Abstract
Refugee children displaced by war suffer incredible amounts of physical and psychological trauma during and post-displacement. War is not partial to children, and they are subjected to as much extreme violence as adults. This paper explores the mental health of refugee children following war and was guided by the research question: What are the mental health experiences of refugee children displaced by war situations? A secondary data analysis was conducted on publicly available documentary short films and instructional videos on psychological therapy with refugee children and families. The data were analysed through Qualitative Conventional Content Analysis (QCCA). Three major categories emerged regarding the well-being of refugee children: (1) children are not spared from war trauma, (2) children live in perpetual fear and anxiety, and (3) war-related violence ignites aggressive behaviours in children. To increase positive mental health outcomes, school psychologists need to implement trauma-informed therapy that focuses on decreasing psychosocial reactions to war. Culturally responsive therapy is recommended as it places indigenous ways of being at the centre of the healing process.
1. Introduction
There are approximately 89.3 million people displaced from their homes and country of origin due to human rights violations [1]. While thirty percent of the world’s population is made up of children, they account for forty-one percent of the refugee population [2]. A startling 34.15 million children are displaced due to forced migration, and a third of children living outside their country of origin are refugees, compared to one in twenty adults [1,3]. Thus, there are disproportionately high amounts of refugee children living in displacement. Additionally, a significant number of refugee children relocate without their families, bringing the total to about 153,300 unaccompanied and separated children worldwide [1]. As a result of war and forced migration, refugee children have often experienced extreme violence and may be living with numerous mental health issues. Poor mental health negatively impacts academic, social, and psychological development. School psychologists have a pivotal role in increasing refugee children’s mental well-being. Yet, schools seem underprepared for diversity and inclusion [4], and many school psychologists are still unaware of evidence-based treatments that are culturally appropriate for non-White student populations [5].
The purpose of this study is to explore the mental health of refugee children displaced by war and conflict. The study makes recommendations for school psychologists to implement trauma-informed therapies that are culturally responsive. Culturally responsive therapy (CRT) acknowledges that clients bring diverse cultural mental health knowledge and healing practices that are essential, valuable, and deserving of inclusion in psychotherapy.
1.1. Background
1.1.1. Migration Experiences That Trigger Poor Mental Health
Thematically, refugee migration can be divided into three phases: pre-migration, migration, and post-migration [6]. Premigration includes events that trigger refugees’ flight from their homes and communities into displacement. In the context of armed conflict, these events are often violent. For example, during the DRC electoral civil unrest, armed soldiers were sent into villages to persecute unarmed citizens who had raised concerns about the fairness of the electoral processes [7]. Soldiers burned and destroyed homes and public infrastructure; they kidnapped, killed, and sexually assaulted adults and forced children into the military [7]. Thus, during pre-migration, children witness traumatic events such as kidnappings, arrests, imprisonment, torture, or killings of family and community members [8,9]. The migration phase is a temporary residence between displacement and resettlement; during this time, many children and their families live in informal settlements, such as refugee camps. Temporary encampments do not have adequate resources to meet human needs. There is inadequate housing, poor sanitation, low-quality water, and poor-grade food [9]. There are also no schools, hospitals, or employment opportunities [10,11]. Therefore, during migration, children live in dire poverty, do not attend schools, and do not receive proper physical and mental health care. Some children also experience sexual and physical abuse [11]. The stress of living in refugee encampments can lead to Post-Traumatic Stress Disorder (PTSD), depression, anxiety, and somatisation symptoms in children and adults alike [11]. Post-migration is the permanent resettlement into a host country after asylum has been granted. Post-migration offers families an opportunity to resettle in a new country and rebuild their lives, but like any other life transition, it comes with its stressors. Lengthy asylum processes, insecure immigration statuses, and political barriers can increase vulnerability to poor mental well-being [12]. Resettlement stressors for children include acculturation into new cultures, communities, and schools. Acculturation begins with learning the local language, and the inability to speak the local language may impede learning and cause school-related barriers [13]. Additionally, host communities are not always receptive to refugees, and children can face social injustice, isolation, and rejection [14]. Research reports that children who had experienced discrimination were more likely to have symptoms of PTSD and depression [15].
All migrant and non-migrant children with mental health challenges deserve quality health care. Refugee children’s mental well-being is unique for several reasons. Firstly, refugee children have experienced severe cumulative trauma across the migration stages. Open war trauma and forced migration “rank among the most traumatic life experiences” [16]. This alone should make the mental well-being of refugee children an urgent school agenda. Secondly, refugee children are underrepresented in mental health services [17]; family factors such as limited mental health knowledge [18], a shortage in finances, transportation, and time make it challenging for refugee parents to access help for their children [19]. In addition to conducting their professional roles, school psychologists have the task of increasing access to mental health care for displaced children. Lastly, because of COVID-19, the global rates of mental health for non-migrant children have risen. World reports are showing similar rates of anxiety and depression in migrant and non-migrant children. Nevertheless, psychologists should consider that refugee mental health tends to be comorbid; for example, refugee youth with anxiety also present with depression and PTSD symptoms [20,21]. Considering the unique nature of refugee children’s mental health, this study recommends an inclusive therapy framework, culturally responsive therapy (CRT), for the mental health care of refugee children. Through inclusion, schools have the potential to become places of genuine refuge for displaced children.
