Abstract
The physiotherapist inevitably experiences clinical uncertainty, as they treat a wide variety of pathologies and, in some situations, will be the first professional contact. However, clinical uncertainty has yet to be sufficiently studied in physiotherapy and is not explicitly contemplated in physiotherapist training. This research aims to evaluate recent physiotherapy graduates’ tolerance to clinical uncertainty to determine their educational needs. A cross-sectional quantitative observational study was conducted in which the sample consisted of 31 recent graduates. They were given a self-developed questionnaire to assess “Tolerance to Uncertainty in Physiotherapy” (TUP). The results showed that the mean score obtained was 57.7 (6.49) points, with a minimum of 43 and a maximum of 69 points. The dimension “sources of uncertainty” scored the highest. The results revealed a profile of novice physiotherapists with a medium intolerance to uncertainty, nervous about unknown diagnoses. It is necessary to consider tolerance to uncertainty in the curricular programmes of physiotherapy degrees that can cover the needs described here.
1. Introduction
Clinical uncertainty (CU) can be defined as the “Subjective perception of inability to provide an accurate explanation of the patient’s health problem” [1]. Clinical uncertainty has been a topic of interest in medicine for decades [2,3,4,5]. However, physiotherapy is a field that has yet to be explored [6]. Physiotherapists will be confronted assiduously with CU due to the great diversity of pathologies they deal with and the individual characteristics of each patient. A bachelor’s degree in physiotherapy does not explicitly include the management of tolerance to clinical uncertainty (CU) within its syllabus’ theoretical and practical content. Moreover, in Spain, the physiotherapist will sometimes be the patient’s first professional contact [7]. According to Almond et al. [6], the strategies that physiotherapists learn to manage uncertainty are primarily attributed to their clinical experiences or models observed during their clinical practice. It is essential to consider that work anxiety has been reported in physicians with intolerance to CU, which may impact their mental wellbeing and professional capabilities [8,9]. Therefore, in recent years, a call has been made for CU management to be included in the health professions’ curricula [9,10,11,12]. Uncertainty should be considered a dynamic process subject to possible modifications [4]. In this way, it is considered that personal traits and learning can act as modulators of uncertainty tolerance [13].
Different taxonomies of clinical uncertainty have been developed to facilitate understanding and are helpful tools for researchers and teachers. In this sense, the authors of ref. [14] structure CU in three dimensions: sources, issues and locus. The “sources” dimension refers primarily to information and is subdivided into probability, ambiguity and complexity. When the information is not well determined but within certain margins, we speak of probability; however, when we do not have enough information or cannot trust it, we speak of ambiguity. If the nature of the question has multiple possibilities despite the information available, we speak of complexity. The second dimension, “issues”, or “substantive issues”, refers to where the focus of concern lies. It is thus subdivided into “scientific uncertainty”, “practical uncertainty”, and “personal uncertainty”. Scientific uncertainty” refers to the pathology itself, diagnosis, prognosis and treatment options. In contrast, “practical uncertainty” refers to the professional and the system, e.g., quality of care and professional competence. As for “personal uncertainty”, this concerns the patient, his or her perspectives and psychosocial consequences. The third dimension, “position”, refers to social interaction, i.e., the CU can be presented to the clinician, the patient or both simultaneously.
Lee et al. [15] developed a taxonomy intended to be useful for medical educators. This classification comprises three interconnected dimensions. The three dimensions are: “sources of uncertainty”, “subjective nature of uncertainty” and “responses to uncertainty”. Sources of uncertainty are a magnitude that reflects aspects related to knowledge and knowledge management. Thus, sources of uncertainty can be listed as lack of knowledge, interpretation of probabilities, ambiguity, complexity and unknown situations. Subjective influences of uncertainty refer to aspects that relate to the subjective nature of uncertainty and its relation to the individual’s characteristics. Thus, we can associate it with personal, professional, and contextual factors. Personality, cognitive ability and personal biases influence the CU experience as modulators. As for the dimension, “reactions to uncertainty”, this refers to the different positions we can adopt in the face of CU, be it a cognitive, behavioural or emotional response. In turn, they can be positive or negative reactions, i.e., adaptive or maladaptive. This taxonomy serves as a guide for the present study because of its applicability to the educational environment and reflects the relationships between the different dimensions of CU.
The main objective of this study is to assess the tolerance to uncertainty in recent graduates to identify the training needs that future graduates may require.
