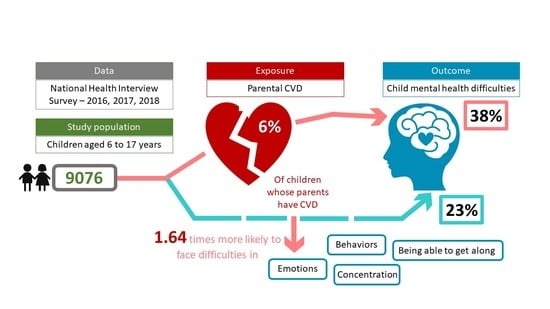
The Influence of Parent’s Cardiovascular Morbidity on Child Mental Health: Results from the National Health Interview Survey
Abstract
:1. Introduction
2. Materials and Methods
2.1. Data
2.2. Measures
2.3. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- World Health Organization. Cardiovascular Diseases (CVDs); World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Esposito, K.; Giugliano, D. Diet and inflammation: A link to metabolic and cardiovascular diseases. Eur. Heart J. 2006, 27, 15–20. [Google Scholar] [CrossRef] [PubMed]
- Virani, S.S.; Alonso, A.; Benjamin, E.J.; Bittencourt, M.S.; Callaway, C.W.; Carson, A.P.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Delling, F.N.; et al. Heart Disease and Stroke Statistics—2020 Update: A Report From the American Heart Association. Circulation 2020, 141, e139–e596. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, E.J.; Virani, S.S.; Callaway, C.W.; Chamberlain, A.M.; Chang, A.R.; Cheng, S.; Chiuve, S.E.; Cushman, M.; Delling, F.N.; Deo, R.; et al. Heart Disease and Stroke Statistics—2018 Update: A Report From the American Heart Association. Circulation 2018, 137, e67–e492. [Google Scholar] [CrossRef] [PubMed]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; Das, S.R.; de Ferranti, S.; Després, J.-P.; Fullerton, H.J.; et al. Heart Disease and Stroke Statistics—2016 Update. Circulation 2016, 133, e38–e360. [Google Scholar] [CrossRef]
- Low, C.A.; Thurston, R.C.; Matthews, K.A. Psychosocial factors in the development of heart disease in women: Current research and future directions. Psychosom. Med. 2010, 72, 842–854. [Google Scholar] [CrossRef] [Green Version]
- Everson-Rose, S.A.; Lewis, T.T. Psychosocial factors and cardiovascular diseases. Annu. Rev. Public Health 2004, 26, 469–500. [Google Scholar] [CrossRef]
- Kivimäki, M.; Kawachi, I. Work Stress as a Risk Factor for Cardiovascular Disease. Curr. Cardiol. Rep. 2015, 17, 74. [Google Scholar] [CrossRef] [Green Version]
- Nagai, M.; Hoshide, S.; Kario, K. Sleep duration as a risk factor for cardiovascular disease—A review of the recent literature. Curr. Cardiol. Rev. 2010, 6, 54–61. [Google Scholar] [CrossRef]
- Dar, T.; Radfar, A.; Abohashem, S.; Pitman, R.K.; Tawakol, A.; Osborne, M.T. Psychosocial Stress and Cardiovascular Disease. Curr. Treat. Options Cardiovasc. Med. 2019, 21, 23. [Google Scholar] [CrossRef]
- Heidenreich, P.A.; Trogdon, J.G.; Khavjou, O.A.; Butler, J.; Dracup, K.; Ezekowitz, M.D.; Finkelstein, E.A.; Hong, Y.; Johnston, S.C.; Khera, A.; et al. Forecasting the Future of Cardiovascular Disease in the United States. Circulation 2011, 123, 933–944. [Google Scholar] [CrossRef]
