Comparison of Malnutrition Indicators and Associated Socio-Demographic Factors among Children in Rural and Urban Public Primary Schools in South Africa
Abstract
:1. Introduction
2. Methods
2.1. Study Design, Population, and Settings
2.2. Sample Size and Sampling Technique
2.3. Data Collection and Tools
2.4. Statistical Analysis
2.5. Ethics Statement
3. Results
3.1. Characteristics of Caregivers and School Children
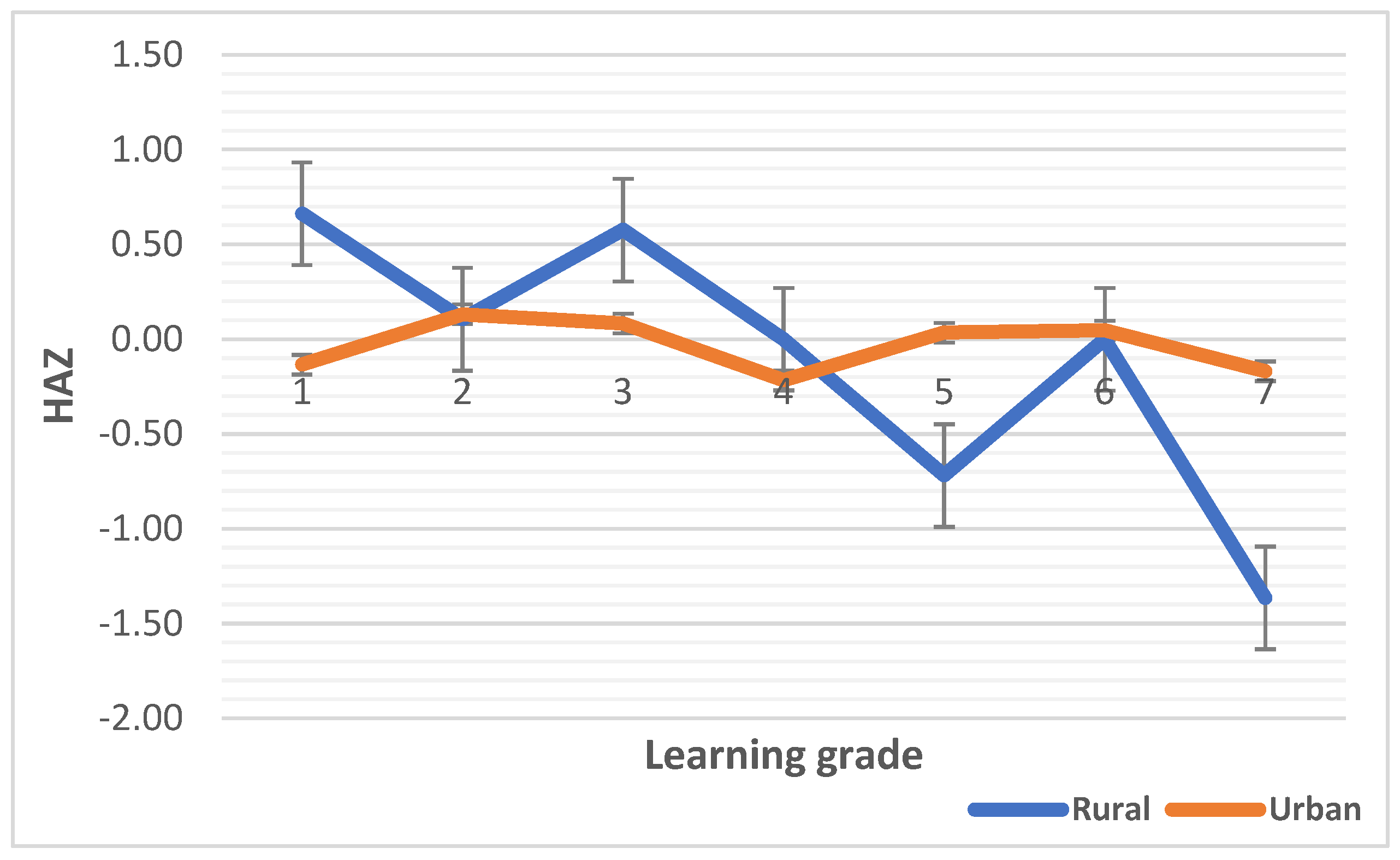
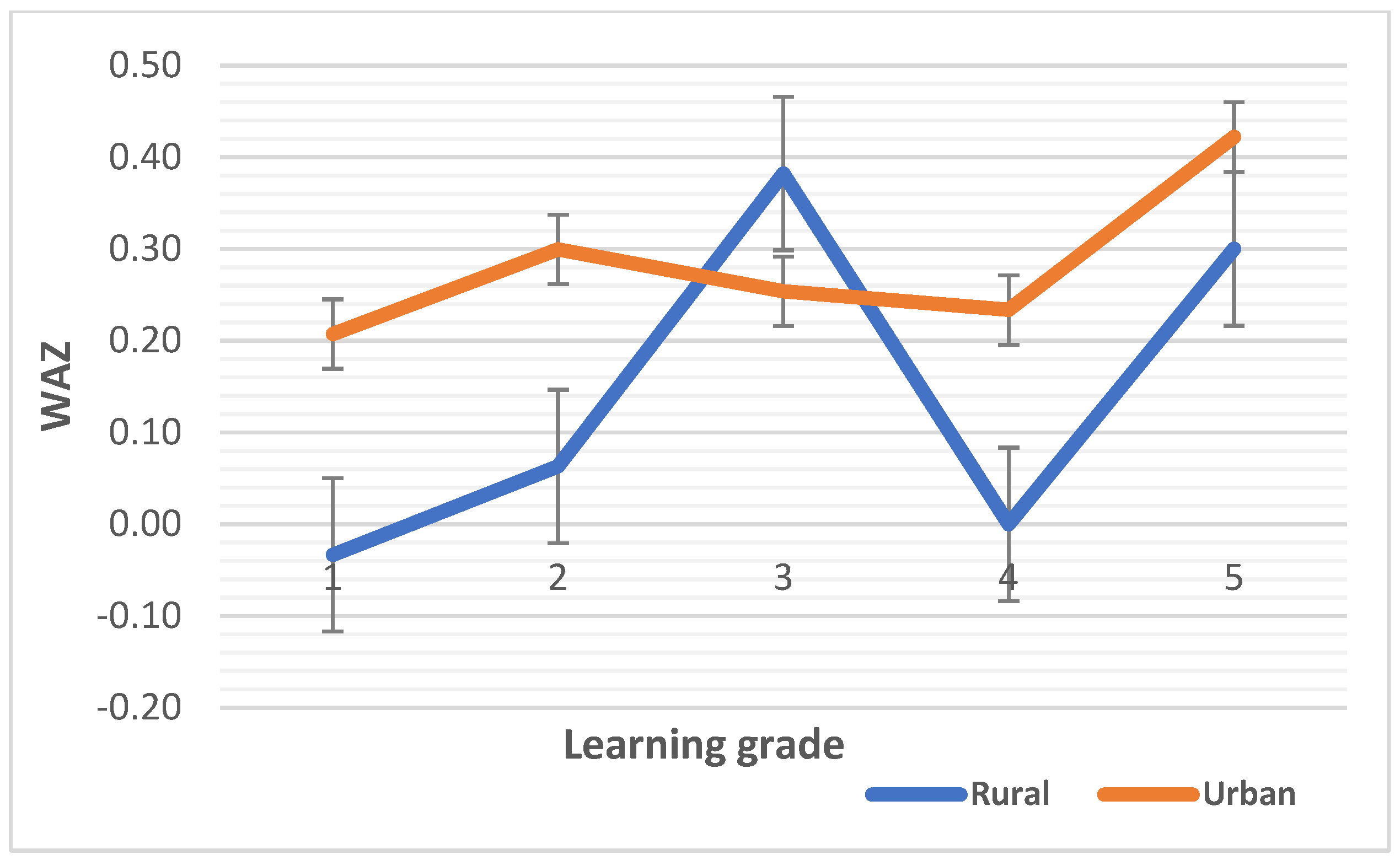
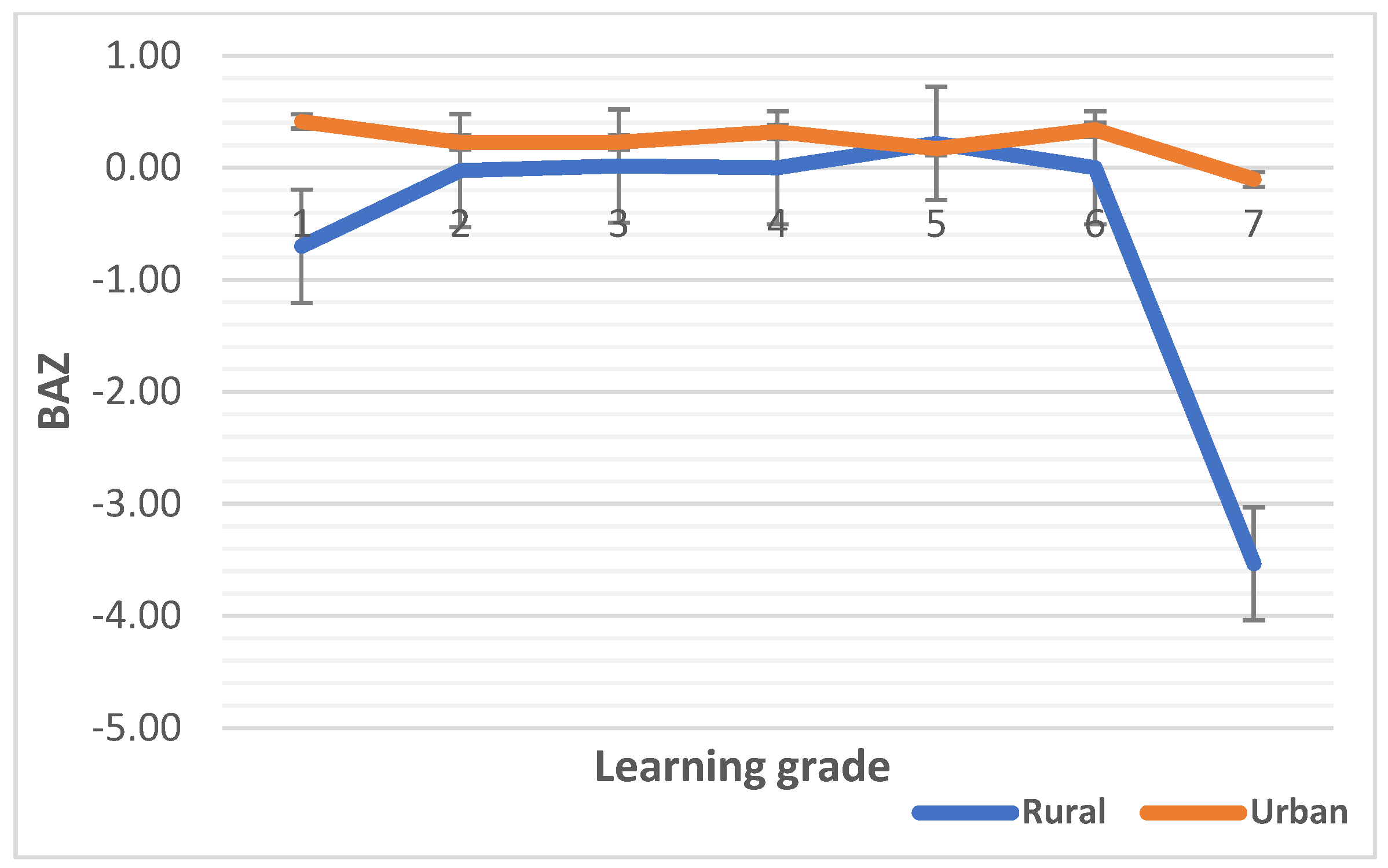
3.2. Median Values of Malnutrition Indicators
3.3. The Association of Malnutrition Indicators with Covariates among School Children
3.3.1. Bivariate Association Using Chi-Square/Fisher Exact Tests
3.3.2. The Association of Malnutrition Indicators Using Multivariable Logistic Regression
4. Discussion
Limitations of This Study
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Black, R.E.; Victora, C.G.; Walker, S.P.; Bhutta, Z.A.; Christian, P.; de Onis, M.; Ezzati, M.; Grantham-McGregor, S.; Katz, J.; Martorell, R.; et al. Maternal and child undernutrition and overweight in low-income and middle-income countries. Lancet 2013, 382, 427–451. [Google Scholar] [CrossRef] [PubMed]
- Modjadji, P.; Madiba, S. The double burden of malnutrition in a rural health and demographic surveillance system site in South Africa: A study of primary schoolchildren and their mothers. BMC Public Health 2019, 19, 1087. [Google Scholar] [CrossRef] [PubMed]
- LBD Double Burden of Malnutrition Collaborators. Mapping local patterns of childhood overweight and wasting in low-and middle-income countries between 2000 and 2017. Nat. Med. 2020, 26, 750–759. [Google Scholar] [CrossRef] [PubMed]
- Modjadji, P.; Madiba, S. Childhood Undernutrition and Its Predictors in a Rural Health and Demographic Surveillance System Site in South Africa. Int. J. Environ. Res. Public Health 2019, 16, 3021. [Google Scholar] [CrossRef]
- WHO. Malnutrition. Available online: https://www.who.int/news-room/fact-sheets/detail/malnutrition (accessed on 10 May 2023).
- UNICEF. What You Need to Know about Malnutrition & Feeding Children. 2020. Available online: https://www.unicef.org/southafrica/stories/what-you-need-know-about-malnutrition-feeding-children (accessed on 15 May 2023).
- Achadi, E.; Ahuja, A.; Bendech, M.A.; Bhutta, Z.A.; De-Regil, L.M.; Fanzo, J.; Fracassi, P.; Grummer-Strawn, L.M.; Haddad, L.J.; Hawkes, C. Global Nutrition Report 2016: From Promise to Impact: Ending Malnutrition by 2030; International Food Policy Research Institute: Washington, DC, USA, 2016. [Google Scholar]