2. Materials and Methods
2.1. Objectives
The aim of the study is twofold: on the one hand, to assess the tolerance to CU of physiotherapists who have just entered the labour market and, on the other hand, to identify their educational needs in terms of tolerance to CU. These data will guide teachers of degrees in physiotherapy in the training of future physiotherapists. A cross-sectional quantitative observational study was carried out.
2.2. Population and Sample
The population included in this study were the physiotherapists who completed their studies for a degree in physiotherapy at the University of Las Palmas de Gran Canaria in the last three years. Thus, it includes the physiotherapists of the cohorts 2016–2020, 2017–2021 and 2018–2022 from the data provided by the university itself on its web page [16] of approximately 180 physiotherapists. A convenience sampling was conducted among physiotherapy graduates from the last three years. They were invited to participate in the study and provided an online questionnaire link. To participate, it was mandatory to provide informed consent. A total of 31 physiotherapists responded during the period established for data collection, representing 17.22% of the population.
2.3. Instrument
For data collection, we designed our questionnaire to assess “Tolerance to Uncertainty in Physiotherapy” (TUP). It was mandatory in order to participate in the study to first provide the informed consent voluntarily. The consent informed of the purpose of the study, guaranteed anonymity and confidential data treatment. In addition, an email address was provided to resolve their doubts and exercise their rights to modify their data or renounce their participation.
We chose to design our questionnaire based on the questionnaires most commonly used in the literature to measure tolerance to uncertainty, to satisfy the following requirements: to be a questionnaire adapted to the characteristics of physiotherapists, and to explore the three dimensions of clinical uncertainty described in the taxonomy by Lee et al. [15]. The questionnaires used as reference were: Budner’s Tolerance of Ambiguity Scale (TOAS), Physicians’ Reactions to Uncertainty (PRU) and Tolerance of Ambiguity (TFA). The TOAS scale has been widely used in the scientific literature. It consists of 16 items, 8 of which are scored positively and 8 negatively, on a 7-point Likert scale [17]. Despite its good test–retest reliability, its internal consistency is controversial [18,19] The main feature of the PRU questionnaire is that it is a measure of uncertainty specific to physicians. It originally consisted of 22 items distributed in two subscales, the “uncertainty stress” scale with 13 items and the “reluctance to share uncertainty” scale with nine items [20]. In a later revision, the PRU scale was reduced to 15 items. Four dimensions were analysed: anxiety about uncertainty, concern about poor outcomes, reluctance to disclose uncertainty, and reluctance to disclose errors to other physicians [21]. The TFA scale was developed to measure uncertainty and establish correlations with physicians’ attitudes and personal characteristics. It consists of 7 items and a 6-point Likert scale [22].
The TUP questionnaire consists of 20 items measured on a 5-point Likert scale and 3 dimensions analysed: sources of uncertainty, subjective influences of uncertainty and responses to uncertainty. Items 1, 3, 6, 15, 17, 18 and 20 are reverse scored. The maximum score that can be obtained in the questionnaire is 100 points, and the minimum score is 20 points, with the average point on the scale being 60 points. A positive linear relationship exists between the score and intolerance to perceived clinical uncertainty. The survey was originally designed and distributed in Spanish to the participants. However, an English version is also now accessible. The global scale’s internal consistency was measured using Cronbach´s alpha coefficient. The resulting value was 0.586.
2.4. Data Collection and Analysis Procedure
The TUP questionnaire was provided to the population online, and data were collected from 14 October to 14 November 2022. The confidentiality and anonymity of the participants were guaranteed at all times. Statistical data analysis was carried out using the statistical software JAMOVI [23,24]. Categorical variables were summarised using percentages and absolute frequencies. The equality of proportions of categories was tested using binomial non-parametric tests. Numerical variables were summarised using the mean and standard deviation (SD), as well as the minimum and maximum values of the data. The comparison of the means of two independent samples, the Student’s t-test, was used, as the data’s normality condition was fulfilled. To analyse the possible association between two ordinal categorical variables, Kendall’s Tau-b correlation coefficient was used. The results were considered statistically significant if the p-value was <0.05.