1.1.2. Rates of Mental Health Difficulties Refugee Children
COVID-19 decreased the mental well-being of all children around the world [22,23], making mental health rates of anxiety and depression in non-immigrant children similar to those of refugee children. For example, 36.6% of non-immigrant children in China reported suffering from depression, and 19% reported experiencing anxiety disorders [24]. Furthermore, 24.1% of non-immigrant children in Germany reported anxiety symptoms [25], and 30.6% of children in the United Kingdom reported psychological distress [26]. The mental health of refugee children during COVID-19 has not been widely documented [22]. However, before COVID-19, 15.77% of refugee children worldwide presented with anxiety disorders [27]. Recently, 23.2–28.9% of Ukrainian refugee children exposed to the recent war reported anxiety disorders [8]. While post-COVID-19 rates of anxiety and depression in non-migrant and migrant children may be comparative, what is also unique about the mental health of refugee children is the aetiology, nature, and reasons for the difficulties. Refugee children’s mental health rates differ based on the type of exposure to violence (i.e., indirect or direct exposure to war) and immigration status (accompanied versus unaccompanied minors). Overall, 38.2% of unaccompanied refugee minors and 23.3% of accompanied minors reported anxiety symptoms [28], compared to 9.2% of Syrian children exposed to war violence [21]. Unaccompanied minors may report higher rates of distress because they have lost family during migration, and they arrive in the resettlement country alone. Depression rates are also country- and context-specific. For instance, 2.9–7.5% of Ukrainian refugee children exposed to the recent war reported experiencing depression symptoms (Osokina et al., 2023) [8]. Furthermore, 42.6% of unaccompanied minors versus 30% of accompanied refugee children residing in Germany reported depression symptoms [28]. Depression rates were also high (27.9%) for refugee children living in a refugee camp [29]. Syrian refugee children presented with a lower than global rate prevalence of 12.5% [21]. For Syrian children, the number of traumatic events was the most robust predictor for depression, anxiety, and PSTD [28].
Depression and PTSD disorders present the most significant mental health differences between non-migrant and refugee children (Hodes, 2022) [22]. Iraqi refugee children living in a Turkish refugee camp reported a very high rate of 43.4% for PTSD [29]. This rate is similar to the 21% to 44.6% rate reported for children exposed to the ongoing Israeli–Palestinian conflict [30]. These rates could be similar because children from Iraq and Israel have been directly exposed to open war. Exposure to war trauma seems to increase the risk of developing adverse mental health; for example, Ukrainian children who had experienced and witnessed more violent events were more than four times more likely to develop PTSD [8]. Children living in open conflict zones also present with high levels of behavioural difficulties [31]. Bosnian refugee children who experienced a long-term separation from a parent, direct exposure to armed combat, or the death of a close friend or relative presented with a 77% rate of behavioural challenges [32]. It seems that exposure to war-related violence leads to behavioural–emotional problems [31]. Due to high exposure to violence, refugee children can act out through aggressive behaviours and thus have reduced interactions with peers [30,33].
Research shows that school psychologists provide trauma-informed therapy for refugee children [34,35,36]. This study suggests a culturally responsive approach to trauma-informed therapy for displaced children. Cultural responsiveness acknowledges the different ways that refugee children have suffered and prioritises indigenous health systems for addressing their mental health.
1.2. Framework: Culturally Responsive Therapy
CRT emphasises the importance of the client’s culture and socioecological location in health services. Culture is the foundation of one’s beliefs, norms, and values and determines attitudes and actions [37]. It influences children’s development, worldviews, and social participation [5]. In mental health, culture influences how families understand their mental health symptoms and directs their health-seeking behaviours [38]. In some cultures, mental health symptoms are experienced, interpreted, and described somatically [39] and as spiritual disturbances/attacks from evil spirits [40]. Clients from these cultures will seek help consistent with their belief systems. CRT offers school psychologists a framework that includes different ways of understanding mental health. CRT has similar intentions as culturally competent and sensitive models; sometimes, the terms responsiveness, competence, and sensitivity are used interchangeably [41]. These approaches challenge monocultural practices within mental health by acknowledging diversity in mental health ways and providing a therapeutic space for inclusive mental health practices. Furthermore, CRT therapists are proactive about acquiring cultural knowledge and transforming their practice [42]. CRT is not a therapy modality like Cognitive Behavioural Therapy (CBT), Emotionally Focused Therapy (EFT), or Solution-Focused Therapy (SFT). It is a therapy framework that prioritises the way culturally diverse clients conceptualise, diagnose, and treat their mental health. As a framework, it can be integrated into therapeutic modalities such as CBT, EFT, and SFT. For example, SFT focuses on the client’s capacities, resources, and assets rather than emphasising problem patterns [43]. A culturally responsive therapist using SFT will inquire about resources and capacities that are culturally important. Therapy techniques can also be made culturally relevant; for example, the miracle question or crystal ball technique from SFT can be posed culturally responsively. The rationale behind these techniques is to inspire the client to imagine and anticipate life without the problem, thereby inspiring hope for the future [44]. Knowing the rationale for these techniques, the therapist might think of a question that captures that motive and will resonate with the client’s worldview, belief systems, and cultural metaphors.
Across the mental health literature, CRT can be summed up in the following principles. These principles can be integrated into trauma-informed therapies when treating refugee schoolchildren:
- CRT requires cultural humility: It compels therapists to reflect on their cultural biases and practice cultural flexibility and humility. Cultural flexibility and humility are the attitudes that precede the practice of CRT. Cultural competence involves flexibility—an ability to understand the child or family’s experience from their frame of reference rather than from one’s own [45]. Cultural humility is the life-long commitment to personal reflexivity and the self-critique of one’s culture and enables medical service providers to develop non-authoritarian relationships with their clients [46]. Culturally responsive school psychology has an ethos of cultural reflexivity where cultural flexibility and humility are practised.
- CRT is radical: It challenges dominant and exclusive knowledge systems and highlights the importance of indigenous ways of being [38]. Therefore, CRT is inclusive and can potentially revolutionise school psychology to benefit diverse learners.