- de Onis, M.; Branca, F. Childhood stunting: A global perspective. Matern. Child Nutr. 2016, 12 (Suppl. S1), 12–26. [Google Scholar] [CrossRef] [PubMed]
- Fekadu, Y.; Mesfin, A.; Haile, D.; Stoecker, B.J. Factors associated with nutritional status of infants and young children in Somali Region, Ethiopia: A cross-sectional study. BMC Public Health 2015, 15, 846. [Google Scholar] [CrossRef] [PubMed]
- Modjadji, P.; Madiba, S. The Multidimension of Malnutrition among School Children in a Rural Area, South Africa: A Mixed Methods Approach. Nutrients 2022, 14, 5015. [Google Scholar] [CrossRef] [PubMed]
- da Silva Fink, J.; Marcadenti, A.; Rabito, E.I.; Silva, F.M. The New European Society for Clinical Nutrition and Metabolism Definition of Malnutrition: Application for Nutrition Assessment and Prediction of Morbimortality in an Emergency Service. J. Parenter. Enter. Nutr. 2018, 42, 550–556. [Google Scholar] [CrossRef]
- Ooi, P.H.; Thompson-Hodgetts, S.; Pritchard-Wiart, L.; Gilmour, S.M.; Mager, D.R. Pediatric Sarcopenia: A Paradigm in the Overall Definition of Malnutrition in Children? J. Parenter. Enter. Nutr. 2020, 44, 407–418. [Google Scholar] [CrossRef]
- Berheto, T.M.; Mikitie, W.K.; Argaw, A. Urban-rural disparities in the nutritional status of school adolescent girls in the Mizan district, south-western Ethiopia. Rural. Remote Health 2015, 15, 404–405. [Google Scholar]
- Irenso, A.A.; Dessie, Y.; Berhane, Y.; Assefa, N.; Canavan, C.R.; Fawzi, W.W. Prevalence and predictors of adolescent linear growth and stunting across the urban–rural gradient in eastern Ethiopia. Trop. Med. Int. Health 2020, 25, 101–110. [Google Scholar] [CrossRef]
- Omigbodun, O.O.; Adediran, K.I.; Akinyemi, J.O.; Omigbodun, A.O.; Adedokun, B.O.; Esan, O. Gender and rural–urban differences in the nutritional status of in-school adolescents in south-western Nigeria. J. Biosoc. Sci. 2010, 42, 653–676. [Google Scholar] [CrossRef] [PubMed]
- Cordeiro, L.S.; Otis, N.P.; Sibeko, L.; Nelson-Peterman, J. Rural-urban disparities in the nutritional status of younger adolescents in Tanzania. PLoS ONE 2021, 16, e0261480. [Google Scholar] [CrossRef] [PubMed]
- Modjadji, P.; Mashishi, J. Persistent Malnutrition and Associated Factors among Children under Five Years Attending Primary Health Care Facilities in Limpopo Province, South Africa. Int. J. Environ. Res. Public Health 2020, 17, 7580. [Google Scholar] [CrossRef]
- Choukem, S.-P.; Tochie, J.N.; Sibetcheu, A.T.; Nansseu, J.R.; Hamilton-Shield, J.P. Overweight/obesity and associated cardiovascular risk factors in sub-Saharan African children and adolescents: A scoping review. Int. J. Pediatr. Endocrinol. 2020, 2020, 6. [Google Scholar] [CrossRef]
