Comparison of Procedural Content Item Generator versus Interactive Tool for Clinical Skills Acquisition in Physiotherapy Students
Abstract
1. Introduction
2. Materials and Methods
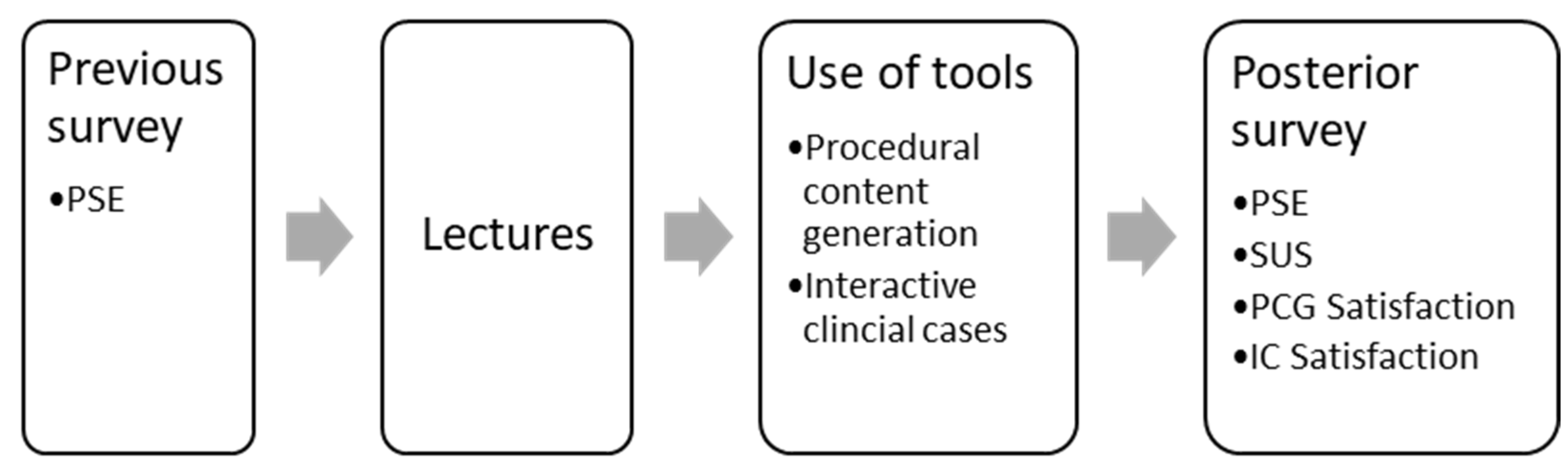
2.1. Design
2.2. Participants
2.3. Instrument
2.4. Assessment
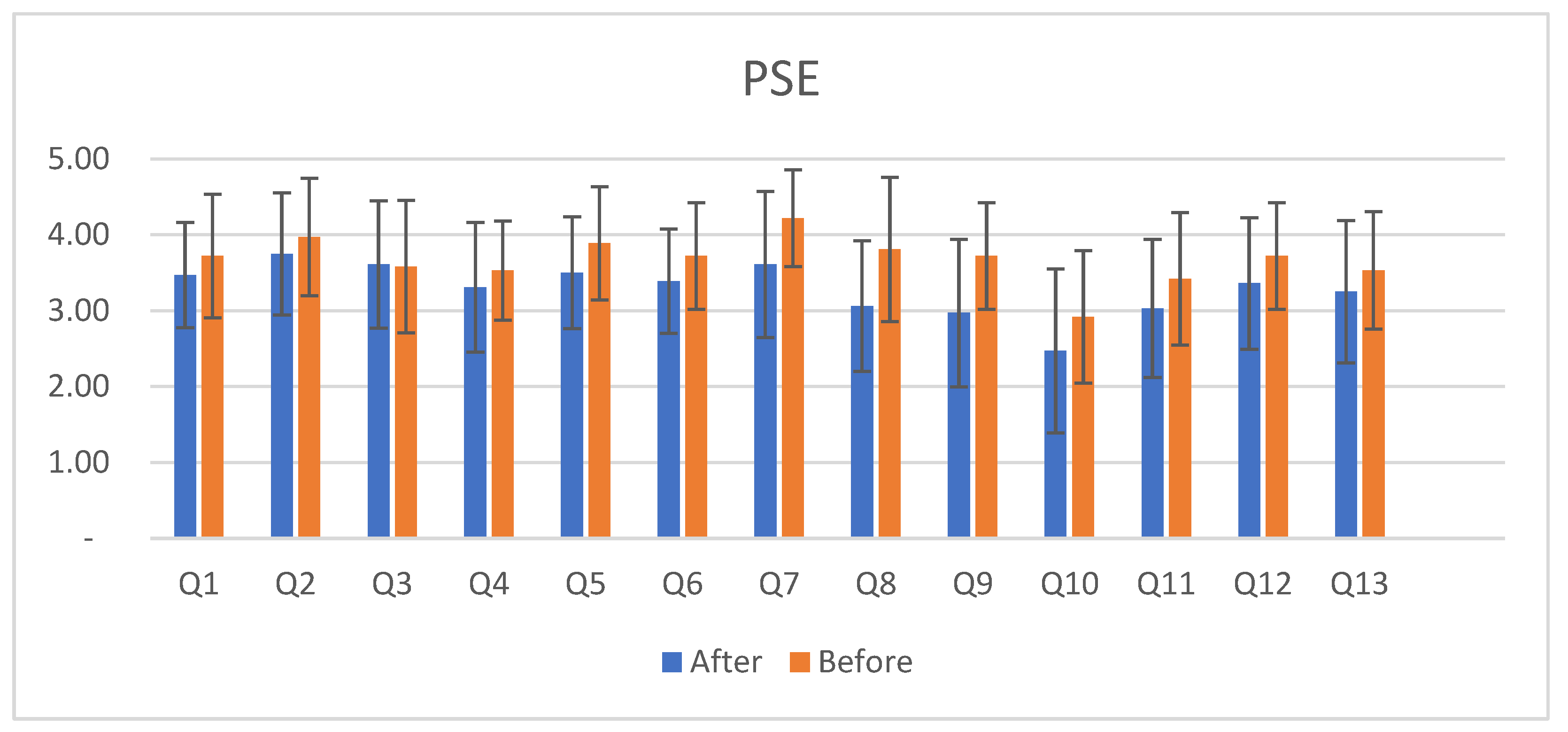
- We assessed self-efficacy using a Spanish version of the physiotherapy self-efficacy scale (PSE), which is being validated, based on the English version of the PSE [16]. Self-efficacy refers to an individual’s belief in their capacity to execute behaviors necessary to produce specific performance attainments. In the context of physiotherapy, self-efficacy is crucial as it can influence a patient’s motivation, adherence to treatment plans, and overall recovery outcomes. The PSE was answered at the beginning of the course (Before PSE) and after (After PSE) using the tools. We used only the results from the students who answered the PSE before and after the course.
