Post-Acute Sequelae of COVID-19 (PASC) in Pediatrics: Factors That Impact Symptom Severity and Referral to Treatment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Procedure
2.2. Integrated Pain and Wellness Program
2.3. Measures
2.4. Data Analysis
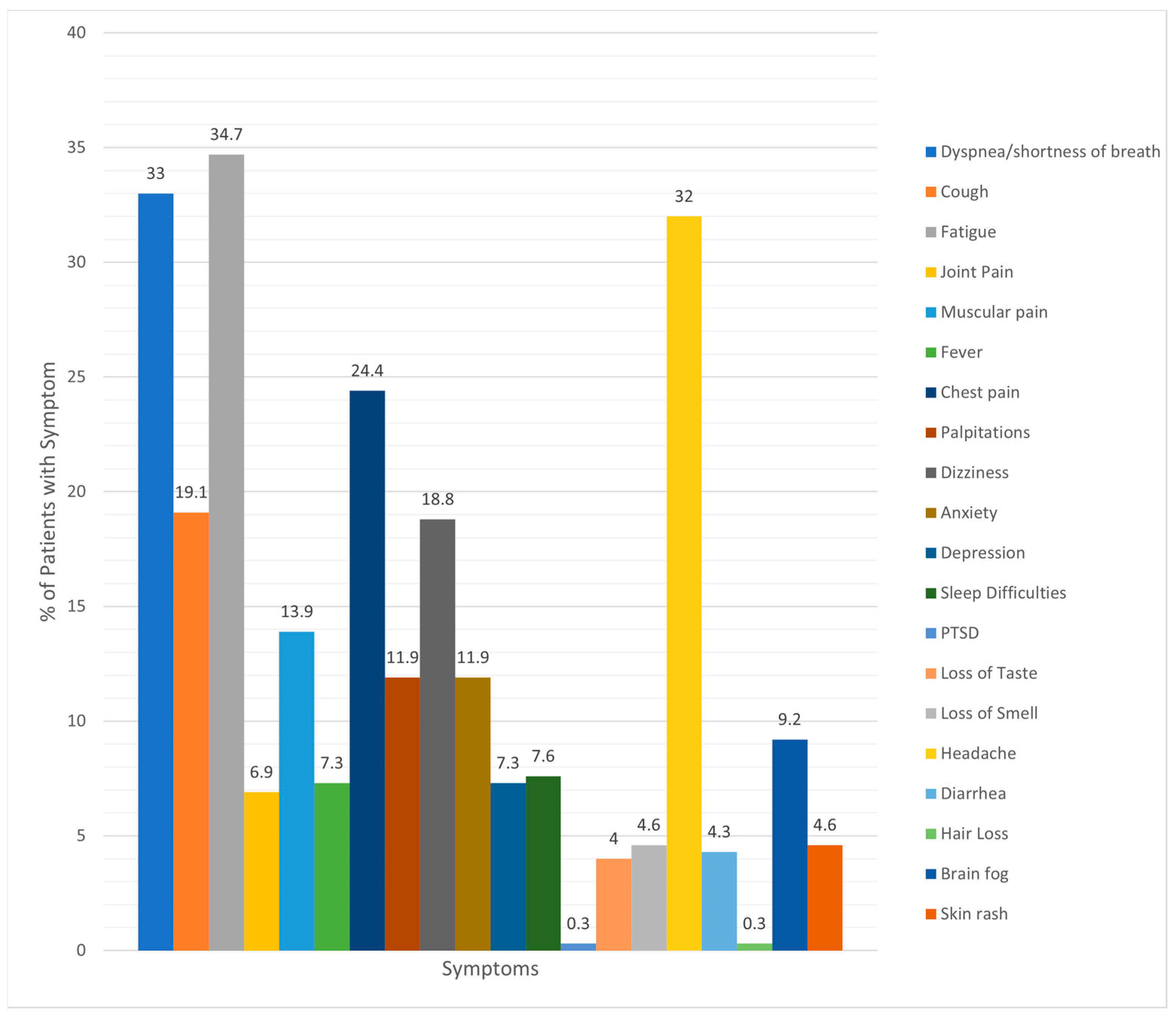
3. Results
3.1. Patient Characteristics
3.2. Vaccination Status
3.3. Integrated Pain and Wellness Program Referrals
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- U.S. Government Accountability Office. Science & Tech Spotlight: Long COVID. Available online: https://www.gao.gov/products/gao-22-105666 (accessed on 28 August 2023).