3. Results
3.1. Descriptive Analysis of the Participating Physiotherapists
The sample consisted of 31 graduates aged between 21 and 33, with a mean age of 23.2 (2.2) years. The gender distribution was balanced (p-value = 1), with 51.6% (16) women and 48.4% (15) men. The graduates finished their studies of a degree in physiotherapy in 2020 (9.7% (3)), 2021 (32.3% (10)) and 2022 (58.1% (18)). Of these, 58.1% (18) had less than one year of work experience, and 41.9% (13) had one year or more of work experience. Some 52% (13) were part of a multidisciplinary team with a doctor, compared to 48% (12) who were not (p-value = 1). Of these, 74.2% (23) were currently working in private health care, 22.6% (7) were not working, and 3.2% (1) were in free practice. Regarding the frequency as first contact professionals with a patient, 52% of the current graduates declared that they were never or hardly ever the first contact professional, with their patients being referred by doctors. Twenty-four per cent stated that they were sometimes, and 24% stated that they were always or almost always.
3.2. Analysis of the Results of the TUP Questionnaire
In the TUP questionnaire, the mean total score obtained was 57.7 (6.49) points, with a minimum of 43 and a maximum of 69 points. Little difference was observed between the groups stratified by work experience. Novice physiotherapists with less than one year´s experience had a mean score of 58.3 (4.50), and those with more than one year´s experience had a mean score of 56.8 (8.66). The difference needs to be more significant to be considered relevant. When we differentiated by gender, we noticed that the female gender received a mean score of 59.8 (SD = 4.6) compared to 55.5 (SD = 7.6) for the male participants, the difference not being significant (p-value = 0.065). Notably, the standard deviation was three points higher in the male gender compared to the female gender. Therefore, it could be inferred that, although greater intolerance was observed in the female gender, the dispersion was more significant in the male gender. Following the model of the taxonomy of tolerance to uncertainty proposed by Lee et al. [15], we analysed the results according to each of the dimensions studied. Table 1 shows the average score obtained by each of the dimensions. It can be seen that the dimension with the highest score was “sources of uncertainty”, which is related to the complexity of the cases, insufficient information or ambiguity of the information.

Table 1.
Analysis of results by dimension.
Consequently, it follows that the aspects related to knowledge and experience were the ones that generated the most intolerance to CU for the physiotherapists surveyed. The magnitude of “responses to uncertainty” was associated with how physiotherapists react to CU and had the second-highest score. Consequently, it was observed that issues such as: knowing when to refer, consulting colleagues or coping with the case contributed to increased intolerance of CU. Greater tolerance was observed with aspects stemming from self-perceived uncertainty, as reflected by a lower score on the dimension “subjective nature of uncertainty”. The nature of uncertainty contained responses to negative self-perceptions of uncertainty, including catastrophic thinking and perceived professional incompetence.
The different specific aspects analysed in each of the dimensions studied can be seen in Table 2. It should be noted that item 4Q, “I tend to feel nervous or anxious when I am not sure about my patient’s treatment, diagnosis or prognosis”, is the item with the highest score. Therefore, novice physiotherapists show more agreement in feeling uneasy about the CU generated by their insecurity. The second variable with the highest agreement is 16Q, “I prefer that patients do not know that I am unsure about which treatments to use”, indicating the physiotherapist’s reluctance to share their uncertainty. Item 5Q, “If I am unsure about my patient’s problem, I always encourage them to ask for more diagnostic tests”, also stands out with a high score, reflecting the physiotherapist’s need for more information in uncertain diagnoses. The assessed physiotherapists also agreed that they were worried about not getting good results with their patients and found it difficult to switch off mentally, as indicated by item 11Q. The physiotherapists surveyed also showed higher agreement in item 17Q_INV, expressing their willingness to share their doubts with colleagues. This variable had an inverse score and was the lowest score as it is associated with a characteristic trait of tolerance to CU. Similarly, item 1Q_INV, which expressed that physiotherapists were aware that they would not always be able to have all the information, obtained a high agreement range and a low score.

Table 2.
Variable analysis of the TUP questionnaire.