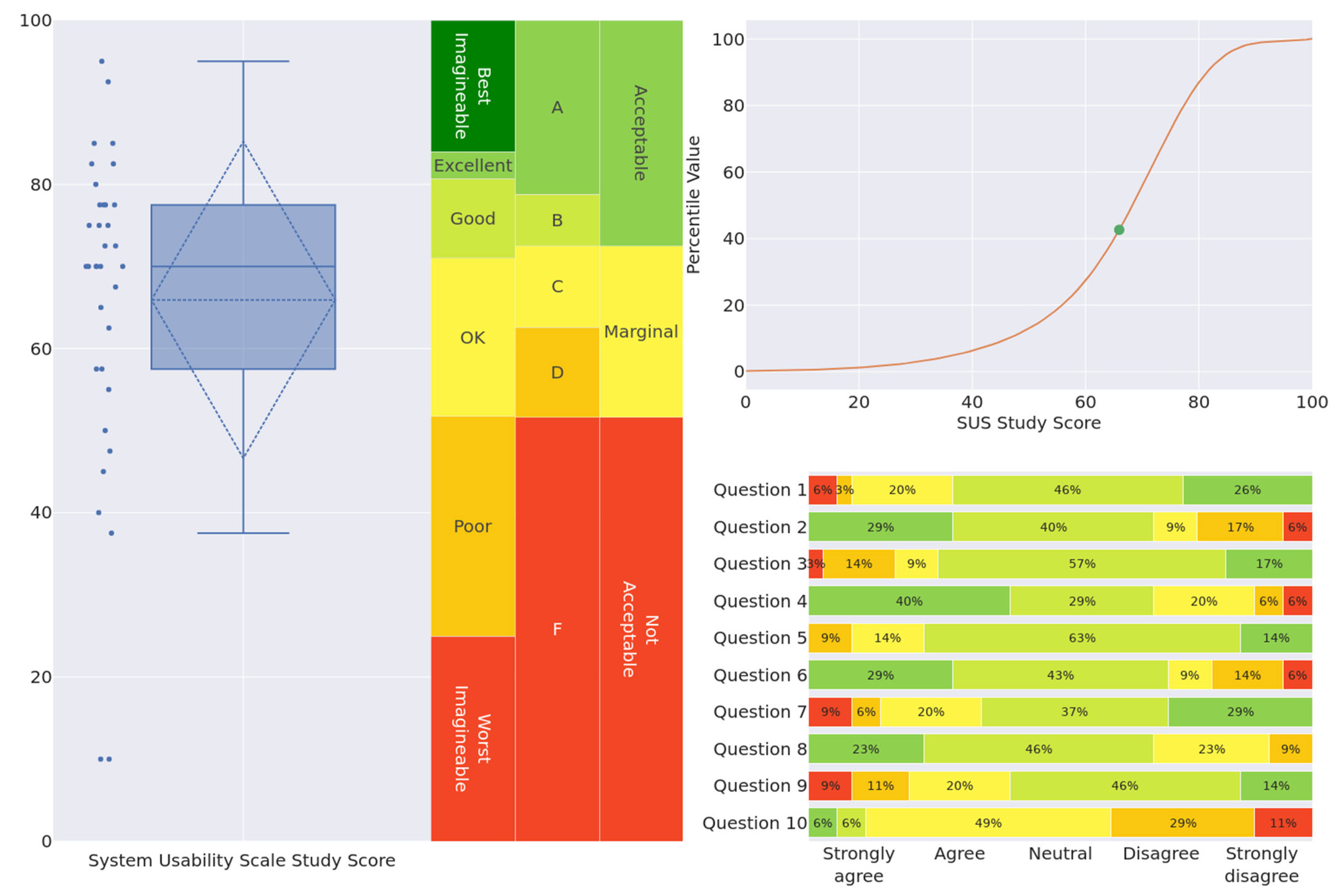
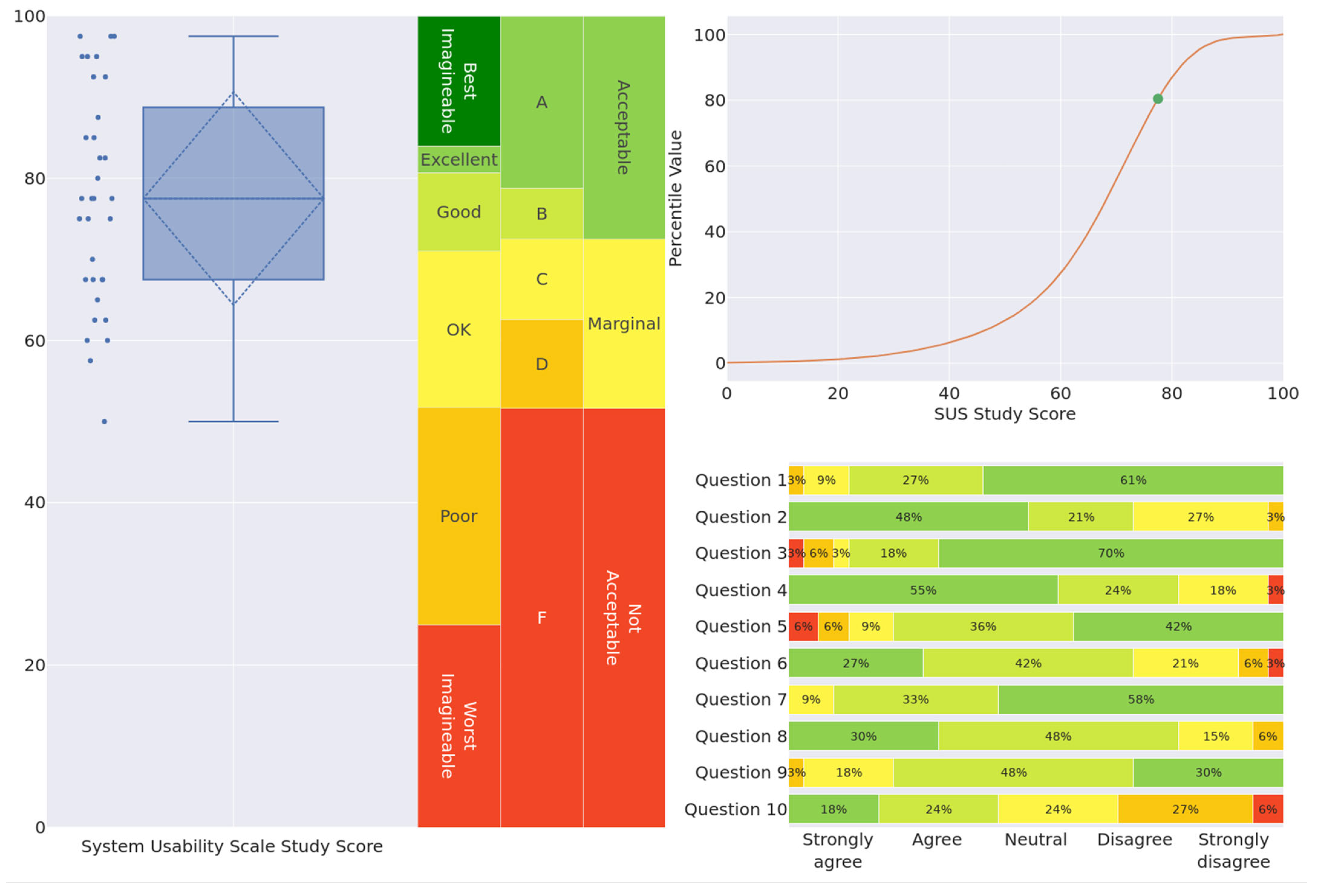
- To analyze the usability and user experience of the interactive tool, we used the Spanish, validated version of the System Usability Scale (SUS) [17]. It encompasses several key aspects: ease of use, effectiveness, efficiency, satisfaction, and learnability. The SUS is a Likert questionnaire that provides a specific score. The mean score will indicate the level of usability of PCG and ICs. The SUS scoring is interpreted as a percentage of usability, where a score above 80 indicates excellent usability, whereas a score under 50 indicates poor usability. Usually, the SUS results are converted into three scales: an adjective scale, a grade scale, and an acceptability scale. The adjective scale consists of the adjective ratings “Worst imaginable”, “Poor”, “OK”, “Good”, ”Excellent”, and “Best imaginable”. A grade scale is suggested using the traditional school grading scale from F to A. The acceptability scale classifies average SUS scores as “Acceptable”, “Marginal”, or “Not acceptable”. A percentile curve contextualization graph is also usually presented [18]. This graph shows the calculated SUS study scores from the uploaded dataset on a percentile curve derived from over 5000 SUS questionnaires. The data for this curve were taken from Sauro et al. [19]. Our study assessed the SUS of PCG and ICs after the students had used it.
- The survey aims to assess the impact of educational activities in a physiotherapy curriculum on several vital outcomes (Table 1): the relevance of acquired knowledge to practice, consolidation of course content, enhancement of problem-solving skills in real-case scenarios, integration of interdisciplinary knowledge, understanding of physiotherapy interventions, mastery of theoretical material, communication, and health education skills, and ability to assess patients’ functional status comprehensively. Additionally, it seeks student feedback on the preference for using clinical case-based approaches across other subjects.
2.5. Statistical Analysis
3. Results
3.1. Self-Efficacy
3.2. Usability
3.3. Satisfaction
4. Discussion
4.1. Theoretical Contribution
4.2. Practical Implications
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A
| Statement | 1 * | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| I feel adequately prepared to undertake a caseload. | 0 | 3 | 14 | 18 | 1 |
| I feel that I am able to verbally communicate effectively and appropriately for a caseload. | 0 | 1 | 14 | 14 | 7 |
| I feel that I am able to communicate in writing effectively and appropriately for a caseload. | 0 | 3 | 13 | 15 | 5 |
| I feel that I am able to perform subjective assessments for a caseload. | 1 | 3 | 19 | 10 | 3 |
| I feel that I am able to perform objective assessment for a caseload. | 0 | 3 | 14 | 17 | 2 |
| I feel that I am able to interpret assessment findings appropriate for a caseload. | 0 | 3 | 17 | 15 | 1 |
| I feel that I am able to identify and prioritize patient’s problems for a caseload. | 1 | 4 | 8 | 18 | 5 |
| I feel that I am able to select appropriate short and long term goals for a caseload. | 1 | 7 | 19 | 7 | 2 |
| I feel that I am able to appropriately perform treatments for a caseload. | 4 | 5 | 15 | 12 | 0 |
| I feel that I am able to perform discharge planning for a caseload. | 7 | 12 | 12 | 3 | 2 |
| I feel that I am able to evaluate my treatments for a caseload. | 2 | 7 | 16 | 10 | 1 |
| I feel that I am able to progress interventions appropriately for a caseload. | 1 | 4 | 14 | 15 | 2 |
| I feel that I am able to deal with the range of patient conditions which may be seen with a caseload. | 2 | 3 | 18 | 10 | 3 |
| Statement | 1 * | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| I feel adequately prepared to undertake a caseload. I feel that I am able to verbally communicate effectively and appropriately for a caseload. I feel that I am able to communicate in writing effectively and appropriately for a caseload. | 0 | 3 | 9 | 19 | 5 |
| 0 | 1 | 8 | 18 | 9 | |
| 0 | 4 | 12 | 15 | 5 | |
| I feel that I am able to perform subjective assessments for a caseload. I feel that I am able to perform objective assessment for a caseload. | 1 | 0 | 14 | 21 | 0 |
