Prevalence of Dual Diagnoses among Children and Adolescents with Mental Health Conditions
Abstract
1. Introduction
1.1. Prevalence
1.2. Types of Comorbidity
2. Materials and Methods
2.1. Eligibility Criteria
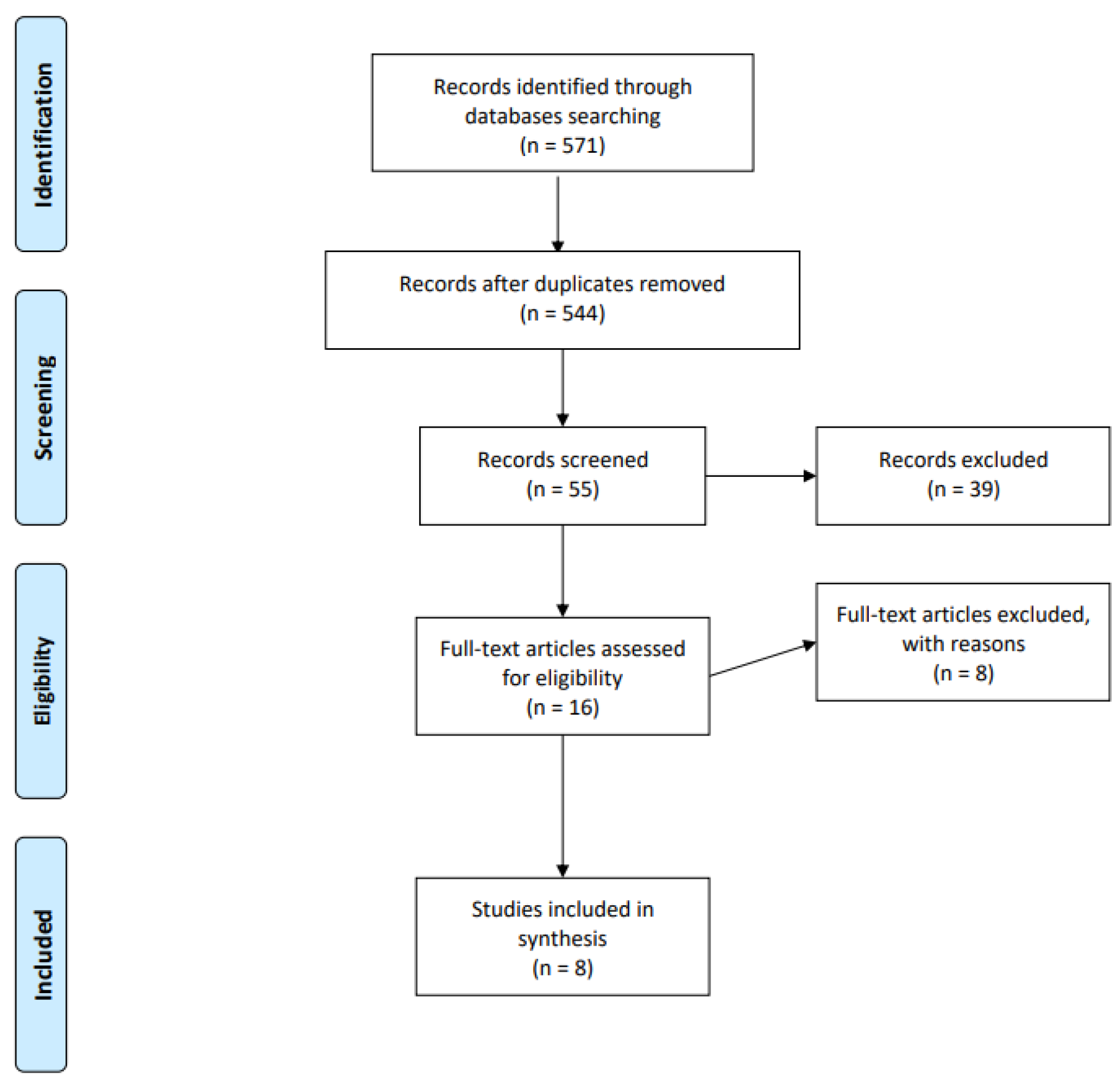
2.2. Selection and Data Collection Process
2.3. Methods
2.4. Ethics
3. Results
3.1. Prevalence of Dual Diagnoses among Children and Adolescents Treated Primarily for Mental Health Conditions
3.2. Gender-Specific Occurrence of Dual Diagnoses
3.3. Diagnostic Tools
3.4. Types of Psychiatric Diagnoses
3.5. Inpatient vs. Outpatient Care
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- EMCDDA. Co-Morbidity—Drug Use and Mental Disorders. In Drugs in Focus, 14th ed.; EMCDDAL: Lisbon, Portugal, 2004. [Google Scholar]
- Hughes, L. Closing the Gap: Dual Diagnosis Framework; DOH/CSIP: London, UK, 2006. [Google Scholar]
- Harvey, C.; McGill, K.; Kinney, C.; Harvey, M.; Blumberg, E.; Farr, J. FDDC-NADD Dual Diagnosis Study, Final Research Study Report; Florida Developmental Disabilities Council: Kingston, NY, USA, 2022. [Google Scholar] [CrossRef]
- Saddichha, S.; Schütz, C.G.; Sinha, B.N.P.; Manjunatha, N. Substance Use and Dual Diagnosis Disorders: Future Epidemiology, Determinants, and Policies. BioMed Res. Int. 2015, 2015, e145905. [Google Scholar] [CrossRef]
- Wise, B.K.; Cuffe, S.P.; Fischer, T. Dual diagnosis and successful participation of adolescents in substance abuse treatment. J. Subst. Abus. Treat. 2001, 21, 161–165. [Google Scholar] [CrossRef]
- Biederman, J.; Wilens, T.; Mick, E.; Faraone, S.V.; Weber, W.; Curtis, S.; Thornell, A.; Pfister, K.; Jetton, J.G.; Soriano, J. Is ADHD a risk factor for psychoactive substance use disorders? Findings from a four-year prospective follow-up study. J. Am. Acad. Child Adolesc. Psychiatry 1997, 36, 21–29. [Google Scholar] [CrossRef] [PubMed]
