Abstract
Several crimes in South Africa cause physical, economic, and mental problems. Xenophobic attacks, mob justice, and other violent conduct directly traumatise children. Service delivery riots and physical and sexual abuse are examples. This evaluation evaluates childhood trauma and exposure to violence interventions. The review describes the therapeutic methods for traumatised children exposed to violence, the healthcare professionals administering them, and the strategies used to tailor the interventions. The researcher systematically searched PsycINFO, Google Scholar, PubMed, Science Direct, and EBSCOhost. Literature from 2011 to 31 July 2023 was searched, and 19 papers were chosen for further review after the systematic search. The authors conducted an eligibility evaluation according to PRISMA guidelines. A thorough review of article texts identified 19 papers that met eligibility standards. Only nineteen studies have validated trauma and violence therapies for children. An effective multi-phased intervention that is feasible and adaptable to varied socioeconomic backgrounds is needed. Further studies on the mental health benefits of brief trauma intervention treatment are needed.
1. Introduction
According to the World Health Organization [1], children from 6 to 17 years are exposed to trauma and violence, which are pervasive public health issues in South Africa. In contrast to other African nations affected by war and natural disasters, the rates of trauma exposure among children are shockingly high [2]. Thus, 98% of South Africans are exposed to community violence, and sexual abuse amongst minors accounts for 54.2%, with increased rates of comorbidity noted [3]. In one study, nearly all adolescents with PTSD had comorbid disorders, predominantly dysthymic disorder and major depression [4]. Violence and trauma increase the risk of mental diseases, including post-traumatic stress disorder [5].
The prevalence of PTSD has been reported among poor urban adolescents. Childhood exposure to trauma and violence increases the probability of developing depression, anxiety, sleeping disorders, PTSD, and eating disorders [6]. Violence can be encountered through direct or indirect means. Direct exposure to violence pertains to the experience of being personally victimised [7]. Indirect exposure to violence, also known as vicarious exposure, relates to the observation, either directly or indirectly, of another individual being victimised [8]. Whether encountered firsthand or indirectly, violence manifests in various manifestations, encompassing physical, emotional, psychological, sexual, and verbal dimensions [9].
Irrespective of one’s victim, witness, or attacker role, empirical studies indicate that violence often leads to detrimental consequences. These consequences encompass a range of distressing experiences and maladaptive outcomes, both in the immediate aftermath and over an extended period [10].
According to research, 22.2% to 23.6% of minors have mental health issues [11]. Physical and emotional abuse, neglect, familial violence, and other forms of child abuse were strongly associated with sexual abuse [12]. The violence against minors, including sexual assault, domestic violence, and community violence, is abhorrent [13].
Child trauma and exposure to violence are strongly associated with drug abuse and potential dependence as a coping mechanism in adulthood [5,8,14]. Childhood trauma can profoundly affect adolescents’ mental health [11]. Furthermore, it has been found that childhood trauma and exposure to violence predict anxiety and depression later in life [14,15]. This is evidence that childhood trauma and exposure to violence is a particularly severe form of maltreatment, consistent with a larger body of research concerning “adverse childhood experiences” [16].
This issue may result in various disabling and expensive problems that pose difficulties throughout one’s lifetime. According to the World Health Organization [17], child trauma and exposure to violence are atypical experiences.
Due to the burden of care experienced at the community level, programmes encompass various initiatives that provide information, training, and skills development facilitated by non-governmental organisations (NGOs) and healthcare clinics. The utilisation of community health workers (CHWs) and lay counsellors as a means of addressing the scarcity of adequately educated healthcare professionals in the mental health field is a progressively favoured approach.
Evidence indicates that the accessibility of mental health treatments is limited in the Southern African region, as the number of mental health professionals per 100,000 individuals ranges from 0.05 to 1.52, in contrast to the estimated figure of 9.9 in Europe [17]. Children and adolescents in low–middle-income countries have a lower treatment prevalence of 159 compared to 664 adults per 100,000 population, according to the WHO [1].
The primary objective of this systematic review is to ascertain various interventions available for addressing African children’s mental health within community settings. Additionally, this research emphasises the self-reported barriers therapists encounter in implementing these interventions.
2. Methodology
The data were initially encoded to investigate aspects that are associated with the purpose of the study, including the type of intervention used, the degree of context that was addressed, and the reported mechanisms for successful implementation. Through induction, several supplementary codes were identified, encompassing various aspects such as psychological conditions linked to the intervention, the specific site where the intervention was implemented, and the individuals responsible for providing the intervention.
2.1. Search Strategy