- Rao, S.; Lee, G.M.; Razzaghi, H.; Lorman, V.; Mejias, A.; Pajor, N.M.; Thacker, D.; Webb, R.; Dickinson, K.; Bailey, L.C.; et al. Clinical Features and Burden of Postacute Sequelae of SARS-CoV-2 Infection in Children and Adolescents. JAMA Pediatr. 2022, 176, 1000–1009. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Foer, D.; MacPhaul, E.; Lo, Y.C.; Bates, D.W.; Zhou, L. PASCLex: A Comprehensive Post-Acute Sequelae of COVID-19 (PASC) Symptom Lexicon Derived from Electronic Health Record Clinical Notes. J. Biomed. Inform. 2022, 125, 103951. [Google Scholar] [CrossRef] [PubMed]
- Munipalli, B.; Seim, L.; Dawson, N.L.; Knight, D.; Dabrh, A.M.A. Post-Acute Sequelae of COVID-19 (PASC): A Meta-Narrative Review of Pathophysiology, Prevalence, and Management. SN Compr. Clin. Med. 2022, 4, 90. [Google Scholar] [CrossRef]
- Nalbandian, A.; Sehgal, K.; Gupta, A.; Madhavan, M.V.; McGroder, C.; Stevens, J.S.; Cook, J.R.; Nordvig, A.S.; Shalev, D.; Sehrawat, T.S.; et al. Post-Acute COVID-19 Syndrome. Nat. Med. 2021, 27, 601–615. [Google Scholar] [CrossRef] [PubMed]
- Freund, O.; Breslavsky, A.; Fried, S.; Givoli-Vilensky, R.; Cohen-Rubin, S.; Zacks, N.; Kleinhendler, E.; Unterman, A.; Frydman, S.; Wand, O.; et al. Interactions and clinical implications of serological and respiratory variables 3 months after acute COVID-19. Clin. Exp. Med. 2023, 23, 3729–3736. [Google Scholar] [CrossRef]
- Wang, C.; Ramasamy, A.; Verduzco-Gutierrez, M.; Brode, W.M.; Melamed, E. Acute and post-acute sequelae of SARS-CoV-2 infection: A review of risk factors and social determinants. Virol. J. 2023, 20, 124. [Google Scholar] [CrossRef]
- Marasco, G.; Cremon, C.; Barbaro, M.R.; Cacciari, G.; Falangone, F.; Kagramanova, A.; Bordin, D.; Drug, V.; Miftode, E.; Fusaroli, P.; et al. Post COVID-19 Irritable Bowel Syndrome. Gut 2022, 72, 484–492. [Google Scholar] [CrossRef]
- Ormiston, C.K.; Świątkiewicz, I.; Taub, P.R. Postural Orthostatic Tachycardia Syndrome as a Sequela of COVID-19. Heart Rhythm. 2022, 19, 1880–1889. [Google Scholar] [CrossRef]
- de Lima, J.B.; Salazar, L.; Fernandes, A.; Teixeira, C.; Marques, L.; Afonso, C. Long COVID in Children and Adolescents: A Retrospective Study in a Pediatric Cohort. Pediatr. Infect. Dis. J. 2023, 42, e109–e111. [Google Scholar] [CrossRef]
- Ndugga, N.; Hill, L.; Artiga, S. COVID-19 Cases and Deaths, Vaccinations, and Treatments by Race/Ethnicity as of Fall 2022. KFF. Available online: https://www.kff.org/racial-equity-and-health-policy/issue-brief/covid-19-cases-and-deaths-vaccinations-and-treatments-by-race-ethnicity-as-of-fall-2022/#:~:text=Age-standardized%20data%20show%20that,White%20counterparts%20(Figure%201) (accessed on 20 December 2022).