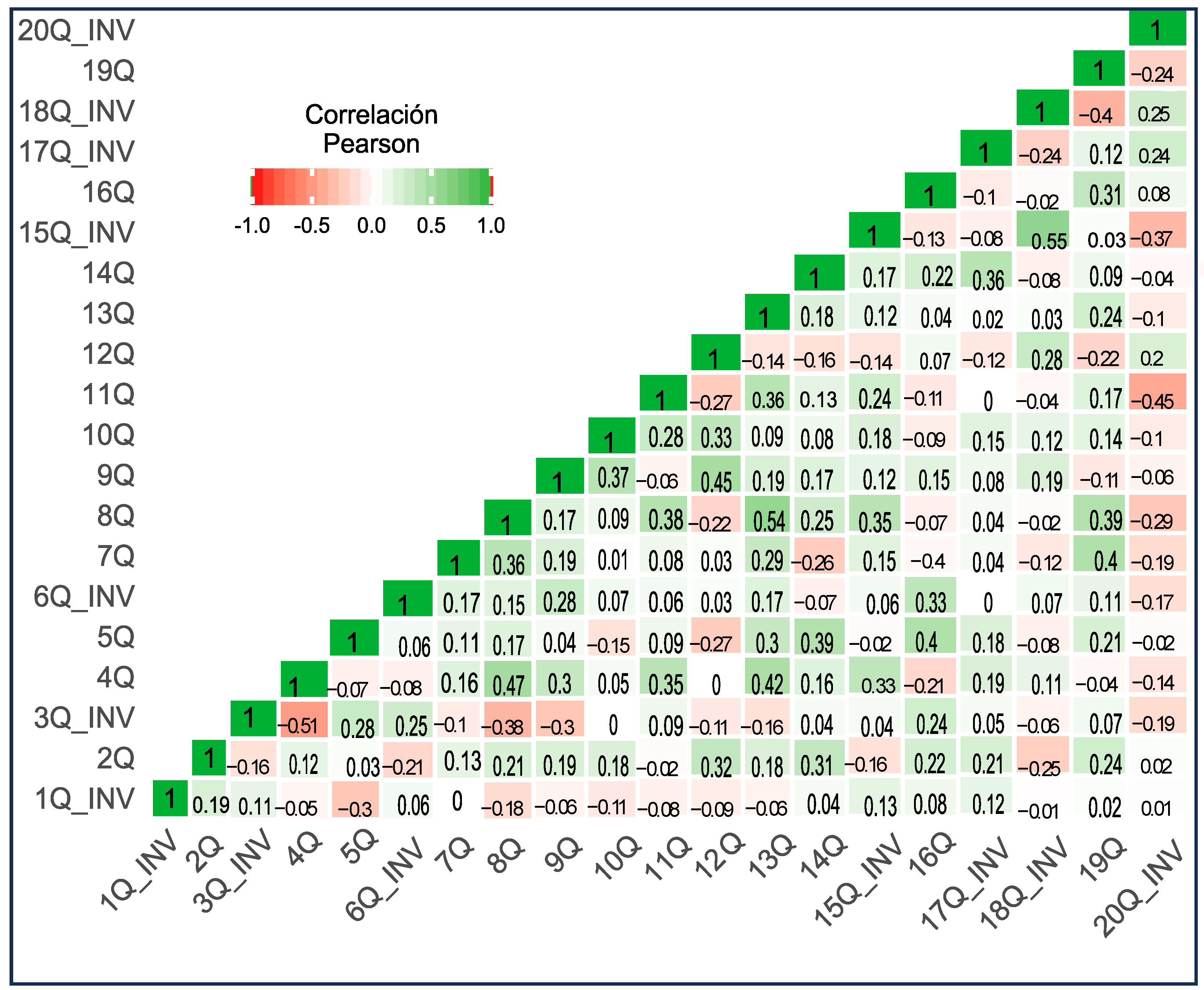
3.3. Correlation Analysis of the TUP Questionnaire Variables
An analysis of the association between the items that comprise the TUP questionnaire was carried out. Of the 20 items that make up the questionnaire, up to 12 (60%) have a statistically significant correlation, as shown in Figure 1. The positive correlation with the highest statistical significance (0.472, p = 0.002) was found between the variables 8Q and 13Q. Both items belong to the dimension “subjective nature of uncertainty” and are associated with the negative perception of uncertainty and catastrophic ideas. Thus, the physiotherapists in the sample who had catastrophic ideas about their actions with the patient were also afraid of possible legal consequences. A positive correlation (0.446, p = 0.004) exists between items 3Q_INV and 4Q. This correlation shows that physiotherapists do not give up experimenting with unknown or complex cases despite feeling uneasy about their insecurity. There is a positive correlation between harbouring catastrophic ideas and feeling nervous or anxious in clinical practice. This association can be seen from the statistically significant correlation between the variables 4Q and 8Q (0.446, p = 0.005), which connect the dimensions “sources of uncertainty” with the “subjective nature of uncertainty”.
Figure 1.
Correlation heat map between TUP questionnaire variables.