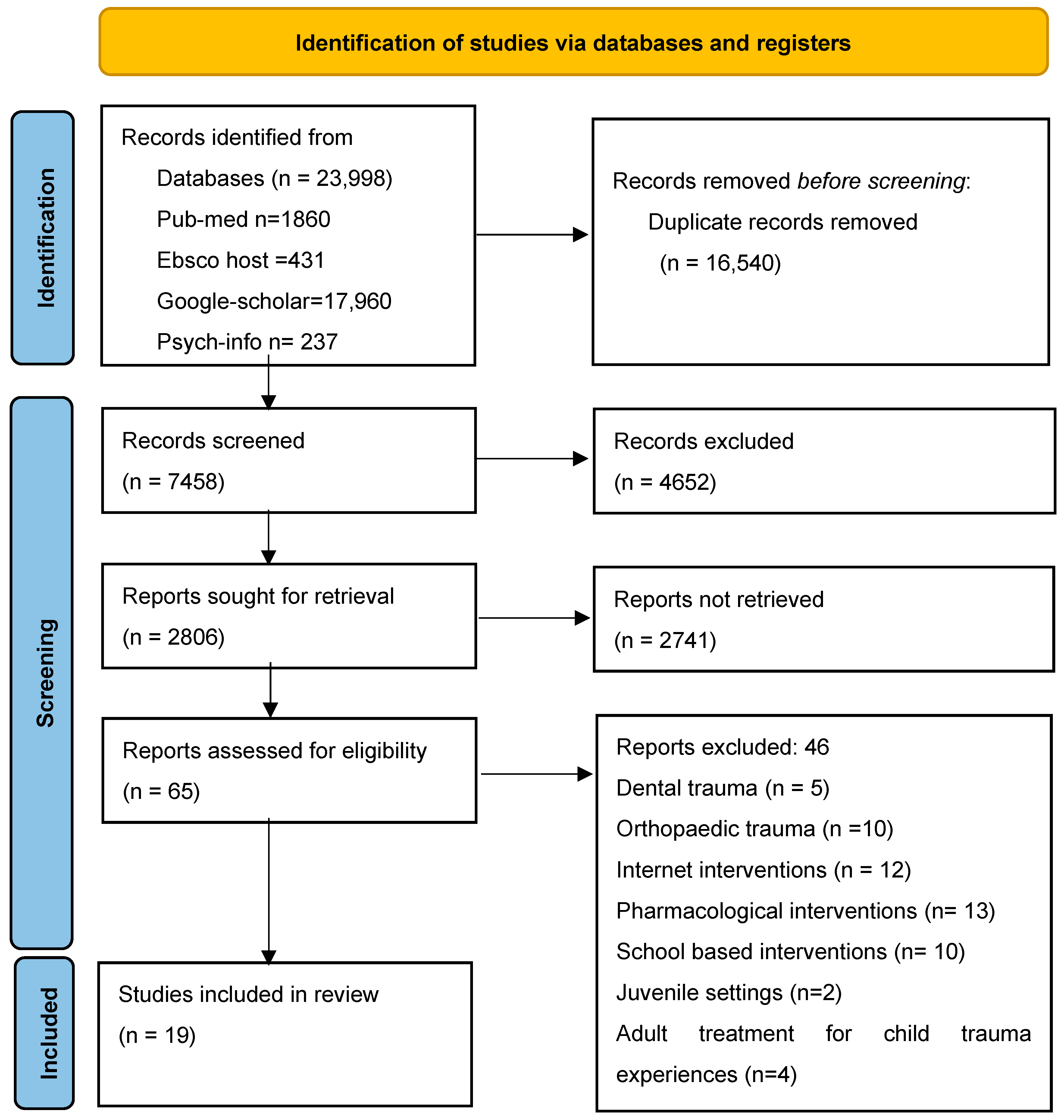
The study commenced by identifying 23,998 studies conducted between 1 January 2011 and 31 July 2023, sourced from PsycINFO, PubMed, Science Direct, Google Scholar, and EBSCOhost. To ensure the quality and relevance of the selected studies, the inclusion criteria were limited to peer-reviewed articles written in English. To refine the search effectively, the researchers employed a Boolean search strategy, a structured technique that permits users to combine or exclude terms to enhance search precision [18]. The Boolean search phrases were “Childhood and Trauma And Intervention” and “Childhood And Exposure To Violence And Intervention” (See Table 1). The initial database search yielded a total of 23,998 articles distributed across various sources, as follows: PubMed (1860), EBSCOhost (431), Science Direct (2987), Google Scholar (17,960), and PsycINFO (237). Subsequently, a systematic process was undertaken to filter and eliminate redundant and irrelevant articles. Initially, 16,540 duplicate entries were removed. Additionally, 4652 articles were eliminated through automated means, leaving a core set of 2806 articles for further scrutiny.

Table 1.
Databases, used index terms, and Boolean search words.
The subsequent phase involved a meticulous review of these 2806 articles. Three authors, PT, LM, and AM, independently assessed the articles based on their titles. Following this initial screening, 65 articles were selected for further evaluation, where the authors scrutinised the abstracts. Finally, a comprehensive full-text review was conducted for these 65 selected articles to determine their suitability for inclusion in the study. Upon completing the full-text review, 46 articles were excluded from the study due to a lack of relevance or non-compliance with the specified inclusion criteria. The rationales for exclusion encompassed articles that concentrated on topics such as dental trauma, orthopaedic trauma, internet-based interventions, pharmacological interventions, school interventions, juvenile settings, adult treatments for childhood trauma, geographic factors, mental illness, study design, or result criteria. Ultimately, the rigorous selection process included 19 articles (as presented in Figure 1) that met the established criteria and were deemed pertinent to the study’s objectives.
Figure 1.
Prisma flow chart [19].
2.2. Inclusion Criteria
The researcher focused on the specific population of children exposed to trauma and violence who have been seen at healthcare facilities or trauma facilities for trauma intervention. Furthermore, the focus intervention of interest was childhood trauma intervention used to treat children exposed to trauma and violence. The study setting included any trauma or healthcare facilities from low- or high-income countries. The language of the articles reviewed was English. The review focused on papers that were addressing children aged 6–17 years of age. The review also focused on papers published from 2011 to 31 July 2023.
2.3. Exclusion Criteria
The studies that were excluded are those that addressed sexual abuse in isolation or specifically sexual abuse as one type of trauma. Most of the studies were excluded if the focus was on clinical diagnoses, such as depression or anxiety, with no history of trauma. Most of the studies were excluded if they only addressed children with behavioural problems with no subsequent trauma, juvenile medical settings, or the social services placements of children with trauma. Studies not conducted in a healthcare setting or by healthcare professionals were excluded. Studies focused on intellectual disability, substance abuse, or neurological problems were excluded. Irrelevant interventions, such as pharmacological interventions, were excluded. Interventions that addressed trauma-related medical examinations (i.e., brain injuries) were also excluded.
2.4. Data Extraction and Quality Assessment
For inter-researcher dependability, two authors (LM, AM) assessed the four papers to confirm data extraction uniformity. The remaining eight articles were split and removed. Author, date, geographic context, study population characteristics, sample size, intervention objective and design, mental disorder targeted, outcomes, results, and implementation facilitators and barriers were important. The essential data fundamentals that were abstracted from different studies were details about trauma-focused treatments aimed at children from 6 to 17 years and treatment outcomes. Details about treating possible mental health challenges and behavioural challenges due to trauma and exposure to violence amongst children were also abstracted. Finally, whether or not the main results of the studies indicated positive outcomes were recorded. Successful and ineffective interventions were included. Analysis of the extracted data was deductive and inductive. To investigate the study objective, trauma intervention, context addressed, and implementation mechanisms were coded. This study team (PT, LM, and AM) compared codes and cross-checked publications with uncertainty.
A critical appraisal checklist was used to assist the researcher in systematically assessing the reliability, relevance, and results to be issued. A critical appraisal checklist was used to assist the researcher in systematically assessing the trustworthiness, relevance, and results to be published [20]. The researchers utilised the CASP critical appraisal tool that consisted of ten questions. The questions were divided into three sections scored as “yes, can’t tell and no”. For each article appraised, the score was on a scale of 0–10 points by counting how many “yes”, “can’t tell”, or “no” responses there were. The articles that scored more than five “yes” responses were evaluated (See Table 2).