- Centers for Disease Control and Prevention, National Center for Health Statistics. Long COVID—Household Pulse Survey. Available online: https://www.cdc.gov/nchs/covid19/pulse/long-covid.htm (accessed on 20 December 2022).
- Oliveira, C.R.; Feemster, K.A.; Ulloa, E.R. Pediatric COVID-19 Health Disparities and Vaccine Equity. J. Pediatr. Infect. Dis. Soc. 2022, 11 (Suppl. S4), S141–S147. [Google Scholar] [CrossRef]
- Saelee, R.; Zell, E.; Murthy, B.P.; Castro-Roman, P.; Fast, H.; Meng, L.; Shaw, L.; Gibbs-Scharf, L.; Chorba, T.; Harris, L.Q.; et al. Disparities in COVID-19 Vaccination Coverage Between Urban and Rural Counties—United States, December 14, 2020–January 31, 2022. MMWR Morb. Mortal. Wkly. Rep. 2022, 71, 335–340. [Google Scholar] [CrossRef] [PubMed]
- Herrera, J.E.; Niehaus, W.N.; Whiteson, J.; Azola, A.; Baratta, J.M.; Fleming, T.K.; Kim, S.Y.; Naqvi, H.; Sampsel, S.; Silver, J.K.; et al. Multidisciplinary Collaborative Consensus Guidance Statement on the Assessment and Treatment of Fatigue in Postacute Sequelae of SARS-CoV-2 Infection (PASC) Patients. PM R 2021, 13, 1027–1043. [Google Scholar] [CrossRef] [PubMed]
- Blitshteyn, S.; Whiteson, J.H.; Abramoff, B.; Azola, A.; Bartels, M.N.; Bhavaraju-Sanka, R.; Chung, T.; Fleming, T.K.; Henning, E.; Miglis, M.G.; et al. Multi-Disciplinary Collaborative Consensus Guidance Statement on the Assessment and Treatment of Autonomic Dysfunction in Patients with Post-Acute Sequelae of SARS-CoV-2 Infection (PASC). PM R 2022, 14, 1270–1291. [Google Scholar] [CrossRef] [PubMed]
- Harris, P.A.; Taylor, R.; Thielke, R.; Payne, J.; Gonzalez, N.; Conde, J.G. Research Electronic Data Capture (REDCap)—A Metadata-Driven Methodology and Workflow Process for Providing Translational Research Informatics Support. J. Biomed. Inform. 2009, 42, 377–381. [Google Scholar] [CrossRef]
- Harris, P.A.; Taylor, R.; Minor, B.L.; Elliott, V.; Fernandez, M.; O’Neal, L.; McLeod, L.; Delacqua, G.; Delacqua, F.; Kirby, J.; et al. REDCap Consortium. The REDCap Consortium: Building an International Community of Software Platform Partners. J. Biomed. Inform. 2019, 95, 103208. [Google Scholar] [CrossRef]
- Varni, J.W.; Stucky, B.D.; Thissen, D.; Dewitt, E.M.; Irwin, D.E.; Lai, J.S.; Yeatts, K.; Dewalt, D.A. PROMIS Pediatric Pain Interference Scale: An Item Response Theory Analysis of the Pediatric Pain Item Bank. J. Pain. 2010, 11, 1109–1119. [Google Scholar] [CrossRef]
- Pilkonis, P.A.; Choi, S.W.; Reise, S.P.; Stover, A.M.; Riley, W.T.; Cella, D.; PROMIS Cooperative Group. Item Banks for Measuring Emotional Distress from the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, Anxiety, and Anger. Assessment 2011, 18, 263–283. [Google Scholar] [CrossRef]
- Ullah, I.; Khan, K.S.; Tahir, M.J.; Ahmed, A.; Harapan, H. Myths and conspiracy theories on vaccines and COVID-19: Potential effect on global vaccine refusals. Vacunas 2021, 22, 93–97. [Google Scholar] [CrossRef]
- American Academy of Pediatrics. Post COVID-19 Conditions in Children and Adolescents. Available online: https://www.aap.org/en/pages/2019-novel-coronavirus-covid-19-infections/clinical-guidance/post-covid-19-conditions-in-children-and-adolescents/ (accessed on 20 December 2022).