- CRT gives prominence to indigenous cultures: Responsive therapists are lifelong learners who commit to learning about their client’s cultures (author, 2020) [47] and seek proactive opportunities to acquire cultural knowledge (Parekh et al., 2014) [42]. They are also mindful of within-group variations and honour how each family culturally identifies [47]. They can locate family indigenous cultural norms, customs, and practices by asking. School psychologists honouring indigenous knowledge can maximise cultural healing practices that are natural to refugee learners.
- CRT is accountable to the needs of stakeholders [41]. Meeting the needs of families as they state them creates an atmosphere of accountability that benefits refugee families [42]. A responsive therapist is accountable because they put their cultural knowledge into practice. As previously stated, migrant children are underrepresented in mental health services [17], and for many refugee children, consultation with a mental health practitioner may be a novel experience; accountability can increase trust and respect in the therapeutic relationship. Rapport, respect, and mutual understanding may increase therapy interest and retention among refugee families.
- CRT is collaborative [47]: Refugee families often present with urgent physical and economic needs that cause them emotional distress. While assisting refugees in acquiring material and financial resources may not be within the scope of practice for psychologists, therapists should not ignore or disregard learners’ material and economic needs. Continuing with psychotherapy with learners who do not have their basic needs met is possibly counterproductive. School psychologists can collaborate with refugee agencies that provide material and financial services to refugee families to assist learners in getting their basic needs fulfilled. Thus, therapists need to establish a strong network of collaboration with agencies that provide various services to refugee families [47].
2. Materials and Methods
2.1. Research Design
A Qualitative Conventional Content Analysis (QCCA) by Hsieh and Shannon (2005) underpinned this study. QCCA is designed to analyse content such as texts, transcripts, videos, and images [48,49] and was used in this study to analyse video materials and transcripts.
2.2. Data Collection
2.2.1. Sample
This study included archived videos on the issue of refugee mental health (N = 5). Two documentaries and three instructional videos were included for analysis. Archival data were used due to the availability of these data compared to data on refugee participants in North America, where the researcher was based at the time of data collection. Table 1 provides details of the final five videos analysed.

Table 1.
Videos Included for Analysis.
2.2.2. Inclusion Criteria
Video documentaries are films that tell the stories of people’s lived experiences, social concerns, and political phenomena [55] and were used in this study to explore the experiences of war, mental health and psychological therapy of refugee children. Documentaries included in this research study featured stories of the following:
- Refugee children who had experienced open war and were displaced as a result of violent conflict.
- Refugee children participating in family or individual trauma-informed psychological therapy.
Instructional videos were selected for use in this study because vignette case studies can connect research with practice [56]. The instructional videos included showcased the following:
- Psychologists and therapists providing family therapy to refugee children.
- Expert discussions on refugee children’s experiences of pre-migration, migration, and post-migration traumatic stressors.
2.2.3. Search Criteria
Videos were identified in academic and professional organisations’ libraries, archives, and databases. The final videos were sourced from the American Psychological Association (APA) video database, the University of Georgia library systems, and the VoicesAcademy professional online continuing education platform. Internet video platforms, such as YouTube and Vimeo, were also searched. However, videos from these platforms were excluded from the final analysis as they did not meet the inclusion criteria.
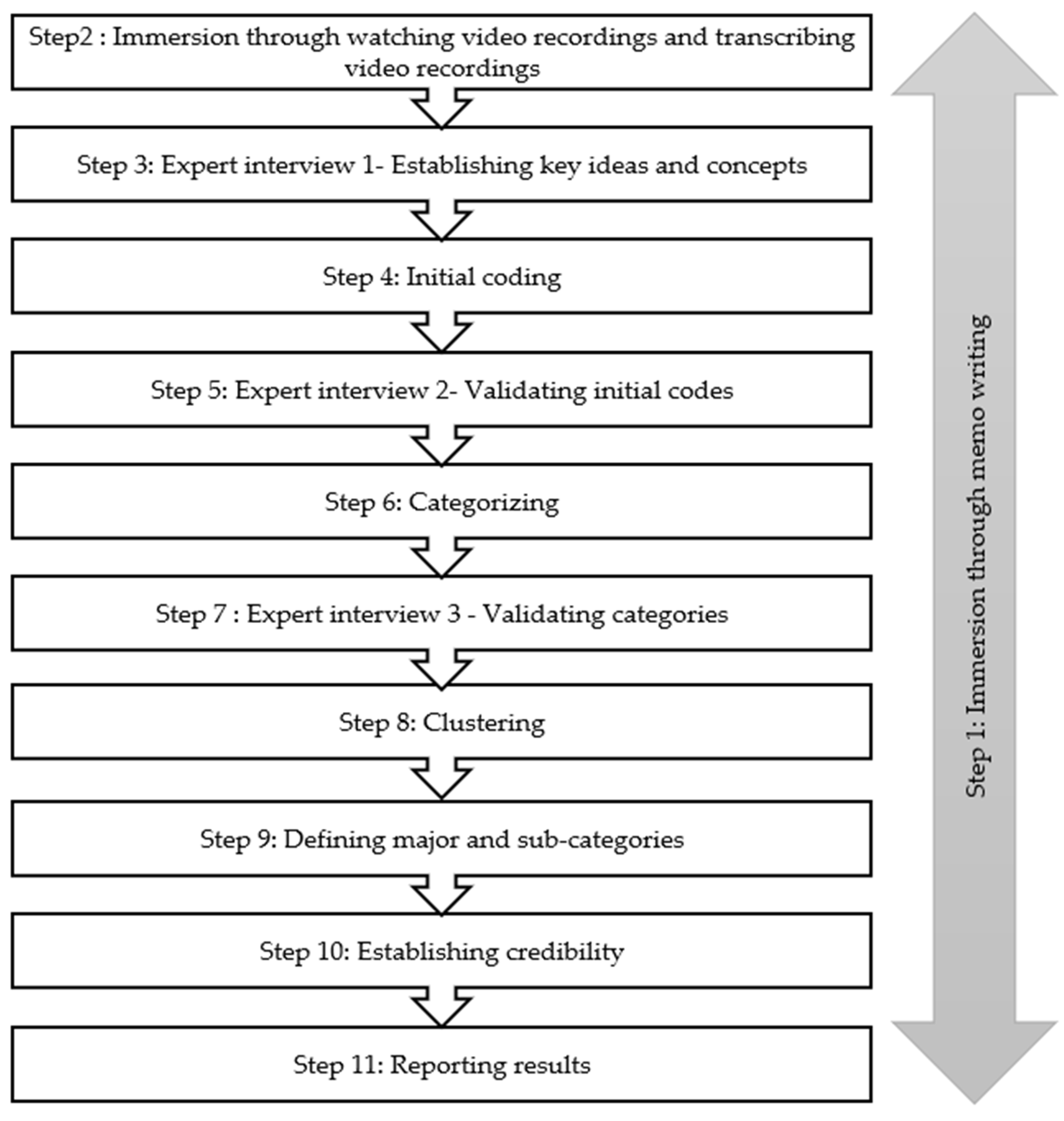
2.3. Data Analysis
In QCCA, data analysis is conducted in the following steps: immersion, initial coding, categorising, clustering, defining categories, reporting the findings, and memo writing [57]. In this study, four additional steps were added to enhance the validity of the findings. Three experts were consulted, one after each step in the analysis, to provide clarity and validation for the emergent codes, and three senior researchers assessed the data audit trail for credibility. The analysis procedure is duplicated in Figure 1.