| 0 | 2 | 6 | 22 | 6 | |
| I feel that I am able to interpret assessment findings appropriate for a caseload. I feel that I am able to identify and prioritize patient’s problems for a caseload. I feel that I am able to select appropriate short and long term goals for a caseload. I feel that I am able to appropriately perform treatments for a caseload. | 0 | 1 | 12 | 19 | 4 |
| 0 | 0 | 4 | 20 | 12 | |
| 1 | 3 | 5 | 20 | 7 | |
| 0 | 2 | 9 | 22 | 3 | |
| I feel that I am able to perform discharge planning for a caseload. | 2 | 9 | 15 | 10 | 0 |
| I feel that I am able to evaluate my treatments for a caseload. | 0 | 6 | 12 | 15 | 3 |
| I feel that I am able to progress interventions appropriately for a caseload. | 0 | 1 | 12 | 19 | 4 |
| I feel that I am able to deal with the range of patient conditions which may be seen with a caseload. | 0 | 4 | 11 | 19 | 2 |
| Pair | Statement | Mean | Std. Deviation |
|---|---|---|---|
| 1 PREVIOUS | My training has adequately prepared me | 3.47 | 0.696 |
| 1 POSTERIOR | My training has adequately prepared me | 3.72 | 0.815 |
| 2 PREVIOUS | My training has adequately prepared me for verbally communicating effectively and appropriately. | 3.75 | 0.806 |
| 2 POSTERIOR | My training has adequately prepared me for verbally communicating effectively and appropriately. | 3.97 | 0.774 |
| 3 PREVIOUS | My training has adequately prepared me for communicating in writing effectively and appropriately. | 3.61 | 0.838 |
| 3 POSTERIOR | My training has adequately prepared me for communicating in writing effectively and appropriately. | 3.58 | 0.874 |
| 4 PREVIOUS | My training has adequately prepared me for performing subjective assessments. | 3.31 | 0.856 |
| 4 POSTERIOR | My training has adequately prepared me for performing subjective assessments. | 3.53 | 0.654 |
| 5 PREVIOUS | My training has adequately prepared me for performing objective assessments. | 3.50 | 0.737 |
| 5 POSTERIOR | My training has adequately prepared me for performing objective assessments. | 3.89 | 0.747 |
| 6 PREVIOUS | My training has adequately prepared me for interpreting assessment findings. | 3.39 | 0.688 |
| 6 POSTERIOR | My training has adequately prepared me for interpreting assessment findings. | 3.72 | 0.701 |
| 7 PREVIOUS | My training has adequately prepared me for identifying and prioritizing patients’ problems. | 3.61 | 0.964 |
| 7 POSTERIOR | My training has adequately prepared me for identifying and prioritizing patients’ problems. | 4.22 | 0.637 |
| 8 PREVIOUS | My training has adequately prepared me for selecting appropriate short- and long-term goals. | 3.06 | 0.860 |
| 8 POSTERIOR | My training has adequately prepared me for selecting appropriate short- and long-term goals. | 3.81 | 0.951 |
| 9 PREVIOUS | My training has adequately prepared me for appropriately performing treatments. | 2.97 | 0.971 |
| 9 POSTERIOR | My training has adequately prepared me for appropriately performing treatments. | 3.72 | 0.701 |
| 10 PREVIOUS | My training has adequately prepared me for performing discharge planning. | 2.47 | 1.082 |
| 10 POSTERIOR | My training has adequately prepared me for performing discharge planning. | 2.92 | 0.874 |
| 11 PREVIOUS | My training has adequately prepared me for evaluating my treatments. | 3.03 | 0.910 |
| 11 POSTERIOR | My training has adequately prepared me for evaluating my treatments. | 3.42 | 0.874 |
| 12 PREVIOUS | My training has adequately prepared me for progressing interventions appropriately. | 3.36 | 0.867 |
| Statement | 1 * | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| I think that I would like to use this system frequently. | 2 | 1 | 7 | 25 | 10 |
| I found the system unnecessarily complex. | 10 | 15 | 10 | 8 | 2 |
| I thought the system was easy to use. | 1 | 5 | 5 | 19 | 6 |
| I think that I would need the support of a technical person to be able to use this system. | 9 | 21 | 11 | 2 | 2 |
| I found the various functions in this system were well integrated. | 0 | 3 | 5 | 20 | 6 |
| I thought there was too much inconsistency in this system. | 11 | 15 | 9 | 8 | 2 |
