Quantitative Analysis of the Head Tilt Using Three-Dimensional Temporal Scan in Children with Torticollis
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Clinical Measurement
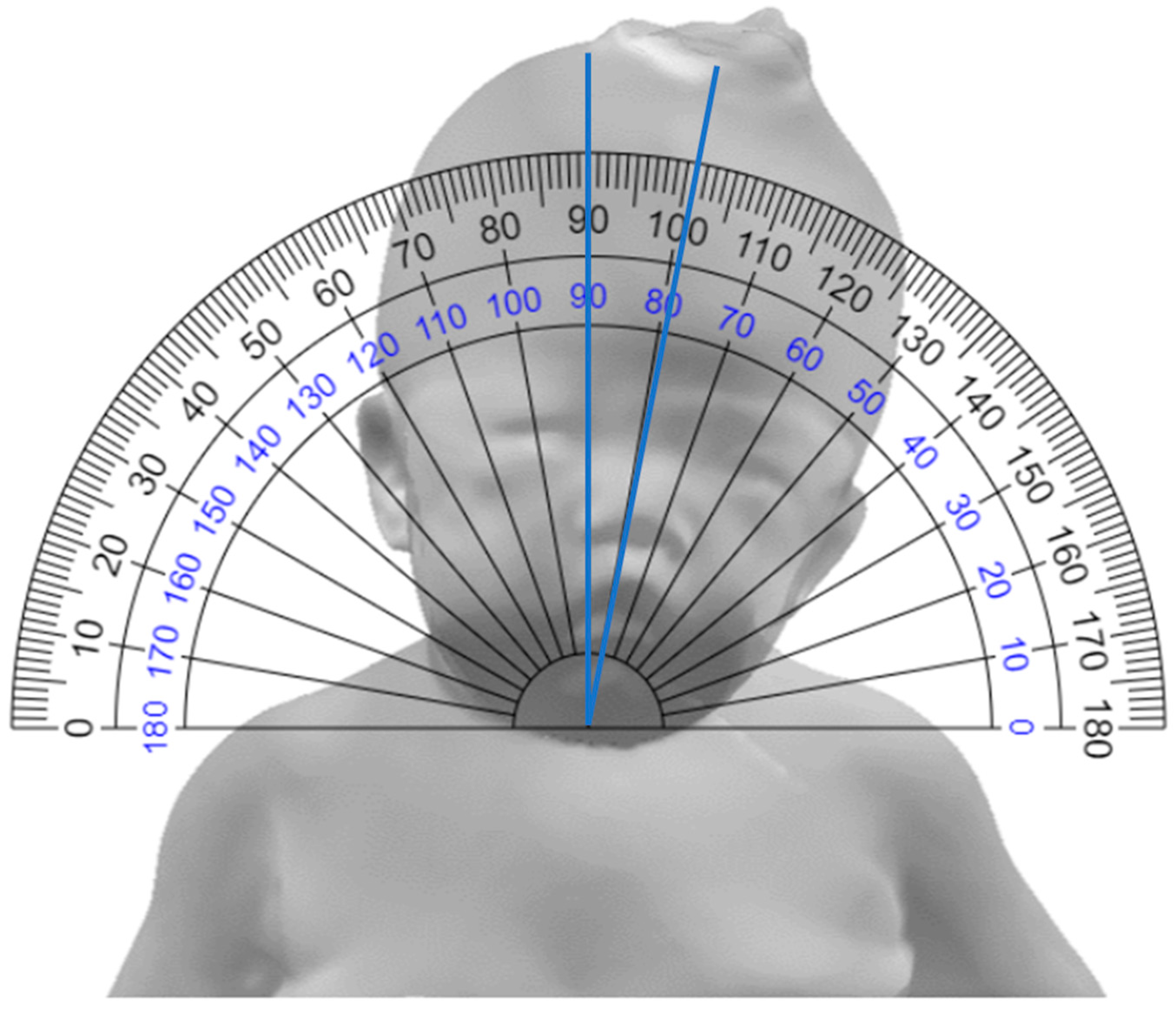
2.2.1. Goniometer Method
2.2.2. Still Photography Method
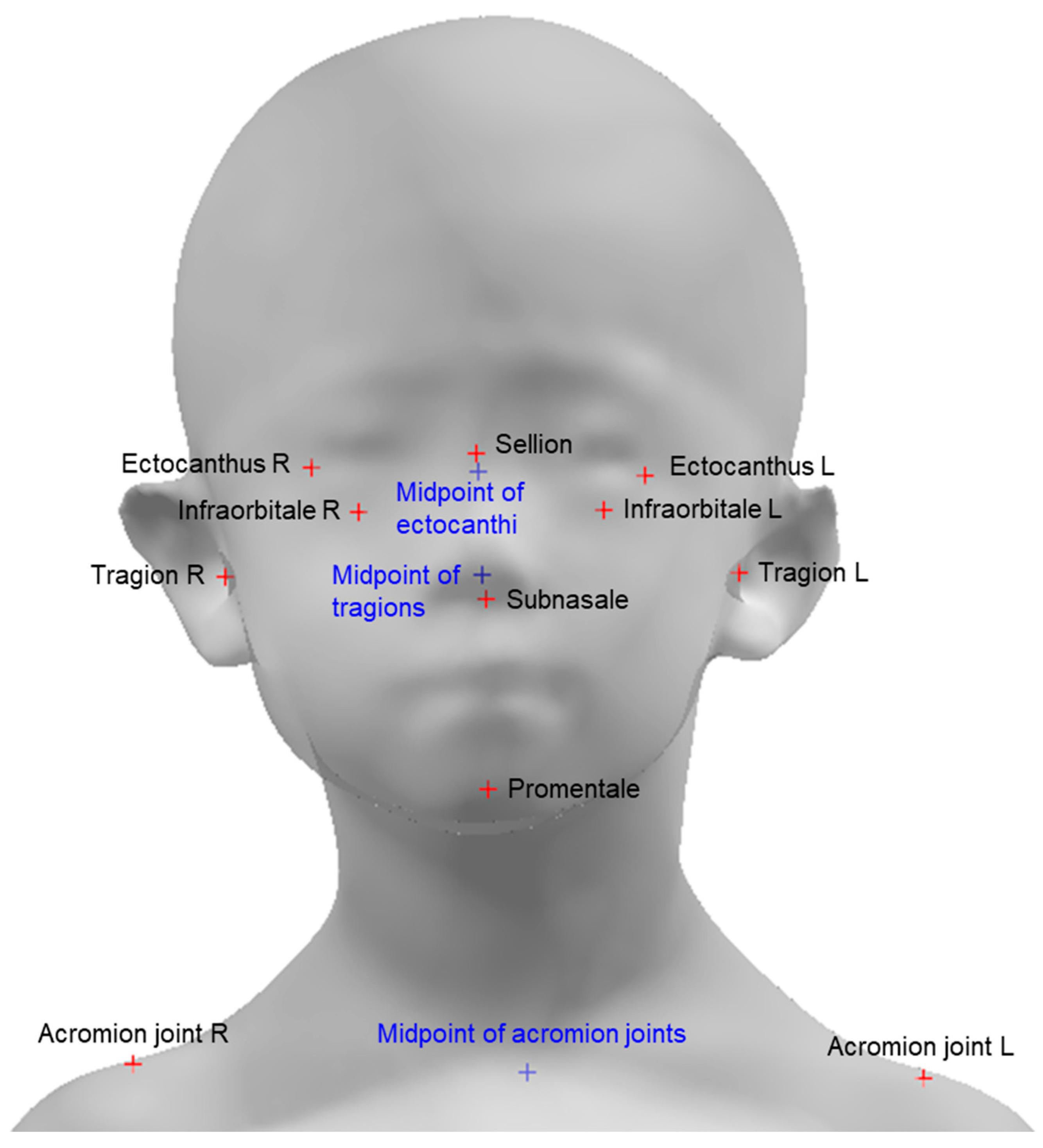
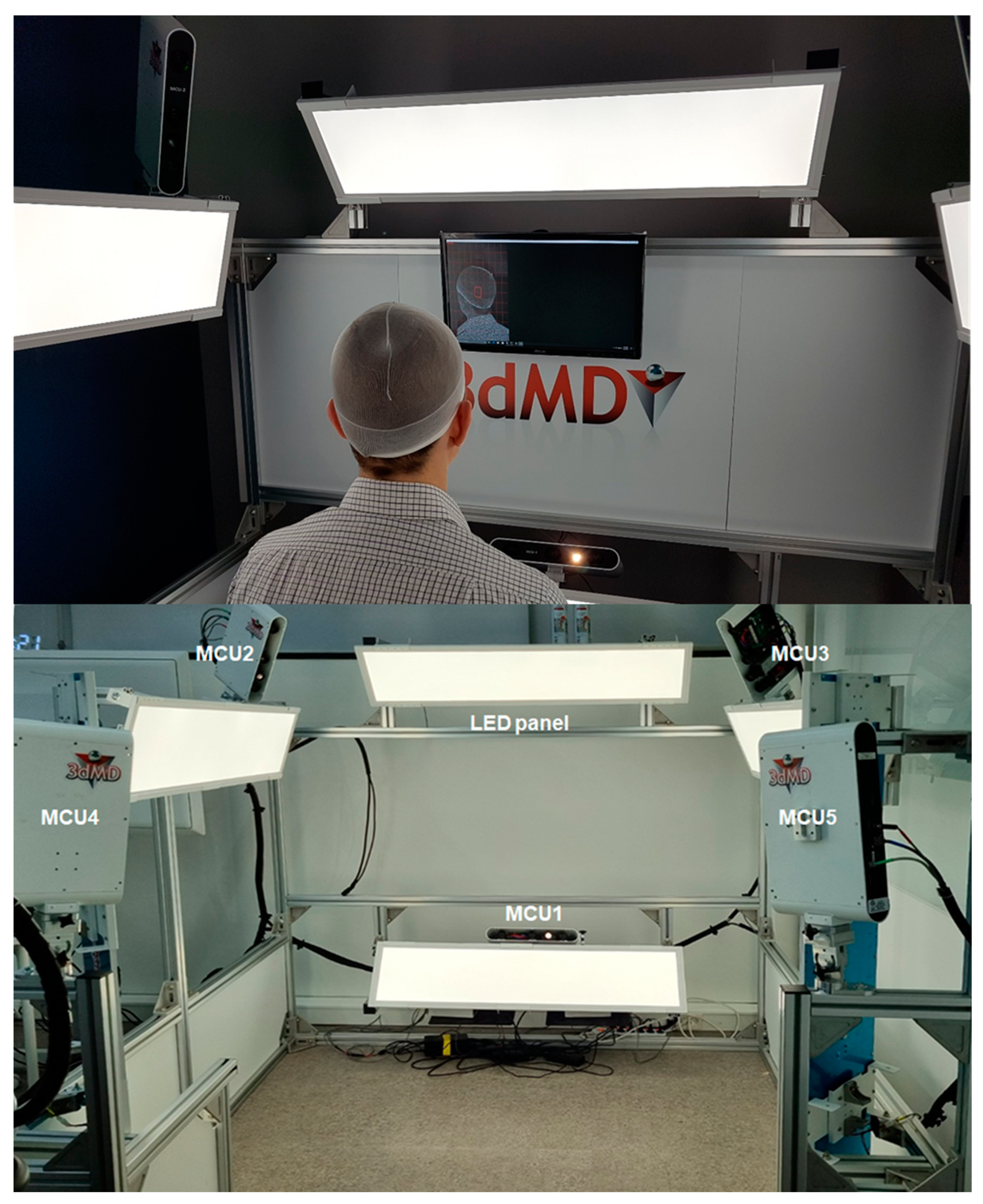
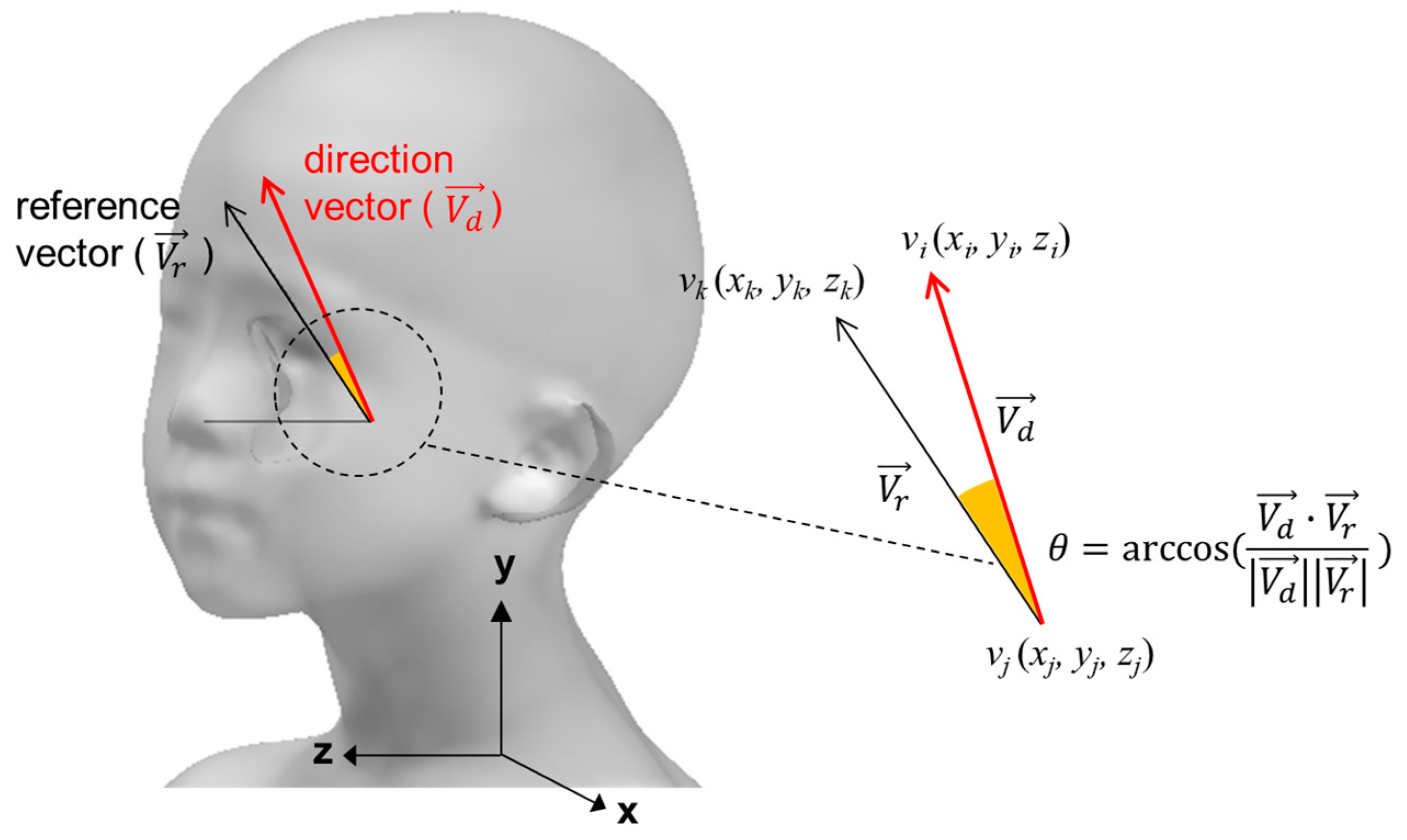
2.2.3. Three-Dimensional Scan Method
2.3. Statistical Analysis
3. Results
3.1. Angles with Multiple Methods
3.2. Reliability of Torticollis Measurement in Goniometer Method
3.3. Reliability of Torticollis Measurement in Goniometer and Still Photography Methods
3.4. Reliability of Torticollis Measurement in Goniometer Method and Roll Angle Using the 3D Scanner
3.5. Correlation between the Goniometer Method and 3D Angle
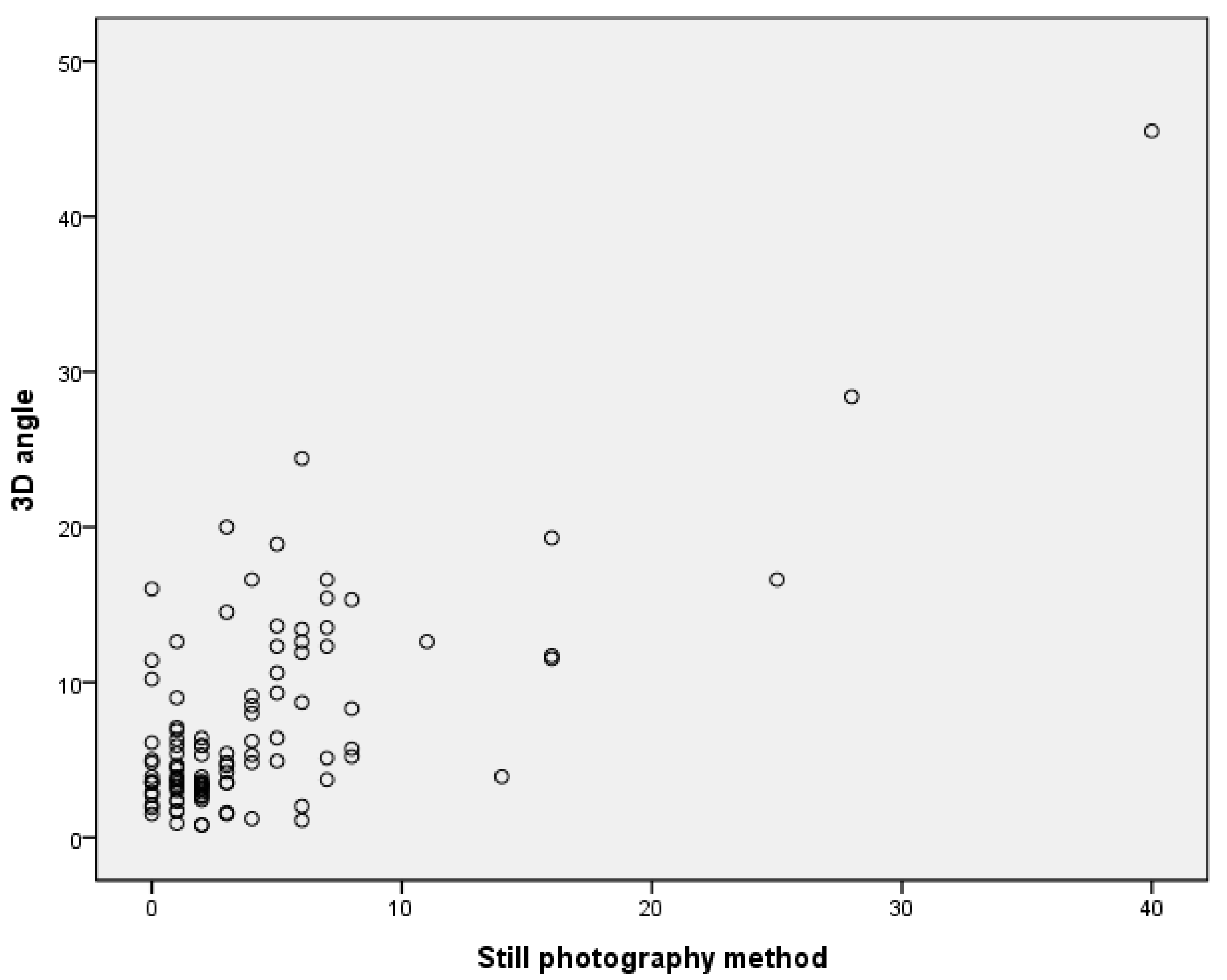
3.6. Correlation between Still Photography Method and 3D Angle
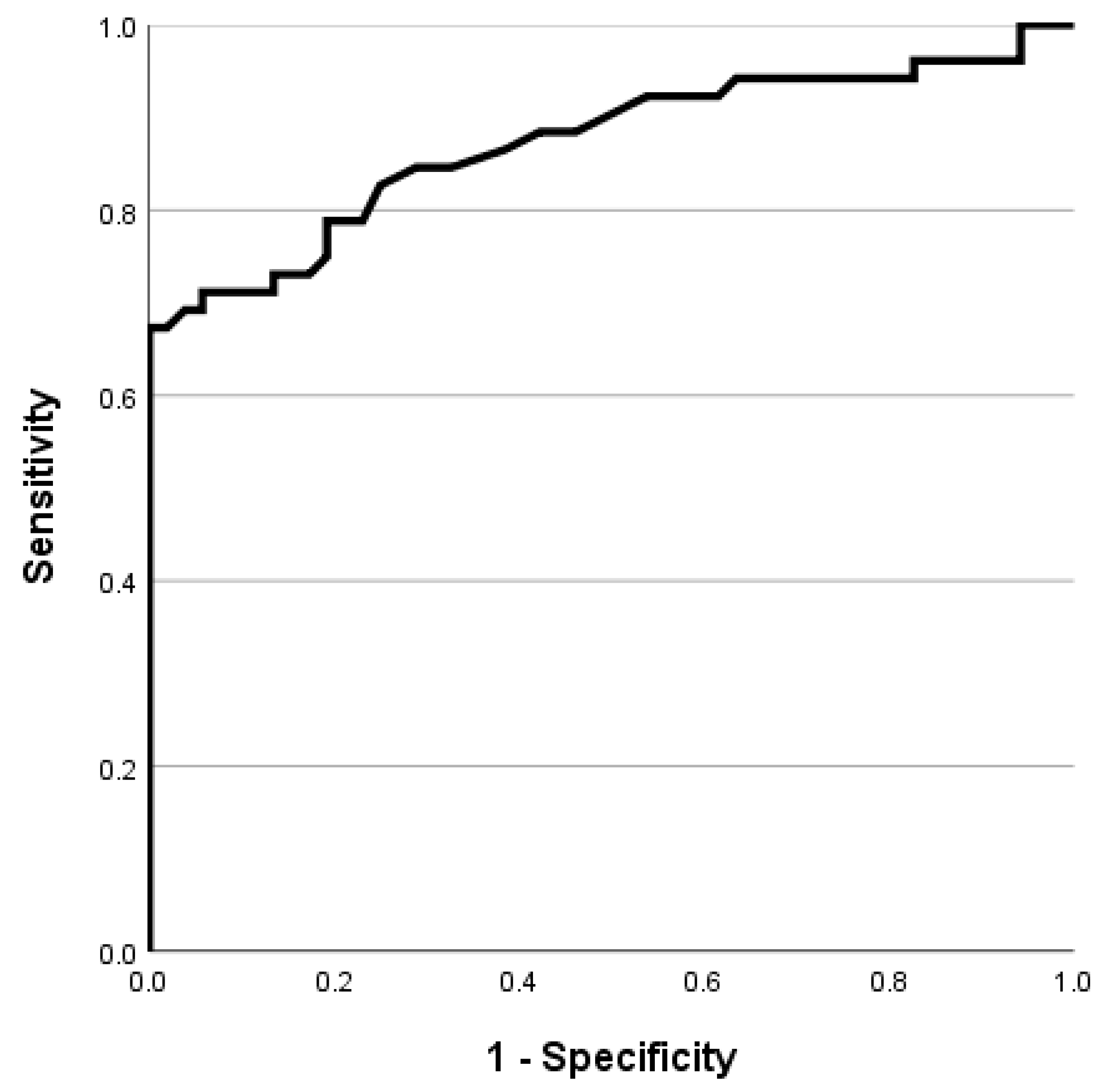
3.7. Cut-Off Value of 3D Angle for Diagnosis of Torticollis
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kaplan, S.L.; Coulter, C.; Fetters, L. Physical therapy management of congenital muscular torticollis: An evidence-based clinical practice guideline: From the Section on Pediatrics of the American Physical Therapy Association. Pediatr. Phys. Ther. 2013, 25, 348–394. [Google Scholar] [CrossRef]