Figure 1.
Data analysis procedure.
Analysis Procedure
- Immersion through memos. The researcher used memos to conceptualise and theoretically link emerging themes.
- Immersion through watching and transcribing video recordings. The researcher watched the video materials several times to become familiar with the data and then transcribed the video materials into written documents.
- Expert interview 1—Establishing key ideas and concepts. This expert was considered an extension of the literature on psychotherapy with refugee families because the literature on this topic is lacking, and they assisted the researcher in defining key ideas and concepts.
- Initial coding. Initial coding was conducted through word-by-word and line-by-line coding.
- Expert interview 2—Validating initial codes. The second expert validated the emerging initial codes.
- Categorising. Initial codes were compared to each other and then conceptually organised into categories.
- Expert interview 3—Validating categories. The third expert validated emerging categories.
- Clustering. Major and sub-categories were organised into meaningful units to create conceptual clusters.
- Defining major and sub-categories. The definitions of the categories were constructed as an ongoing process from initial coding to clustering. In this step, emerging definitions were solidified.
- Establishing credibility. Three senior researchers ensured the study’s credibility by analysing the audit trail.
- Reporting results. Findings are reported in major categories. Exemplar quotations from the transcripts are given to substantiate the reported categories.
2.4. Ethical Considerations
Due to the use of publicly available data, this research study is exempt from institutional ethical permission. Nevertheless, research using publicly available data should be carried out with beneficence, respect, and justice [58].
3. Results
Three major categories relating to children’s experiences of war trauma are reported [47]: (1) children are not spared from war trauma, (2) children live in perpetual fear and anxiety, and (3) war-related violence ignites aggressive behaviours in children.
- Theme 1: Children are not spared from war trauma.
Children are not spared from war trauma, which means that exposure to violent events has no age limit. The children in this study experienced personal physical and psychological harm, the murder of family members, and massacres of their community members. The perpetrators did not consider them too young for brutality, and they were attacked as viciously as adults [47]. The psychologists in this study reported that memories of war horrors and psychological trauma can stay with child survivors into adulthood. Jacques was five years old when his family was attacked, and as an 18-year-old, he has not forgotten his experiences and vividly remembers the war events.
I was terrified. I didn’t know what was happening. I saw everyone running, and I had no idea why. Everyone was screaming. When war broke out in my region, we were taken to a stadium, it was a soccer stadium. I stayed there for about four days. There were so many people and lots of disease and massacring. Then things went bad to the very worst. The weather was awful. It was raining, and blood flowed everywhere. We were swimming in blood; there were so many wounded. That has stayed with me; it won’t go away…. At five, I had no idea what a massacre was. (Ampersand Film & Video Tape Productions, 2005, 00:10:53)
Some children have never known peace. They have faced violence since birth. They move from one refugee camp to another until they arrive in Canada. For these children, the conflict remains within, and it’s still active. (Multimedia Group of Canada, 2000, 00:02:17)
Children such as Jaques, who lost family members during forced migration, have the additional traumatic stress of being unaccompanied minors. Possibly due to the loss or separation of/from family members, unaccompanied minors report higher rates of anxiety and depression when compared to children who have immigrated with a family relative [28]. While resettlement is conflict-free, poor mental health does not quickly improve upon relocation to the host country. Dr. Chan put it this way:
Often, we have this myth or belief that now that they are in the U.S., life is fine. It’s just everyday challenges, but some of the things we have to remember are, first, how the pre-migration experiences impact the post-migration. (American Psychological Association, 2009, 00:00:22.11)
The children in this study lived in fear and anxiety during pre- and post-migration. School psychologists should pay close attention to unaccompanied minors who have family members left behind in countries in open war. Such children may be living in constant worry and may, at any point, actually lose family members to the war.
- Theme 2: Children live in perpetual fear and anxiety.
Refugee children reported constant fear for their lives and the lives of their loved ones. This fear arose from actual experiences of tragedy, including the death of loved ones during the war and being personally shot by soldiers.