Similarly, the correlation between items 15Q_INV and 18Q_INV (0.451, p = 0.004) stands out. The recently graduated physiotherapists in the sample willing to share their uncertainty with their patients agree that this is positive for establishing trusting relationships with their patients. Likewise, respondents who share their uncertainty with their patients are open to referral to another professional, as seen in the statistically significant correlation between the 15Q_INV and 20Q_INV (−0.376, p = 0.021). Note the correlation between items 14Q and 5Q (0.335, p = 0.031). The physiotherapists in the sample who, in the face of their insecurity, demanded more diagnostic tests also coincided with quoting their patients more frequently. This relationship links the dimensions of “uncertainty responses” with “sources of uncertainty”.
4. Discussion
The first notable finding of the present study is that the TUP questionnaire revealed that the physiotherapists evaluated obtained a score of medium intolerance to CU (57.7 (6.49)). This statement suggests that the physiotherapists in the sample, faced with situations beyond their control because they are unknown, complex or ambiguous, had a high likelihood of feeling stress or anxiety. It is not easy to compare the scores obtained with other values previously presented in the scientific literature. This is because, on the one hand, in the present study, CU was assessed with a self-developed tool; therefore, it is the first time that data have been obtained in this way. On the other hand, multiple scales to assess CU tolerance make it challenging to unify criteria. There needs to be a consensus on the definition of CU to establish clear criteria for developing a measurement instrument [1]. However, it can be inferred that the CU intolerance score is medium, considering the parameters of the questionnaire and its maximum score. To our knowledge, this is the first time that CU tolerance has been assessed in physiotherapists. Almond et al. [6] conducted a qualitative study with a sample of 17 novice physiotherapists investigating how they managed CU but did not measure CU tolerance. Simmonds et al. [25] assessed how beliefs, knowledge and tolerance to uncertainty influenced physiotherapists’ approach to patients with low back pain. They used a modified version of the Intolerance Uncertainty Scale (IUS) by Freeston et al. [26] consisting of 12 items on a 5-point Likert scale that studied two dimensions: anxiety and avoidance of intolerance to uncertainty. The sample consisted of 108 physiotherapists from Quebec with a mean age of 36.7 (9.7) years and a mean score of 24.25 (7.27) on the IUS scale. It is worth mentioning that when adjusting for age, physiotherapists younger than 35 had a slightly higher intolerance to uncertainty score compared to physiotherapists older than 35 years.
Focusing on medicine, the study by Weissenstein et al. [27] assessed intolerance to uncertainty in medical students. They analysed CU in students from the first year of training to the sixth year and found no significant differences. However, they concluded that the level of uncertainty tolerance in medical students was low. Ying et al. [28] assessed CU tolerance in surgical residents and found no statistically significant difference between junior and senior residents with more experience. Likewise, they also found no significant differences in CU tolerance between sexes. These results are consistent with the study presented here, in which the female gender showed higher CU intolerance scores than the male gender but without statistical significance.
Notably, the dimension studied that scored the highest and contributed most to intolerance to CU among the surveyed physiotherapists was “sources of uncertainty”. The “sources dimension” refers to, among other aspects, using available information and knowledge. Consequently, aspects related to lack of knowledge, ambiguity of information and complexity of cases were associated with higher levels of CU in the sample. It has been described that the CU generated by the perception of a lack of knowledge may be related to a dualistic conception of knowledge, i.e., a consideration of what is true or correct versus what is uncertain or incorrect. Over the years, this perception has given way to a more flexible conception of knowledge [29]. More experienced health professionals are distinguished by a more remarkable ability to recognise clinical patterns useful in clinical diagnosis [30]. In a field such as health care, where new information and scientific evidence are constantly becoming available, professionals must rely on their clinical experience, and recent graduates need this experience [31].
The item with the highest score was 4Q “I tend to feel nervous or anxious when I am unsure of my patient’s treatment, diagnosis or prognosis”. This result aligns with the results of different studies that relate intolerance to CU to high levels of stress and work discomfort, which may contribute to the development of future burnout syndrome [8,32]. Lally & Cantillon [10], found a relationship between intolerance of uncertainty and psychological distress in fourth-year Irish medical students.
The second highest scoring item was 16Q: “I prefer patients not to know that I am unsure about which treatments to use”. It has been related that physicians with low tolerance to CU tend not to share all information with patients or to hide their doubts [33]. As with physicians, physiotherapists may act in the same way, and this may be due to an inability to recognise their limitations.
Another variable that should be highlighted for obtaining a high degree of agreement is 5Q. This item refers to the predilection of physiotherapists to request more diagnostic tests when uncertain about their diagnosis. It has been linked, in medicine, with those doctors with higher levels of intolerance to uncertainty requesting more diagnostic tests with the consequent higher health care costs that this entails [9].
