, F.; Burger, S.; Ebert, D.D.; Auerbach, R.P.; et al. Examining the effectiveness of a web-based intervention for symptoms of depression and anxiety in college students: Study protocol of a randomised controlled trial. BMJ Open 2019, 9, e028739. [Google Scholar] [CrossRef]
- Keeling, S.; Aiken, S.K.o.S.C.; Shaffer, L.S.; Zalewski, J.M.; Gordon, V.N.; Steele, M.J. Advising the Millennial Generation. NACADA J. 2003, 23, 30–36. [Google Scholar] [CrossRef]
- Filho, W.L.; Wall, T.; Rayman-Bacchus, L.; Mifsud, M.; Pritchard, D.J.; Lovren, V.O.; Farinha, C.; Petrovic, D.S.; Balogun, A.-L. Impacts of COVID-19 and social isolation on academic staff and students at universities: A cross-sectional study. BMC Public Health 2021, 21, 1213. [Google Scholar] [CrossRef]
- Zhai, Y.; Du, X. Addressing collegiate mental health amid COVID-19 pandemic. Psychiatry Res. 2020, 288, 113003. [Google Scholar] [CrossRef]
- Wathelet, M.; Duhem, S.; Vaiva, G.; Baubet, T.; Habran, E.; Veerapa, E.; Debien, C.; Molenda, S.; Horn, M.; Grandgenèvre, P.; et al. Factors associated with mental health disorders among College students in France confined during the COVID-19 pandemic. JAMA Netw. Open 2020, 3, e2025591. [Google Scholar] [CrossRef]
- Huckins, J.F.; Dasilva, A.W.; Wang, W.; Hedlund, E.; Rogers, C.; Nepal, S.K.; Wu, J.; Obuchi, M.; I Murphy, E.; Meyer, M.L.; et al. Mental Health and Behavior of College Students During the Early Phases of the COVID-19 Pandemic: Longitudinal Smartphone and Ecological Momentary Assessment Study. J. Med. Internet Res. 2020, 22, e20185. [Google Scholar] [CrossRef]
- Domínguez-González, A.; Guzmán-Valdivia, G.; Ángeles-Téllez, F.; Manjarrez-Ángeles, M.; Secín-Diep, R. Depression and suicidal ideation in Mexican medical students during COVID-19 outbreak. A longitudinal study. Heliyon 2022, 8, e08851. [Google Scholar] [CrossRef] [PubMed]
- Son, C.; Hegde, S.; Smith, A.; Wang, X.; Sasangohar, F. Effects of COVID-19 on College Students’ Mental Health in the United States: Interview Survey Study. J. Med. Internet Res. 2020, 22, e21279. [Google Scholar] [CrossRef] [PubMed]
- Ma, Z.; Zhao, J.; Li, Y.; Chen, D.; Wang, T.; Zhang, Z.; Chen, Z.; Yu, Q.; Jiang, J.; Fan, F.; et al. Mental health problems and correlates among 746 217 college students during the coronavirus disease 2019 outbreak in China. Epidemiol. Psychiatr. Sci. 2020, 29, e181. [Google Scholar] [CrossRef] [PubMed]
- Wang, X.; Hegde, S.; Son, C.; Keller, B.; Smith, A.; Sasangohar, F. Investigating Mental Health of US College Students during the COVID-19 Pandemic: Cross-Sectional Survey Study. J. Med. Internet Res. 2020, 22, e22817. [Google Scholar] [CrossRef]
- Peng, X.; Liang, S.; Liu, L.; Cai, C.; Chen, J.; Huang, A.; Wang, X.; Zhao, J. Prevalence and associated factors of depression, anxiety and suicidality among Chinese high school E-learning students during the COVID-19 lockdown. Curr. Psychol. 2022, 1–12. [Google Scholar] [CrossRef]
- Ward, C.; McLafferty, M.; McLaughlin, J.; McHugh, R.; McBride, L.; Brady, J.; Bjourson, A.J.; Walsh, C.P.; O’Neill, S.M.; Murray, E.K. Suicidal behaviours and mental health disorders among students commencing college. Psychiatry Res. 2021, 307, 114314. [Google Scholar] [CrossRef]