- Mosha, M.V.; Msuya, S.E.; Kasagama, E.; Ayieko, P.; Todd, J.; Filteau, S. Prevalence and correlates of overweight and obesity among primary school children in Kilimanjaro, Tanzania. PLoS ONE 2021, 16, e0249595. [Google Scholar] [CrossRef] [PubMed]
- Williams, A.J.; Wyatt, K.M.; Hurst, A.J.; Williams, C.A. A systematic review of associations between the primary school built environment and childhood overweight and obesity. Health Place 2012, 18, 504–514. [Google Scholar] [CrossRef]
- Mamabolo, R.L.; Alberts, M.; Steyn, N.P.; Delemarre-van de Waal, H.A.; Levitt, N.S. Prevalence and determinants of stunting and overweight in 3-year-old black South African children residing in the Central Region of Limpopo Province, South Africa. Public Health Nutr. 2005, 8, 501–508. [Google Scholar] [CrossRef]
- Modjadji, P.; Masilela, L.N.; Cele, L.; Mathibe, M.; Mphekgwana, P.M. Evidence of Concurrent Stunting and Obesity among Children under 2 Years from Socio-Economically Disadvantaged Backgrounds in the Era of the Integrated Nutrition Programme in South Africa. Int. J. Environ. Res. Public Health 2022, 19, 12501. [Google Scholar] [CrossRef]
- Symington, E.A.; Gericke, G.J.; Nel, J.H.; Labadarios, D. The relationship between stunting and overweight among children from South Africa: Secondary analysis of the national food consumption survey-Fortification baseline I. S.Afr. Med. J. 2016, 106, 65–69. [Google Scholar] [CrossRef]
- Tathiah, N.; Moodley, I.; Mubaiwa, V.; Denny, L.; Taylor, M. South Africa’s nutritional transition: Overweight, obesity, underweight and stunting in female primary school learners in rural KwaZulu-Natal, South Africa. S. Afr. Med. J. = Suid-Afr. Tydskr. Vir Geneeskd. 2013, 103, 718–723. [Google Scholar] [CrossRef]
- Marwat, Z.I.; Nawaz, S.; Wazir, A.K.; Afzal, E.; Gul, C.; Khan, M.J.; Ahmad, A. Nutritional assessment of school going children in district Abbottabad, KP Pakistan. Int. J. Sci. Rep. 2019, 5, 59–65. [Google Scholar] [CrossRef]
- Hadley, C.; Belachew, T.; Lindstrom, D.; Tessema, F. The shape of things to come? household dependency ratio and adolescent nutritional status in rural and urban Ethiopia. Am. J. Phys. Anthropol. 2011, 144, 643–652. [Google Scholar] [CrossRef] [PubMed]
- Keino, S.; Plasqui, G.; Ettyang, G.; van den Borne, B. Determinants of stunting and overweight among young children and adolescents in sub-Saharan Africa. Food Nutr. Bull. 2014, 35, 167–178. [Google Scholar] [CrossRef] [PubMed]