Table 2.
CASP for selected studies.
Of the nineteen studies selected, there were (n = 19) studies in the field under investigation that provided information regarding the outcomes of their interventions. Out of the total of 19 research studies examined, 3 of the studies indicated that TF-CBT was shown to be more feasible to train counsellors on. Three (3) studies on the different interventions used indicated positive results when used amongst children with TF-CBT. Four studies yielded statistically significant impact sizes, but the other two, randomised controlled trials (RCTs), showed non-significant effect sizes. The two systematic reviews indicated the need for a multimodal feasible intervention in one of the randomised controlled trials (RCTs) under consideration. The other indicated the positive impact of TF-CBT on treating children affected by trauma.
2.5. Characteristics of Included Studies and CASP Appraisal
The critical appraisal method was followed, explained as a procedure to carefully and systematically investigate research to critique its trustworthiness, value, and significance. The critical appraisal process involves selecting literature carefully and systematically as a tool that will be utilised for data analysis to assist the researcher in summarising the evidence found to judge its trustworthiness [40]. In applying the critical appraisal method, the researcher considered psychosocial interventions to manage trauma and exposure to violence among children (Table 3).

Table 3.
Critical appraisal table.
3. Methods
Based on the final search results, 19 papers were chosen as suitable for inclusion in the review. The majority of these papers were characterised by a quantitative [11] research approach with two qualitative studies [24,26], three systematic reviews [21,23,32], and two case studies [28]. According to Clarke [41], when there is significant variation in methodology, a systematic review can leave the findings of the studies to derive an average estimate. Consequently, the present study employed narrative synthesis to synthesise the data, employing thematic analysis as the analytical approach [42]. Textual analysis has been conceptualised as a technique for detecting, analysing, and reporting patterns or themes and searching for meaning within literature or data [43,44]. This study employed a six-step process for synthesising data through thematic analysis to identify recurring themes [45]. These steps included becoming acquainted with the data, creating initial (sub) codes, identifying (sub) themes, reviewing (sub) themes, and organising ideas or issues through charting [45].
3.1. Results
The thematic analysis yielded four themes (see Table 4), including “Effectiveness of childhood trauma intervention” [21,22,23,24,25,26,27,28,29], “Impact of trauma intervention” [22,26,28,29], “Barriers and facilitators of trauma” [24,25,29], “Coping strategies of children exposed to trauma” [21,22,24], and “Psychological burden of trauma” [22,26,27,29]. Table 5 provides key interventions reported to bear positive outcomes regarding childhood trauma management.

Table 4.
Themes emerging from selected studies.

Table 5.
Results.
3.2. The Effectiveness and Impact of Trauma Intervention
PFA may be used for post-disaster therapies despite limited evidence. The iatrogenic effects of Critical Incident Stress Debriefing in adults render PFA unproven. PFA research is very early. Thus, while unlikely, negative impacts on children’s psychological functioning may still be found in Gilbert et al. [21]. The pilot intervention reduced PTSD and depression symptoms, although Woollett et al. [22] noted other benefits. Behavioural problems decreased. They understood, expressed, and controlled emotions through art and play. Finally, children and adolescents benefit from high-quality, systematic mindfulness therapy. These findings, paired with well-studied adult therapy, may reduce childhood trauma-related health problems. Ortiz et al. [23]. The lay counsellors stressed the necessity of Trauma-Focused Cognitive Behavioural Therapy (TF-CBT) in their community and cultural, belief, and socioeconomic sensitivity when working with participants. The authors also emphasised the importance of collaborating with various entities to effectively tackle socioeconomic obstacles [24]. The present study was unable to incorporate a comparison or waiting control group. The absence of a control group introduces ambiguity regarding the attribution of the outcomes to the specific components of TF-CBT or to non-specific factors such as the passage of time, the level of participation from the therapist, or the expectations associated with the treatment. This was further reiterated by [32], who indicated that three common problems in their findings were small sample sizes, the lack of a control group, and the lack of long-term follow-up. The examination of therapist–client relationships was not conducted in this study. These factors may have exerted an influence on results in conjunction with the impact of the treatment model. Therapists who conducted patient evaluations may have exhibited bias. The limited size of the sample hinders the ability to make generalisations [26].
Tabone et al. [27] examined CANS-ARC mapping in community-based clinical settings. The ARC framework and CANS assessed various traumatic symptoms in children and linked them to treatment planning and adjustment. After controlling for gender, race, age, guardianship, and service sites, the study indicated that children’s trauma-related symptoms improved considerably in all outcome categories. In their investigations, Fazel et al. [28] found that narrative exposure therapy (NET) is a child-specific therapy with expanding data. Lay or professional therapists tried it on refugees and asylum seekers in low, moderate, and high-income contexts. NET (or the child “KIDNET” version) therapy trials for PTSD in refugee children reveal that it is effective, scalable, and culturally adjustable. Dorsey et al. [29] found that TF-CBT can help children with PTS who lost a parent. However, results may vary. TF-CBT outperformed conventional care after therapy in urban Kenya, rural Kenya, and urban Tanzania, but not rural Tanzania. The 12-month follow-up showed condition discrepancies only in Kenya’s urban and rural districts. Secondary outcomes showed that TF-CBT had the greatest impact for rural Kenyan children after treatment and at 12 months for urban and rural Kenyan children.
3.3. Trauma Intervention Implementation
Kenyans and Tanzanians may have faced different hardships and adversity. Kenyan children and guardians had lower health, food deprivation, and higher stress. National statistics may have helped Kenyan children with typical care maintain symptoms during implementation [29]. Psychologists performed weekly online surveys documenting TF-CBT sessions with children and caregivers during the trauma intervention [26]. Psychologists recorded the following for each session: TF-CBT component(s) addressed, techniques/activities employed, skills taught, session length, barriers/challenges encountered, and next-session plans. Psychologists received self-reported feedback on treatment regimen compliance. To verify treatment model conformity, psychologists presented their TF-CBT cases during group consultation calls and received comments. This trauma profile matches childhood adversity in other low- and middle-income nations and is expected to be numerous [29]. Note the strong caregiver participation in treatment. TF-CBT relies on caregiver participation, which might be difficult in school-based child mental health treatment. Woollett et al. [22] used Art and play therapy with TF-CBT to produce a structured and client-led session. “Psychoeducation and parenting skills; Relaxation skills; Affective regulation abilities; Cognitive coping skills; Trauma narrative and cognitive processing of traumatic event(s) (PRACTICE); “In vivo mastery of trauma reminders; Conjoint child-parent sessions; and Enhancing safety and future developmental trajectory” constitute the TF-CBT acronym PRACTICE.