- Rodgers, J.L.; Jones, J.; Bolleddu, S.I.; Vanthenapalli, S.; Rodgers, L.E.; Shah, K.; Karia, K.; Panguluri, S.K. Cardiovascular Risks Associated with Gender and Aging. J. Cardiovasc. Dev. Dis. 2019, 6, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fayaz, A.; Ayis, S.; Panesar, S.S.; Langford, R.M.; Donaldson, L.J. Assessing the relationship between chronic pain and cardiovascular disease: A systematic review and meta-analysis. Scand. J. Pain 2016, 13, 76–90. [Google Scholar] [CrossRef] [PubMed]
- Higgins, K.S.; Birnie, K.A.; Chambers, C.T.; Wilson, A.C.; Caes, L.; Clark, A.J.; Lynch, M.; Stinson, J.; Campbell-Yeo, M. Offspring of parents with chronic pain: A systematic review and meta-analysis of pain, health, psychological, and family outcomes. Pain 2015, 156, 2256–2266. [Google Scholar] [CrossRef] [PubMed]
- Kaasbøll, J.; Lydersen, S.; Indredavik, M.S. Psychological symptoms in children of parents with chronic pain—The HUNT study. Pain 2012, 153, 1054–1062. [Google Scholar] [CrossRef] [PubMed]
- Cozza, S.J.; Holmes, A.K.; Van Ost, S.L. Family-Centered Care for Military and Veteran Families Affected by Combat Injury. Clin. Child Fam. Psychol. Rev. 2013, 16, 311–321. [Google Scholar] [CrossRef] [PubMed]
- Kaasbøll, J.; Skokauskas, N.; Lydersen, S.; Sund, A.M. Parental Chronic Illness, Internalizing Problems in Young Adulthood and the Mediating Role of Adolescent Attachment to Parents: A Prospective Cohort Study. Front. Psychiatry 2021, 12, 807563. [Google Scholar] [CrossRef]
- Gan, Y.; Gong, Y.; Tong, X.; Sun, H.; Cong, Y.; Dong, X.; Wang, Y.; Xu, X.; Yin, X.; Deng, J.; et al. Depression and the risk of coronary heart disease: A meta-analysis of prospective cohort studies. BMC Psychiatry 2014, 14, 371. [Google Scholar] [CrossRef] [Green Version]
- Havranek, E.P.; Mujahid, M.S.; Barr, D.A.; Blair, I.V.; Cohen, M.S.; Cruz-Flores, S.; Davey-Smith, G.; Dennison-Himmelfarb, C.R.; Lauer, M.S.; Lockwood, D.W.; et al. Social Determinants of Risk and Outcomes for Cardiovascular Disease. Circulation 2015, 132, 873–898. [Google Scholar] [CrossRef] [Green Version]
- Levine, G.N.; Cohen, B.E.; Commodore-Mensah, Y.; Fleury, J.; Huffman, J.C.; Khalid, U.; Labarthe, D.R.; Lavretsky, H.; Michos, E.D.; Spatz, E.S.; et al. Psychological Health, Well-Being, and the Mind-Heart-Body Connection: A Scientific Statement From the American Heart Association. Circulation 2021, 143, e763–e783. [Google Scholar] [CrossRef]
- Smith, M. Parental mental health: Disruptions to parenting and outcomes for children. Child Fam. Soc. Work. 2004, 9, 3–11. [Google Scholar] [CrossRef]
- Amrock, S.M.; Weitzman, M. Parental Psychological Distress and Children’s Mental Health: Results of a National Survey. Acad. Pediatr. 2014, 14, 375–381. [Google Scholar] [CrossRef] [PubMed]
- Madigan, S.; Oatley, H.; Racine, N.; Fearon, R.P.; Schumacher, L.; Akbari, E.; Cooke, J.E.; Tarabulsy, G.M. A Meta-Analysis of Maternal Prenatal Depression and Anxiety on Child Socioemotional Development. J. Am. Acad. Child Adolesc. Psychiatry 2018, 57, 645–657.e8. [Google Scholar] [CrossRef] [PubMed]