- Smith, L.; Ruel, M.; Ndiaye, A. Why Is Child Malnutrition Lower in Urban Than in Rural Areas? Evidence from 36 Developing Countries. World Dev. 2005, 33, 1285–1305. [Google Scholar] [CrossRef]
- Monyeki, M.A.; Awotidebe, A.; Strydom, G.L.; De Ridder, J.H.; Mamabolo, R.L.; Kemper, H.C. The challenges of underweight and overweight in South African children: Are we winning or losing the battle? A systematic review. Int. J. Environ. Res. Public Health 2015, 12, 1156–1173. [Google Scholar] [CrossRef]
- Dapi, L.N.; Hörnell, A.; Janlert, U.; Stenlund, H.; Larsson, C. Energy and nutrient intakes in relation to sex and socio-economic status among school adolescents in urban Cameroon, Africa. Public Health Nutr. 2011, 14, 904–913. [Google Scholar] [CrossRef]
- Srinivasan, C.S.; Zanello, G.; Shankar, B. Rural-urban disparities in child nutrition in Bangladesh and Nepal. BMC Public Health 2013, 13, 581. [Google Scholar] [CrossRef]
- Sharaf, M.F.; Rashad, A.S. Regional inequalities in child malnutrition in Egypt, Jordan, and Yemen: A Blinder-Oaxaca decomposition analysis. Health Econ. Rev. 2016, 6, 23. [Google Scholar] [CrossRef]
- Fagbamigbe, A.F.; Kandala, N.B.; Uthman, A.O. Demystifying the factors associated with rural–urban gaps in severe acute malnutrition among under-five children in low- and middle-income countries: A decomposition analysis. Sci. Rep. 2020, 10, 11172. [Google Scholar] [CrossRef]
- Kubeka, Z.; Modjadji, P. Association of Stunting with Socio-Demographic Factors and Feeding Practices among Children under Two Years in Informal Settlements in Gauteng, South Africa. Children 2023, 10, 1280. [Google Scholar] [CrossRef] [PubMed]
- Masilela, L.N.; Modjadji, P. Child Nutrition Outcomes and Maternal Nutrition-Related Knowledge in Rural Localities of Mbombela, South Africa. Children 2023, 10, 1294. [Google Scholar] [CrossRef] [PubMed]
- Stamoulis, K.G.; Pingali, P.L.; Shetty, P. Emerging challenges for food and nutrition policy in developing countries. Ejade Electron. J. Agric. Dev. Econ. 2004, 1, 154–167. [Google Scholar]
- WHO. The Physical School Environment: An Essential Component of a Health-Promoting School; World Health Organiazation: Geneva, Switzerland, 2004. Available online: https://www.who.int/publications/i/item/physical-school-environment-element-of-a-health-promoting-school (accessed on 10 June 2021).
- Expatica. Education in South Africa. 2023. Available online: https://www.expatica.com/za/education/children-education/education-in-south-africa-803205/#:~:text=Aside%20from%20international%20schools%2C%20there%20are%20three%20main,the%20quality%20of%20education%20varies%20significantly%20between%20areas (accessed on 20 June 2023).