3.4. Barriers and Facilitators of Trauma
In a study conducted by Woods-jager et al. [24], Counsellors also discussed the difficulties in getting participants to articulate their feelings, noting that feelings are often unrecognised in their culture (for example, “Sometimes even sadness does not have a label in their language”). Counsellors pointed out that discussing death or speaking badly of the departed is usually not culturally acceptable. Steward et al. [26] indicated that the evaluators were the same therapists treating the patients, which could have created bias. Finally, the findings need to be more generalisable to other populations due to the small sample size. Witnessing participants’ unmet social and economic needs was noted as something that weighed on some counsellors and made TF-CBT implementation challenging at times [24]. According to Meetken et al. [25], it is an organised eight-phase technique to deal with the traumatic memory’s past, present, and future elements. During the sessions, a child is asked to choose a memory from a past hospitalisation that is currently the most traumatic to them. The painful thoughts are desensitised through regulated rhythmic eye motions, and pleasant and optimistic thoughts are programmed.
3.5. The Psychological Burden of Trauma in Children
According to Woollett et al. [22], violence harms children, affecting their mental, physical, and social well-being. Meta-analyses show that youth violence increases internalising and externalising difficulties. Steward et al. [26] also highlight El Salvador’s early challenges. Most children (90.7%) had experienced multiple stressful events. Most children experienced index traumas of domestic violence, physical abuse, and sexual abuse [26]. Trauma causes post-traumatic stress and other childhood mental and behavioural issues. Extensive literature relates childhood trauma to adult psychopathology and disability [44]. Childhood traumatic events cause mental distress in many persons who need mental health services, and the severity, frequency, and breadth of unpleasant experiences affect mental health. Childhood trauma is strongly linked to adult psychosis [11]. Ethnic minorities and the poor also endure more trauma. Most children (90.7%) had experienced multiple stressful events. Most children in the study encountered primary traumas such as domestic violence, physical abuse, and sexual abuse. This trauma pattern aligns with childhood adversity experiences observed in other low- and middle-income nations [29]. It is also consistent with expectations, given the prevalent exposure to armed conflicts, gang-related violence, and high homicide rates in many Central American countries [26,31]. It is important to note that employing standardised assessment data has its limitations. This is because attempting to condense the diverse challenges traumatised children face into a single diagnosis, such as post-traumatic stress disorder, may lead to misclassification or result in the assignment of multiple unrelated disorders [27].
3.6. Coping Strategies of Children Exposed to Trauma and Violence
Trauma exposure in early childhood may affect youth coping behaviours. Trauma may affect emotional and behavioural consequences by affecting coping skills. Self-portraits were used to examine coping resources and how children saw themselves and others. A comprehensive “Safe Place” fostered active conversation and planning [27]. Exposure to violence can result in sorrow, anxiety, thoughts of suicide, difficulties in peer relationships, and academic challenges [32]. Coping techniques are frequently integrated into social–emotional learning curricula, including school-based initiatives, and some have resulted in notable improvements in children’s well-being and academic performance from their early years through high school [33]. Vaughn-Coaxum et al. [33] underscore the significance of intervening during the school years when coping skills may be especially amenable to change. Wollet et al. [22] identify a practice guide that emphasises interventions to help children cope: “Psychoeducation and Parenting skills; Relaxation skills; Affective regulation skills; Cognitive coping skills; Trauma narrative and cognitive processing of the traumatic event(s); Conjoint child-parent sessions; In-person mastery of trauma reminders; and Improving safety and future development.”. PFA’s modularity is a benefit. Each module targets a distinct therapeutic aim (e.g., self-efficacy, coping skills, safety, connectivity) [21]. The first four groups taught children and guardians behavioural and cognitive coping techniques for parental loss and bereavement [24].
Table 5 illustrates that recent research has consistently demonstrated favourable results for children exposed to trauma through a range of therapeutic approaches, such as TF-CBT, child-centred play therapy, art-based therapy, narrative therapy, and psychoeducation [24,28,35,36,37,38,39].
4. Discussions
This review’s results indicated the limited research interventions conducted amongst children exposed to trauma and violence. The results obtained in this research offer validation for the suitability and acceptability of TF-CBT as an effective treatment method for enhancing the mental well-being of children. This aligns with Woollett et al. [22], who emphasised the significance of comprehending the strategies employed by non-specialist counsellors to ensure that the treatment remains culturally and socioeconomically relevant to the participants. This insight can inform the implementation of future Evidence-Based Treatments (EBTs) in an African context. Furthermore, these findings are corroborated by Copeland et al. [46], who reported that there was limited utilisation of mental health services by children and adolescents in programs not specifically designed for them. Moreover, the research underscores the importance of assessing interventions’ validity and cultural appropriateness in such contexts. Firstly, while the frequency of traumatic events is higher in post-conflict nations, the disparity of traumatic event categories differs significantly by location [47]. These findings reveal the effect of the socio-political and socio-economical context on the distribution of traumatic experiences [48]. Finally, we looked at new research suggesting how traumatic event exposure is becoming increasingly crucial in developing child mental health disorders. Most articles use more adopted interventions and lack cultural adaptability; however, according to Katsonga-Phiri [32], there is a significant increase in interventions adapted with input from community experts and local people regarding language and cultural relatability. The review further identified promising 21st-century therapies, particularly those utilising cognitive behavioural methods and cultural adaptations [32]. As indicated, both the methodology and results of adaptations should be documented and published to further this rapidly expanding study field. Other studies indicated positive results when using the interventions cross-culturally, although the techniques might not be effective due to cultural differences and contexts. Interventions to reduce the influence of traumatic event exposure and PTSD on the emergence of child chronic mental disorders are needed to address the high and growing burden of chronic mental health disorders among children.
The review results indicated the limited research interventions conducted for children exposed to trauma and violence in an African country as more focused on youth and indicated to be between 14 and 25 years [18,32,45]. Moreover, the validity and cultural reliability of the interventions are highlighted minimally. However, Coetzer et al. [49] highlighted the need for a multimodal intervention to address the challenges children might be experiencing and also, in their findings, they indicated the need for follow-ups, which were attributed to improved symptoms [50].