- Sieh, D.S.; Meijer, A.M.; Oort, F.J.; Visser-Meily, J.M.A.; Van der Leij, D.A.V. Problem Behavior in Children of Chronically Ill Parents: A Meta-Analysis. Clin. Child Fam. Psychol. Rev. 2010, 13, 384–397. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pakenham, K.I.; Cox, S. The Effects of Parental Illness and Other Ill Family Members on the Adjustment of Children. Ann. Behav. Med. 2014, 48, 424–437. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Barkmann, C.; Romer, G.; Watson, M.; Schulte-Markwort, M. Parental Physical Illness as a Risk for Psychosocial Maladjustment in Children and Adolescents: Epidemiological Findings From a National Survey in Germany. Psychosomatics 2007, 48, 476–481. [Google Scholar] [CrossRef]
- Pilato, J.; Dorard, G.; Chevrier, B.; Leu, A.; Untas, A. Quality of Life of Adolescents Facing a Parental Illness: A Person-Oriented Approach. Int. J. Environ. Res. Public Health 2022, 19, 7892. [Google Scholar] [CrossRef]
- de Roos, S.A.; Iedema, J.; de Boer, A.H. Quality of Life of Schoolchildren Living with a Long-Term Sick Parent: The Role of Tasks at Home, Life Circumstances and Social Support. Int. J. Environ. Res. Public Health 2022, 19, 7043. [Google Scholar] [CrossRef]
- Jørgensen, S.E.; Thygesen, L.C.; Andersen, A.; Due, P.; Michelsen, S.I. Parental Illness and Life Satisfaction among Young People: A Cross-Sectional Study of the Importance of School Factors. Int. J. Environ. Res. Public Health 2022, 19, 2719. [Google Scholar] [CrossRef]
- Aldridge, J. Where are we now? Twenty-five years of research, policy and practice on young carers. Crit. Soc. Policy 2017, 38, 155–165. [Google Scholar] [CrossRef] [Green Version]
- Kavanaugh, M.S.; Stamatopoulos, V.; Cohen, D.; Zhang, L. Unacknowledged Caregivers: A Scoping Review of Research on Caregiving Youth in the United States. Adolesc. Res. Rev. 2016, 1, 29–49. [Google Scholar] [CrossRef]
- Cheesbrough, S.; Harding, C.; Webster, H.; Taylor, L.; Aldridge, J. The Lives of Young Carers in England Omnibus Survey Report: Research Report; Department for Education: London, UK, 2017.
- Stamatopoulos, V. The young carer penalty: Exploring the costs of caregiving among a sample of Canadian youth. Child Youth Serv. 2018, 39, 180–205. [Google Scholar] [CrossRef]
- Becker, S. Global Perspectives on Children’s Unpaid Caregiving in the Family: Research and Policy on ‘Young Carers’ in the UK, Australia, the USA and Sub-Saharan Africa. Glob. Soc. Policy 2007, 7, 23–50. [Google Scholar] [CrossRef] [Green Version]
- Levine, C.; Hunt, G.G.; Halper, D.; Hart, A.Y.; Lautz, J.; Gould, D.A. Young Adult Caregivers: A First Look at an Unstudied Population. Am. J. Public Health 2005, 95, 2071–2075. [Google Scholar] [CrossRef] [PubMed]
- Bursnall, S.; Pakenham, K.I. Too Small for Your Boots! Understanding the experience of children when family members acquire a neurological condition. In Health and Healing after Traumatic Brain Injury: Understanding the Power of Family, Friends, Community, and Other Support Systems: Understanding the Power of Family, Friends, Community, and Other Support Systems; ABC-CLIO: Santa Barbara, CA, USA, 2013; pp. 87–100. [Google Scholar]