- Couwenbergh, C.; van den Brink, W.; Zwart, K.; Vreugdenhil, C.; van Wijngaarden-Cremers, P.; van der Gaag, R.J. Comorbid psychopathology in adolescents and young adults treated for substance use disorders: A review. Eur. Child Adolesc. Psychiatry 2006, 15, 319–328. [Google Scholar] [CrossRef] [PubMed]
- Belcher, H.M.; Shinitzky, H.E. Substance Abuse in Children: Prediction, Protection, and Prevention. Arch. Pediatr. Adolesc. Med. 1998, 152, 952–960. [Google Scholar] [CrossRef]
- Aarons, G.A.; Brown, S.A.; Hough, R.L.; Garland, A.F.; Wood, P.A. Prevalence of Adolescent Substance Use Disorders Across Five Sectors of Care. J. Am. Acad. Child Adolesc. Psychiatry 2001, 40, 419–426. [Google Scholar] [CrossRef]
- Stephens, J.R.; Heffner, J.L.; Adler, C.M.; Blom, T.J.; Anthenelli, R.M.; Fleck, D.E.; Welge, J.A.; Strakowski, S.M.; DelBello, M.P. Risk and Protective Factors Associated with Substance Use Disorders in Adolescents with First-Episode Mania. J. Am. Acad. Child Adolesc. Psychiatry 2014, 53, 771–779. [Google Scholar] [CrossRef]
- Arnevik, E.A.; Helverschou, S.B. Autism Spectrum Disorder and Co-occurring Substance Use Disorder—A Systematic Review. Subst. Abus. Res. Treat. 2016, 10, 69–75. [Google Scholar] [CrossRef]
- Tejeda-Romero, C.; Kobashi-Margáin, R.A.; Alvarez-Arellano, L.; Corona, J.C.; González-García, N. Differences in substance use, psychiatric disorders and social factors between Mexican adolescents and young adults: Dual diagnosis in Mexican adolescents. Am. J. Addict. 2018, 27, 625–631. [Google Scholar] [CrossRef] [PubMed]
- Goldstein, B.I.; Strober, M.; Axelson, D.; Goldstein, T.R.; Gill, M.K.; Hower, H.; Dickstein, D.; Hunt, J.; Yen, S.; Kim, E.; et al. Predictors of First-Onset Substance Use Disorders During the Prospective Course of Bipolar Spectrum Disorders in Adolescents. J. Am. Acad. Child Adolesc. Psychiatry 2013, 52, 1026–1037. [Google Scholar] [CrossRef] [PubMed]
