Therapeutic Approaches to Dysautonomia in Childhood, with a Special Focus on Long COVID
Abstract
:1. Introduction
2. Materials and Methods
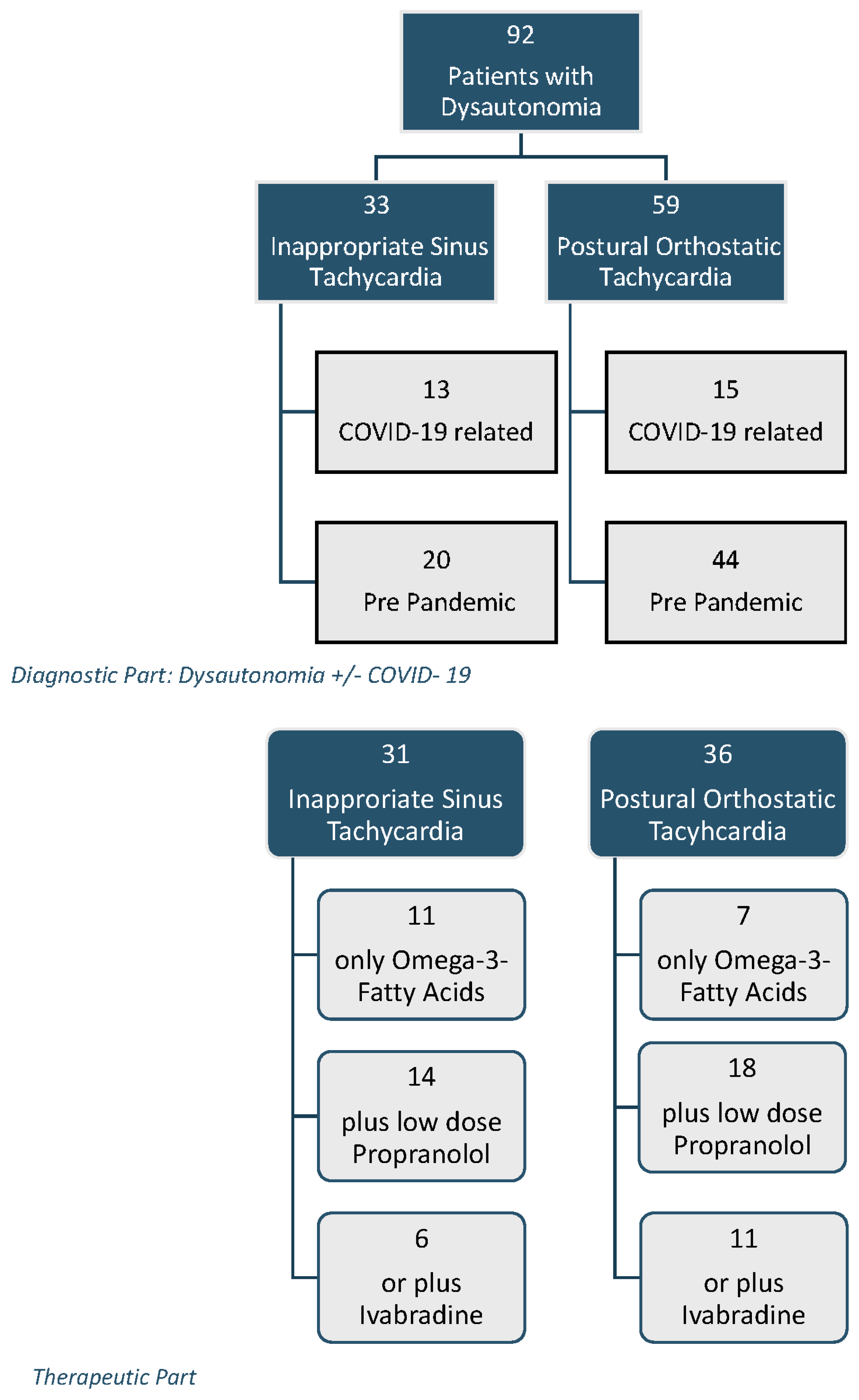
2.1. Patients
2.2. HRV Analysis
2.2.1. Time Domain HRV
- Average heart rates in beats per minute = mean heart rates of each 5 min interval;
- rMSSD in milliseconds = root mean square of differences between successive NN intervals; this parameter reflects parasympathetic influence.
2.2.2. Stress Index
2.2.3. Frequency Domain HRV
- Very low-frequency power (VLF = 0.00–0.04 Hz) in ms2;
- Low-frequency power (LF = 0.04–0.15 Hz) in ms2;
- High-frequency power (HF = 0.15–0.4 Hz) in ms2;
- LF/HF ratio;
- Total power (TP) in ms2.