- McDowell, D.J.; Parke, R.D. Parental correlates of children’s peer relations: An empirical test of a tripartite model. Dev. Psychol. 2009, 45, 224. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Williams, K.D. Ostracism. Annu. Rev. Psychol. 2006, 58, 425–452. [Google Scholar] [CrossRef]
- Thapar, A.; Collishaw, S.; Pine, D.S.; Thapar, A.K. Depression in adolescence. Lancet 2012, 379, 1056–1067. [Google Scholar] [CrossRef] [Green Version]
- Gaspar, T.; Gomez-Baya, D.; Trindade, J.S.; Botelho Guedes, F.; Cerqueira, A.; de Matos, M.G. Relationship Between Family Functioning, Parents’ Psychosocial Factors, and Children’s Well-Being. J. Fam. Issues 2022, 43, 2380–2397. [Google Scholar] [CrossRef]
- Min, Y.I.; Anugu, P.; Butler, K.R.; Hartley, T.A.; Mwasongwe, S.; Norwood, A.F.; Sims, M.; Wang, W.; Winters, K.P.; Correa, A. Cardiovascular Disease Burden and Socioeconomic Correlates: Findings from the Jackson Heart Study. J. Am. Heart Assoc. 2017, 6, e004416. [Google Scholar] [CrossRef]
- Andrade, C.; Gillen, M.; Molina, J.A.; Wilmarth, M.J. The Social and Economic Impact of Covid-19 on Family Functioning and Well-Being: Where do we go from here? J. Fam. Econ. Issues 2022, 43, 205–212. [Google Scholar] [CrossRef]
- Madjid, M.; Safavi-Naeini, P.; Solomon, S.D.; Vardeny, O. Potential Effects of Coronaviruses on the Cardiovascular System: A Review. JAMA Cardiol. 2020, 5, 831–840. [Google Scholar] [CrossRef]
| Percentage of Children | |||
|---|---|---|---|
| All | Parent Did Not Have CVD | Parent Had CVD | |
| Child’s sex | |||
| Male | 51.21 | 51.33 | 49.35 |
| Female | 48.79 | 48.67 | 50.65 |
| Race | |||
| White | 52.48 | 52.16 | 57.41 |
| Black | 14.27 | 14.31 | 13.76 |
| Hispanic | 23.89 | 24.2 | 19.18 |
| Other | 9.36 | 9.34 | 9.66 |
| Parent’s sex | |||
| Male | 29.43 | 29.26 | 31.98 |
| Female | 70.57 | 70.74 | 68.02 |
| Parent’s marital status | |||
| Married | 61.27 | 61.54 | 57.25 |
| Never married | 12.8 | 13.01 | 9.55 |
| Living with partner | 6.35 | 6.48 | 4.27 |
| Widowed/divorced/separated | 19.58 | 18.97 | 28.93 |
| Parent’s education | |||
| College graduate | 36.26 | 36.29 | 35.83 |
| <High school diploma | 12.85 | 13 | 10.59 |
| High school graduate | 19.01 | 19.21 | 16.03 |
| Some college | 31.87 | 31.5 | 37.56 |
| Parent’s employment | |||
| Not employed | 26.27 | 25.75 | 34.26 |
| Employed | 73.73 | 74.25 | 65.74 |
| Parent’s self-reported health | |||
| Excellent | 30.6 | 31.63 | 14.86 |
| Very good | 34.62 | 35.22 | 25.41 |
| Good | 25.74 | 25.25 | 33.14 |
| Fair | 7.43 | 6.67 | 19.07 |
| Poor | 1.62 | 1.23 | 7.51 |
| Household income | |||
| ≥400% of FPL | 30.39 | 30.53 | 28.29 |
| <100% of FPL | 19.8 | 19.48 | 24.67 |
| 100% to <200% of FPL | 22.8 | 22.96 | 20.35 |
| 200% to <400% of FPL | 27.01 | 27.03 | 26.69 |
| Observations | 9076 | 8513 | 563 |