- Papapetropoulos, S.; Baez, S.; Zitser, J.; Sengun, C.; Singer, C. Retrocollis: Classification, clinical phenotype, treatment outcomes and risk factors. Eur. Neurol. 2008, 59, 71–75. [Google Scholar] [CrossRef] [PubMed]
- Youdas, J.W.; Carey, J.R.; Garrett, T.R. Reliability of measurements of cervical spine range of motion—Comparison of three methods. Phys. Ther. 1991, 71, 98–104. [Google Scholar] [CrossRef]
- Fortin, C.; Feldman, D.E.; Cheriet, F.; Labelle, H. Clinical methods for quantifying body segment posture: A literature review. Disabil. Rehabil. 2011, 33, 367–383. [Google Scholar] [CrossRef] [Green Version]
- Antonaci, F.; Ghirmai, S.; Bono, G.; Nappi, G. Current methods for cervical spine movement evaluation: A review. Clin. Exp. Rheumatol. 2000, 18, S45–S52. [Google Scholar]
- Jordan, K. Assessment of published reliability studies for cervical spine range-of-motion measurement tools. J. Manip. Physiol. Ther. 2000, 23, 180–195. [Google Scholar] [CrossRef] [PubMed]
- de Koning, C.H.; van den Heuvel, S.P.; Staal, J.B.; Smits-Engelsman, B.C.; Hendriks, E.J. Clinimetric evaluation of active range of motion measures in patients with non-specific neck pain: A systematic review. Eur. Spine J. 2008, 17, 905–921. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Whitcroft, K.L.; Massouh, L.; Amirfeyz, R.; Bannister, G. Comparison of methods of measuring active cervical range of motion. Spine 2010, 35, E976–E980. [Google Scholar] [CrossRef] [PubMed]
