Passive Solid Chemosensor as Saliva Point of Need Analysis for Ammonium Determination by Using a Smartphone
Abstract
1. Introduction
2. Materials and Methods
2.1. Reagents and Solutions
2.2. Apparatus
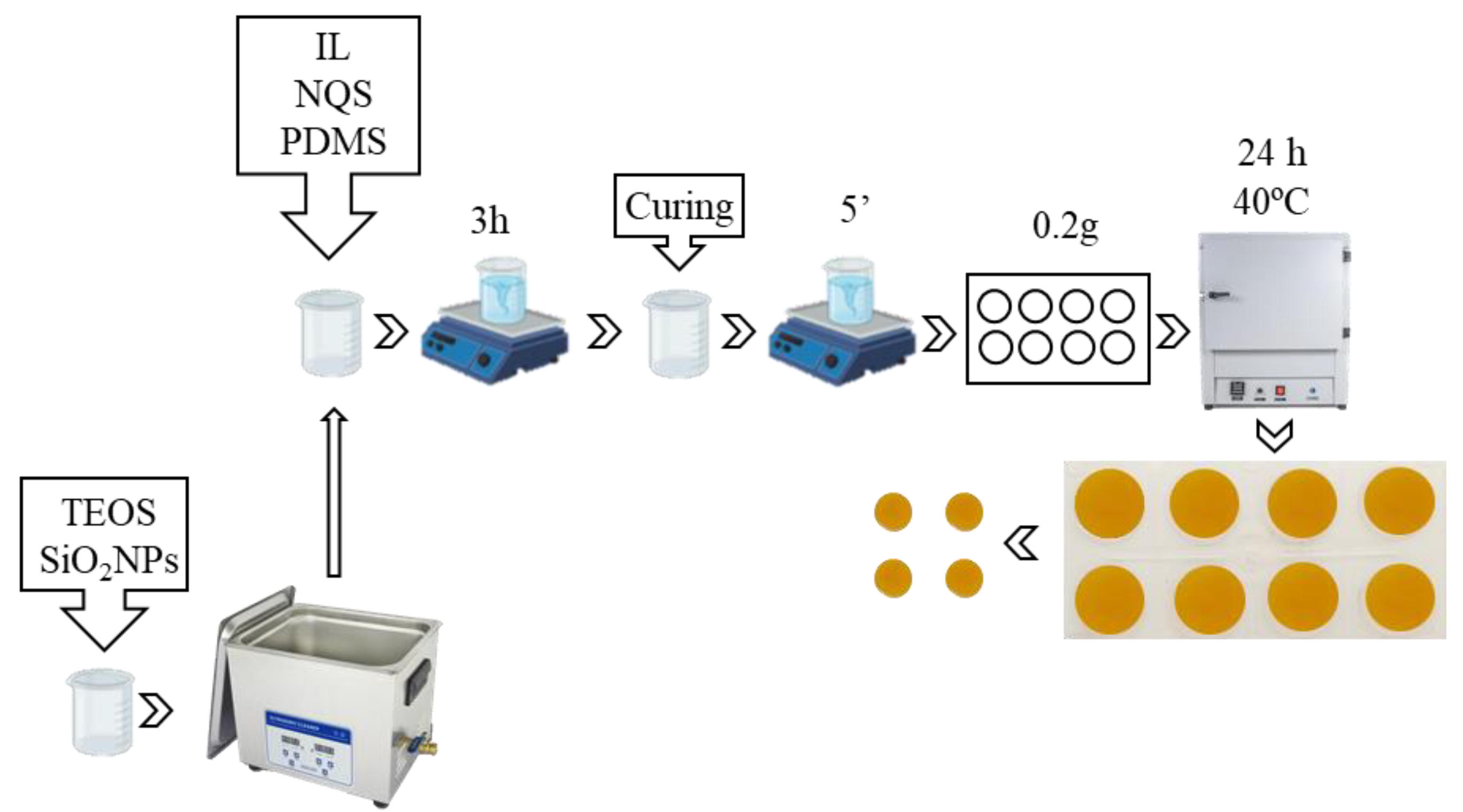
2.3. Preparation of the PDMS/TEOS-SiO2NPs-OMIM PF6-NQS Sensing Membranes
2.4. Procedure for Ammonia Determination
2.5. Application to Saliva Samples
3. Results and Discussion
3.1. Study of the Influence of Salivary pH
3.2. Analytical Parameters of Ammonium Determination
3.3. Application to Real Samples
4. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Adlimoghaddam, A.; Sabbir, M.G.; Albensi, B.C. Ammonia as a Potential Neurotoxic Factor in Alzheimer’s Disease. Front. Mol. Neurosci. 2016, 9, 57. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.; Metsälä, M.; Vaittinen, O.; Halonen, L. The Origin of Mouth-Exhaled Ammonia. J. Breath Res. 2014, 8, 036003. [Google Scholar] [CrossRef] [PubMed]
- Thepchuay, Y.; Costa, C.F.A.; Mesquita, R.B.R.; Sampaio-Maia, B.; Nacapricha, D.; Rangel, A.O. Flow-Based Method for the Determination of Biomarkers Urea and Ammoniacal Nitrogen in Saliva. Bioanalysis 2020, 12, 455–465. [Google Scholar] [CrossRef] [PubMed]
- Suresh, G.; Ravi Kiran, A.; Samata, Y.; Purnachandrarao Naik, N.; Vijay Kumar, A. Analysis of Blood and Salivary Urea Levels in Patients Undergoing Haemodialysis and Kidney Transplant. J. Clin. Diagn. Res. 2014, 8, 18–20. [Google Scholar] [CrossRef]
- Chen, C.C.; Hsieh, J.C.; Chao, C.H.; Yang, W.S.; Cheng, H.T.; Chan, C.K.; Lu, C.J.; Meng, H.F.; Zan, H.W. Correlation between Breath Ammonia and Blood Urea Nitrogen Levels in Chronic Kidney Disease and Dialysis Patients. J. Breath Res. 2020, 14, 036002. [Google Scholar] [CrossRef]
- Limeres, J.; Garcez, J.F.; Marinho, J.S.; Loureiro, A.; Diniz, M.; Diz, P. A Breath Ammonia Analyser for Monitoring Patients with End-Stage Renal Disease on Haemodialysis. Br. J. Biomed. Sci. 2017, 74, 24–29. [Google Scholar] [CrossRef]
- Bevc, S.; Mohorko, E.; Kolar, M.; Brglez, P.; Holobar, A.; Kniepeiss, D.; Podbregar, M.; Piko, N.; Hojs, N.; Knehtl, M.; et al. Measurement of Breath Ammonia for Detection of Patients with Chronic Kidney Disease. Clin. Nephrol. 2017, 88, S14–S17. [Google Scholar] [CrossRef]