- Mafugu, T. Challenges encountered in a South African school nutrition programme. J. Public Health Res. 2021, 10, 1982. [Google Scholar] [CrossRef] [PubMed]
- Molotja, C.M.; Maliwichi, L.L.; Jideani, A.I. Nutrition knowledge and food choices of primary school learners in Limpopo Province, South Africa. J. Consum. Sci. 2020, 2020, 98–114. [Google Scholar]
- De Onis, M.; Blössner, M.; Borghi, E. Prevalence and trends of stunting among pre-school children, 1990–2020. Public Health Nutr. 2012, 15, 142–148. [Google Scholar] [CrossRef]
- Onyango, A.W.; Jean-Baptiste, J.; Samburu, B.; Mahlangu, T.L.M. Regional Overview on the Double Burden of Malnutrition and Examples of Program and Policy Responses: African Region. Ann. Nutr. Metab. 2019, 75, 127–130. [Google Scholar] [CrossRef]
- Lettau, J. The Impact of Children’s Academic Competencies and School Grades on their Life Satisfaction: What Really Matters? Child Indic. Res. 2021, 14, 2171–2195. [Google Scholar] [CrossRef]
- Melaku, Y.A.; Zello, G.A.; Gill, T.K.; Adams, R.J.; Shi, Z. Prevalence and factors associated with stunting and thinness among adolescent students in Northern Ethiopia: A comparison to World Health Organization standards. Arch. Public Health 2015, 73, 44. [Google Scholar] [CrossRef]
- Shrimpton, R.; Rokx, C. The Double Burden of Malnutrition: A Review of Global Evidence; The World Bank: Washington, DC, USA, 2012. [Google Scholar]
- Reilly, J.J.; Kelly, J. Long-term impact of overweight and obesity in childhood and adolescence on morbidity and premature mortality in adulthood: Systematic review. Int. J. Obes. 2011, 35, 891–898. [Google Scholar] [CrossRef]
- Berejena, T.; Kleynhans, I.; Vibetti, S. Challenges of the secondary school nutrition programmes in the City of Tshwane, South Africa. Afr. J. Phys. Act. Health Sci. 2018, 24, 233–244. [Google Scholar]
- Graham, L.; Hochfeld, T.; Stuart, L.; Van Gent, M. Evaluation Study of the National School Nutrition Programme and the Tiger Brands Foundation In-School Breakfast Feeding Programme in the Lady Frere and Qumbu Districts of the Eastern Cape; Centre for Social Development in Africa, University of Johannesburg: Johannesburg, South Africa, 2015. [Google Scholar]
- Kwatubana, S.; Thabo, M. Parental Involvement in the Process of Implementation of the National School Nutrition Programme in Public Schools. Int. J. Educ. Sci. 2015, 9, 315–323. [Google Scholar] [CrossRef]
- Debeila, S.; Modjadji, P.; Madiba, S. High prevalence of overall overweight/obesity and abdominal obesity amongst adolescents: An emerging nutritional problem in rural high schools in Limpopo Province, South Africa. Afr. J. Prim. Health Care Fam. Med. 2021, 13, e1–e9. [Google Scholar] [CrossRef]
- UN. Sustainable Development Goals. Available online: http://www.un.org/sustainabledevelopment/news/communications-material/ (accessed on 4 March 2023).
- Oduniyi, O.S. Climate Change Awareness: A Case Study of Small Scale Maize Farmers in Mpumalanga Province, South Africa. Master’s Thesis, University of South Africa, Cape Town, South Africa, 2013. [Google Scholar]
- Africa, S.S. Statistical Release P0441. Gross Domestic Product 2003. Available online: http://www.statssa.gov.za (accessed on 4 March 2023).
- Modjadji, S.E.P.; Madiba, S. Growth Patterns and Socio-Cultural Beliefs and Practices in Dikgale, Limpopo Province. Ph.D. Thesis, Sefako Makgatho Health Sciences University, Ga-Rankuwa, South Africa, 2019. [Google Scholar]
- Modjadji, P. Engaging Mothers on the Growth of School-Age Children in a Rural South African Health and Demographic Site: A Qualitative Insight. Healthcare 2021, 9, 225. [Google Scholar] [CrossRef]
- Modjadji, P. Socio-Demographic determinants of overweight and obesity among mothers of primary school children living in a rural health and demographic surveillance system site, South Africa. Open Public Health J. 2020, 13, 518–528. [Google Scholar] [CrossRef]
- UNICEF. Strategy for Improved Nutrition of Children and Women in Developing Countries UNICEF Policy Review; UNICEF: New York, NY, USA, 1991; Available online: http://repository.forcedmigration.org/show_metadata.jsp?pid=fmo:3066 (accessed on 19 August 2013).
- Bronfenbrenner, U. Ecology of the family as a context for human development: Research perspectives. Dev. Psychol. 1986, 22, 723. [Google Scholar] [CrossRef]
- Herrador, Z.; Sordo, L.; Gadisa, E.; Moreno, J.; Nieto, J.; Benito, A.; Aseffa, A.; Cañavate, C.; Custodio, E. Cross-sectional study of malnutrition and associated factors among school aged children in rural and urban settings of Fogera and Libo Kemkem districts, Ethiopia. PLoS ONE 2014, 9, e105880. [Google Scholar] [CrossRef]
- Hightower, C.; Scott, K. Infer more, describe less: More powerful survey conclusions through easy inferential tests. Issues Sci. Technol. Librariansh. 2012, 69, 1. [Google Scholar] [CrossRef]
- Maimela, E.; Alberts, M.; Modjadji, S.E.; Choma, S.S.; Dikotope, S.A.; Ntuli, T.S.; Van Geertruyden, J.-P. The prevalence and determinants of chronic non-communicable disease risk factors amongst adults in the Dikgale health demographic and surveillance system (HDSS) site, Limpopo Province of South Africa. PLoS ONE 2016, 11, e0147926. [Google Scholar] [CrossRef]
- Modjadji, S.E.P. Nutritional Factors Involved in Development of Neural tube Defects in Offspring of Women Residing in a High Risk Area. Ph.D. Thesis, University of Limpopo (Turfloop Campus), Mankweng, South Africa, 2009. [Google Scholar]
- Norton, K. Standards for Anthropometry Assessment. Kinanthropometry Exerc. Physiol. 2018, 4, 68–137. [Google Scholar]
- WHO. WHO AnthroPlus for Personal Computers Manual: Software for Assessing Growth of the World’s Children and Adolescents; WHO: Geneva, Switzerland, 2009; Volume 45.