- Tyson, S. A Systematic Review of Methods to Measure Posture. Phys. Ther. Rev. 2003, 8, 45–50. [Google Scholar] [CrossRef]
- Lynch-Caris, T.; Majeske, K.D.; Brelin-Fornari, J.; Nashi, S. Establishing reference values for cervical spine range of motion in pre-pubescent children. J. Biomech. 2008, 41, 2714–2719. [Google Scholar] [CrossRef] [PubMed]
- Lewandowski, J.; Szulc, P. The range of motion of the cervical spine in children aged from 3 to 7 years-an electrogoniometric study. Folia Morphol. 2003, 62, 459–461. [Google Scholar]
- Arbogast, K.B.; Gholve, P.A.; Friedman, J.E.; Maltese, M.R.; Tomasello, M.F.; Dormans, J.P. Normal cervical spine range of motion in children 3–12 years old. Spine 2007, 32, E309–E315. [Google Scholar] [CrossRef] [PubMed]
- Hald, E.S.; Hertle, R.W.; Yang, D. Application of a digital head-posture measuring system in children. Am. J. Ophthalmol. 2011, 151, 66–70.e2. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.C.; Wong, M.W.; Tang, S.P.; Chen, T.M.; Shum, S.L.; Wong, E.M. Clinical determinants of the outcome of manual stretching in the treatment of congenital muscular torticollis in infants. A prospective study of eight hundred and twenty-one cases. J. Bone. Jt. Surg. Am. 2001, 83, 679–687. [Google Scholar] [CrossRef] [Green Version]