- Chuang, M.Y.; Chen, C.C.; Zan, H.W.; Meng, H.F.; Lu, C.J. Organic Gas Sensor with an Improved Lifetime for Detecting Breath Ammonia in Hemodialysis Patients. ACS Sens. 2017, 2, 1788–1795. [Google Scholar] [CrossRef]
- Bayrakli, I.; Turkmen, A.; Akman, H.; Sezer, M.T.; Kutluhan, S. Applications of External Cavity Diode Laser-Based Technique to Noninvasive Clinical Diagnosis Using Expired Breath Ammonia Analysis: Chronic Kidney Disease, Epilepsy. J. Biomed. Opt. 2016, 21, 087004. [Google Scholar] [CrossRef]
- Thepchuay, Y.; Mesquita, R.B.R.; Nacapricha, D.; Rangel, A.O.S.S. Micro-PAD Card for Measuring Total Ammonia Nitrogen in Saliva. Anal. Bioanal. Chem. 2020, 412, 3167–3176. [Google Scholar] [CrossRef]
- Zilberman, Y.; Sonkusale, S.R. Microfluidic Optoelectronic Sensor for Salivary Diagnostics of Stomach Cancer. Biosens. Bioelectron. 2015, 67, 465–471. [Google Scholar] [CrossRef] [PubMed]
- Lasisi, T.J.; Raji, Y.R.; Salako, B.L. Salivary Creatinine and Urea Analysis in Patients with Chronic Kidney Disease: A Case Control Study. BMC Nephrol. 2016, 17, 10. [Google Scholar] [CrossRef] [PubMed]
- Mogilnicka, I.; Bogucki, P.; Ufnal, M. Microbiota and Malodor—Etiology and Management. Int. J. Mol. Sci. 2020, 21, 2886. [Google Scholar] [CrossRef]
- Bollen, C.M.L.; Beikler, T. Halitosis: The Multidisciplinary Approach. Int. J. Oral Sci. 2012, 4, 55–63. [Google Scholar] [CrossRef]
- Mégraud, F.; Floch, P.; Labenz, J.; Lehours, P. Diagnostic of Helicobacter pylori Infection. Helicobacter 2016, 21, 8–13. [Google Scholar] [CrossRef]
- Graham, D.Y.; Miftahussurur, M. Helicobacter Pylori Urease for Diagnosis of Helicobacter pylori Infection: A Mini Review. J. Adv. Res. 2018, 13, 51–57. [Google Scholar] [CrossRef]
- Mathew, T.L.; Pownraj, P.; Abdulla, S.; Pullithadathil, B. Technologies for Clinical Diagnosis Using Expired Human Breath Analysis. Diagnostics 2015, 5, 27–60. [Google Scholar] [CrossRef]