- WHO. Physical Status: The Use and Interpretation of Anthropometry; WHO: Geneva, Switzerland, 1995.
- Ashwell, M.; Cole, T.J.; Dixon, A.K. Ratio of waist circumference to height is strong predictor of intra-abdominal fat. BMJ 1996, 313, 559–560. [Google Scholar] [CrossRef] [PubMed]
- Ashwell, M.; Gibson, S. Waist-to-height ratio as an indicator of ‘early health risk’: Simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open 2016, 6, e010159. [Google Scholar] [CrossRef]
- WMA. Declaration of Helsinki. Ethical principles for medical research involving human subjects. Jahrb. Für Wiss. Und Ethik 2009, 14, 233–238. [Google Scholar] [CrossRef]
- DeWet, T.J. The South African Labour Market. University of Pretoria. 2003. Available online: https://repository.up.ac.za/bitstream/handle/2263/25937/03chapter3.pdf?sequence=4 (accessed on 14 May 2023).
- Fransman, T.; Yu, D. Multidimensional poverty in South Africa in 2001–16. Dev. S. Afr. 2019, 36, 50–79. [Google Scholar] [CrossRef]
- Niessen, L.W.; Mohan, D.; Akuoku, J.K.; Mirelman, A.J.; Ahmed, S.; Koehlmoos, T.P.; Trujillo, A.; Khan, J.; Peters, D.H. Tackling socioeconomic inequalities and non-communicable diseases in low-income and middle-income countries under the Sustainable Development agenda. Lancet 2018, 391, 2036–2046. [Google Scholar] [CrossRef]
- Egbujie, B.A.; Igumbor, E.U.; Puoane, T. A cross-sectional study of socioeconomic status and cardiovascular disease risk among participants in the Prospective Urban Rural Epidemiological (PURE) Study. S. Afr. Med. J. = Suid-Afr. Tydskr. Vir Geneeskd. 2016, 106, 900–906. [Google Scholar] [CrossRef]
- Peer, N.; Bradshaw, D.; Laubscher, R.; Steyn, N.; Steyn, K. Urban-rural and gender differences in tobacco and alcohol use, diet and physical activity among young black South Africans between 1998 and 2003. Glob. Health Action 2013, 6, 19216. [Google Scholar] [CrossRef]
- Peltzer, K.; Phaswana-Mafuya, N.; Pengpid, S. Rural-urban health disparities among older adults in South Africa. Afr. J. Prim. Health Care Fam. Med. 2019, 11, e1–e6. [Google Scholar] [CrossRef]
- van der Hoeven, M.; Kruger, A.; Greeff, M. Differences in health care seeking behaviour between rural and urban communities in South Africa. Int. J. Equity Health 2012, 11, 31. [Google Scholar] [CrossRef]
- Wu, F.; Guo, Y.; Chatterji, S.; Zheng, Y.; Naidoo, N.; Jiang, Y.; Biritwum, R.; Yawson, A.; Minicuci, N.; Salinas-Rodriguez, A.; et al. Common risk factors for chronic non-communicable diseases among older adults in China, Ghana, Mexico, India, Russia and South Africa: The study on global AGEing and adult health (SAGE) wave 1. BMC Public Health 2015, 15, 88. [Google Scholar] [CrossRef]
- Modjadji, P.; Molokwane, D.; Ukegbu, P.O. Dietary Diversity and Nutritional Status of Preschool Children in North West Province, South Africa: A Cross Sectional Study. Children 2020, 7, 174. [Google Scholar] [CrossRef]
- Drake, L.; Woolnough, A.; Bundy, D.; Burbano, C. Global School Feeding Sourcebook: Lessons from 14 Countries; World Scientific: London, UK, 2016. [Google Scholar]
- Department of Education. Age Requiremen t for Admission to an Ordinary Public School Governement Gazette. 1998. Available online: https://www.education.gov.za/Portals/0/Documents/Legislation/Gov%20Not/Age%20requirements%20for%20admission%20to%20an%20ordinary%20public%20school.pdf?ver=2008-07-02-153110-123 (accessed on 14 May 2023).
- Brou, A.M.; Djalega, F.A.; Tokpa, V.; Seri, E.C.G.; Anoua, A.L.F.; Robinson, J.A. Urban-rural differences in the relationship between stunting, preschool attendance, home learning support, and school readiness: A study in Côte d’Ivoire. Front. Public Health 2022, 10, 1035488. [Google Scholar] [CrossRef] [PubMed]
- National Planning Commission. South Africa’s Implementation of the 2030 Agenda for Sustainable Development ‘Solving Complex Challenges Together’; National Planning Commission: Pretoria, South Africa, 2019.