| No Difficulty | Difficulties | |||
|---|---|---|---|---|
| Minor | Definite | Severe | ||
| Parent’s CVD | ||||
| No | 77.03 | 16.88 | 4.61 | 1.48 |
| (75.89, 78.16) | (15.89, 17.87) | (4.05, 5.16) | (1.18, 1.79) | |
| Yes | 62.00 | 23.89 | 11.39 | 2.73 |
| (56.92, 67.07) | (19.58, 28.19) | (8.02, 14.77) | (1.27, 4.19) | |
| Difference | ||||
| CVD—No CVD | −15.03 *** | 7.00 ** | 6.79 *** | 1.24 |
| (−20.22, −9.85) | (2.6, 11.41) | (3.37, 10.21) | (−0.24, 2.72) | |
| Observations | 6832 | 1608 | 477 | 159 |
| Original Specification | Sensitivity Analysis | |||
|---|---|---|---|---|
| Crude Odds Ratio | Adjusted Odds Ratio | Crude Odds Ratio | Adjusted Odds Ratio | |
| CVD | 2.056 *** | 1.641 *** | 2.535 *** | 1.862 *** |
| (1.643, 2.571) | (1.279, 2.105) | (1.843, 3.487) | (1.295, 2.677) | |
| Child’s age | 1.016 | 1.014 | 1.028 | 1.030 |
| (0.998, 1.033) | (0.993, 1.036) | (0.999, 1.059) | (0.997, 1.065) | |
| Child’s sex | ||||
| Male | Ref. | Ref. | Ref. | Ref. |
| Female | 0.627 *** | 0.609 *** | 0.517 *** | 0.509 *** |
| (0.561, 0.701) | (0.541, 0.685) | (0.424, 0.630) | (0.412, 0.630) | |
| Race | ||||
| White | Ref. | Ref. | Ref. | Ref. |
| Black | 0.988 | 0.710 ** | 0.859 | 0.542 ** |
| (0.816, 1.196) | (0.565, 0.892) | (0.642, 1.151) | (0.369, 0.798) | |
| Hispanic | 0.698 *** | 0.553 *** | 0.724 * | 0.493 *** |
| (0.596, 0.816) | (0.457, 0.669) | (0.561, 0.934) | (0.364, 0.667) | |
| Other | 0.816 * | 0.758 * | 0.778 | 0.645 * |
| (0.666, 0.999) | (0.611, 0.941) | (0.547, 1.107) | (0.447, 0.933) | |
| Parent’s age | 0.992 | 0.992 | 0.989 | 0.988 |
| (0.984, 1.000) | (0.982, 1.002) | (0.975, 1.003) | (0.972, 1.005) | |
| Parent’s sex | ||||
| Male | Ref. | Ref. | Ref. | Ref. |
| Female | 1.593 *** | 1.352 *** | 2.031 *** | 1.634 *** |
| (1.374, 1.846) | (1.147, 1.595) | (1.549, 2.662) | (1.222, 2.186) | |
| Parent’s marital status | ||||
| Married | Ref. | Ref. | Ref. | Ref. |
| Never married | 1.748 *** | 1.550 *** | 1.931 *** | 1.438 |
| (1.466, 2.085) | (1.233, 1.949) | (1.465, 2.545) | (0.999, 2.070) | |
| Living with partner | 1.796 *** | 1.658 *** | 2.655 *** | 2.352 *** |
| (1.418, 2.274) | (1.283, 2.142) | (1.867, 3.776) | (1.624, 3.406) | |
| Widowed/divorced/separated | 1.709 *** | 1.471 *** | 2.277 *** | 1.676 *** |
| (1.477, 1.978) | (1.236, 1.750) | (1.796, 2.887) | (1.262, 2.226) | |
| Parent’s education | ||||
| College graduate | Ref. | Ref. | Ref. | Ref. |
| < High school diploma | 1.211 | 0.957 | 1.374 | 0.755 |
| (0.983, 1.491) | (0.733, 1.248) | (0.960, 1.965) | (0.492, 1.156) | |
| High school graduate | 1.182 | 0.903 | 1.446 * | 0.835 |
| (0.999, 1.398) | (0.732, 1.113) | (1.077, 1.941) | (0.598, 1.168) | |
| Some college | 1.448 *** | 1.086 | 1.373 * | 0.774 |
| (1.254, 1.673) | (0.914, 1.292) | (1.073, 1.756) | (0.594, 1.009) | |
| Parent’s employment | ||||
| Not employed | Ref. | Ref. | Ref. | Ref. |
| Employed | 0.676 *** | 0.812 ** | 0.672 *** | 0.996 |