The item with the lowest value was item 17Q_INV, “When I am not sure about a patient’s problem. I always share it with other physiotherapist colleagues”. Asking for help from more experienced or knowledgeable colleagues has been a characteristic trait of professionals with low tolerance to CU. However, it cannot be considered only as a negative aspect. It can be seen as an adaptive response to self-perceived ignorance [29]. Professionals with a high tolerance for CU may not consult with other professionals, refusing to doubt their abilities [33]. In the same vein, item 20Q_INV, “when I am not sure of the diagnosis, I prefer to tell the patient and refer to another professional”, can be considered a strategy to reduce uncertainty by disassociating oneself from responsibility [29]. However, if the ability to share uncertainty with the patient and act on it is valued, it is a positive strategy for responding to uncertainty.
The significant correlations between variables 4Q and 8Q reflect that recently graduated physiotherapists feel nervous or anxious when unsure about a patient’s diagnosis or treatment, which is strongly correlated with catastrophic ideas about their performance. The catastrophic thinking of the physiotherapist adds to the fear that, at some point, he/she may be denounced, as explained by the positive relationship between questions 13Q and 8Q. Similarly, the correlation of item 4Q with question 13Q shows that the fear of being judged or denounced may contribute to this discomfort in ambiguous situations. However, as the positive correlation between items 4Q and 3Q reflects, despite feeling nervous or anxious, they do not shy away from experiencing new cases or complexes. The novice physiotherapist with a negative perception of uncertainty avoids putting themself in situations that could compromise them. They prefer not to treat colleagues, as shown by the correlation between 9Q and 12Q. However, the correlation between the variables 15Q_INV and 18Q_INV reflects those physiotherapists who have a positive perception of uncertainty sharing their doubts with patients and understanding that this communication improves the relationship of trust with them. Likewise, the physiotherapists in the sample who shared their uncertainty with patients agreed on the need to refer to another professional when they were unsure of their diagnoses. The correlation between the variables 15Q_INV and 20_INV demonstrates this association.
Different needs have been identified in the management of CU that can be addressed by educational actions during the training of physiotherapists. Aspects related to information management, sharing uncertainty and decision-making in situations of uncertainty are still pending in recent graduates.
5. Limitations
Considering the limitations of the study, such as the small sample size, it is impossible to generalize the results. The sampling method used was convenience sampling and an online questionnaire, which is cost-effective and efficient for wide distribution. However, the absence of incentives to participate often results in low response rates. In addition, only physiotherapists from the same university centre were included, which cannot be considered representative. In addition, most of the sample works in private centres. In the future, the inclusion of physiotherapists from a broader selection of different universities would provide a more complete picture and diverse perspectives.
It should be noted that the questionnaire still under development was used, so the scores obtained should still be considered relevant. The focus was to identify correlations between questions to determine which provided the most valuable information. This approach made it possible to identify aspects or situations that caused uncertainty for recent graduates in the sample. The aim is to refine the questionnaire and validate it shortly.
6. Conclusions
The newly graduated physiotherapists in this sample showed a medium average tolerance profile to CU. Unfamiliar diagnoses and treatment insecurities may lead to catastrophic ideas or fear of repercussions, resulting in nervousness and anxiety. These situations lead them to request more diagnostic tests and more frequent appointments. Moreover, they find it difficult to switch off mentally when they do not get the desired prognosis. For this reason, they tend not to share their uncertainty with patients because they will lose their trust and hide their limitations. They will also avoid situations that may be a source of insecurity, such as dealing with colleagues in the profession. However, novice physiotherapists understand that CU is inexorable in their work and that it is necessary to refer to another professional when unsure.
It is necessary to consider the tolerance to CU in the curricular programmes of degrees in physiotherapy that can cover the needs described here.