| I would imagine that most people would learn to use this system very quickly. | 3 | 2 | 7 | 13 | 10 |
| I found the system very cumbersome to use. | 5 | 14 | 13 | 3 | 0 |
| I felt very confident using the system. | 3 | 5 | 8 | 14 | 5 |
| I needed to learn a lot of things before I could get going with this system. | 3 | 2 | 10 | 16 | 4 |
| Statement | 1 * | 2 | 3 | 4 | 5 |
|---|---|---|---|---|---|
| I think that I would like to use this system frequently. | 0 | 1 | 3 | 9 | 20 |
| I found the system unnecessarily complex. | 15 | 15 | 17 | 1 | 0 |
| I thought the system was easy to use. | 1 | 2 | 2 | 9 | 22 |
| I think that I would need the support of a technical person to be able to use this system. | 18 | 14 | 15 | 0 | 1 |
| I found the various functions in this system were well integrated. | 2 | 2 | 3 | 16 | 14 |
| I thought there was too much inconsistency in this system. | 15 | 14 | 16 | 2 | 1 |
| I would imagine that most people would learn to use this system very quickly. | 0 | 0 | 3 | 14 | 19 |
| I found the system very cumbersome to use. | 8 | 21 | 7 | 2 | 0 |
| I felt very confident using the system. | 0 | 1 | 6 | 16 | 10 |
| I needed to learn a lot of things before I could get going with this system. | 5 | 6 | 9 | 16 | 2 |
| Statement | Totally Disagree | Disagree | Slightly Disagree | Slightly Agree | Agree | Totally Agree |
|---|---|---|---|---|---|---|
| To what extent would you like these types of clinical cases to be used in other subjects? | 2 | 3 | 12 | 7 | 15 | 24 |
| The content of the activity allows me to assess the patient’s functional status, considering the physical, psychological, and social aspects | 5 | 6 | 8 | 10 | 18 | 16 |
| The content of the activity allows me to establish effective communication with patients, family, social groups, and peers and to promote health education. | 4 | 7 | 11 | 9 | 23 | 9 |
| I believe I have a good command of the theoretical material of the General Physiotherapy Procedures II course | 5 | 5 | 13 | 17 | 17 | 6 |
| Carrying out the activity allows me a better understanding of the possibilities and limitations of interventions in physiotherapy | 6 | 6 | 5 | 10 | 15 | 21 |
| The content of the activity helps me integrate and relate the knowledge acquired from this and other subjects by applying them to a real clinical case | 6 | 5 | 9 | 8 | 19 | 16 |
| The knowledge acquired during the activity enables me to better identify and analyze the crucial elements to solve the problems of a real case | 6 | 4 | 7 | 9 | 20 | 17 |
| The content of the activity helps me consolidate the knowledge acquired in the General Physiotherapy Procedures II course | 6 | 7 | 3 | 15 | 19 | 13 |
| The knowledge acquired during the activity is relevant for the practice of physiotherapy | 7 | 4 | 9 | 8 | 18 | 17 |
| Statement | Totally Disagree | Disagree | Slightly Disagree | Slightly Agree | Agree | Totally Agree |
|---|---|---|---|---|---|---|
| To what extent would you like these types of clinical cases to be used in other subjects? | 1 | 0 | 8 | 7 | 12 | 35 |
| The content of the activity allows me to assess the patient’s functional status, considering the physical, psychological, and social aspects | 1 | 2 | 9 | 6 | 23 | 22 |
| The content of the activity allows me to establish effective communication with patients, family, social groups, and peers and to promote health education. | 1 | 1 | 9 | 8 | 24 | 20 |
| I believe I have a good command of the theoretical material of the General Physiotherapy Procedures II course | 1 | 2 | 10 | 17 | 18 | 15 |
| Carrying out the activity allows me a better understanding of the possibilities and limitations of interventions in physiotherapy | 1 | 0 | 5 | 7 | 20 | 30 |
| The content of the activity helps me integrate and relate the knowledge acquired from this and other subjects by applying them to a real clinical case | 1 | 1 | 8 | 4 | 18 | 31 |
| The knowledge acquired during the activity enables me to better identify and analyze the crucial elements to solve the problems of an actual case | 2 | 1 | 5 | 6 | 21 | 28 |
| The content of the activity helped me consolidate the knowledge acquired in the General Physiotherapy Procedures II course | 1 | 2 | 5 | 6 | 18 | 31 |