| (0.598, 0.766) | (0.694, 0.951) | (0.548, 0.825) | (0.785, 1.263) | |
| Parent’s self-reported health | ||||
| Excellent | Ref. | Ref. | Ref. | Ref. |
| Very good | 1.656 *** | 1.596 *** | 1.812 *** | 1.685 ** |
| (1.391, 1.971) | (1.326, 1.921) | (1.297, 2.530) | (1.190, 2.385) | |
| Good | 2.526 *** | 2.455 *** | 3.376 *** | 3.137 *** |
| (2.114, 3.017) | (2.017, 2.988) | (2.423, 4.702) | (2.192, 4.490) | |
| Fair | 3.679 *** | 3.305 *** | 5.480 *** | 4.694 *** |
| (2.913, 4.646) | (2.547, 4.288) | (3.798, 7.908) | (3.109, 7.086) | |
| Poor | 7.088 *** | 4.856 *** | 11.865 *** | 7.873 *** |
| (4.702, 10.686) | (3.128, 7.539) | (7.085, 19.871) | (4.462, 13.891) | |
| Household income | ||||
| ≥400% of FPL | Ref. | Ref. | Ref. | Ref. |
| <100% of FPL | 1.752 *** | 1.073 | 2.416 *** | 1.570 * |
| (1.474, 2.082) | (0.832, 1.384) | (1.802, 3.241) | (1.031, 2.392) | |
| 100% to <200% of FPL | 1.384 *** | 1.037 | 1.979 *** | 1.516 * |
| (1.172, 1.635) | (0.837, 1.284) | (1.499, 2.613) | (1.094, 2.100) | |
| 200% to <400% of FPL | 1.176 | 0.970 | 1.073 | 0.886 |
| (0.997, 1.386) | (0.802, 1.172) | (0.789, 1.459) | (0.628, 1.249) | |
| Observations | 9076 | 8663 | 9076 | 8663 |
| Has Many Worries/Often Seemed Worried | Often Unhappy/ Depressed/ Tearful | Well Behaved/ Usually Does What Adults Request | Has Good Attention Span | |
|---|---|---|---|---|
| A. Unadjusted | ||||
| CVD | 1.754 *** | 1.866 *** | 0.617 | 0.604 ** |
| (1.406, 2.187) | (1.440, 2.419) | (0.349, 1.090) | (0.447, 0.818) | |
| Observations | 9070 | 9070 | 9075 | 9072 |
| B. Adjusted | ||||
| CVD | 1.307 * | 1.401 * | 0.764 | 0.717 * |
| (1.034, 1.653) | (1.060, 1.852) | (0.414, 1.411) | (0.516, 0.996) | |
| Observations | 8658 | 8660 | 8663 | 8660 |
| Base Outcome: No Difficulty | Outcome I: Minor Difficulties | Outcome II: Definite Difficulties | Outcome III: Severe Difficulties | |
|---|---|---|---|---|
| A. Unadjusted | ||||
| CVD | Ref. | 1.758 *** | 3.073 *** | 2.282 ** |
| (1.363, 2.268) | (2.128, 4.439) | (1.265, 4.118) | ||
| B. Adjusted | ||||
| CVD | Ref. | 1.480 ** | 2.250 *** | 1.605 |
| (1.129, 1.938) | (1.465, 3.455) | (0.890, 2.897) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Datta, B.K.; Tiwari, A.; Pollard, E.; Ravula, H. The Influence of Parent’s Cardiovascular Morbidity on Child Mental Health: Results from the National Health Interview Survey. Children 2023, 10, 138. https://doi.org/10.3390/children10010138
Datta BK, Tiwari A, Pollard E, Ravula H. The Influence of Parent’s Cardiovascular Morbidity on Child Mental Health: Results from the National Health Interview Survey. Children. 2023; 10(1):138. https://doi.org/10.3390/children10010138
Chicago/Turabian StyleDatta, Biplab Kumar, Ashwini Tiwari, Elinita Pollard, and Havilah Ravula. 2023. "The Influence of Parent’s Cardiovascular Morbidity on Child Mental Health: Results from the National Health Interview Survey" Children 10, no. 1: 138. https://doi.org/10.3390/children10010138