According to meta-analytic studies, it has been found that children in sub-Saharan Africa have greater prevalence rates of sexual, physical, and emotional abuse compared to other regions [51]. Specifically, around 83% of male and female children record instances of emotional abuse, while 64% report incidents of physical abuse [52]. Furthermore, it has been reported that 19% of boys in this region have experienced childhood sexual abuse [53]. There is evidence to show that male children in sub-Saharan African settings may face a greater susceptibility to physical abuse [54]. However, the factors contributing to this phenomenon are not well comprehended, and it should be noted that not all research indicates disparities in abuse rates based on gender [55].
The investigation of this subject holds significant importance, especially in sub-Saharan Africa, where peri-urban people face notable challenges such as extreme material poverty, inadequate infrastructure, and environmental risks [56]. Material deprivation can impact mental well-being via mechanisms such as experiencing financial difficulties, living in deteriorated neighbourhood environments, or facing limited opportunities [57].
Individuals who endured childhood physical abuse had lower life satisfaction, especially when combined with interpersonal violence [58]. Despite global efforts to eradicate violent discipline, low-income countries still witness the physical and psychological abuse of children under five [59]. This underscores the need for research on childhood exposure to violence interventions involving caregivers [60]. Interventions should address how children and adolescents interpret parental information and whether aggressive behaviour is reactive or intentional [61].
Studies show less physical violence by adolescents against parents in families with strong cohesion but more violence in families with high conflict [62]. Healthcare practitioners must enhance their capacity to recognise and address mental health issues to secure future generations’ well-being, using validated evidence for timely interventions [63]. Further research is essential to comprehensively understand caregiver and child victimisation [64]. This can enable social workers to collaborate with families and communities for effective interventions. Community violence can foster pessimism, disrupt social bonds, alter societal norms, and exacerbate violence frequency and trauma symptoms [65].
5. Evidence-Based Recommendations
A multi-phased and multi-modal intervention that encourages participants’ emotional needs to be expressed in a fluid and flexible manner is needed, advocating for additional studies into the effects of shorter treatments that impact positive mental health outcomes.
The intervention must guide the therapist and participant while permitting self-expression and the creative mastery of complex themes. The results of this review indicate the need for an intervention advocating for greater study on the influence of shorter impactful treatments on mental health and the involvement of stakeholders who can also be psycho-educated about trauma and its effects to ensure sustainability and empowerment. A phase-based approach that integrates techniques from different interventions to ensure that it fosters flexibility and the fluid expression of participant’s emotional needs while ensuring cultural sensitivity will guide the therapist and participant while allowing self-expression and the creative mastery of complicated issues.
Advocating for further investigation on the efficacy of abbreviated therapies and their effects on mental well-being encourages self-expression and creative problem-solving while maintaining cultural sensitivity and flexibility in meeting participants’ emotional needs. While many therapies have demonstrated adaptability, there remains an issue regarding the methodologies employed and their cultural acceptability across different societies. Moreover, this analysis highlights the necessity for further investigation to inform the execution and clinical results of interventions, specifically focusing on developing and customising interventions for children who have experienced trauma and violence.
6. Conclusions
This process highlighted five topics and interventions targeting a child’s underlying mental health due to trauma and exposure to violence. Three primary themes emerged: the effectiveness and implementation of trauma interventions, trauma intervention implementation, the barriers and facilitators of trauma, the psychological burden of trauma in children, and the coping strategies of children exposed to trauma. TF-CBT is the most used and most effective intervention that yields improved symptoms in children and youth, although the youth in most studies were around 19–25 years [14,66].
Informal settlements can worsen mental health difficulties because of the swift transformations in social frameworks and the stress caused by economic insecurity [67]. The confluence of social marginalisation, limited access to official services, and pervasive unemployment can cause a complex interplay of trauma, poverty, and depression among children [68].
Cognitive behavioural therapy has been shown to work in high-income environments and in children. Nevertheless, it is essential to note that in low-income contexts, significant disparities exist in allocating resources and accessibility to mental health services [69]. Consequently, implementing conventional mental healthcare models becomes impractical in such circumstances.
The outcomes of our study indicate that cognitive behavioural therapies must address both the root causes of exposure to violence and early trauma concurrently [70].
This study has several limitations. It should be noted that systematic reviews can result in fragmented evidence, which limits their ability to give adequate research information. Because this evaluation’s eligibility requirements are sensitive, a small but focused research group was chosen—furthermore, the included studies used samples that were largely male and Caucasian. As a result, this research may not represent different nationalities, cultures, or socioeconomic circumstances. These findings are limited in generalisability and applicability beyond the indicated situations. Many factors must be considered when adapting first-world outcomes to third-world settings.
Author Contributions
P.T. was responsible for conducting the study, which included data collection through a literature search, analysis, and the writing of the manuscript. L.M. was the main supervisor of the research and was responsible for supervision, feedback, and revisions. A.M. was the co-supervisor and contributed to revisions. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no specific grant from any funding agency in the public, commercial, or non-profit sectors.
Institutional Review Board Statement
This article followed all ethical standards for research without direct contact with human or animal subjects.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data sharing does not apply to this article, as no new data were created. The data used for this study are readily available; consult the reference list.
Acknowledgments
The authors would like to thank the co-authors for their meaningful contributions and guidance.
Conflicts of Interest
The author(s) declare that they have no financial or personal relationship(s) that may have inappropriately influenced them in writing this article.
References
- WHO. Violence against Children; WHO: Geneva, Switzerland, 2022.