- McLafferty, M.; Brown, N.; McHugh, R.; Ward, C.; Stevenson, A.; McBride, L.; Brady, J.; Bjourson, A.J.; O’Neill, S.M.; Walsh, C.P.; et al. Depression, anxiety and suicidal behaviour among college students: Comparisons pre-COVID-19 and during the pandemic. Psychiatry Res. Commun. 2021, 1, 100012. [Google Scholar] [CrossRef]
- Kessler, R.C.; Santiago, P.N.; Colpe, L.J.; Dempsey, C.L.; First, M.B.; Heeringa, S.G.; Stein, M.B.; Fullerton, C.S.; Gruber, M.J.; Naifeh, J.A.; et al. Clinical reappraisal of the Composite International Diagnostic Interview Screening Scales (CIDI-SC) in the Army Study to Assess Risk and Resilience in Servicemembers (Army STARRS). Int. J. Methods Psychiatr. Res. 2013, 22, 303–321. [Google Scholar] [CrossRef] [PubMed]
- Kroenke, K.; Spitzer, R.L. The PHQ-9: A New Depression Diagnostic and Severity Measure. Psychiatr. Ann. 2002, 32, 509–515. [Google Scholar] [CrossRef]
- Spitzer, R.L.; Kroenke, K.; Williams, J.B.W.; Löwe, B. A Brief Measure for Assessing Generalized Anxiety Disorder: The GAD-7. Arch. Intern. Med. 2006, 166, 1092–1097. [Google Scholar] [CrossRef]
- Fruehwirth, J.C.; Biswas, S.; Perreira, K.M. The Covid-19 pandemic and mental health of first-year college students: Examining the effect of Covid-19 stressors using longitudinal data. PLoS ONE 2021, 16, e0247999. [Google Scholar] [CrossRef]
- Knox, L.; Karantzas, G.C.; Romano, D.; Feeney, J.A.; Simpson, J.A. One year on: What we have learned about the psychological effects of COVID-19 social restrictions: A meta-analysis. Curr. Opin. Psychol. 2022, 46, 101315. [Google Scholar] [CrossRef]
- Racine, N.; McArthur, B.A.; Cooke, J.E.; Eirich, R.; Zhu, J.; Madigan, S. Global Prevalence of Depressive and Anxiety Symptoms in Children and Adolescents During COVID-19: A Meta-analysis. JAMA Pediatr. 2021, 175, 1142–1150. [Google Scholar] [CrossRef] [PubMed]
- Saraswathi, I.; Saikarthik, J.; Kumar, K.S.; Srinivasan, K.M.; Ardhanaari, M.; Gunapriya, R. Impact of COVID-19 outbreak on the mental health status of undergraduate medical students in a COVID-19 treating medical college: A prospective longitudinal study. PeerJ 2020, 8, e10164. [Google Scholar] [CrossRef] [PubMed]
- Thiemann, P.; Brimicombe, J.; Benson, J.; Quince, T. When investigating depression and anxiety in undergraduate medical students timing of assessment is an important factor—A multicentre cross-sectional study. BMC Med. Educ. 2020, 20, 125. [Google Scholar] [CrossRef] [PubMed]
- Keane, C.; Waldeck, D.; Holliman, A.; Goodman, S.; Choudhry, K. Exploring the Experience of Anxiety among Final Year Students at University: A Thematic Analysis. Qual. Rep. 2021, 26, 2621–2630. [Google Scholar] [CrossRef]
- Durning, S.J.; Dong, T.; Ratcliffe, T.; Schuwirth, L.; Anthony, R.A.; Boulet, J.R.; Kevin, E. Comparing Open-Book and Closed-Book Examinations: A Systematic Review. Acad. Med. J. Assoc. Am. Med. Coll. 2016, 91, 583–599. [Google Scholar] [CrossRef]
- Slack, H.R.; Priestley, M. Online learning and assessment during the Covid-19 pandemic: Exploring the impact on undergraduate student well-being. Assess. Evaluation High. Educ. 2022, 48, 333–349. [Google Scholar] [CrossRef]