- Richardson, T. Correlates of substance use disorder in bipolar disorder: A systematic review and meta-analysis. Ment. Health Subst. Use Dual Diagn. 2011, 4, 239–255. [Google Scholar] [CrossRef]
- Wolitzky-Taylor, K.; Bobova, L.; Zinbarg, R.E.; Mineka, S.; Craske, M.G. Longitudinal investigation of the impact of anxiety and mood disorders in adolescence on subsequent substance use disorder onset and vice versa. Addict. Behav. 2012, 37, 982–985. [Google Scholar] [CrossRef]
- Kim-Cohen, J.; Caspi, A.; Moffitt, T.E.; Harrington, H.; Milne, B.J.; Poulton, R. Prior Juvenile Diagnoses in Adults with Mental Disorder: Developmental Follow-Back of a Prospective-Longitudinal Cohort. Arch. Gen. Psychiatry 2003, 60, 709–717. [Google Scholar] [CrossRef] [PubMed]
- Basith, S.A.; Nakaska, M.M.; Sejdiu, A.; Shakya, A.; Namdev, V.; Gupta, S.; Mathialagan, K.; Makani, R. Substance Use Disorders (SUD) and Suicidal Behaviors in Adolescents: Insights From Cross-Sectional Inpatient Study. Cureus J. Med. Sci. 2021, 13, e15602. [Google Scholar] [CrossRef] [PubMed]
- Queeneth, U.; Bhimanadham, N.N.; Mainali, P.; Onyeaka, H.K.; Pankaj, A.; Patel, R.S. Heroin Overdose-Related Child and Adolescent Hospitalizations: Insight on Comorbid Psychiatric and Substance Use Disorders. Behav. Sci. 2019, 9, 77. [Google Scholar] [CrossRef] [PubMed]
- Babor, T.F.; Stenius, K.; Pates, R.; Miovský, M.; O’reilly, J.; Candon, P. (Eds.) Publishing Addiction Science: A Guide for the Perplexed; Ubiquity Press: London, UK, 2017; Available online: http://www.jstor.org/stable/j.ctv3t5qxw (accessed on 30 September 2022).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Medicine 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 5.0.1; The Cochrane Collaboration: London, UK, 2011; Available online: http://handbook.cochrane.org (accessed on 4 August 2022).