2.3. Pharmacotherapy and Nutritional Supplementation
2.4. Statistics
3. Results
4. Discussion
- (1)
- Is PASC a comparable disease of the autonomic nervous system, similar to what we know from the treatment of psychosomatic diseases prior to the pandemic?
- (2)
- Can we objectively measure an effect on heart rate regulation for our most commonly used treatments (low-dose propranolol, ivabradine, and omega-3 fatty acid supplementation)?
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Abbreviations
References
- Rees, C.A. Lost among the trees? The autonomic nervous system and paediatrics. Arch. Dis. Child. 2014, 99, 552–562. [Google Scholar] [CrossRef] [PubMed]
- Ravens-Sieberer, U.; Erhart, M.; Devine, J.; Gilbert, M.; Reiss, F.; Barkmann, C.; Kaman, A. Child and Adolescent Mental Health During the COVID-19 Pandemic: Results of the Three-Wave Longitudinal COPSY Study. J. Adolesc. Health Off. Publ. Soc. Adolesc. Med. 2022, 71, 570–578. [Google Scholar] [CrossRef] [PubMed]
- Bisaccia, G.; Ricci, F.; Recce, V.; Serio, A.; Iannetti, G.; Chahal, A.A.; Gallina, S. Post-Acute Sequelae of COVID-19 and Cardiovascular Autonomic Dysfunction: What Do We Know? J. Cardiovasc. Dev. Dis. 2021, 8, 156. [Google Scholar] [CrossRef] [PubMed]
- Chung, T.H.; Azar, A. Autonomic Nerve Involvement in Post-Acute Sequelae of SARS-CoV-2 Syndrome (PASC). J. Clin. Med. 2022, 12, 73. [Google Scholar] [CrossRef]
- Chee, Y.J.; Fan, B.E.; Young, B.E.; Dalan, R.; Lye, D.C. Clinical trials on the pharmacological treatment of long COVID: A systematic review. J. Med. Virol. 2022, 95, e28289. [Google Scholar] [CrossRef]
- Davis, H.E.; McCorkell, L.; Vogel, J.M.; Topol, E.J. Long COVID: Major findings, mechanisms and recommendations. Nat. Rev. Microbiol. 2023, 1–14. [Google Scholar] [CrossRef]
- Rowe, S.; Spies, J.M.; Urriola, N. Severe treatment-refractory antibody positive autoimmune autonomic ganglionopathy after mRNA COVID19 vaccination. Autoimmun. Rev. 2022, 21, 103201. [Google Scholar] [CrossRef]
- Rubin, R. Large Cohort Study Finds Possible Association Between Postural Orthostatic Tachycardia Syndrome and COVID-19 Vaccination but Far Stronger Link With SARS-CoV-2 Infection. JAMA 2023. [Google Scholar] [CrossRef] [PubMed]
- Sheldon, R.S.; Grubb, B.P., II; Olshansky, B.; Shen, W.K.; Calkins, H.; Brignole, M.; Raj, S.R.; Krahn, A.D.; Morillo, C.A.; Stewart, J.M.; et al. 2015 heart rhythm society expert consensus statement on the diagnosis and treatment of postural tachycardia syndrome, inappropriate sinus tachycardia, and vasovagal syncope. Heart Rhythm. 2015, 12, e41–e63. [Google Scholar] [CrossRef]
- Buchhorn, J.; Buchhorn, R. The postural orthostatic stress syndrome in childhood: HRV analysis and the active standing test. Prev. Med. Community Health 2020, 3, 1–7. [Google Scholar]