- Rapanta, C.; Botturi, L.; Goodyear, P.; Guàrdia, L.; Koole, M. Balancing Technology, Pedagogy and the New Normal: Post-pandemic Challenges for Higher Education. Postdigital Sci. Educ. 2021, 3, 715–742. [Google Scholar] [CrossRef]
- Rasli, A.; Tee, M.; Lai, Y.L.; Tiu, Z.C.; Soon, E.H. Post-COVID-19 strategies for higher education institutions in dealing with unknown and uncertainties. Front. Educ. 2022, 7, 992063. [Google Scholar] [CrossRef]
- Lewis, R.; Roden, L.C.; Scheuermaier, K.; Gomez-Olive, F.X.; Rae, D.E.; Iacovides, S.; Bentley, A.; Davy, J.P.; Christie, C.J.; Zschernack, S.; et al. The impact of sleep, physical activity and sedentary behaviour on symptoms of depression and anxiety before and during the COVID-19 pandemic in a sample of South African participants. Sci. Rep. 2021, 11, 24059. [Google Scholar] [CrossRef]
- Schweizer, S.; Lawson, R.P.; Blakemore, S.-J. Uncertainty as a driver of the youth mental health crisis. Curr. Opin. Psychol. 2023, 53, 101657. [Google Scholar] [CrossRef] [PubMed]
- Ungar, M.; Connelly, G.; Liebenberg, L.; Theron, L. How Schools Enhance the Development of Young People’s Resili-ence. Soc. Indic. Res. 2019, 145, 615–627. [Google Scholar] [CrossRef]
- Dohaney, J.; de Róiste, M.; Salmon, R.A.; Sutherland, K. Benefits, barriers, and incentives for improved resilience to disruption in university teaching. Int. J. Disaster Risk Reduct. 2020, 50, 101691. [Google Scholar] [CrossRef] [PubMed]
- Ford, T.; John, A.; Gunnell, D. Mental health of children and young people during pandemic. BMJ 2021, 372, n614. [Google Scholar] [CrossRef]
- Brien, N.O.; Lawlor, M.; Chambers, F.; O’Brien, W. Mental fitness in higher education: Intervention Mapping programme design. Health Educ. 2020, 120, 21–39. [Google Scholar] [CrossRef]
- O’connor, K.; Wrigley, M.; Jennings, R.; Hill, M.; Niazi, A. Mental health impacts of COVID-19 in Ireland and the need for a secondary care mental health service response. Ir. J. Psychol. Med. 2020, 38, 99–107. [Google Scholar] [CrossRef] [PubMed]
- Breslin, G.; Haughey, T.; O’brien, W.; Caulfield, L.; Robertson, A.; Lawlor, M. Increasing Athlete Knowledge of Mental Health and Intentions to Seek Help: The State of Mind Ireland (SOMI) Pilot Program. J. Clin. Sport Psychol. 2018, 12, 39–56. [Google Scholar] [CrossRef]

| Total | NI | ROI | |||||||
|---|---|---|---|---|---|---|---|---|---|
| PHQ-9 Scores | N | M | SD | N | M | SD | N | M | SD |
| Year 1 (2019) | 497 | 4.67 | 5.43 | 406 | 4.33 | 5.20 | 91 | 6.18 | 6.17 |
| Year 2 (2020) | 497 | 6.44 | 5.63 | 406 | 6.42 | 5.59 | 91 | 6.52 | 5.81 |
| Year 3 (2021) | 497 | 6.05 | 5.74 | 406 | 6.04 | 5.70 | 91 | 6.08 | 5.92 |
| End Year 3 (2022) | 229 | 7.41 | 6.19 | 180 | 7.25 | 5.98 | 49 | 8.04 | 6.97 |
| Total | NI | ROI | |||||||
|---|---|---|---|---|---|---|---|---|---|
| GAD-7 Scores | N | M | SD | N | M | SD | N | M | SD |
| Year 1 (2019) | 499 | 6.70 | 6.54 | 413 | 6.83 | 6.67 | 86 | 6.08 | 5.87 |
| Year 2 (2020) | 499 | 5.90 | 5.24 | 413 | 5.78 | 5.17 | 86 | 6.50 | 5.55 |
| Year 3 (2021) | 499 | 5.58 | 5.25 | 413 | 5.58 | 5.23 | 86 | 5.69 | 5.37 |