Author Contributions
Conceptualization, A.I.G.; methodology, A.I.G. and M.D.P.E.B.; validation, A.I.G., M.d.P.Q.M. and M.D.P.E.B.; formal analysis, A.I.G. and M.d.P.Q.M.; investigation, A.I.G.; data curation, A.I.G. and M.d.P.Q.M.; writing—original draft preparation, A.I.G.; writing—review and editing, A.I.G., M.d.P.Q.M. and M.D.P.E.B.; visualization, A.I.G. and M.d.P.Q.M.; supervision, A.I.G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
Restrictions apply to the availability of these data. Data are not publicly available due to ethics and third-party institutional restrictions.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Bhise, V.; Rajan, S.S.; Sittig, D.F.; Morgan, R.O.; Chaudhary, P.; Singh, H. Defining and Measuring Diagnostic Uncertainty in Medicine: A Systematic Review. J. Gen. Intern. Med. 2018, 33, 103–115. [Google Scholar] [CrossRef] [PubMed]
- Simpkin, A.L.; Schwartzstein, R.M. Tolerating Uncertainty-The Next Medical Revolution? N. Engl. J. Med. 2016, 375, 1713–1715. [Google Scholar] [CrossRef] [PubMed]
- Helou, M.A.; DiazGranados, D.; Ryan, M.S.; Cyrus, J.W. Uncertainty in Decision Making in Medicine: A Scoping Review and Thematic Analysis of Conceptual Models. Acad. Med. 2020, 95, 157–165. [Google Scholar] [CrossRef] [PubMed]
- Hillen, M.A.; Gutheil, C.M.; Strout, T.D.; Smets, E.M.A.; Han, P.K.J. Tolerance of Uncertainty: Conceptual Analysis, Integrative Model, and Implications for Healthcare. Soc. Sci. Med. 2017, 180, 62–75. [Google Scholar] [CrossRef] [PubMed]
- Ilgen, J.S.; Eva, K.W.; de Bruin, A.; Cook, D.A.; Regehr, G. Comfort with Uncertainty: Reframing Our Conceptions of How Clinicians Navigate Complex Clinical Situations. Adv. Health Sci. Educ. 2019, 24, 797–809. [Google Scholar] [CrossRef] [PubMed]
- Almond, A.; Zou, Y.; Forbes, R. Navigating Diagnostic Uncertainty in Musculoskeletal Practice: The Perspectives and Experiences of New Graduate Physiotherapists. Musculoskelet. Sci. Pract. 2021, 52, 102354. [Google Scholar] [CrossRef]
- Souto Camba, S. Autonomía Profesional y Acceso Directo En Fisioterapia. Fisioterapia 2013, 35, 89–91. [Google Scholar] [CrossRef]
- Simpkin, A.L.; Khan, A.; West, D.C.; Garcia, B.M.; Sectish, T.C.; Spector, N.D.; Landrigan, C.P. Stress from Uncertainty and Resilience Among Depressed and Burned Out Residents: A Cross-Sectional Study. Acad. Pediatr. 2018, 18, 698–704. [Google Scholar] [CrossRef]
- Iannello, P.; Mottini, A.; Tirelli, S.; Riva, S.; Antonietti, A. Ambiguity and Uncertainty Tolerance, Need for Cognition, and Their Association with Stress. A Study among Italian Practicing Physicians. Med. Educ. Online 2017, 22, 1270009. [Google Scholar] [CrossRef]
- Lally, J.; Cantillon, P. Uncertainty and Ambiguity and Their Association with Psychological Distress in Medical Students. Acad. Psychiatry 2014, 38, 339–344. [Google Scholar] [CrossRef]
- Escourrou, E.; Bergeaut, M.; Gimenez, L.; Durliat, I.; Stillmunkés, A.; Oustric, S.; Dupouy, J. Evolution Uncertainty of among Reactions Residents to during a Clinical Rotation. Fam. Med. 2020, 52, 339–345. [Google Scholar] [CrossRef] [PubMed]
- Taylor, D.; Picker, B.; Woolever, D.; Thayer, E.; Carney, P.; Galper, A. A Pilot Study to Address Tolerance of Uncertainty Among Family Medicine Residents. Fam. Med. 2018, 50, 531–538. [Google Scholar] [CrossRef]
- Stephens, G.C.; Rees, C.E.; Lazarus, M.D. Exploring the Impact of Education on Preclinical Medical Students’ Tolerance of Uncertainty: A Qualitative Longitudinal Study. Adv. Health Sci. Educ. 2021, 26, 53–77. [Google Scholar] [CrossRef] [PubMed]
- Han, P.K.J.; Klein, W.M.P.; Arora, N.K. Varieties of Uncertainty in Health Care: A Conceptual Taxonomy. Med. Decis. Mak. 2011, 31, 828–838. [Google Scholar] [CrossRef]
- Lee, C.; Hall, K.; Anakin, M.; Pinnock, R. Towards a New Understanding of Uncertainty in Medical Education. J. Eval. Clin. Pract. 2020, 27, 1194–1204. [Google Scholar] [CrossRef]
- Available online: https://www2.ulpgc.es/index.php?pagina=transparencia&ver=egresados (accessed on 30 January 2023).