- Malik, M. Heart rate variability: Standards of measurement, physiological interpretation and clinical use. Task Force of the European Society of Cardiology and the North American Society of Pacing and Electrophysiology. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Buchhorn, R.; Baumann, C.; Gündogdu, S.; Rakowski, U.; Willaschek, C. Diagnosis and management of an inappropriate sinus tachycardia in adolescence based upon a Holter ECG: A retrospective analysis of 479 patients. PLoS ONE 2020, 15, e0238139. [Google Scholar] [CrossRef] [PubMed]
- Hidayat, K.; Yang, J.; Zhang, Z.; Chen, G.C.; Qin, L.Q.; Eggersdorfer, M.; Zhang, W. Effect of omega-3 long-chain polyunsaturated fatty acid supplementation on heart rate: A meta-analysis of randomized controlled trials. Eur. J. Clin. Nutr. 2018, 72, 805–817. [Google Scholar] [CrossRef]
- van Campen, C.; Visser, F.C. Orthostatic Intolerance in Long-Haul COVID after SARS-CoV-2: A Case-Control Comparison with Post-EBV and Insidious-Onset Myalgic Encephalomyelitis/Chronic Fatigue Syndrome Patients. Healthcare 2022, 10, 2058. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.; Pothineni, N.V.K.; Charate, R.; Garg, J.; Elbey, M.; de Asmundis, C.; Lakkireddy, D. Inappropriate Sinus Tachycardia: Etiology, Pathophysiology, and Management: JACC Review Topic of the Week. J. Am. Coll. Cardiol. 2022, 79, 2450–2462. [Google Scholar] [CrossRef] [PubMed]
- Raj, S.R.; Fedorowski, A.; Sheldon, R.S. Diagnosis and management of postural orthostatic tachycardia syndrome. CMAJ Can. Med. Assoc. J./J. L’association Med. Can. 2022, 194, E378–E385. [Google Scholar] [CrossRef] [PubMed]
- Sotzny, F.; Filgueiras, I.S.; Kedor, C.; Freitag, H.; Wittke, K.; Bauer, S.; Scheibenbogen, C. Dysregulated autoantibodies targeting vaso- and immunoregulatory receptors in Post COVID Syndrome correlate with symptom severity. Front. Immunol. 2022, 13, 981532. [Google Scholar] [CrossRef]
- Buchhorn, R.; Meyer, C.; Schulze-Forster, K.; Junker, J.; Heidecke, H. Autoantibody release in children after corona virus mRNA vaccination: A risk factor of multisystem inflammatory syndrome? Vaccines 2021, 9, 1353. [Google Scholar] [CrossRef]
- Hall, J.; Bourne, K.M.; Vernino, S.; Hamrefors, V.; Kharraziha, I.; Nilsson, J.; Raj, S.R. Detection of G Protein-Coupled Receptor Autoantibodies in Postural Orthostatic Tachycardia Syndrome Using Standard Methodology. Circulation 2022, 146, 613–622. [Google Scholar] [CrossRef]
- Buchhorn, R. Dysautonomia in Children with Post-Acute Sequelae of Coronavirus 2019 Disease and/or Vaccination. Vaccines 2022, 10, 1686. [Google Scholar] [CrossRef]
- Lindgren, M.; Robertson, J.; Adiels, M.; Schaufelberger, M.; Åberg, M.; Torén, K.; Rosengren, A. Resting heart rate in late adolescence and long term risk of cardiovascular disease in Swedish men. Int. J. Cardiol. 2018, 259, 109–115. [Google Scholar] [CrossRef]
- Lessmeier, T.J.; Gamperling, D.; Johnson-Liddon, V.; Fromm, B.S.; Steinman, R.T.; Meissner, M.D.; Lehmann, M.H. Unrecognized paroxysmal supraventricular tachycardia. Potential for misdiagnosis as panic disorder. Arch. Intern. Med. 1997, 157, 537–543. [Google Scholar] [CrossRef] [PubMed]