| The knowledge acquired during the activity is relevant to the practice of physiotherapy | 1 | 0 | 6 | 6 | 21 | 29 |
References
- Perez, A.; Green, J.; Moharrami, M.; Gianoni-Capenakas, S.; Kebbe, M.; Ganatra, S.; Sharmin, N. Active learning in undergraduate classroom dental education—A scoping review. PLoS ONE 2023, 18, e0293206. [Google Scholar] [CrossRef] [PubMed]
- Stanley, T. Case-Based Learning. In Authentic Learning; Routledge: New York, NY, USA, 2021; pp. 79–90. [Google Scholar] [CrossRef]
- Thistlethwaite, J.E.; Davies, D.; Ekeocha, S.; Kidd, J.M.; MacDougall, C.; Matthews, P.; Clay, D. The effectiveness of case-based learning in health professional education. A BEME systematic review: BEME Guide No. 23. Med. Teach. 2012, 34, e421–e444. [Google Scholar] [CrossRef] [PubMed]
- Ulvik, M.; Eide, H.M.K.; Eide, L.; Helleve, I.; Jensen, V.S.; Ludvigsen, K.; Torjussen, L.P.S. Teacher educators reflecting on case-based teaching—A collective self-study. Prof. Dev. Educ. 2022, 48, 657–671. [Google Scholar] [CrossRef]
- Gravett, S.; de Beer, J.; Odendaal-Kroon, R.; Merseth, K.K. The affordances of case-based teaching for the professional learning of student-teachers. J. Curric. Stud. 2016, 49, 369–390. [Google Scholar] [CrossRef]
- Rose’Meyer, R.; Singh, I. Digital Technologies for Teaching for Allied Healthcare Students and Future Directions. In Emerging Technologies and Work-Integrated Learning Experiences in Allied Health Education; Singh, I., Raghuvanshi, K., Eds.; IGI Global: Hershey, PA, USA, 2018; pp. 301–317. [Google Scholar] [CrossRef]
- Serbezova, I.; Hristova, T.; Lukanova, Y. E-Learning in Healthcare Within Higher Education. Knowl. Int. J. 2019, 34, 475–481. [Google Scholar] [CrossRef]
- Pickering, J.D. Developing the Evidence-Base to Support the Integration of Technology-Enhanced Learning in Healthcare Education. Med. Sci. Educ. 2017, 27, 903–905. [Google Scholar] [CrossRef]
- Kilgour, J.M.; Grundy, L.; Monrouxe, L.V. A Rapid Review of the Factors Affecting Healthcare Students’ Satisfaction with Small-Group, Active Learning Methods. Teach. Learn. Med. 2016, 28, 15–25. [Google Scholar] [CrossRef]
- Luo, S.; Yang, H.H. Using technologies in nursing research education: A Mixed Methods Case Study. CIN—Comput. Inform. Nurs. 2018, 36, 293–304. [Google Scholar] [CrossRef]
- Smart, D.; Ross, K.; Carollo, S.; Williams-Gilbert, W. Contextualizing instructional technology to the demands of nursing education. CIN—Comput. Inform. Nurs. 2020, 38, 18–27. Available online: https://journals.lww.com/cinjournal/fulltext/2020/01000/contextualizing_instructional_technology_to_the.4.aspx (accessed on 17 July 2024). [CrossRef]
- Aycock, J. Procedural Content Generation. In Retrogame Archeology; Springer International Publishing: Cham, Switzerland, 2016; pp. 109–143. [Google Scholar]
- Murdoch, N.L.; Bottorff, J.L.; McCullough, D. Simulation education approaches to enhance collaborative healthcare: A best practices review. Int. J. Nurs. Educ. Sch. 2014, 10, 307–321. [Google Scholar] [CrossRef]
- Des Jarlais, D.C.; Lyles, C.; Crepaz, N.; Trend Group. CDC Improving the Reporting Quality of Nonrandomized Evaluations of Behavioral and Public Health Interventions: The TREND Statement. Am. J. Public Health 2004, 94, 361–366. [Google Scholar] [CrossRef] [PubMed]
- Lam, O.T.; Strenger, D.M.; Chan-Fee, M.; Pham, P.T.; Preuss, R.A.; Robbins, S.M. Effectiveness of the McKenzie Method of Mechanical Diagnosis and Therapy for Treating Low Back Pain: Literature Review With Meta-analysis. J. Orthop. Sports Phys. Ther. 2018, 48, 476–490. [Google Scholar] [CrossRef] [PubMed]
- Van Lankveld, W.; Jones, A.; Brunnekreef, J.J.; Seeger, J.P.H.; Bart Staal, J. Assessing physical therapist students’ self-efficacy: Measurement properties of the Physiotherapist Self-Efficacy (PSE) questionnaire. BMC Med. Educ. 2017, 17, 250. [Google Scholar] [CrossRef] [PubMed]
- Sevilla-Gonzalez, M.D.R.; Loaeza, L.M.; Lazaro-Carrera, L.S.; Ramirez, B.B.; Rodríguez, A.V.; Peralta-Pedrero, M.L.; Almeda-Valdes, P. Spanish version of the system usability scale for the assessment of electronic tools: Development and validation. JMIR Hum. Factors 2020, 7, e21161. [Google Scholar] [CrossRef] [PubMed]