- Klackenberg, E.P.; Elfving, B.; Haglund-Åkerlind, Y.; Carlberg, E.B. Intra-rater reliability in measuring range of motion in infants with congenital muscular torticollis. Adv. Physiother. 2005, 7, 84–91. [Google Scholar] [CrossRef]
- Murgia, M.; Venditto, T.; Paoloni, M.; Hodo, B.; Alcuri, R.; Bernetti, A.; Santilli, V.; Mangone, M. Assessing the Cervical Range of Motion in Infants with Positional Plagiocephaly. J. Craniofac. Surg. 2016, 27, 1060–1064. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ohman, A.M.; Nilsson, S.; Beckung, E.R. Validity and reliability of the muscle function scale, aimed to assess the lateral flexors of the neck in infants. Physiother. Theory Pract. 2009, 25, 129–137. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.H.; Yum, T.H.; Shim, J.S. Secondary Cervicothoracic Scoliosis in Congenital Muscular Torticollis. Clin. Orthop. Surg. 2019, 11, 344–351. [Google Scholar] [CrossRef]
- Rahlin, M.; Sarmiento, B. Reliability of still photography measuring habitual head deviation from midline in infants with congenital muscular torticollis. Pediatr. Phys. Ther. 2010, 22, 399–406. [Google Scholar] [CrossRef]
- Kekunnaya, R.; Isenberg, S.J. Effect of strabismus surgery on torticollis caused by congenital superior oblique palsy in young children. Indian J. Ophthalmol. 2014, 62, 322–326. [Google Scholar] [CrossRef]