- Powell, B.J.; Patel, S.V.; Haley, A.D.; Haines, E.R.; Knocke, K.E.; Chandler, S.; Katz, C.C.; Seifert, H.P.; Ake, G.; Amaya-Jackson, L.; et al. Determinants of Implementing Evidence-Based Trauma-Focused Interventions for Children and Youth: A Systematic Review. Adm. Policy Ment. Health Ment. Health Serv. Res. 2020, 47, 705–719. [Google Scholar] [CrossRef] [PubMed]
- Kleber, R.J. Trauma and Public Mental Health: A Focused Review. Front. Psychiatry 2019, 10, 451. [Google Scholar] [CrossRef]
- Forke, C.M.; Myers, R.K.; Localio, A.R.; Wiebe, D.J.; Fein, J.A.; Grisso, J.A.; Catallozzi, M. Intimate Partner Violence: Childhood Witnessing and Subsequent Experiences of College Undergraduates. J. Interpers. Violence 2019, 36, NP9670–NP9692. [Google Scholar] [CrossRef] [PubMed]
- Batchelder, A.W.; Safren, S.A.; Coleman, J.N.; Boroughs, M.S.; Thiim, A.; Ironson, G.H.; Shipherd, J.C.; O’cleirigh, C. Indirect Effects From Childhood Sexual Abuse Severity to PTSD: The Role of Avoidance Coping. J. Interpers. Violence 2018, 36, NP5476–NP5495. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Pan, Y.; Liu, G.; Chen, W.; Lu, J.; Li, X. Perceived social support and self-esteem mediate the relationship between childhood maltreatment and psychosocial flourishing in Chinese undergraduate students. Child. Youth Serv. Rev. 2020, 117, 105303. [Google Scholar] [CrossRef]
- Dye, H. The impact and long-term effects of childhood trauma. J. Hum. Behav. Soc. Environ. 2018, 28, 381–392. [Google Scholar] [CrossRef]
- Dubé, C.; Gagné, M.-H.; Clément, M.; Chamberland, C. Community Violence and Associated Psychological Problems Among Adolescents in the General Population. J. Child Adolesc. Trauma 2018, 11, 411–420. [Google Scholar] [CrossRef]
- Xavier, A.; Cunha, M.; Pinto-Gouveia, J. The Indirect Effect of Early Experiences on Deliberate Self-Harm in Adolescence: Mediation by Negative Emotional States and Moderation by Daily Peer Hassles. J. Child Fam. Stud. 2015, 25, 1451–1460. [Google Scholar] [CrossRef]
- Rivara, F.; Menestrel, S.L. Preventing Bullying: Through Science, Policy and Practice; The National Academic Press: Washington, DC, USA, 2016. [Google Scholar]
- Naz, S.; Sulman, N. Mother And Father’s Behavioral Practices Towards Children With And Without Intellectual Disability Disorder (IDD). Pak. J. Gend. Stud. 2019, 18, 179–192. [Google Scholar] [CrossRef]
- Wittbrodt, M.T.; Moazzami, K.; Lima, B.B.; Alam, Z.S.; Corry, D.; Hammadah, M.; Campanella, C.; Ward, L.; Quyyumi, A.A.; Shah, A.J.; et al. Early childhood trauma alters neurological responses to mental stress in patients with coronary artery disease. J. Affect. Disord. 2019, 254, 49–58. [Google Scholar] [CrossRef]
- Sweeney, A.; Taggart, D. (Mis)understanding trauma-informed approaches in mental health. J. Ment. Health 2018, 27, 383–387. [Google Scholar] [CrossRef] [PubMed]
- Hatcher, A.M.; Gibbs, A.; Jewkes, R.; McBride, R.-S.; Peacock, D.; Christofides, N. Effect of Childhood Poverty and Trauma on Adult Depressive Symptoms Among Young Men in Peri-Urban South African Settlements. J. Adolesc. Health 2018, 64, 79–85. [Google Scholar] [CrossRef] [PubMed]
- Allen, J.J.; Anderson, C.A. Aggression and Violence: Definitions and Distinctions. The Wiley Handbook of Violence and Aggression; John Wiley & Sons: New York, NY, USA, 2017. [Google Scholar] [CrossRef]
- Brown, R.C.; Witt, A.; Fegert, J.M.; Keller, F.; Rassenhofer, M.; Plener, P.L. Psychosocial interventions for children and adolescents after man-made and natural disasters: A meta-analysis and systematic review. Psychol. Med. 2017, 47, 1893–1905. [Google Scholar] [CrossRef]
- WHO. Violence against Children; WHO: Geneva, Switzerland, 2020.
- Chen, B.; Cao, J.; Luo, Y.; Rutkowski, L. Asymptotic Output Tracking of Probabilistic Boolean Control Networks. IEEE Trans. Circuits Syst. I Regul. Pap. 2020, 67, 2780–2790. [Google Scholar] [CrossRef]
- Liberati, A.; Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 151, W-65–W-94. [Google Scholar] [CrossRef] [PubMed]
- Al-Jundi, A. Critical Appraisal of Clinical Research. J. Clin. Diagn. Res. 2017, 11, JE01–JE05. [Google Scholar] [CrossRef]
- Gilbert, R.; Abel, M.R.; Vernberg, E.M.; Jacobs, A.K. The Use of Psychological First Aid in Children Exposed to Mass Trauma. Curr. Psychiatry Rep. 2021, 23, 53. [Google Scholar] [CrossRef]
- Woollett, N.; Bandeira, M.; Hatcher, A. Trauma-informed art and play therapy: Pilot study outcomes for children and mothers in domestic violence shelters in the United States and South Africa. Child Abus. Negl. 2020, 107, 104564. [Google Scholar] [CrossRef]
- Ortiz, R.; Sibinga, E.M. The Role of Mindfulness in Reducing the Adverse Effects of Childhood Stress and Trauma. Children 2017, 4, 16. [Google Scholar] [CrossRef]
- Woods-Jaeger, B.A.; Kava, C.M.; Akiba, C.F.; Lucid, L.; Dorsey, S. The art and skill of delivering culturally responsive trauma-focused cognitive behavioral therapy in Tanzania and Kenya. Psychol. Trauma Theory Res. Pract. Policy 2017, 9, 230–238. [Google Scholar] [CrossRef]
- Meentken, M.G.; van Beynum, I.M.; Aendekerk, E.W.C.; Legerstee, J.S.; El Marroun, H.; van der Ende, J.; Lindauer, R.J.L.; Hillegers, M.H.J.; Moll, H.A.; Helbing, W.A.; et al. Eye movement desensitization and reprocessing (EMDR) in children and adolescents with subthreshold PTSD after medically related trauma: Design of a randomized controlled trial. Eur. J. Psychotraumatology 2018, 9, 1536287. [Google Scholar] [CrossRef]
- Stewart, R.W.; Orengo-Aguayo, R.; Villalobos, B.T.; Nicasio, A.V.; Dueweke, A.R.; Alto, M.; Cohen, J.A.; Mannarino, A.P.; de Arellano, M.A. Implementation of an Evidence-Based Psychotherapy for Trauma-Exposed Children in a Lower-Middle Income Country: The Use of Trauma-Focused Cognitive Behavioral Therapy in El Salvador. J. Child Adolesc. Trauma 2020, 14, 433–441. [Google Scholar] [CrossRef] [PubMed]
- Tabone, J.K.; Rishel, C.W.; Hartnett, H.P.; Szafran, K.F. Trauma-Informed Intervention with Children: Integrating the CANS Assessment with the ARC Framework in a Clinical Setting. J. Child Adolesc. Trauma 2021, 15, 65–74. [Google Scholar] [CrossRef]