- Blattgerste, J.; Behrends, J.; Pfeiffer, T. A Web-Based Analysis Toolkit for the System Usability Scale. In Proceedings of the 15th International Conference on PErvasive Technologies Related to Assistive Environments (PETRA ’22), Corfu, Greece, 29 June–1 July 2022. [Google Scholar] [CrossRef]
- Sauro, J.; Lewis, J.R. Standardized Usability Questionnaires. Quantifying User Exp. 2012, 185–240. [Google Scholar] [CrossRef]
- Xu, Y.; Smeets, R.; Bidarra, R. Procedural generation of problems for elementary math education. Int. J. Serious Games 2021, 8, 49–66. [Google Scholar] [CrossRef]
- Hooshyar, D.; Yousefi, M.; Lim, H. A Procedural Content Generation-Based Framework for Educational Games: Toward a Tailored Data-Driven Game for Developing Early English Reading Skills. J. Educ. Comput. Res. 2017, 56, 293–310. [Google Scholar] [CrossRef]
- Gierl, M.J.; Lai, H. Evaluating the quality of medical multiple-choice items created with automated processes. Med. Educ. 2013, 47, 726–733. [Google Scholar] [CrossRef]
- Kıyak, Y.S.; Budakoğlu, I.İ.; Coşkun, Ö.; Koyun, E. The First Automatic Item Generation in Turkish for Assessment of Clinical Reasoning in Medical Education. Tıp Eğitimi Dünyası 2023, 22, 72–90. [Google Scholar] [CrossRef]
- Gierl, M.J.; Lai, H.; Pugh, D.; Touchie, C.; Boulais, A.P.; De Champlain, A. Evaluating the Psychometric Characteristics of Generated Multiple-Choice Test Items. Appl. Meas. Educ. 2016, 29, 196–210. [Google Scholar] [CrossRef]
- Lai, H.; Gierl, M.J.; Touchie, C.; Pugh, D.; Boulais, A.P.; De Champlain, A. Using Automatic Item Generation to Improve the Quality of MCQ Distractors. Teach. Learn. Med. 2016, 28, 166–173. [Google Scholar] [CrossRef] [PubMed]
- Shappell, E.; Podolej, G.; Ahn, J.; Tekian, A.; Park, Y.S. Notes From the Field: Automatic Item Generation, Standard Setting, and Learner Performance in Mastery Multiple-Choice Tests. Eval. Health Prof. 2020, 44, 315–318. [Google Scholar] [CrossRef] [PubMed]
- Jones, A.; Sheppard, L. Self-efficacy and clinical performance: A physiotherapy example. Adv. Physiother. 2011, 13, 79–83. [Google Scholar] [CrossRef]
- Hough, J.; Levan, D.; Steele, M.; Kelly, K.; Dalton, M. Simulation-based education improves student self-efficacy in physiotherapy assessment and management of paediatric patients. BMC Med. Educ. 2019, 19, 463. [Google Scholar] [CrossRef]
- Forbes, R.; Mandrusiak, A.; Smith, M.; Russell, T. Training physiotherapy students to educate patients: A randomised controlled trial. Patient Educ. Couns. 2018, 101, 295–303. [Google Scholar] [CrossRef]
- van Lankveld, W.; Maas, M.; van Wijchen, J.; Visser, V.; Staal, J.B. Self-regulated learning in physical therapy education: A non-randomized experimental study comparing self-directed and instruction-based learning. BMC Med. Educ. 2019, 19, 50. [Google Scholar] [CrossRef] [PubMed]
- Young, C. Initiating self-assessment strategies in novice physiotherapy students: A method case study. Assess. Eval. High. Educ. 2013, 38, 998–1011. [Google Scholar] [CrossRef]
- Fu, W. Development of an Innovative Tool to Assess Student Physical Therapists’ Clinical Reasoning Competency. J. Phys. Ther. Educ. 2015, 29, 14–26. [Google Scholar] [CrossRef]
- Abbaszadeh-Amirdehi, M.; Talebi, G.; Gholamnia-Shirvani, Z.; Ghaemi-Amiri, M.; Taghipour, M.; Javanshir, K.; Mousavi-Khatir, S.R. Assessment through Objective Structured Clinical Examination: How to Promote the Satisfaction of Physiotherapy Students. J. Mod. Rehabil. 2023, 17, 21–26. [Google Scholar] [CrossRef]
- Furze, J.; Gale, J.R.; Black, L.; Cochran, T.M.; Jensen, G.M. Clinical Reasoning: Development of a Grading Rubric for Student Assessment. J. Phys. Ther. Educ. 2015, 29, 34–45. [Google Scholar] [CrossRef]
- Riopel, M.A.; Benham, S.; Landis, J.; Falcone, S.; Harvey, S. The Clinical Reasoning Assessment Tool for Learning from Standardized Patient Experiences: A Pilot Study. Internet J. Allied Health Sci. Practice. 2022, 20, 9. [Google Scholar] [CrossRef]
- Van Nuland, S.E.; Eagleson, R.; Rogers, K.A. Educational software usability: Artifact or Design? Anat. Sci. Educ. 2016, 10, 190–199. [Google Scholar] [CrossRef] [PubMed]