- Sforza, C.; Grassi, G.; Fragnito, N.; Turci, M.; Ferrario, V. Three-dimensional analysis of active head and cervical spine range of motion: Effect of age in healthy male subjects. Clin. Biomech. 2002, 17, 611–614. [Google Scholar] [CrossRef] [PubMed]
- Walter, S.D.; Eliasziw, M.; Donner, A. Sample size and optimal designs for reliability studies. Stat. Med. 1998, 17, 101–110. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Lang, A.G.; Buchner, A. G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behav. Res. Methods 2007, 39, 175–191. [Google Scholar] [CrossRef] [PubMed]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.-G. Statistical power analyses using G*Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef] [Green Version]
- Park, T.K.; Kim, J.R.; Park, R.J.; Cho, M.S. Effect of Myofascial Release Therapy on Newborns and Infants with Congenital Torticollis. J. Korean Soc. Phys. Ther. 2006, 18, 1–11. [Google Scholar]
- van Det, M.J.; Meijerink, W.J.; Hoff, C.; van Veelen, M.A.; Pierie, J.P. Ergonomic assessment of neck posture in the minimally invasive surgery suite during laparoscopic cholecystectomy. Surg. Endosc. 2008, 22, 2421–2427. [Google Scholar] [CrossRef] [Green Version]
- Nilesh, K.; Mukherji, S. Congenital muscular torticollis. Annu. Maxillofac. Surg. 2013, 3, 198–200. [Google Scholar] [CrossRef] [Green Version]
- Oledzka, M.M.; Sweeney, J.K.; Evans-Rogers, D.L.; Coulter, C.; Kaplan, S.L. Experiences of Parents of Infants Diagnosed with Mild or Severe Grades of Congenital Muscular Torticollis. Pediatr. Phys. Ther. 2020, 32, 322–329. [Google Scholar] [CrossRef]