- Fazel, M.; Stratford, H.J.; Rowsell, E.; Chan, C.; Griffiths, H.; Robjant, K. Five Applications of Narrative Exposure Therapy for Children and Adolescents Presenting With Post-Traumatic Stress Disorders. Front. Psychiatry 2020, 11, 19. [Google Scholar] [CrossRef] [PubMed]
- Dorsey, S.; Lucid, L.; Martin, P.; King, K.M.; O’Donnell, K.; Murray, L.K.; Wasonga, A.I.; Itemba, D.K.; Cohen, J.A.; Manongi, R.; et al. Effectiveness of task-shifted trauma-focused cognitive behavioral therapy for children who experienced parental death and posttraumatic stress in Kenya and Tanzania: A randomized clinical trial. JAMA Psychiatry 2020, 77, 464–473. [Google Scholar] [CrossRef] [PubMed]
- Danielson, C.K.; McCart, M.R.; Walsh, K.; de Arellano, M.A.; White, D.; Resnick, H.S. Reducing substance use risk and mental health problems among sexually assaulted adolescents: A pilot randomized controlled trial. J. Fam. Psychol. 2012, 26, 628–635. [Google Scholar] [CrossRef]
- Deblinger, E.; Mannarino, A.P.; Cohen, J.A.; Runyon, M.K.; Steer, R.A. Trauma-focused cognitive behavioral therapy for children: Impact of the trauma narrative and treatment length. Depress. Anxiety 2010, 28, 67–75. [Google Scholar] [CrossRef]
- Katsonga-Phiri, T.; Grant, K.E.; Brown, M. Trauma Intervention in Sub-Saharan African Children: A Systematic Literature Review. Trauma Violence Abus. 2017, 20, 453–469. [Google Scholar] [CrossRef]
- Lokuge, K.; Shah, T.; Pintaldi, G.; Thurber, K.; Martínez-Viciana, C.; Cristobal, M.; Palacios, L.; Dear, K.; Banks, E. Mental health services for children exposed to armed conflict: Médecins Sans Frontières’ experience in the Democratic Republic of Congo, Iraq and the occupied Palestinian territory. Paediatr. Int. Child Health 2013, 33, 259–272. [Google Scholar] [CrossRef]
- Ford, J.D.; Steinberg, K.L.; Hawke, J.; Levine, J.; Zhang, W. Randomized Trial Comparison of Emotion Regulation and Relational Psychotherapies for PTSD with Girls Involved in Delinquency. J. Clin. Child Adolesc. Psychol. 2012, 41, 27–37. [Google Scholar] [CrossRef]
- Ray, D.C.; Burgin, E.; Gutierrez, D.; Ceballos, P.; Lindo, N. Child-centered play therapy and adverse childhood experiences: A randomized controlled trial. J. Couns. Dev. 2021, 100, 134–145. [Google Scholar] [CrossRef]
- Morris, J.; Belfer, M.; Daniels, A.; Flisher, A.; Villé, L.; Lora, A.; Saxena, S. Treated prevalence of and mental health services received by children and adolescents in 42 low-and-middle-income countries. J. Child Psychol. Psychiatry 2011, 52, 1239–1246. [Google Scholar] [CrossRef] [PubMed]
- Malhi, P.; Bharti, B. Using innovative narrative therapies with children who witness intimate partner violence. Indian Pediatr. Case Rep. 2022, 2, 17–20. [Google Scholar] [CrossRef]
- Pernebo, K.; Fridell, M.; Almqvist, K. Reduced psychiatric symptoms at 6 and 12 months’ follow-up of psychotherapeutic and psychoeducative group interventions for children exposed to intimate partner violence. Child Abus. Negl. 2019, 93, 228–238. [Google Scholar] [CrossRef]
- Mannarino, A.P.; Cohen, J.A.; Deblinger, E.; Runyon, M.K.; Steer, R.A. Trauma-focused cognitive-behavioral therapy for children: Sustained impact of treatment 6 and 12 months later. Child Maltreatment 2012, 17, 231–241. [Google Scholar] [CrossRef]
- Bettany-Saltikov, J. EBOOK: How to Do a Systematic Literature Review in Nursing: A Step-by-Step Guide; Open University Press: London, UK, 2016. [Google Scholar]
- Clarke, M. Overview of methods. In Reviewing Research Evidence for Nursing Practice: Systematic Reviews; Webb, C., Roe, B., Eds.; Blackwell Publishing: Oxford, UK, 2007; pp. 3–7. [Google Scholar]
- Rodgers, M.; Sowden, A.; Petticrew, M.; Arai, L.; Roberts, H.; Britten, N.; Popay, J. Testing Methodological Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. Evaluation 2009, 15, 49–73. [Google Scholar] [CrossRef]
- Amuyunzu-Nyamongo, M. The social and cultural aspects of mental health in African societies. In Commonwealth Health Partnerships 2013; Commonwealth Secretariat: London, UK, 2013. [Google Scholar]
- Ritchie, J.; Lewis, J.; Nicholas, C.M.; Ormston, R. Qualitative Research Practice: A Guide for Social Science Student and Researchers; Sage: London, UK, 2014. [Google Scholar]
- Botma, Y.; Greeff, M.; Makhado, L.; Mulaudzi, F.M. Research in Health Sciences, 2nd ed.; Pearson South Africa (Pty) Ltd.: Cape Town, South Africa, 2022. [Google Scholar]
- Copeland, W.E.; Shanahan, L.; Hinesley, J.; Chan, R.F.; Aberg, K.A.; Fairbank, J.A.; Oord, E.J.C.G.v.D.; Costello, E.J. Association of Childhood Trauma Exposure With Adult Psychiatric Disorders and Functional Outcomes. JAMA Netw. Open 2018, 1, e184493. [Google Scholar] [CrossRef]
- Jafarzade, M.; Ardakan, A.M.; Saleh, Y.R.M. The Effectiveness of Play Therapy Combined With a Trauma-focused Cognitive Behavioral Therapy on Trauma Symptoms and the Loneliness Feeling. Pract. Clin. Psychol. 2023, 11, 211–222. [Google Scholar] [CrossRef]
- Cohen, J.A.; Mannarino, A.P.; Iyengar, S. Community treatment of posttraumatic stress disorder for children exposed to intimate partner violence: A randomized controlled trial. Arch. Pediatr. Adolesc. Med. 2011, 165, 16–21. [Google Scholar] [CrossRef]
- Coetzer, J.A.; Bold, A.; van der Mark, E.J. Exploring mental health interventions for youth in Southern Africa: A rapid review. Acta Psychol. 2022, 229, 103699. [Google Scholar] [CrossRef]
- Morison, L.; Simonds, L.; Stewart, S.-J.F. Effectiveness of creative arts-based interventions for treating children and adolescents exposed to traumatic events: A systematic review of the quantitative evidence and meta-analysis. Arts Health 2021, 14, 237–262. [Google Scholar] [CrossRef]
- Yule, K.; Houston, J.; Grych, J. Resilience in Children Exposed to Violence: A Meta-analysis of Protective Factors Across Ecological Contexts. Clin. Child Fam. Psychol. Rev. 2019, 22, 406–431. [Google Scholar] [CrossRef]
- UNODC. Global Study on Homicide. 2019. Available online: https://www.unodc.org/documents/data-and-analysis/gsh/Booklet1.pdf (accessed on 19 August 2023).