- Budner, S. Intolerance of Ambiguity as a Personality Variable. J. Pers. 1962, 30, 29–50. [Google Scholar] [CrossRef]
- Bors, D.A.; Gruman, J.A.; Shukla, S. Measuring Tolerance of Ambiguity: Item Polarity, Dimensionality, and Criterion Validity. Eur. Rev. Appl. Psychol. 2010, 60, 239–245. [Google Scholar] [CrossRef]
- Benjamin, A.J.; Riggio, R.E.; Mayes, B.T. Reliability and Factor Structure of Budner’s Tolerance for Ambiguity Scale. J. Soc. Behav. Personal. 1996, 11, 625–632. [Google Scholar]
- Gerrity, M.S.; Devellis, R.F.; Earp, J.A. Physicians’ Reactions to Uncertainty in Patient Care: A New Measure and New Insights. Care 1990, 28, 724–736. [Google Scholar] [CrossRef]
- Gerrity, M.S.; White, K.P.; DeVellis, R.F.; Dittus, R.S. Physicians’ Reactions to Uncertainty: Refining the Constructs and Scales. Motiv. Emot. 1995, 19, 175–191. [Google Scholar] [CrossRef]
- Geller, G.; Tambor, E.S.; Chase, G.A.; Holtzman, N.A. Measuring Physicians’ Tolerance for Ambiguity and Its Relationship to Their Reported Practices Regarding Genetic Testing. Med. Care 1993, 31, 989–1001. [Google Scholar] [CrossRef] [PubMed]
- The Jamovi Project. Jamovi (Version 2.3) [Computer Software]. 2022. Available online: https://www.jamovi.org (accessed on 10 November 2022).
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2020; Available online: https://www.R-project.org/ (accessed on 10 November 2022).
- Simmonds, M.J.; Derghazarian, T.; Vlaeyen, J.W.S. Physiotherapists’ Knowledge, Attitudes, and Intolerance of Uncertainty Influence Decision Making in Low Back Pain. Clin. J. Pain 2012, 28, 467–474. [Google Scholar] [CrossRef] [PubMed]
- Freeston, M.H.; Rhéaume, J.; Letarte, H.; Dugas, M.J.; Ladouceur, R. Why Do People Worry? Pers. Individ. Dif. 1994, 17, 791–802. [Google Scholar] [CrossRef]
- Weissenstein, A.; Ligges, S.; Brouwer, B.; Marschall, B.; Friederichs, H. Measuring the Ambiguity Tolerance of Medical Students: A Cross-Sectional Study from the First to Sixth Academic Years. BMC Fam. Pract. 2014, 15, 6. [Google Scholar] [CrossRef] [PubMed]
- Ying, L.D.; Harrington, A.; Assi, R.; Thiessen, C.; Contessa, J.; Hubbard, M.; Yoo, P.; Nadzam, G. Measuring Uncertainty Intolerance in Surgical Residents Using Standardized Assessments. J. Surg. Res. 2020, 245, 145–152. [Google Scholar] [CrossRef]
- Han, P.K.J.; Strout, T.D.; Gutheil, C.; Germann, C.; King, B.; Ofstad, E.; Gulbrandsen, P.; Trowbridge, R. How Physicians Manage Medical Uncertainty: A Qualitative Study and Conceptual Taxonomy. Orig. Artic. Med. Decis. Mak. 2021, 41, 275–291. [Google Scholar] [CrossRef]
- Santhosh, L.; Chou, C.L.; Connor, D.M. Diagnostic Uncertainty: From Education to Communication. Diagnosis 2019, 6, 121–126. [Google Scholar] [CrossRef]
- Ghosh, A.K. On the Challenges of Using Evidence-Based Information: The Role of Clinical Uncertainty. J. Lab. Clin. Med. 2004, 144, 60–64. [Google Scholar] [CrossRef]
- Hancock, J.; Mattick, K. Tolerance of Ambiguity and Psychological Well-Being in Medical Training: A Systematic Review. Med. Educ. 2020, 54, 125–137. [Google Scholar] [CrossRef]
- Reis-Dennis, S.; Gerrity, M.S.; Geller, G. Tolerance for Uncertainty and Professional Development: A Normative Analysis. J. Gen. Intern. Med. 2021, 36, 2408–2413. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).