Soldiers scare me when they shoot. When they shoot real bullets, I am scared one of the bullets might hit my brothers or sisters. (Ampersand Film & Video Tape Productions, 00:16:03)
This child had recently experienced her older cousin’s death in that war. Brutal killings of family members are not uncommon during wartime [8,9]. Siblings often live in anxiety and worry about older siblings who may be participating (as soldiers) in the war. These anxieties can be expressed in different ways, for example:
She wakes up in the middle of the night crying. She has nightmares about tanks crushing us. They will raze the house while we’re asleep, crushing us, and no one will know. (Ampersand Film & Video Tape Productions, 2005, 00:06.25)
Devastatingly, shortly after the recording of the documentary, soldiers came into the child’s village and indeed razed her home to the ground. Refugee children live in a world where their worst nightmares can quickly become a reality. A 21-year-old young man who soldiers shot woke up from a four-month-long coma and had to return to the same village, where the open conflict continued. Living amidst an open war can inspire constant anxiety and worry and prolong psychological trauma from the experienced violence.
Ahmed is 21. He lives with his family in Rafah. A year ago, during an incursion by the Israeli army, he was hit in the chest by two bullets fired from a tank turret. He was plunged into a four-month coma but eventually awoke and survived. (Ampersand Film & Video Tape Productions, 2005, 00.02.55)
Anxiety and worry often persist post-relocation. The psychologists in this study report that anxiety and trauma reactions can be triggered in resettlement. This means that school psychologists should not assume children live fear-free lives because they are out of immediate danger. Fear- and trauma-related symptoms can manifest at a later stage of life.
Among children, post-traumatic stress disorders generally manifest themselves as anxiety attacks, difficulty concentrating, loss of interest in everyday activities, trouble in school, fatigue, insomnia, nightmares, and aggression. Such symptoms can appear months or years after the trauma, the memory of which is triggered by a simple sensory event. (Multimedia Group of Canada, 2000, 00:24:42)
- Theme 3: War-related violence ignites aggressive behaviours in children.
This study demonstrates that refugee children can display behavioural and social challenges. Significantly, aggressive behaviours are triggered by traumatic stimuli or are a result of learned behaviours from prolonged experiences of violence. These findings are congruent with the literature reports that indicate a link between experiences of war brutality and behavioural difficulties [31]. Child psychologists shared their insights from providing psychotherapy to refugee children.
In war situations, violence is constantly reactivated by events, of course. This is particularly important in children. How do they grow up in violence without that violence becoming an integral part of them? (Ampersand Film & Video Tape Productions, 2005, 00:30:24)
All the anger and sadness they were exposed to ends up manifesting itself as destructiveness. The anger they carry inside must not become self-destructive or destructive to others through anti-social behaviour. (Multimedia Group of Canada, 2000, 00:25:56)
These psychologists highlight that exposure to violence can lead to deep-seated psychological traumatic responses such as anger and sadness, and these emotions can ignite aggressive behaviours. Violent behaviours can also be due to a lack of social skills to resolve conflict with peers appropriately. One psychologist reported that war conflict leads to a breakdown in human relationships because it involves human-on-human violence. Thus, it breaks the trust in humanity and increases the fear of other human beings in children.
The most damaging traumas are those arising from human violence. The psychological repercussions are always more significant in such cases. The capacity to trust others is deeply affected. (Multimedia Group of Canada, 2000, 00:11:33)
While exposure to war violence can trigger anxiety and socially violent behaviours, refugee children should not be viewed as inherently violent. School psychologists should assist the school community in interpreting these behaviours for what they are: the residue of having experienced extreme violence and cruelty.
4. Discussion
This study shows that refugee children experience as much violence as refugee adults. Traumatic stressors experienced during forced migration lead to mental health disorders. The children in this study presented with psychological trauma, fear, anxiety, and aggressive behaviours. This is consistent with literature reports of a high prevalence of anxiety, depression, and PTSD among refugee children [27,28]. This study shows that refugee children have a hard time socially adjusting and concurs with [31] that aggressive behaviours should be interpreted as a traumatic response to exposure to life-threatening violence.
Various psychotherapy models are effectively used to treat refugee trauma; for example, see [35,59]. This study recommends the integration of CRT into the trauma-informed treatment models for services offered to refugee children. CRT is based on ideas of multiculturism, which is complementary to social justice [60]. CRT, multiculturism, and social justice all propose that therapy has an ethical obligation to acknowledge cultural diversity and to treat clients in a culturally attuned manner that resonates with their indigenous healing views and practices.
4.1. Considerations for Culturally Responsive School Psychology
In a strange and unfamiliar country, a culturally responsive approach may be necessary, as it places the learner’s culture and sense of being at the centre of their healing process. Table 2 provides suggestions for how CRT can be incorporated into psychotherapy.

Table 2.
Culturally responsive considerations for refugee mental health.
The practice of CRT requires cultural humility. Therapists who do not give preference to their own cultures are open to practising radical school psychology. Refugee children can quickly acculturate to the culture of their host country and may seem to have assimilated into the host country’s culture. However, school psychologists should ensure these children understand the host country’s cultural nuances. The best practice would be to remain culturally sensitive, even to children who seem to have acculturated.
4.2. Study limitations
It can be challenging to recruit refugee minors for research participation. Where there is access to informed consent and assent, research can be limited by challenges such as language barriers and a lack of language translators and cultural brokers. Thus, this research study relied on publicly available data to address the research question. The limitation of using secondary data is that there was no way for the researcher to interact directly with the participants in the videos and, where necessary, engage in follow-up questions and make full-view observations of non-verbal communications. To mitigate this limitation, the researcher engaged with experts in refugee mental health to triangulate emerging themes in refugee mental health.
5. Conclusions
This study showed that refugee children suffer enormous amounts of psychological trauma during war displacement and, as a result, suffer poor mental health, including psychological trauma, fear, anxiety, and aggressive behaviours. Therapists have an ethical and moral obligation to ensure that psychotherapy is aligned with the values of inclusive education and social justice. This study recommends CRT as a therapeutic framework that is aligned with the values of inclusive education and social justice and prioritises diverse ways of understanding and treating children’s mental health.