- Soni, S.; Agrawal, P.; Kumar, N.; Mittal, G.; Nishad, D.K.; Chaudhury, N.K.; Bhatnagar, A.; Basu, M.; Chhillar, N. Salivary Biochemical Markers as Potential Acute Toxicity Parameters for Acute Radiation Injury. Hum. Exp. Toxicol. 2016, 35, 221–228. [Google Scholar] [CrossRef]
- Zhang, A.; Sun, H.; Wang, X. Saliva Metabolomics Opens Door to Biomarker Discovery, Disease Diagnosis, and Treatment. Appl. Biochem. Biotechnol. 2012, 168, 1718–1727. [Google Scholar] [CrossRef]
- Ilea, A.; Andrei, V.; Feurdean, C.N.; Bǎbtan, A.M.; Petrescu, N.B.; Câmpian, R.S.; Bosca, A.B.; Ciui, B.; Tertis, M.; Sǎndulescu, R.; et al. Saliva, a Magic Biofluid Available for Multilevel Assessment and a Mirror of General Health—A Systematic Review. Biosensors 2019, 9, 27. [Google Scholar] [CrossRef]
- Kaczor-Urbanowicz, K.E.; Martin Carreras-Presas, C.; Aro, K.; Tu, M.; Garcia-Godoy, F.; Wong, D.T.W. Saliva Diagnostics—Current Views and Directions. Exp. Biol. Med. 2017, 242, 459–472. [Google Scholar] [CrossRef]
- Evans, R.; Calice-Silva, V.; Raimann, J.G.; Hemmila, U.; Craik, A.; Mtekateka, M.; Hamilton, F.; Kawale, Z.; Dobbie, H.; Dreyer, G.; et al. Diagnostic Performance of a Saliva Urea Nitrogen Dipstick to Detect Kidney Disease in Malawi. Kidney Int. Rep. 2017, 2, 219–227. [Google Scholar] [CrossRef]
- Milanowski, M.; Pomastowski, P.; Ligor, T.; Buszewski, B. Saliva–Volatile Biomarkers and Profiles. Crit. Rev. Anal. Chem. 2017, 47, 251–266. [Google Scholar] [CrossRef]
- Chen, W.; Laiho, S.; Vaittinen, O.; Halonen, L.; Ortiz, F.; Forsblom, C.; Groop, P.H.; Lehto, M.; Metsälä, M. Biochemical Pathways of Breath Ammonia (NH3) Generation in Patients with End-Stage Renal Disease Undergoing Hemodialysis. J. Breath Res. 2016, 10, 036011. [Google Scholar] [CrossRef]
- Huizenga, J.R.; Gips, C.H. Determination of Ammonia in Saliva U Sing Indophenol, an Ammonium Electrode and an Enzymatic Method: A Comparative Investigation. Huizenga Gips: Determ. Ammon. Saliva 1982, 20, 571–574. [Google Scholar] [CrossRef]
- Campíns-Falcó, P.; Moliner-Martínez, Y.; Herráez-Hernández, R.; Verdú-Andrés, J.; Jornet-Matínez, N.P. Device for the detection and/or determination in situ of amines and ammonia. Patents ES 2 619 356 B1, ES 2 519 891 A1, EP 3 001 184 B1.