- Freund, O.; Breslavsky, A.; Givoli-Vilensky, R.; Zacks, N.; Gershman, E.; Melloul, A.; Wand, O.; Bilenko, N.; Bar-Shai, A. Assessment of a close respiratory follow-up schedule at 3 and 6 months after acute COVID-19 and its related investigations. Respir. Med. 2023, 217, 107367. [Google Scholar] [CrossRef]
- Gorna, R.; MacDermott, N.; Rayner, C.; O’Hara, M.; Evans, S.; Agyen, L.; Nutland, W.; Rogers, N.; Hastie, C. Long COVID Guidelines Need to Reflect Lived Experience. Lancet 2021, 397, 455–457. [Google Scholar] [CrossRef]
- Kuitunen, I. Long COVID-19 is rarely diagnosed in children: Nationwide register-based analysis. Arch. Dis. Child. 2023, 108, 151. [Google Scholar] [CrossRef] [PubMed]
- Garai, R.; Krivácsy, P.; Herczeg, V.; Kovács, F.; Tél, B.; Kelemen, J.; Máthé, A.; Zsáry, E.; Takács, J.; Veres, D.S.; et al. Clinical assessment of children with long COVID syndrome. Pediatr. Res. 2023, 93, 1616–1625. [Google Scholar] [CrossRef] [PubMed]
- Copley, M.; Kozminski, B.; Gentile, N.; Geyer, R.; Friedly, J. Postacute Sequelae of SARS-CoV-2: Musculoskeletal Conditions and Pain. Phys. Med. Rehabil. Clin. 2023, 34, 585–605. [Google Scholar] [CrossRef] [PubMed]
| Gender Identity | % |
| Female | 55.4 |
| Male | 44.2 |
| Nonbinary | 0.3 |
| Race | % |
| White | 67 |
| Black | 14.9 |
| Asian | 2.6 |
| Other Pacific Islander | 0.3 |
| Mixed/Biracial | 0.3 |
| Other PI | 14.9 |
| Ethnicity | % |
| Hispanic | 20.8 |
| Non-Hispanic | 79.2 |
| Symptom | Vaccinated/ Symptom Present | Vaccinated/ Symptom Not Present | Not Vaccinated/ Symptom Present | Not Vaccinated/ Symptom Not Present | p-Value |
|---|---|---|---|---|---|
| Dyspnea/ shortness of breath | 37 | 58 | 51 | 135 | 0.49 |
| Cough | 21 | 74 | 30 | 156 | 0.219 |
| Fatigue | 35 | 60 | 66 | 120 | 0.822 |
| Joint pain | 8 | 87 | 12 | 174 | 0.544 |
| Muscular pain | 12 | 83 | 30 | 156 | 0.437 |
| Fever | 5 | 90 | 16 | 1370 | 0.314 |
| Chest pain | 21 | 74 | 43 | 143 | 0.848 |
| Palpitations | 8 | 87 | 24 | 162 | 0.263 |
| Dizziness | 19 | 76 | 32 | 154 | 0.565 |
| Anxiety | 16 | 79 | 19 | 167 | 0.112 |
| Depression | 10 | 85 | 12 | 174 | 0.229 |
| Sleep difficulties | 7 | 88 | 16 | 170 | 0.721 |
| PTSD | 0 | 95 | 1 | 185 | 0.474 |
| Loss of taste | 3 | 92 | 8 | 178 | 0.64 |
| Loss of smell | 3 | 92 | 11 | 175 | 0.315 |
| Headache | 31 | 64 | 58 | 128 | 0.805 |
| Diarrhea | 3 | 92 | 10 | 176 | 0.402 |
| Hair loss | 0 | 95 | 1 | 185 | 0.474 |