Funding
This research received no external funding.
Informed Consent Statement
Patient consent was waived as the data employed in this study are publicly available data.
Data Availability Statement
Data references stated in Table 1, this may be removed.
Acknowledgments
This manuscript emerged from the author’s PhD dissertation research. The author wishes to acknowledge the support of the dissertation committee: Jerry Gale, Jennifer Gonyea, and Elizabeth Wieling.
Conflicts of Interest
The author declares no conflicts of interest.
References
- United Nations High Council for Refugees (UNHCR). Global Appeal Report 2021. 2021. Available online: https://reporting.unhcr.org/globalreport2021 (accessed on 26 December 2023).
- United Nations High Council for Refugees (UNHCR). Global Trends Forced Displacement in 2022. 2022. Available online: https://www.unhcr.org/global-trends-report-2022 (accessed on 26 December 2023).
- United Nations Children’s Fund (UNICEF). Child Displacement and Refugees. 2022. Available online: https://data.unicef.org/topic/child-migration-and-displacement/displacement/ (accessed on 31 December 2023).
- Walker, A. Transformative Potential of Culturally Responsive Teaching: Examining Preservice Teachers’ Collaboration Practices Centering Refugee Youth. Educ. Sci. 2023, 13, 621. [Google Scholar] [CrossRef]
- Castro-Olivo, S.M. Introduction to Special Issue: Culturally Responsive School-Based Mental Health Interventions. Contemp. Sch. Psychol. 2017, 21, 177–180. [Google Scholar] [CrossRef]
- Kirmayer, L.J.; Narasiah, L.; Munoz, M.; Rashid, M.; Ryder, A.G.; Guzder, J.; Hassan, G.; Rousseau, C.; Pottie, K. Common Mental Health Problems in Immigrants and Refugees: General Approach in Primary Care. Can. Med. Assoc. J. 2011, 183, E959–E967. [Google Scholar] [CrossRef]
- Human Rights Watch. World Report 2019: Events of 2018. 2019. Available online: https://www.hrw.org/world-report/2019 (accessed on 31 December 2023).
- Osokina, O.; Silwal, S.; Bohdanova, T.; Hodes, M.; Sourander, A.; Skokauskas, N. Impact of the Russian Invasion on Mental Health Of Adolescents in Ukraine. J. Am. Acad. Child Adolesc. Psychiatry 2023, 62, 335–343. [Google Scholar] [CrossRef] [PubMed]
- Rizkalla, N.; Mallat, N.K.; Arafa, R.; Adi, S.; Soudi, L.; Segal, S.P. “Children are not Children Anymore; They are a Lost Generation”: Adverse Physical and Mental Health Consequences on Syrian Refugee Children. Int. J. Environ. Res. 2020, 17, 8378. [Google Scholar] [CrossRef] [PubMed]
- Bemak, F.; Chung, R.C.Y. Refugee Trauma: Culturally Responsive Counseling Interventions. J. Couns. Dev. 2017, 95, 299–308. [Google Scholar] [CrossRef]
- Vossoughi, N.; Jackson, Y.; Gusler, S.; Stone, K. Mental Health Outcomes for Youth Living in Refugee Camps: A Review. Trauma Violence Abus. 2018, 19, 528–542. [Google Scholar] [CrossRef]
- Gleeson, C.; Frost, R.; Sherwood, L.; Shevlin, M.; Hyland, P.; Halpin, R.; Murphy, J.; Silove, D. Post-Migration Factors and Mental Health Outcomes in Asylum-Seeking and Refugee Populations: A Systematic Review. Eur. J. Psychotraumatol. 2020, 11, 1793567. [Google Scholar] [CrossRef]
- Joyce, L.; Liamputtong, P. Acculturation Stress and Social Support for Young Refugees in Regional Areas. Child. Youth Serv. Rev. 2017, 77, 18–26. [Google Scholar] [CrossRef]
- Beiser, M.; Hou, F. Predictors of Positive Mental Health Among Refugees: Results from Canada’s General Social Survey. Transcult. Psychiatry 2017, 54, 675–695. [Google Scholar] [CrossRef]
- Fazel, M.; Reed, V.R.; Panther-Brick, C.; Stein, A. Mental Health of Displaced and Refugee Children Resettled in High-Income Countries: Risk and Protective Factors. Lancet 2012, 379, 266–282. [Google Scholar] [CrossRef] [PubMed]
- Grasser, L.R. Addressing Mental Health Concerns in Refugees and Displaced Populations: Is Enough Being Done? Risk Manag. Healthc. Policy 2022, 15, 909–922. [Google Scholar] [CrossRef] [PubMed]
- Gubi, E.; Sjöqvist, H.; Viksten-Assel, K.; Bäärnhielm, S.; Dalman, C.; Hollander, A.-C. Mental health service use among migrant and Swedish-born children and youth: A register-based cohort study of 472,129 individuals in Stockholm. Soc. Psychiatry Psychiatr. Epidemiol. 2022, 57, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Filler, T.; Georgiades, K.; Khanlou, N.; Wahoush, O. Understanding Mental Health and Identity from Syrian Refugee Adolescents’ Perspectives. Int. J. Ment. Health Addict. 2021, 19, 764–777. [Google Scholar] [CrossRef]
- Taylor, J.; Haintz, G.L. Influence of the Social Determinants of Health on Access to Healthcare Services among Refugees in Australia. Aust. J. Prim. Health 2018, 24, 14–28. [Google Scholar] [CrossRef] [PubMed]