- Díaz, R.; Goti, J.; García, M.; Gual, A.; Serrano, L.; González, L.; Calvo, R.; Castro-Fornieles, J. Patterns of substance use in adolescents attending a mental health department. Eur. Child Adolesc. Psychiatry 2011, 20, 279–289. [Google Scholar] [CrossRef]
- Hirschtritt, M.E.; Pagano, M.E.; Christian, K.M.; McNamara, N.K.; Stansbrey, R.J.; Lingler, J.; Faber, J.E.; Demeter, C.A.; Bedoya, D.; Findling, R.L. Moderators of fluoxetine treatment response for children and adolescents with comorbid depression and substance use disorders. J. Subst. Abus. Treat. 2012, 42, 366–372. [Google Scholar] [CrossRef]
- Masroor, A.; Patel, R.S.; Bhimanadham, N.N.; Raveendran, S.; Ahmad, N.; Queeneth, U.; Pankaj, A.; Mansuri, Z. Conduct Disorder-Related Hospitalization and Substance Use Disorders in American Teens. Behav. Sci. 2019, 9, 73. [Google Scholar] [CrossRef]
- Wilens, T.E.; Martelon, M.; Anderson, J.P.; Shelley-Abrahamson, R.; Biederman, J. Difficulties in emotional regulation and substance use disorders: A controlled family study of bipolar adolescents. Drug Alcohol Depend. 2013, 132, 114–121. [Google Scholar] [CrossRef]
- Wu, L.T.; Gersing, K.; Burchett, B.; Woody, G.E.; Blazer, D.G. Substance use disorders and comorbid Axis I and II psychiatric disorders among young psychiatric patients: Findings from a large electronic health records database. J. Psychiatr. Res. 2011, 45, 1453–1462. [Google Scholar] [CrossRef]
- Korsgaard, H.O.; Torgersen, S.; Wentzel-Larsen, T.; Ulberg, R. Substance abuse and personality disorder comorbidity in adolescent outpatients: Are girls more severely ill than boys? Child Adolesc. Psychiatry Ment. Health 2016, 10, 8. [Google Scholar] [CrossRef] [PubMed]
- Lachman, A.; Nassen, R.; Hawkridge, S.; Emsley, R.A. A retrospective chart review of the clinical and psychosocial profile of psychotic adolescents with co-morbid substance use disorders presenting to acute adolescent psychiatric services at Tygerberg Hospital. South Afr. J. Psychiatry 2012, 18, 53–60. [Google Scholar] [CrossRef]
- Hollen, V.; Ortiz, G. Mental Health and Substance Use Comorbidity Among Adolescents in Psychiatric Inpatient Hospitals: Prevalence and Covariates. J. Child Adolesc. Subst. Abus. 2015, 24, 102–112. [Google Scholar] [CrossRef]
| Study (First Author) | Year of Publication | Country | Sample (n = x) | Range in Sample (Years) | Prevalence of Dual Diagnosis (%) | Interview PD and SUD |
|---|---|---|---|---|---|---|
| Diáz et al., 2011 [22] | 2011 | Spain | 237 | 12–17 | THC 10.1% alcohol 3.4% others 0.4% | DSM IV (YSR and CBCL) |
| Wu et al., 2011 [26] | 2011 | USA | n1 = 6210 n2 = 5247 | 2–12 13–17 | 1.6% 25% | DSM IV |
| Hirschtritt et al., 2012 [23] | 2012 | USA | 34 | 12–17 | THC abuse 47% (41.2% dependence) alcohol 29.4% (8.8%) polyvalent 2.9% | DSM IV KSADS |
| Lachman et al., 2012 [28] | 2012 | RSA | 141 | 13–18 | 54% | DSM IV |
| Wilens et al., 2013 [25] | 2013 | USA | 303 | 10–18 | BD subjects 30% CD subjects 42% | DSM IV KSADS-E SCID |
| Hollen & Oritz, 2015 [29] | 2015 | USA | 9154 | 11–17 | 25% | ICD 9 |
| Korsgaard et al., 2016 [27] | 2016 | Norway | 153 | 14–17 | 18.3 % | DSM IV M.I.N.I. |
| Masroor et al., 2019 [24] | 2019 | USA | 800614 | 12–18 | Amphetamins70.8% opioids 66.7% alcohol 52.7% THC 50.9% | ICD 9 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tomáš, J.; Lenka, Š. Prevalence of Dual Diagnoses among Children and Adolescents with Mental Health Conditions. Children 2023, 10, 293. https://doi.org/10.3390/children10020293
Tomáš J, Lenka Š. Prevalence of Dual Diagnoses among Children and Adolescents with Mental Health Conditions. Children. 2023; 10(2):293. https://doi.org/10.3390/children10020293
Chicago/Turabian StyleTomáš, Jandáč, and Šťastná Lenka. 2023. "Prevalence of Dual Diagnoses among Children and Adolescents with Mental Health Conditions" Children 10, no. 2: 293. https://doi.org/10.3390/children10020293
APA StyleTomáš, J., & Lenka, Š. (2023). Prevalence of Dual Diagnoses among Children and Adolescents with Mental Health Conditions. Children, 10(2), 293. https://doi.org/10.3390/children10020293