- Scott, J.E. Technology Acceptance and ERP Documentation Usability. Commun. ACM 2008, 51, 121–124. [Google Scholar] [CrossRef]
- Granić, A. Experience with usability evaluation of e-learning systems. Univers. Access Inf. Soc. 2008, 7, 209–221. [Google Scholar] [CrossRef]
- Aileni, R.M.; Radulescu, R.I.; Chiriac, L. A new perspective in e-learning training toolkit development for advanced textile research centres in Morocco and Jordan. Ind. Textila 2021, 72, 569–578. [Google Scholar] [CrossRef]
- Bourges-Waldegg, P.; Moreno, L.; Rojano, T. The role of usability on the implementation and evaluation of educational technology. In Proceedings of the Annual Hawaii International Conference on System Sciences, Maui, HI, USA, 7 January 2000. [Google Scholar]
- Gendreau, E.; Summers, J.D.; Benhayoun-Sadafiyine, L.; Le Dain, M.A. Investigating Usability of an Innovation Management Decision Aid. In Proceedings of the ASME Design Engineering Technical Conference, Anaheim, CA, USA, 18–21 August 2019. [Google Scholar] [CrossRef]
- Jiménez-Mejías, E.; Amezcua-Prieto, C.; Martínez-Ruiz, V.; Olvera-Porcel, M.C.; Jiménez-Moleón, J.J.; Lardelli Claret, P. Medical students’ satisfaction and academic performance with problem-based learning in practice-based exercises for epidemiology and health demographics. Innov. Educ. Teach. Int. 2013, 52, 510–521. [Google Scholar] [CrossRef]
- Younis, G.A.; Al-Metyazidy, H.A. Effectiveness of High Fidelity Simulation versus Traditional Clinical Teaching Strategies on Undergraduate Nursing Students’ Achievement. Int. J. Nurs. Didact. 2016, 6, 1–13. [Google Scholar] [CrossRef]
- Tolsgaard, M.G.; Gustafsson, A.; Rasmussen, M.B.; Høiby, P.; Müller, C.; Ringsted, C. Student teachers can be as good as associate professors in teaching clinical skills. Med. Teach. 2007, 29, 553–557. [Google Scholar] [CrossRef]
- Steinert, Y.; Mann, K.; Centeno, A.; Dolmans, D.; Spencer, J.; Gelula, M.; Prideaux, D. A systematic review of faculty development initiatives designed to improve teaching effectiveness in medical education: BEME Guide No. 8. Med. Teach. 2006, 28, 497–526. [Google Scholar] [CrossRef]
- Nickles, D.; Dolansky, M.; Marek, J.; Burke, K. Nursing students use of teach-back to improve patients’ knowledge and satisfaction: A quality improvement project. J. Prof. Nurs. 2020, 36, 70–76. [Google Scholar] [CrossRef] [PubMed]
- Feixas, M.; Martínez-Usarralde, M.J.; López-Martín, R. Do teaching innovation projects make a difference? Assessing the impact of small-scale funding. Tert. Educ. Manag. 2018, 24, 267–283. [Google Scholar] [CrossRef]
- Bandura, A. Self-Efficacy: The Exercise of Control; Worth Publishers: Broadway, UK, 1997. [Google Scholar]
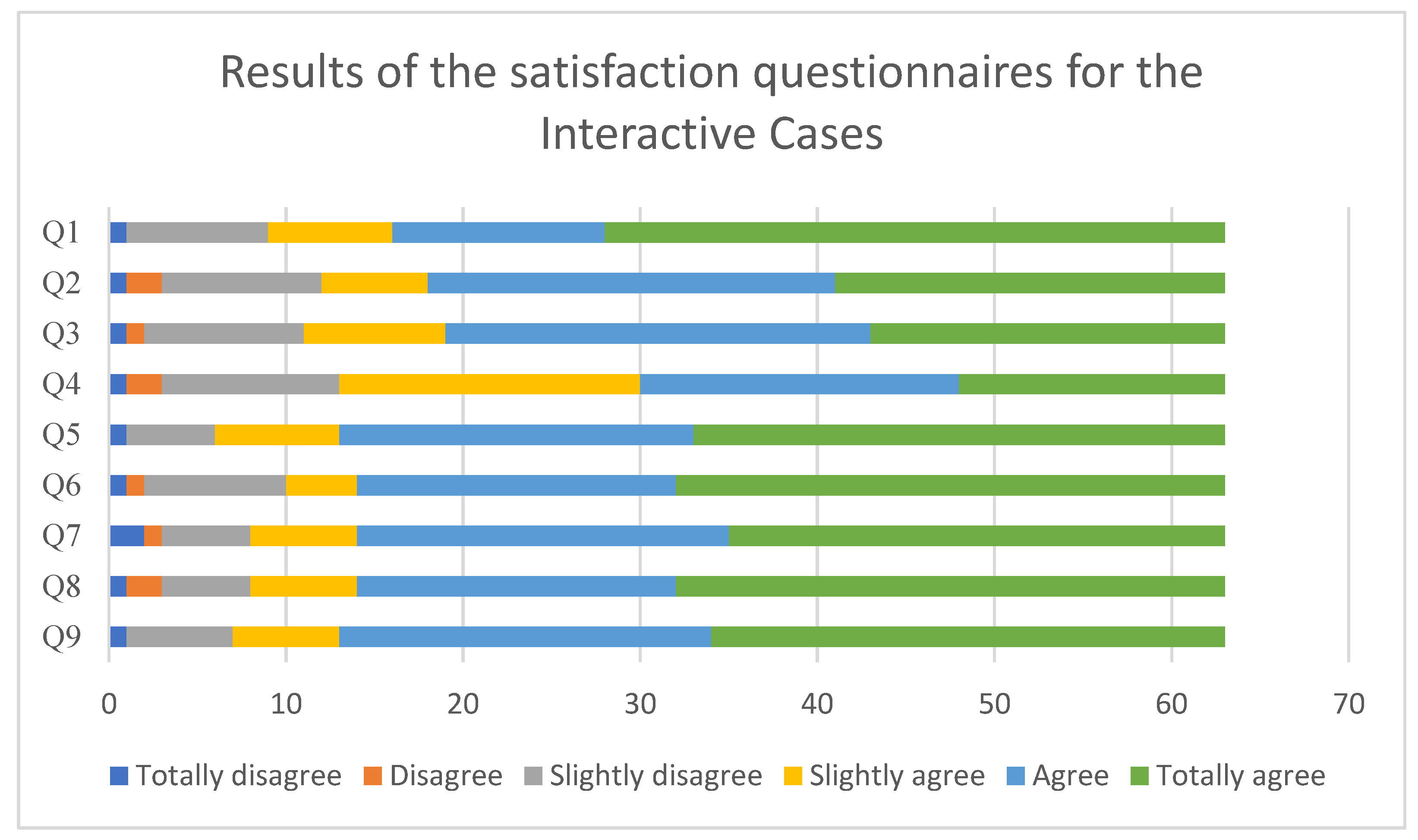
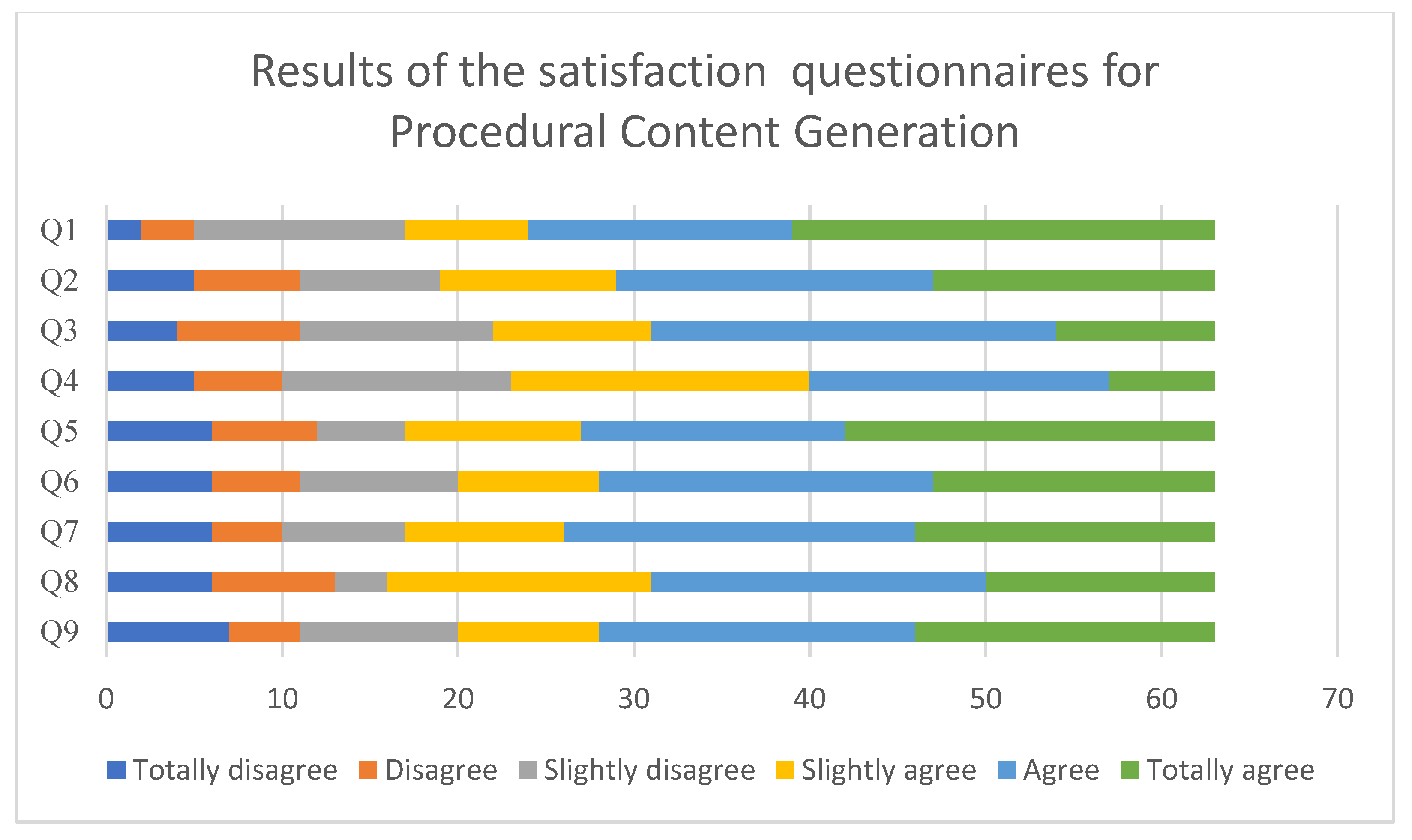
| Statement |
|---|
| 1. To what extent would you like these types of clinical cases to be used in other subjects? |
| 2. The content of the activity allows me to establish effective communication with patients, family, social groups, and peers and to promote health education. |
| 3. The content of the activity allows me to assess the patient’s functional status, considering the physical, psychological, and social aspects |
| 4. I believe I have a good command of the theoretical material of the Methods in Physiotherapy course |
| 5. Carrying out the activity allows me a better understanding of the possibilities and limitations of interventions in physiotherapy |
| 6. The content of the activity helps me integrate and relate the knowledge acquired from this and other subjects by applying them to a real clinical case |
| 7. The knowledge acquired during the activity enables me to better identify and analyze the crucial elements to solve the problems of a real case |
| 8. The content of the activity helps me consolidate the knowledge acquired in the Methods in Physiotherapy course |
| 9. The knowledge acquired during the activity is relevant for the practice of physiotherapy |
| Before PSE (n = 63) | After PSE (n = 36) | SUS (PCG) (n = 35) | SUS (IC) (n = 33) | Satisfaction (n = 63) | |
|---|---|---|---|---|---|
| Gender | |||||
| Male | 26 | 16 | 20 | 18 | 31 |
| Female | 36 | 19 | 16 | 15 | 31 |
| Nonbinary | 1 | 1 | 0 | 0 | 1 |