- McCleary, J.S. The Impact of Resettlement on Karen Refugee Family Relationships: A Qualitative Exploration. Child Fam. Soc. Work 2017, 22, 1464–1471. [Google Scholar] [CrossRef]
- Scherer, N.; Hameed, S.; Acarturk, C.; Deniz, G.; Sheikhani, A.; Volkan, S.; Örücü, A.; Pivato, I.; Akıncı, İ.; Patterson, A.; et al. Prevalence of Common Mental Disorders Among Syrian Refugee Children and Adolescents in Sultanbeyli District, Istanbul: Results of a Population-Based Survey. Epidemiol. Psychiatr. Sci. 2020, 29, e192. [Google Scholar] [CrossRef]
- Hodes, M. Editorial Perspective: Mental Health of Young Asylum Seekers and Refugees in the Context of COVID-19. Child Adolesc. Ment. Health 2022, 27, 190–191. [Google Scholar] [CrossRef]
- Kauhanen, L.; Wan Mohd Yunus, W.M.A.; Lempinen, L.; Peltonen, K.; Gyllenberg, D.; Mishina, K.; Gilbert, S.; Bastola, K.; Brown, J.S.; Sourander, A. A Systematic Review of the Mental Health Changes of Children and Young People Before and During the COVID-19 Pandemic. Eur. Child Adolesc. Psychiatry 2023, 32, 995–1013. [Google Scholar] [CrossRef]
- Chen, X.; Qi, H.; Liu, R.; Feng, Y.; Li, W.; Xiang, M.; Cheung, T.; Jackson, T.; Wang, G.; Xiang, Y.T. Depression, Anxiety and Associated Factors Among Chinese Adolescents During The COVID-19 Outbreak: A Comparison of Two Cross-Sectional Studies. Transl. Psychiatry 2021, 11, 148. [Google Scholar] [CrossRef]
- Ravens-Sieberer, U.; Kaman, A.; Erhart, M.; Devine, J.; Schlack, R.; Otto, C. Impact of the COVID-19 Pandemic on Quality of Life and Mental Health in Children and Adolescents in Germany. Eur. Child Adolesc. Psychiatry 2021, 31, 879–889. [Google Scholar] [CrossRef]
- Niedzwiedz, C.L.; Green, M.J.; Benzeval, M.; Campbell, D.; Craig, P.; Demou, E.; Leyland, A.; Pearce, A.; Thomson, R.; Whitley, E.; et al. Mental Health and Health Behaviours Before and During the Initial Phase of the COVID-19 Lockdown: Longitudinal Analyses of the UK Household Longitudinal Study. J. Epidemiol. Community Health 2021, 75, 224–231. [Google Scholar] [CrossRef] [PubMed]
- Blackmore, R.; Gray, K.M.; Boyle, J.A.; Fazel, M.; Ranasinha, S.; Fitzgerald, G.; Misso, M.; Gibson-Helm, M. Systematic Review, and Meta-Analysis: The Prevalence of Mental Illness in Child and Adolescent Refugees and Asylum Seekers. J. Am. Acad. Child Adolesc. Psychiatry 2020, 59, 705–714. [Google Scholar] [CrossRef] [PubMed]
- Müller, L.R.F.; Büter, K.P.; Rosner, R.; Unterhitzenberger, J. Mental Health and Associated Stress Factors in Accompanied and Unaccompanied Refugee Minors Resettled in Germany: A Cross-Sectional Study. Child Adolesc. Psychiatry Ment. Health 2019, 13, 8. [Google Scholar] [CrossRef] [PubMed]
- Nasıroğlu, S.; Çeri, V.; Erkorkmaz, Ü.; Semerci, B. Determinants of Psychiatric Disorders in Children Refugees in Turkey’s Yazidi Refugee Camp. Psychiatry Clin. Psychopharmacol. 2018, 28, 291–299. [Google Scholar] [CrossRef]
- Slone, M.; Mann, S. Effects of War, Terrorism and Armed Conflict on Young Children: A Systematic Review. Child Psychiatry Hum. Dev. 2016, 47, 950–965. [Google Scholar] [CrossRef] [PubMed]
- Jayuphan, J.; Sangthong, R.; Hayeevani, N.; Assanangkornchai, S.; McNeil, E. Mental Health Problems from Direct Vs Indirect Exposure to Violent Events Among Children Born and Growing Up in a Conflict Zone of Southern Thailand. Soc. Psychiatry Psychiatr. Epidemiol. 2020, 55, 57–62. [Google Scholar] [CrossRef] [PubMed]
- Geltman, P.L.; Augustyn, M.; Barnett, E.D.; Klass, P.E.; Groves, B.M. War Trauma Experience and Behavioral Screening of Bosnian Refugee Children Resettled in Massachusetts. J. Dev. Behav. Pediatr. 2002, 21, 255–261. [Google Scholar] [CrossRef] [PubMed]
- Hart, R. Child Refugees, Trauma and Education: Interactionist Considerations on Social and Emotional Needs and Development. Educ. Psychol. Pract. 2009, 25, 351–368. [Google Scholar] [CrossRef]
- Cowling, M.M.; Anderson, J.R. The Effectiveness of Therapeutic Interventions on Psychological Distress in Refugee Children: A Systematic Review. J. Clin. Psychol. 2023, 79, 1857–1874. [Google Scholar] [CrossRef]
- Chipalo, E. Is Trauma Focused-Cognitive Behavioral Therapy (TF-CBT) Effective in Reducing Trauma Symptoms among Traumatized Refugee Children? A Systematic Review. J. Child Adolesc. Trauma 2021, 14, 545–558. [Google Scholar] [CrossRef]
- Lawton, K.; Spencer, A. A Full Systematic Review on the Effects of Cognitive Behavioural Therapy for Mental Health Symptoms in Child Refugees. J. Immigr. Minor. Health 2021, 23, 624–639. [Google Scholar] [CrossRef]
- Lawless, J.J.; Gale, J.E.; Bacigalupe, G. The Discourse of Race and Culture in Family Therapy Supervision: A Conversation Analysis. Contemp. Fam. Ther. 2001, 23, 181–197. [Google Scholar] [CrossRef]