- Ballester-Caudet, A.; Hakobyan, L.; Moliner-Martinez, Y.; Molins-Legua, C.; Campíns-Falcó, P. Ionic-Liquid Doped Polymeric Composite as Passive Colorimetric Sensor for Meat Freshness as a Use Case. Talanta 2021, 223, 121778. [Google Scholar] [CrossRef]
- Martínez-Aviño, A.; Molins-Legua, C.; Pilar, C.F. Scaling the Analytical Information Given by Several Types of Colorimetric and Spectroscopic Instruments Including Smartphones: Rules for Their Use and Establishing Figures of Merit of Solid Chemosensors. Anal. Chem. 2021, 93, 6043–6052. [Google Scholar] [CrossRef] [PubMed]
- Pla-Tolós, J.; Moliner-Martínez, Y.; Molins-Legua, C.; Campíns-Falcó, P. Solid Glucose Biosensor Integrated in a Multi-Well Microplate Coupled to a Camera-Based Detector: Application to the Multiple Analysis of Human Serum Samples. Sens. Actuators B Chem. 2018, 258, 331–341. [Google Scholar] [CrossRef]
- Martínez-Aviño, A.; de Diego-Llorente-Luque, M.; Molins-Legua, C.; Campíns-Falcó, P. Advances in the Measurement of Polymeric Colorimetric Sensors Using Portable Instrumentation: Testing the Light Influence. Polymers 2022, 14, 4285. [Google Scholar] [CrossRef] [PubMed]
- Carrero-Ferrer, I.; Molins-Legua, C.; Campíns-Falcó, P. Plasmonic sensor for hydrogen sulphide in saliva: Multisensor platform and bag format. Talanta 2022, 245, 123449. [Google Scholar] [CrossRef] [PubMed]






| Samples | Urinary pH | pH (NaOH) | pH (CO32−/HCO3−) |
|---|---|---|---|
| S1 | 6.70 | 12.28 | 10.81 |
| S2 | 5.76 | 12.20 | 10.13 |
| S3 | 7.16 | 11.99 | 10.47 |
| S4 | 6.86 | 11.69 | 10.53 |
| S5 | 6.41 | 12.09 | 10.09 |
| S7 | 6.79 | 12.13 | 10.50 |
| S8 | 6.37 | 11.74 | 10.17 |
| S9 | 5.09 | 11.87 | 9.87 |
| S10 | 6.31 | 12.34 | 10.30 |
| S11 | 7.18 | 12.24 | 10.30 |
| S12 | 6.89 | 11.88 | 10.19 |
| Reaction Time | Method | Linearity | LOD | Linear Interval LOQ-Higher C | |||
|---|---|---|---|---|---|---|---|
| b1 ± Sb1 | b0 ± Sb0 | R2 | |||||
| t = 20 min | Diffuse reflectance | Intraday | (a) 0.366 ± 0.019 | 0.088 ± 0.015 | 0.98 | 0.06 | 0.20–1.5 |
| (b) 0.70 ± 0.04 | 0.088 ± 0.015 | 0.98 | 0.03 | 0.10–0.74 | |||
| Interday | (a) 0.342 ± 0.019 | 0.092 ± 0.014 | 0.98 | 0.06 | 0.20–1.5 | ||
| (b) 0.65 ± 0.04 | 0.092 ± 0.014 | 0.98 | 0.03 | 0.11–0.74 | |||
| Go Spectro | Intraday | (a) 0.322 ± 0.015 | 0.098 ± 0.007 | 0.99 | 0.14 | 0.44–0.95 | |
| (b) 0.61 ± 0.03 | 0.098 ± 0.007 | 0.99 | 0.08 | 0.2–0.56 | |||
| Interday | (a) 0.31 ± 0.09 | 0.095 ± 0.005 | 0.99 | 0.15 | 0.45–0.95 | ||
| (b) 0.58 ± 0.02 | 0.095 ± 0.005 | 0.99 | 0.08 | 0.2–0.56 | |||
| RGB (Red) | Intraday | (a) −77 ± 6 | 212 ± 3 | 0.97 | 0.16 | 0.49–0.95 | |
| (b) −146 ± 12 | 212 ± 3 | 0.97 | 0.09 | 0.26–0.56 | |||
| Interday | (a) −67 ± 5 | 214 ± 2 | 0.98 | 0.19 | 0.56–0.95 | ||