- Sello, M.; Adedini, S.A.; Odimegwu, C.; Petlele, R.; Tapera, T. The Relationship between Childcare-Giving Arrangements and Children’s Malnutrition Status in South Africa. Int. J. Environ. Res. Public Health 2023, 20, 2572. [Google Scholar] [CrossRef] [PubMed]
- Kekana, M.J.; Mabapa, N.S.; Mbhenyane, X.G. Impact of the child support grant on the diet and nutritional status of children under 5 years old in Mogalakwena Municipality, Limpopo Province, South Africa. S. Afr. J. Child Health 2020, 14, 15–19. [Google Scholar]
- Tzioumis, E.; Adair, L.S. Childhood Dual Burden of Under- and Overnutrition in Low- and Middle-inCome Countries: A Critical Review. Food Nutr. Bull. 2014, 35, 230–243. [Google Scholar] [CrossRef] [PubMed]
- Iftikhar, A.; Bari, A.; Bano, I.; Masood, Q. Impact of maternal education, employment and family size on nutritional status of children. Pak. J. Med. Sci. 2017, 33, 1401–1405. [Google Scholar] [CrossRef] [PubMed]
- Moura, A.F.; Philippe, K. Where is the father? Challenges and solutions to the inclusion of fathers in child feeding and nutrition research. BMC Public Health 2023, 23, 1183. [Google Scholar] [CrossRef]
- Granlund, S.; Hochfeld, T. ‘That Child Support Grant Gives Me Powers’—Exploring Social and Relational Aspects of Cash Transfers in South Africa in Times of Livelihood Change. J. Dev. Stud. 2020, 56, 1230–1244. [Google Scholar] [CrossRef]
- Hall, K.; Sambu, W. Income Poverty, Unemployment and Social Grants. S. Afr. Child Gauge Child. Fam. State. 2018, 27, 137–143. [Google Scholar]
- Zerga, A.A.; Tadesse, S.E.; Ayele, F.Y.; Ayele, S.Z. Impact of malnutrition on the academic performance of school children in Ethiopia: A systematic review and meta-analysis. SAGE Open Med. 2022, 10, 20503121221122398. [Google Scholar] [CrossRef]
| Variables | Categories | All n (%) | Rural n (%) | Urban n (%) | Chi-Square/Fisher Exact Test p |
|---|---|---|---|---|---|
| Caregivers age (years) | <35 | 123 (28) | 109 (28) | 144 (28) | 0.968 |
| ≥35 | 650 (72) | 281 (72) | 369 (72) | ||
| Marital status | Single | 491 (56) | 264 (68) | 227 (44) | <0.0001 |
| Married | 332 (35) | 85 (22) | 247 (48) | ||
| Divorced/Widow | 80 (9) | 41 (11) | 39 (8) | ||
| Education level | No schooling | 40 (4) | 29 (7) | 11 (2) | <0.0001 |
| Primary | 110 (13) | 86 (22) | 24 (5) | ||
| Secondary | 216 (25) | 118 (30) | 98 (19) | ||
| Grade 12 | 222 (24) | 76 (19) | 146 (28) | ||
| Tertiary | 315 (34) | 81 (21) | 234 (46) | ||
| Employed | No | 437 (51) | 259 (66) | 178 (35) | <0.0001 |
| Yes | 466 (49) | 131 (34) | 335 (65) | ||
| Receiving CSG | No | 496 (50) | 101 (26) | 395 (74) | <0.0001 |
| Yes | 407 (50) | 289 (77) | 118 (23) | ||
| Household head | Self | 520 (59) | 262 (68) | 258 (50) | <0.0001 |
| Partner/Spouse | 190 (20) | 43 (12) | 147 (29) | ||
| Parents | 55 (12) | 24 (6) | 86 (17) | ||
| Relatives | 74 (9) | 52 (14 | 22 (4) | ||
| Household income (monthly) | <USD 52.51 | 489 (55) | 259 (66) | 230 (45) | <0.0001 |
| USD 52.51–USD 262.60 | 204 (23) | 109 (28) | 95 (19) | ||
| USD 262.60–USD 525.20 | 210 (22) | 22 (6) | 188 (37) | ||
| >USD 525.20 | 0 (0) | 0 (0) | 0 (0) | ||
| Source of energy | Electricity | 888 (98) | 378 (97) | 510 (99) | <0.0001 |
| Other | 15(2) | 12 (3) | 3 (1) | ||
| Refrigerator use | No | 390 (36) | 251 (64) | 139 (8) | <0.0001 |
| Yes | 513 (64) | 43 (36) | 470 (92) | ||
| Access to water | No | 20 (3) | 20 (5) | 2 (0) | <0.0001 |
| Yes | 880 (97) | 370 (95) | 510 (100) |
| Variables | Categories | All n (%) | Rural n (%) | Urban n (%) | Chi-Square/Fisher Exact Test p |
|---|---|---|---|---|---|
| Age (years) | 6–9 | 460 (58) | 283 (73) | 222 (43) | <0.0001 |
| ≥10 | 398 (42) | 107 (27) | 291 (56) | ||
| Child sex | Boys | 441 (50) | 206 (53) | 235 (46) | <0.0001 |
| Girls | 390 (50) | 184 (47) | 206 (54) | ||
| Learning phases | Foundation | 526 (61) | 302 (77) | 224 (44) | <0.0001 |
| Intermediate | 297 (39) | 88 (23) | 289 (56) | ||
| Underweight | Yes | 45 (10) | 40 (17) | 5 (2) | <0.0001 |
| Stunting | Yes | 93 (12) | 77 (20) | 16 (3) | <0.0001 |
| Thinness | Yes | 116 (18) | 95 (28) | 21 (7) | <0.0001 |
| Overweight/obesity | Yes | 194 (24) | 55 (19) | 139 (28) | <0.0001 |