- Arnold, A.C.; Haman, K.; Garland, E.M.; Raj, V.; Dupont, W.D.; Biaggioni, I.; Raj, S.R. Cognitive dysfunction in postural tachycardia syndrome. Clin. Sci. 2015, 128, 39–45. [Google Scholar] [CrossRef]
- Knoop, I.; Picariello, F.; Jenkinson, E.; Gall, N.; Chisari, C.; Moss-Morris, R. Self-reported symptom burden in postural orthostatic tachycardia syndrome (POTS): A narrative review of observational and interventional studies. Auton. Neurosci. Basic Clin. 2023, 244, 103052. [Google Scholar] [CrossRef]
- Arnold, A.C.; Okamoto, L.E.; Diedrich, A.; Paranjape, S.Y.; Raj, S.R.; Biaggioni, I.; Gamboa, A. Low-dose propranolol and exercise capacity in postural tachycardia syndrome: A randomized study. Neurology 2013, 80, 1927–1933. [Google Scholar] [CrossRef] [PubMed]
- Raj, S.R.; Black, B.K.; Biaggioni, I.; Paranjape, S.Y.; Ramirez, M.; Dupont, W.D.; Robertson, D. Propranolol decreases tachycardia and improves symptoms in the postural tachycardia syndrome: Less is more. Circulation 2009, 120, 725–734. [Google Scholar] [CrossRef] [PubMed]
- Cappato, R.; Castelvecchio, S.; Ricci, C.; Bianco, E.; Vitali-Serdoz, L.; Gnecchi-Ruscone, T.; Lupo, P.P. Clinical efficacy of ivabradine in patients with inappropriate sinus tachycardia: A prospective, randomized, placebo-controlled, double-blind, crossover evaluation. J. Am. Coll. Cardiol. 2012, 60, 1323–1329. [Google Scholar] [CrossRef] [PubMed] [Green Version]




| Healthy Control | Inappropriate Sinus Tachycardia | Postural Orthostatic Tachycardia | |||
|---|---|---|---|---|---|
| Prior to Pandemic | PASC/Post Vaccination | Prior to Pandemic | PASC/Post Vaccination | ||
| Patients | 47 | 20 | 13 | 44 | 15 |
| Age [Years] | 14.2 ± 3.8 | 14.7 ± 2.5 | 15.4 ± 2.9 | 14.9 ± 2.2 | 14.4 ± 2.7 |
| Height [cm] | 160.1 ± 14.2 | 160.9 ± 9.8 | 162.1 ± 8.3 | 167 ± 10 | 165 ± 12 |
| Weight [kg] | 52.6 ± 14.3 | 48.2 ± 7.7 | 53.0 ± 12.3 | 55.4 ± 11.6 | 54.5 ± 12.7 |
| Sys. BP [mmHg] | 114.5 ± 9.2 | 119.4 ± 9.5 | 129.1 ± 7.3 ** | 116.7 ± 9.3 | 110.3 ± 2.8 * |
| Diast. BP [mmHg] | 61.7 ± 11.2 | 73.6 ± 9.5 | 80.4 ± 8.6 * | 63.5 ± 11.6 | 69.5 ± 6.0 |
| FS [%] | 38.9 ± 6.2 | 37.0 ± 3.6 | 44.9 ± 5.3 | 37.8 ± 4.8 * | |
| LVIMP | 0.13 ± 0.1 | 0.20 ± 0.1 | 0.22 ± 0.08 | 0.1 ± 0.07 ** | |
| HR Increase | 16.2 ± 7.1 | 25.7 ± 14.5 | 21.9 ± 12.6 | 43.3 ± 8.7 | 43.0 ± 5.8 |
| Lying HR | 73.6 ± 12.5 | 107.9 ± 16.2 | 101.9 ± 9.2 | 72.5 ± 10.9 | 69.2 ± 13.2 |
| Standing HR | 89.8 ± 13.2 | 133.6 ± 16.4 | 123.8 ± 12.6 * | 115.6 ± 15.3 | 112.3 ± 13.4 |
| rMSSD Lying | 85.1 ± 56.2 | 19.6 ± 15.2 | 22.8 ± 14.1 | 63.4 ± 41.4 | 88.7 ± 46.0 |
| rMSSD Standing | 40.4 ± 22.7 | 12.5 ± 15.2 | 15.5 ± 17.2 | 16.4 ± 9.4 | 24.5 ± 29.0 |
| Stress Index Lying | 98 ± 85 | 638 ± 654 | 350 ± 205 | 151 ± 252 | 75 ± 80 |
| Stress Index Standing | 168 ± 116 | 1111 ± 666 | 734 ± 632 | 561 ± 437 | 607 ± 578 |
| HF lying | 2920 ± 4403 | 210 ± 201 | 383 ± 517 | 2151 ± 4315 | 3798 ± 5574 |
| HF standing | 949 ± 1222 | 104 ± 170 | 212 ± 452 | 123 ± 126 | 813 ± 1981 |
| LF lying | 1518 ± 2795 | 226 ± 153 | 449 ± 364 | 1280 ± 1585 | 1021 ± 569 |
| LF standing | 1331 ± 1115 | 527 ± 413 | 242 ± 201 | 570 ± 632 | 1047 ± 1494 |