- D’Andrea, W.; Ford, J.; Stolbach, B.; Spinazzola, J.; van der Kolk, B.A. Understanding interpersonal trauma in children: Why we need a developmentally appropriate trauma diagnosis. Am. J. Orthopsychiatry 2012, 82, 187–200. [Google Scholar] [CrossRef] [PubMed]
- Pope, C.; Ziebland, S.; Mays, N. Qualitative research in health care. Analysing qualitative data. BMJ 2000, 320, 114–116. [Google Scholar] [CrossRef]
- Pedras, S.; AS Moreira, P.; Ramalho, S.; Inman, R.A.; Faria, S.; Araújo, M. The exposure to violence questionnaire in adolescents: Psychometrics and associations with well-being. J. Child Fam. Stud. 2021, 30, 633–649. [Google Scholar] [CrossRef]
- Vaughn-Coaxum, R.A.; Wang, Y.; Kiely, J.; Weisz, J.R.; Dunn, E.C. Associations Between Trauma Type, Timing, and Accumulation on Current Coping Behaviors in Adolescents: Results from a Large, Population-based Sample. J. Youth Adolesc. 2017, 47, 842–858. [Google Scholar] [CrossRef]
- Beeckman, D.; Schoonhoven, L.; Boucqué, H.; Van Maele, G.; Defloor, T. Pressure ulcers: E-learning to improve classification by nurses and nursing students. J. Clin. Nurs. 2008, 17, 1697–1707. [Google Scholar] [CrossRef] [PubMed]
- LaBrenz, C.A.; Dell, P.J.; Fong, R.; Liu, V. Happily Ever After? Life Satisfaction After Childhood Exposure to Violence. J. Interpers. Violence 2019, 36, NP6747–NP6766. [Google Scholar] [CrossRef]
- Cuartas, J.; McCoy, D.C.; Rey-Guerra, C.; Britto, P.R.; Beatriz, E.; Salhi, C. Early childhood exposure to non-violent discipline and physical and psychological aggression in low-and middle-income countries: National, regional, and global prevalence estimates. Child Abus. Negl. 2019, 92, 93–105. [Google Scholar] [CrossRef]
- Schneider, S. Associations between childhood exposure to community violence, child maltreatment and school outcomes. Child Abus. Negl. 2020, 104, 104473. [Google Scholar] [CrossRef]
- Contreras, L.; León, S.P.; Cano-Lozano, M.C. Socio-cognitive variables involved in the relationship between violence exposure at home and child-to-parent violence. J. Adolesc. 2020, 80, 19–28. [Google Scholar] [CrossRef] [PubMed]
- Beckmann, L. Family Relationships as Risks and Buffers in the Link between Parent-to-Child Physical Violence and Adolescent-to-Parent Physical Violence. J. Fam. Violence 2019, 35, 131–141. [Google Scholar] [CrossRef]
- Gartland, D.; Giallo, R.; Woolhouse, H.; Mensah, F.; Brown, S. Intergenerational Impacts of Family Violence—Mothers and Children in a Large Prospective Pregnancy Cohort Study. eClinicalMedicine 2019, 15, 51–61. [Google Scholar] [CrossRef] [PubMed]
- Guzmán, D.B.; Miller-Graff, L.E.; Scheid, C.R. Types of Childhood Exposure to Violence and Association With Caregiver Trauma in Peru. J. Interpers. Violence 2020, 37, NP1125–NP1146. [Google Scholar] [CrossRef]
- Martin, R.; Rajan, S.; Shareef, F.; Xie, K.C.; Allen, K.A.; Zimmerman, M.; Jay, J. Racial Disparities in Child Exposure to Firearm Violence Before and During COVID-19. Am. J. Prev. Med. 2022, 63, 204–212. [Google Scholar] [CrossRef]
- Lloyd, M. Domestic Violence and Education: Examining the Impact of Domestic Violence on Young Children, Children, and Young People and the Potential Role of Schools. Front. Psychol. 2018, 9, 2094. [Google Scholar] [CrossRef]
- Pang, L.H.G.; Thomas, S.J. Exposure to Domestic Violence during Adolescence: Coping Strategies and Attachment Styles as Early Moderators and their Relationship to Functioning during Adulthood. J. Child Adolesc. Trauma 2019, 13, 185–198. [Google Scholar] [CrossRef]
- Heinze, J.E.; Cook, S.H.; Wood, E.P.; Dumadag, A.C.; Zimmerman, M.A. Friendship Attachment Style Moderates the Effect of Adolescent Exposure to Violence on Emerging Adult Depression and Anxiety Trajectories. J. Youth Adolesc. 2018, 47, 177–193. [Google Scholar] [CrossRef]
- van Geel, M.; Goemans, A.; Vedder, P.H. The relation between peer victimization and sleeping problems: A meta-analysis. Sleep Med. Rev. 2015, 27, 89–95. [Google Scholar] [CrossRef]
- Kutcher, S.; Perkins, K.; Gilberds, H.; Udedi, M.; Ubuguyu, O.; Njau, T.; Chapota, R.; Hashish, M. Creating evidence-based youth mental health policy in Sub-Saharan Africa: A description of the integrated approach to addressing the issue of youth depression in Malawi and Tanzania. Front. Psychiatry 2019, 10, 542. [Google Scholar]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).