- Carenzio, G.; Carlisi, E.; Morani, I.; Tinelli, C.; Barak, M.; Bejor, M.; Dalla Toffola, E. Early rehabilitation treatment in newborns with congenital muscular torticollis. Eur. J. Phys. Rehabilit. Med. 2015, 51, 539–545. [Google Scholar]
- Tomczak, K.K.; Rosman, N.P. Torticollis. J. Child Neurol. 2013, 28, 365–378. [Google Scholar] [CrossRef]
- Ahn, A.R.; Rah, U.W.; Woo, J.E.; Park, S.; Kim, S.; Yim, S.Y. Craniovertebral Junction Abnormalities in Surgical Patients with Congenital Muscular Torticollis. J. Craniofac. Surg. 2018, 29, e327–e331. [Google Scholar] [CrossRef] [PubMed]
- Stellwagen, L.; Hubbard, E.; Chambers, C.; Jones, K.L. Torticollis, facial asymmetry and plagiocephaly in normal newborns. Arch. Dis. Child. 2008, 93, 827–831. [Google Scholar] [CrossRef] [Green Version]
- Han, M.H.; Kang, J.Y.; Do, H.J.; Park, H.S.; Noh, H.J.; Cho, Y.H.; Jang, D.H. Comparison of Clinical Findings of Congenital Muscular Torticollis between Patients with and without Sternocleidomastoid Lesions as Determined by Ultrasonography. J. Pediatr. Orthop. 2019, 39, 226–231. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.T.; Kang, J.H.; Yoo, C.I. Head tilt and facial asymmetry in congenital muscular torticollis. J. Korean Orthop. Assoc. 2003, 38, 217–222. [Google Scholar] [CrossRef]