| (b) −127 ± 9 | 214 ± 2 | 0.98 | 0.10 | 0.30–0.56 | |||
| Reaction Time | Measurement | Linearity | LOD | Linear Interval LOQ-Higher C | |||
|---|---|---|---|---|---|---|---|
| b1 ± Sb1 | b0 ± Sb0 | R2 | |||||
| t = 45 min | Diffuse reflectance | Intraday | (a) 1.06 ± 0.09 | 0.041 ± 0.013 | 0.97 | 0.02 | 0.06–0.56 |
| (b) 2.02 ± 0.17 | 0.041 ± 0.013 | 0.97 | 0.01 | 0.03–0.15 | |||
| Interday | (a) 1.04 ± 0.06 | 0.049 ± 0.009 | 0.98 | 0.02 | 0.07–0.56 | ||
| (b) 1.97 ± 0.12 | 0.049 ± 0.009 | 0.98 | 0.01 | 0.04–0.15 | |||
| Go Spectro | Intraday | (a) 0.92 ± 0.05 | 0.049 ± 0.013 | 0.98 | 0.05 | 0.15–0.56 | |
| (b) 1.75 ± 0.10 | 0.049 ± 0.013 | 0.98 | 0.03 | 0.08–0.15 | |||
| Interday | (a) 0.89 ± 0.07 | 0.069 ± 0.006 | 0.99 | 0.05 | 0.16–0.56 | ||
| (b) 1.69 ± 0.05 | 0.069 ± 0.006 | 0.99 | 0.03 | 0.08–0.15 | |||
| RGB (Red) | Intraday | (a) −152 ± 8 | 217 ± 2 | 0.98 | 0.08 | 0.25–0.56 | |
| (b) −287 ± 15 | 217 ± 2 | 0.98 | 0.04 | 0.13–0.26 | |||
| Interday | (a) −140 ± 8 | 213 ± 2 | 0.98 | 0.09 | 0.27–0.56 | ||
| (b) −265 ± 15 | 213 ± 2 | 0.98 | 0.05 | 0.14–0.26 | |||
| Measurement | Linearity (mg NH4+/mL Saliva) | |||
|---|---|---|---|---|
| b1 ± sb1 | b0 ± sb0 | R2 | ||
| Diffuse reflectance | External calibration | 1.97 ± 0.11 | 0.049 ± 0.009 | 0.98 |
| Standard addition | 1.53 ± 0.10 | 0.052 ± 0.006 | 0.99 | |
| Go Spectro | External calibration | 1.69 ± 0.05 | 0.069 ± 0.006 | 0.99 |
| Standard addition | 1.174 ± 0.014 | 0.0212 ± 0.0008 | 0.99 | |
| RGB (Red) | External calibration | −265 ± 15 | 213 ± 2 | 0.98 |
| Standard addition | −239 ± 42 | 188 ± 3 | 0.97 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Monforte-Gómez, B.; Hakobyan, L.; Molins-Legua, C.; Campíns-Falcó, P. Passive Solid Chemosensor as Saliva Point of Need Analysis for Ammonium Determination by Using a Smartphone. Chemosensors 2023, 11, 387. https://doi.org/10.3390/chemosensors11070387
Monforte-Gómez B, Hakobyan L, Molins-Legua C, Campíns-Falcó P. Passive Solid Chemosensor as Saliva Point of Need Analysis for Ammonium Determination by Using a Smartphone. Chemosensors. 2023; 11(7):387. https://doi.org/10.3390/chemosensors11070387
Chicago/Turabian StyleMonforte-Gómez, Belén, Lusine Hakobyan, Carmen Molins-Legua, and Pilar Campíns-Falcó. 2023. "Passive Solid Chemosensor as Saliva Point of Need Analysis for Ammonium Determination by Using a Smartphone" Chemosensors 11, no. 7: 387. https://doi.org/10.3390/chemosensors11070387
APA StyleMonforte-Gómez, B., Hakobyan, L., Molins-Legua, C., & Campíns-Falcó, P. (2023). Passive Solid Chemosensor as Saliva Point of Need Analysis for Ammonium Determination by Using a Smartphone. Chemosensors, 11(7), 387. https://doi.org/10.3390/chemosensors11070387