| End Year 3 (2022) | 229 | 6.85 | 5.73 | 180 | 6.67 | 5.62 | 49 | 7.51 | 6.15 |
| Very Positive % | Positive % | Neutral % | Negative % | Very Negative % | |
|---|---|---|---|---|---|
| Social aspects of college life | 4.8 | 3.5 | 19.2 | 29.3 | 43.2 |
| Sense of belonging in college | 3.9 | 7.9 | 30.1 | 29.7 | 28.4 |
| Interacting with others—academic staff, peers, etc. | 6.6 | 10.0 | 20.1 | 38.0 | 25.3 |
| Opportunities for summer work, internships or exchanges | 5.2 | 10.0 | 31.9 | 30.1 | 22.7 |
| Hands on experience/practical work (10.9% not applicable) | 10.0 | 7.4 | 20.1 | 29.3 | 22.3 |
| Being prepared for the future | 6.1 | 14.4 | 29.7 | 31.9 | 17.9 |
| Employment opportunities | 6.6 | 12.7 | 36.7 | 26.6 | 17.5 |
| Volunteering opportunities | 3.9 | 8.3 | 41.5 | 28.8 | 17.5 |
| Opportunities for independent living | 7.0 | 12.7 | 41.9 | 21.8 | 16.6 |
| Plans to continue at college | 6.6 | 15.7 | 41.0 | 21.4 | 15.3 |
| Placement experience (18.8% not applicable) | 10.9 | 10.0 | 22.7 | 22.7 | 14.8 |
| Opportunities to realise career aspirations | 8.3 | 14.4 | 38.0 | 26.6 | 12.7 |
| Academic achievement/grades | 6.1 | 17.5 | 30.6 | 33.6 | 12.2 |
| Being prepared for exams | 6.1 | 13.5 | 35.4 | 33.6 | 11.4 |
| Completing assessments or assignments | 7.4 | 21.8 | 26.6 | 33.2 | 10.9 |
| Very Positive % | Positive % | Neutral % | Negative % | Very Negative % | |
|---|---|---|---|---|---|
| Social life | 0.9 | 6.6 | 17.5 | 45.0 | 30.1 |
| Lifestyle | 3.9 | 13.5 | 26.2 | 43.2 | 13.1 |
| Ability to participate in physical activity | 3.9 | 17.5 | 27.5 | 40.2 | 10.9 |
| Diet | 3.1 | 11.8 | 31.0 | 39.3 | 14.8 |
| Access to mental health services/medical support | 4.8 | 8.3 | 38.9 | 32.2 | 15.7 |
| Finances | 4.8 | 24.5 | 28.8 | 26.6 | 15.3 |
| Relationship with friends | 7.4 | 20.1 | 38.9 | 26.6 | 7.0 |
| Relationship with family | 12.2 | 32.3 | 35.8 | 12.2 | 7.4 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
McLafferty, M.; Ward, C.; Walsh, C.P.; O’Neill, S.; Bjourson, A.J.; McHugh, R.; Brown, N.; McBride, L.; Brady, J.; Murray, E.K. College Student Mental Health and Wellbeing Prior to and during the COVID-19 Pandemic. Educ. Sci. 2023, 13, 1154. https://doi.org/10.3390/educsci13111154
McLafferty M, Ward C, Walsh CP, O’Neill S, Bjourson AJ, McHugh R, Brown N, McBride L, Brady J, Murray EK. College Student Mental Health and Wellbeing Prior to and during the COVID-19 Pandemic. Education Sciences. 2023; 13(11):1154. https://doi.org/10.3390/educsci13111154
Chicago/Turabian StyleMcLafferty, Margaret, Caoimhe Ward, Colum P. Walsh, Siobhan O’Neill, Anthony J. Bjourson, Rachel McHugh, Natasha Brown, Louise McBride, John Brady, and Elaine K. Murray. 2023. "College Student Mental Health and Wellbeing Prior to and during the COVID-19 Pandemic" Education Sciences 13, no. 11: 1154. https://doi.org/10.3390/educsci13111154
APA StyleMcLafferty, M., Ward, C., Walsh, C. P., O’Neill, S., Bjourson, A. J., McHugh, R., Brown, N., McBride, L., Brady, J., & Murray, E. K. (2023). College Student Mental Health and Wellbeing Prior to and during the COVID-19 Pandemic. Education Sciences, 13(11), 1154. https://doi.org/10.3390/educsci13111154