- Baratta, V.M.; Linden, O.E.; Byrne, M.E.; Sullivan, S.R.; Taylor, H.O. A Quantitative Analysis of Facial Asymmetry in Torticollis Using 3-Dimensional Photogrammetry. Cleft Palate-Craniofac. J. 2022, 59, 40–46. [Google Scholar] [CrossRef] [PubMed]
- Swets, J.A. Measuring the accuracy of diagnostic systems. Science 1988, 240, 1285–1293. [Google Scholar] [CrossRef] [Green Version]
- Greiner, M.; Pfeiffer, D.; Smith, R.D. Principles and practical application of the receiver-operating characteristic analysis for diagnostic tests. Prev. Vet. Med 2000, 45, 23–41. [Google Scholar] [CrossRef]




| Control Group | Torticollis Group | p-Value | |
|---|---|---|---|
| Goniometer method by physiatrist 1 | 1.13 ± 1.10 | 6.67 ± 7.45 | <0.01 |
| Goniometer method by physiatrist 2 | 1.15 ± 1.02 | 6.77 ± 7.24 | <0.01 |
| Still photography method | 1.38 ± 1.07 | 6.98 ± 7.26 | <0.01 |
| Yaw angle with 3D scanner | 1.54 ± 0.91 | 6.08 ± 5.97 | <0.01 |
| Roll angle with 3D scanner | 2.13 ± 1.60 | 6.19 ± 6.33 | <0.01 |
| Pitch angle with 3D scanner | 5.78 ± 3.52 | 10.37 ± 6.65 | <0.01 |
| 3D angle (comprehensive angle considering yaw, roll, and pitch angles) | 3.60 ± 1.55 | 11.07 ± 7.65 | <0.01 |
| ICC (3,1) | 95% CI | p-Value | |
|---|---|---|---|
| Goniometer method of two physiatrists | 0.997 | 0.995–0.998 | <0.001 |
| Goniometer method by physiatrist 1 and still photography method | 0.996 | 0.994–0.997 | <0.001 |