- Ancis, J.R. Culturally Responsive Practice. In Culturally Responsive Interventions: Innovative Approaches to Working with Diverse Populations; Ancis, J.R., Ed.; Brunner-Routledge: New York, NY, USA, 2004; pp. 2–20. [Google Scholar]
- Hinton, D.E.; Kredlow, M.A.; Bui, E.; Pollack, M.H.; Hofmann, S.G. Treatment Change of Somatic Symptoms and Cultural Syndromes Among Cambodian Refugees with PTSD. Depress. Anxiety 2012, 29, 148–155. [Google Scholar] [CrossRef]
- Byrow, Y.; Pajak, R.; Specker, P.; Nickerson, A. Perceptions of mental health and perceived barriers to mental health help-seeking amongst refugees: A systematic review. Clin. Psychol. Rev. 2020, 75, 101812. [Google Scholar] [CrossRef] [PubMed]
- Seponski, D.M.; Lewis, D.C.; Megginson, M.C. A Responsive Evaluation of Mental Health Treatment in Cambodia: Intentionally Addressing Poverty to Increase Cultural Responsiveness in Therapy. Glob. Public Health 2014, 9, 1211–1224. [Google Scholar] [CrossRef] [PubMed]
- Ellis, H.B.; Murray, K.; Barrett, C. Understanding the Mental Health of Refugees: Trauma, Stress, and the Cultural Context. In The Massachusetts General Hospital Textbook on Diversity and Cultural Sensitivity in Mental Health; Parekh, R., Ed.; Human Press: Boston, MA, USA, 2014; pp. 165–187. [Google Scholar]
- Molnar, A.; De Shazer, S. Solution-focused Therapy: Toward the Identification of Therapeutic Tasks. J. Marital Fam. Ther. 1987, 13, 349–358. [Google Scholar] [CrossRef]
- De Shazer, S. Clues: Investigating Solutions in Brief Therapy; W.W. Norton: New York, NY, USA, 1988. [Google Scholar]
- Clauss-Ehlers, C.S.; Serpell, Z.N.; Weist, M.D. Introduction: Making the Case for Culturally Responsive School Mental Health. In Handbook of Culturally Responsive School Mental Health: Advancing Research, Training, Practice, and Policy; Clauss-Ehlers, C.S., Serpell, Z.N., Weist, M.D., Eds.; Springer: New York, NY, USA, 2013; pp. 135–145. [Google Scholar]
- Tervalon, M.; Murray-Garcia, J. Cultural Humility Versus Cultural Competence: A Critical Distinction in Defining Physician Training Outcomes in Multicultural Education. J. Health Care Poor Underserved 1998, 9, 117–125. [Google Scholar] [CrossRef]
- Somo, C.M. Trauma-Informed Family Therapy: Considerations for The Systemic Treatment of Trauma in Refugee Communities. Ph.D. Dissertation, University of Georgia, Athens, GA, USA.
- Roller, M.R. A Quality Approach to Qualitative Content Analysis: Similarities and Differences Compared to Other Qualitative Methods. Forum Qual. Soc. Res. 2019, 20, 31. [Google Scholar]
- Zhang, Y.; Widermuth, B.M. Qualitative Analysis of Content. In Applications of Social Research Methods to Questions in Information and Library Science, 2nd ed.; Wildermuth, B.M., Ed.; Libraries Unlimited: Santa Barbara, CA, USA, 2009; pp. 159–176. [Google Scholar]
- Ampersand Film and Video Tape Productions. After the Outrage: Violence, Trauma, and Recovery, Ampersand Film & Video Tape Productions & Films Media Group: Quebec, QC, Canada, 2005; ISBN 978-1-62290-222-4.
- Multimedia Group of Canada. Post-Traumatic Stress Disorder: When the Memories Won’t Go Away; Multimedia Group of Canada: Montréal, QC, Canada, 2000; ISBN 978142137145-0. [Google Scholar]
- American Psychological Association. Series V-Multicultural Counseling: Working with Immigrants; APA Videos: Washington, DC, USA, 2008; ISBN 978-1-4338-0369-7. [Google Scholar]
- Ochberg, F.; Panos, A. Living with PTSD: Lessons for Partners, Friends and Supporters; Psychotherapy.net/videos: Radnor, PA, USA, 2012; ISBN 1-60124-300-6. [Google Scholar]
- VoicesAcademy. Interpreting for Refugees in Social Service Encounters. 2014. Available online: https://voicesacademy.com/interpreting-for-refugees-in-social-service-encounters/ (accessed on 16 December 2023).
- Slutskaya, N.; Game, A.M.; Simpson, R.C. Better Together: Examining the Role of Collaborative Ethnographic Documentary in Organizational Research. Organ. Res. Methods 2018, 21, 341–365. [Google Scholar] [CrossRef]
- Skilling, K.; Stylianides, G.J. Using Vignettes in Educational Research: A Framework for Vignette Construction. Int. J. Res. Method. Educ. 2020, 43, 541–556. [Google Scholar] [CrossRef]
- Hsieh, H.F.; Shannon, S.E. Three Approaches to Qualitative Content Analysis. Qual. Health Res. 2005, 15, 1277–1288. [Google Scholar] [CrossRef]
- Williams, S.G. The Ethics of Internet Research. Online J. Nurs. Inform. 2012, 16, 1277–1288. [Google Scholar]
- Morina, N.; Nickerson, A. (Eds.) Mental Health of Refugee and Conflict-Affected Populations: Theory, Research and Clinical Practice; Springer: Cham, Switzerland, 2018. [Google Scholar]
- Ratts, M.J. Multiculturalism, and Social Justice: Two Sides of the Same Coin. J. Multicult. Couns. Dev. 2011, 39, 24–37. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).