| VLF lying | 1553 ± 2182 | 639 ± 818 | 457 ± 368 | 1094 ± 1867 | 2103 ± 2483 |
| VLF standing | 1299± 1506 | 242 ± 201 | 455 ± 421 | 451 ± 440 | 864 ± 1245 |
| TP lying | 5819 ± 6203 | 876 ± 1164 | 1290 ± 349 | 4509 ± 6300 | 6435 ± 5318 |
| TP standing | 3579 ± 3012 | 349 ± 1132 | 1194 ± 1132 | 1145 ± 980 | 2726 ± 3910 |
| LF/HF Lying | 0.97 ± 1.10 | 3.08 ± 2.8 | 2.61 ± 2.67 | 1.12 ± 0.82 | 0.71 ± 0.51 |
| LF/HF Standing | 2.54 ± 1.95 | 4.85 ± 4.8 | 5.54 ± 2.79 | 7.66 ± 4.89 | 5.79 ± 6.94 |
| Propranolol + O3-FA (n = 18) | Ivabradine + O3-FA (n = 11) | O3-FA without Pharmacotherapy (n = 7) | ||||
| Postural Orthostatic Tachycardia Syndrome | ||||||
| HR Increase | 42.2 ± 15.9 | 27.2 ± 17.4 *** | 37.5 ± 16.4 | 23.6 ± 8.12 * | 44.0 ± 11.9 | 25.6 ± 8.4 * |
| HR Lying | 85.3 ± 21.4 | 75.8 ± 11.8 | 80.6 ± 17.9 | 77.9 ± 14.5 | 82.2 ± 17.6 | 84.3 ± 13.9 |
| HR Standing | 127.6 ± 18.1 | 101.9 ± 18.9 *** | 118.2 ± 15.0 | 101.4 ± 16.9 ** | 126.2 ± 11.4 | 109.9 ± 16.9 * |
| RMSSD Lying | 44.2 ± 32.7 | 67.0 ± 59.4 | 52.0 ± 17.0 | 44.0 ± 6.0 | 87.6 ± 35.0 | 54.6 ± 12.4 |
| RMSSD Standing | 11.3 ± 9.8 | 32.7 ± 34.4 * | 17.5 ± 3.8 | 24.5 ±9.5 | 11.8 ± 3.2 | 27.2 ± 12.6 |
| Stress Index Lying | 314 ± 521 | 122 ± 112 | 232 ± 73 | 185 ± 38 | 192 ± 182 | 146 ± 111 |
| Stress Index Standing | 989 ± 719 | 401 ± 374 ** | 609 ± 123 | 548 ± 197 | 855 ± 160 | 561 ± 217 |
| Inappropriate Sinus Tachycardia | ||||||
| Propranolol + O3-FA (n = 14) | Ivabradine + O3-FA (n = 6) | O3-FA without Pharmacotherapy (n = 11) | ||||
| HR Increase | 29.3 ± 16.0 | 19.4 ± 15.6 | 25.3 ± 11.6 | 21.2 ± 15.7 | 25.1 ± 12.5 | 23.5 ± 9.7 |
| HR Lying | 102.7 ± 20.8 | 81.6 ± 10.1 ** | 103.3 ± 12.2 | 84.2 ± 8.4 *** | 96.4 ± 8.6 | 88.6 ± 7.9 * |
| HR Standing | 132.1 ± 16.5 | 101.0 ± 18.8 *** | 128.6 ± 12.2 | 105.4 ± 14.6 ** | 121.5 ± 11.9 | 112.1 ± 14.9 * |
| RMSSD Lying | 26.7 ± 22.6 | 63.8 ± 54.5 ** | 15.0 ± 7.9 | 26.8 ± 14.3 * | 28.3 ± 14.3 | 40.6 ± 21.1 |
| RMSSD Standing | 10.7 ± 7.9 | 46.3 ± 39.1 ** | 11.2 ± 8.6 | 13.8 ±8.1 | 19.1 ± 18.1 | 17.9 ± 10.4 |
| Stress Index Lying | 573 ± 729 | 123 ± 81 * | 667 ± 633 | 272 ± 179 | 313 ± 186 | 207 ± 159 |
| Stress Index Standing | 1126 ± 759 | 403 ± 406 ** | 1083 ± 801 | 617 ± 353 | 613 ± 384 | 753 ± 1262 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Buchhorn, R. Therapeutic Approaches to Dysautonomia in Childhood, with a Special Focus on Long COVID. Children 2023, 10, 316. https://doi.org/10.3390/children10020316
Buchhorn R. Therapeutic Approaches to Dysautonomia in Childhood, with a Special Focus on Long COVID. Children. 2023; 10(2):316. https://doi.org/10.3390/children10020316
Chicago/Turabian StyleBuchhorn, Reiner. 2023. "Therapeutic Approaches to Dysautonomia in Childhood, with a Special Focus on Long COVID" Children 10, no. 2: 316. https://doi.org/10.3390/children10020316
APA StyleBuchhorn, R. (2023). Therapeutic Approaches to Dysautonomia in Childhood, with a Special Focus on Long COVID. Children, 10(2), 316. https://doi.org/10.3390/children10020316