| Rural | Urban | |||||
|---|---|---|---|---|---|---|
| Variables Categories | Stunting p n (%) | Thinness p n (%) | Ov/Ob p n (%) | Stunting p n (%) | Thinness p n (%) | Ov/Ob p n (%) |
| Marital status (p) | 0.995 | 0.539 | 0.959 | 0.347 | 0.856 | 0.706 |
| Single | 52 (20) | 67 (30 | 37 (19) | 6 (3) | 10 (6) | 65 (30) |
| Married | 17 (20) | 17 (23) | 12 (18) | 10 (4) | 9 (5) | 65 (27) |
| Divorced/Widow | 8 (21) | 11 (31) | 6 (20) | 0 (0) | 2 (7) | 9 (24) |
| Education level (p) | 0.320 | 0.824 | 0.989 | 0.476 | 0.857 | 0.989 |
| No schooling | 8 (28) | 8 (31) | 3 (14) | 1 (9) | 1 (13) | 3 (30) |
| Primary | 14 (17) | 18 (19) | 13 (19) | 1 (4) | 1 (6) | 23 (30) |
| Secondary | 18 (16) | 27 (27) | 17 (19) | 5 (5) | 5 (7) | 93 (30) |
| Grade 12 | 19 (25) | 22 (33) | 10 (19) | 3 (2) | 6 (5) | 39 (28) |
| Tertiary | 18 (23) | 20 (29) | 12 (20) | 6 (3) | 8 (5) | 62 (27) |
| Employed (p) | 0.815 | 0.249 | 0.849 | 0.444 | 0.969 | 0.020 |
| No | 52 (20) | 68 (30) | 35 (18) | 7 (4) | 8 (6) | 37 (22) |
| Yes | 25 (19) | 27 (24) | 20 (19) | 9 (3) | 13 (6) | 102 (32) |
| Receive CSG (p) | 0.134 | 0.203 | 0.365 | 0.161 | 0.029 | 0.961 |
| No | 5 (25) | 9 (23) | 18 (22) | 10 (3) | 12 (4) | 108 (28) |
| Yes | 52 (18) | 76 (30) | 37 (17) | 6 (5) | 9 (10) | 31 (28) |
| H. income/month (p) | 0.158 | 0.034 | 0.542 | 0.576 | 0.122 | 0.186 |
| <USD 52.51 | 52 (20) | 68 (30) | 35 (18) | 9 (4) | (5) | 54 (24) |
| USD 52.51–USD 262.60 | 24 (22) | 27 (28) | 14 (17) | 3 (3) | 7 (11) | 30 (34) |
| USD 262.60–USD 525.20 | 1 (5) | 0 (0.0) | 6 (27) | 4 (2) | 5 (4) | 55 (30) |
| Setting | OR (95% CI) | p | AOR (95% CI) | p |
|---|---|---|---|---|
| Stunting | ||||
| No | 1 | 1 | ||
| Yes | 0.13 (0.07–0.23) | ≤0.0001 | 0.33 (0.13–0.87) | 0.024 |
| Underweight | ||||
| No | 1 | 1 | ||
| Yes | 0.15 (0.09–0.25) | ≤0.0001 | 0.16 (0.06–0.42) | ≤0.0001 |
| Thinness | ||||
| No | 1 | |||
| Yes | 0.11 (0.04–0.29) | ≤0.0001 | (collinearity) | |
| Overweight/obesity | ||||
| No | 1 | |||
| Yes | 1.72 (1.21–2.44) | 0.003 | (Collinearity) |
| Malnutrition Indicator | OR (95% CI) | p | AOR (95% CI) | p |
|---|---|---|---|---|
| Stunting | ||||
| Sex | ||||
| Girls | 1 | 1 | ||
| Boys | 0.41 (0.25–0.69) | 0.001 | 0.53 (0.30–0.94) | 0.029 |
| Learning grades | ||||
| Foundation phase | 1 | 1 | ||
| Intermediate phase | 8.63 (4.95–1506) | ≤0.0001 | 7.87 (4.48–13.82) | ≤0.0001 |
| Malnutrition Indicator | OR (95% CI) | p | AOR (95% CI) | p |
|---|---|---|---|---|
| Thinness | ||||
| CSG | ||||
| No | 1 | 1 | ||
| Yes | 2.64 (1.07–6.50) | 0.034 | 2.49 (0.90–6.86) | 0.078 |
| Household income/month | ||||
| <USD 52.51 | 1 | 1 | ||
| USD 52.51–USD 262.60 | 2.79 (0.99–7.88) | 0.052 | 2.89 (1.01–8.24) | 0.047 |
| USD 262.60–USD 525.20 | 0.76 (0.25–2.33) | 0.636 | 1.18 (0.32–3.91 | |
| Overweight/Obesity | ||||
| Sex | ||||
| Girls | 1 | 1 | ||
| Boys | 0.80 (0.54–1.19) | 0.264 | 0.81 (0.54–1.20) | 0.289 |
| Household income/month | ||||
| <USD 52.51 | 1 | 1 | ||
| USD 52.51–USD 262.60 | 1.80 (1.03–3.12) | 0.038 | 1.80 (1.02–3.10) | 0.042 |
| USD 262.60–USD 525.20 | 1.35 (0.87–2.09) | 0.177 | 1.35 (0.87–2.09) | 0.177 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hlahla, M.O.; Kunene, L.A.; Mphekgwana, P.M.; Madiba, S.; Monyeki, K.D.; Modjadji, P. Comparison of Malnutrition Indicators and Associated Socio-Demographic Factors among Children in Rural and Urban Public Primary Schools in South Africa. Children 2023, 10, 1749. https://doi.org/10.3390/children10111749
Hlahla MO, Kunene LA, Mphekgwana PM, Madiba S, Monyeki KD, Modjadji P. Comparison of Malnutrition Indicators and Associated Socio-Demographic Factors among Children in Rural and Urban Public Primary Schools in South Africa. Children. 2023; 10(11):1749. https://doi.org/10.3390/children10111749
Chicago/Turabian StyleHlahla, Mosebudi Olga, Lindy Agatha Kunene, Peter Modupi Mphekgwana, Sphiwe Madiba, Kotsedi Dan Monyeki, and Perpetua Modjadji. 2023. "Comparison of Malnutrition Indicators and Associated Socio-Demographic Factors among Children in Rural and Urban Public Primary Schools in South Africa" Children 10, no. 11: 1749. https://doi.org/10.3390/children10111749