| Brain fog | 7 | 88 | 18 | 168 | 0.52 |
| Skin rash | 6 | 89 | 8 | 178 | 0.463 |
| Fully Vaccinated | Not Fully Vaccinated | |||
|---|---|---|---|---|
| Age (mean) | 14.44 (2.99) | 12.93 (3.24) | F(2) = 7.60, p = 0.001 | |
| Biological sex at birth | χ2(2) = 5.68, p = 0.058 | |||
| Male | 40 | 78 | ||
| Female | 55 | 108 | ||
| Gender | χ2(4) = 6.11, p = 0.191 | |||
| Male | 40 | 79 | ||
| Female | 55 | 106 | ||
| Nonbinary | 0 | 1 | ||
| Race | χ2(10) = 13.52, p = 1.96 | |||
| White/Caucasian | 64 | 122 | ||
| Black/African American | 13 | 31 | ||
| Asian | 6 | 2 | ||
| Other Pacific Islander | 0 | 1 | ||
| Mixed Race/Biracial | 1 | 0 | ||
| Other | 11 | 30 | ||
| Ethnicity | χ2(2) = 1.99, p = 0.370 | |||
| Hispanic | 21 | 40 | ||
| Not Hispanic | 74 | 146 | ||
| Treatment Type | # of Visits | SD | Range |
|---|---|---|---|
| Physical therapy | 3.87 | 6.46 | 0–30 |
| Occupational therapy | 0.61 | 1.58 | 0–7 |
| Integrative medicine | 1.17 | 2.01 | 0–8 |
| Psychology | 2.75 | 2.61 | 0–10 |
| PROMIS Anxiety (T-score) | Caregiver | Teen | |
| 45.4 | 43.5 | ||
| 54 | 45.1 | ||
| 55.8 | 54 | ||
| 70.5 | |||
| 85.2 | |||
| 85.2 | |||
| PROMIS Pain Interference (T-score) | Caregiver | Teen | |
| 63 | 59.9 | ||
| 64.2 | 61.5 | ||
| 66 | 68.9 | ||
| 74.2 | |||
| 77.6 | |||
| 77.6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Soprano, C.M.; Ngo, R.; Konys, C.A.; Bazier, A.; Salamon, K.S. Post-Acute Sequelae of COVID-19 (PASC) in Pediatrics: Factors That Impact Symptom Severity and Referral to Treatment. Children 2023, 10, 1805. https://doi.org/10.3390/children10111805
Soprano CM, Ngo R, Konys CA, Bazier A, Salamon KS. Post-Acute Sequelae of COVID-19 (PASC) in Pediatrics: Factors That Impact Symptom Severity and Referral to Treatment. Children. 2023; 10(11):1805. https://doi.org/10.3390/children10111805
Chicago/Turabian StyleSoprano, Catherine M., Ryan Ngo, Casey A. Konys, Ashley Bazier, and Katherine S. Salamon. 2023. "Post-Acute Sequelae of COVID-19 (PASC) in Pediatrics: Factors That Impact Symptom Severity and Referral to Treatment" Children 10, no. 11: 1805. https://doi.org/10.3390/children10111805
APA StyleSoprano, C. M., Ngo, R., Konys, C. A., Bazier, A., & Salamon, K. S. (2023). Post-Acute Sequelae of COVID-19 (PASC) in Pediatrics: Factors That Impact Symptom Severity and Referral to Treatment. Children, 10(11), 1805. https://doi.org/10.3390/children10111805