| Goniometer method by physiatrist 2 and still photography method | 0.997 | 0.996–0.998 | <0.001 |
| Goniometer method by physiatrist 1 and roll angle with 3D scanner | 0.944 | 0.918–0.962 | <0.001 |
| Goniometer method by physiatrist 2 and roll angle with 3D scanner | 0.949 | 0.925–0.965 | <0.001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Yun, R.; Jung, H.; Cui, X.; Huh, S.; Lee, W.; You, H.; Kim, S. Quantitative Analysis of the Head Tilt Using Three-Dimensional Temporal Scan in Children with Torticollis. Children 2023, 10, 225. https://doi.org/10.3390/children10020225
Yun R, Jung H, Cui X, Huh S, Lee W, You H, Kim S. Quantitative Analysis of the Head Tilt Using Three-Dimensional Temporal Scan in Children with Torticollis. Children. 2023; 10(2):225. https://doi.org/10.3390/children10020225
Chicago/Turabian StyleYun, Rayu, Hayoung Jung, Xin Cui, Sungchul Huh, Wonsup Lee, Heecheon You, and Sooyeon Kim. 2023. "Quantitative Analysis of the Head Tilt Using Three-Dimensional Temporal Scan in Children with Torticollis" Children 10, no. 2: 225. https://doi.org/10.3390/children10020225
APA StyleYun, R., Jung, H., Cui, X., Huh, S., Lee, W., You, H., & Kim, S. (2023). Quantitative Analysis of the Head Tilt Using Three-Dimensional Temporal Scan in Children with Torticollis. Children, 10(2), 225. https://doi.org/10.3390/children10020225