| Mean age (standard deviation) | 21.30 (2.39) | 21.03 (4.11) | 22.93 (4.64) | 22.22 (4.00) | 21.97 (3.26) |
| Degree | |||||
| Science of physical activities and sport + physiotherapy | 25 | 8 | 8 | 6 | 14 |
| Nursing + physiotherapy | 17 | 14 | 17 | 8 | 21 |
| Human nutrition + physiotherapy | 13 | 10 | 4 | 13 | 11 |
| Physiotherapy | 8 | 4 | 8 | 6 | 17 |
| Metric/Question | PCG | IC |
|---|---|---|
| SUS Study Score | 65.93 | 77.5 |
| Median | 70 | 77.5 |
| Standard Deviation | 19.3 | 13.13 |
| Adjective | OK | Good |
| Grade | C | B |
| Acceptability | Marginal | Acceptable |
| Quartile | 2nd | 3rd |
| Conclusiveness | 100% | 100 |
| Answers to the questions | PCG | IC |
| Q1: I think that I would like to use this system frequently. | 7.07 | 8.64 |
| Q2: I found the system unnecessarily complex. | 6.71 | 7.88 |
| Q3: I thought the system was easy to use. | 6.79 | 8.64 |
| Q4: I think that I would need the support of a technical person to be able to use this system. | 7.29 | 8.18 |
| Q5: I found the various functions in this system were well integrated. | 7.07 | 7.58 |
| Q6: I thought there was too much inconsistency in this system. | 6.86 | 7.12 |
| Q7: I imagine most people would learn to use this system very quickly. | 6.79 | 8.71 |
| Q8: I found the system very cumbersome to use. | 7.07 | 7.58 |
| Q9: I felt very confident using the system. | 6.14 | 7.65 |
| Q10: I needed to learn a lot of things before I could get going with this system. | 4.14 | 5.53 |
| Number | Questions |
|---|---|
| Q1 | To what extent would you like these types of clinical cases to be used in other subjects? |
| Q2 | The content of the activity allows me to assess the patient’s functional status, considering the physical, psychological, and social aspects |
| Q3 | The content of the activity allows me to establish effective communication with patients, family, social groups, and peers and to promote health education. |
| Q4 | I believe I have a good command of the theoretical material of the Methods in Physiotherapy course |
| Q5 | Carrying out the activity allows me a better understanding of the possibilities and limitations of interventions in physiotherapy |
| Q6 | The content of the activity helps me integrate and relate the knowledge acquired from this and other subjects by applying them to a real clinical case |
| Q7 | The knowledge acquired during the activity enables me to better identify and analyze the crucial elements to solve the problems of a real case |
| Q8 | The content of the activity helps me consolidate the knowledge acquired in the Methods in Physiotherapy course |
| Q9 | The knowledge acquired during the activity is relevant for the practice of physiotherapy |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Barranco-i-Reixachs, D.; Bravo, C.; Fernández-Lago, H.; Martínez-Soldevila, J.; Martínez-Navarro, O.; Masbernat-Almenara, M.; Rubí-Carnacea, F. Comparison of Procedural Content Item Generator versus Interactive Tool for Clinical Skills Acquisition in Physiotherapy Students. Educ. Sci. 2024, 14, 1049. https://doi.org/10.3390/educsci14101049
Barranco-i-Reixachs D, Bravo C, Fernández-Lago H, Martínez-Soldevila J, Martínez-Navarro O, Masbernat-Almenara M, Rubí-Carnacea F. Comparison of Procedural Content Item Generator versus Interactive Tool for Clinical Skills Acquisition in Physiotherapy Students. Education Sciences. 2024; 14(10):1049. https://doi.org/10.3390/educsci14101049
Chicago/Turabian StyleBarranco-i-Reixachs, David, Cristina Bravo, Helena Fernández-Lago, Jordi Martínez-Soldevila, Oriol Martínez-Navarro, Maria Masbernat-Almenara, and Francesc Rubí-Carnacea. 2024. "Comparison of Procedural Content Item Generator versus Interactive Tool for Clinical Skills Acquisition in Physiotherapy Students" Education Sciences 14, no. 10: 1049. https://doi.org/10.3390/educsci14101049
APA StyleBarranco-i-Reixachs, D., Bravo, C., Fernández-Lago, H., Martínez-Soldevila, J., Martínez-Navarro, O., Masbernat-Almenara, M., & Rubí-Carnacea, F. (2024). Comparison of Procedural Content Item Generator versus Interactive Tool for Clinical Skills Acquisition in Physiotherapy Students. Education Sciences, 14(10), 1049. https://doi.org/10.3390/educsci14101049






