Patient-Specific 3D-Printed Models in Pediatric Congenital Heart Disease
Abstract
1. Introduction
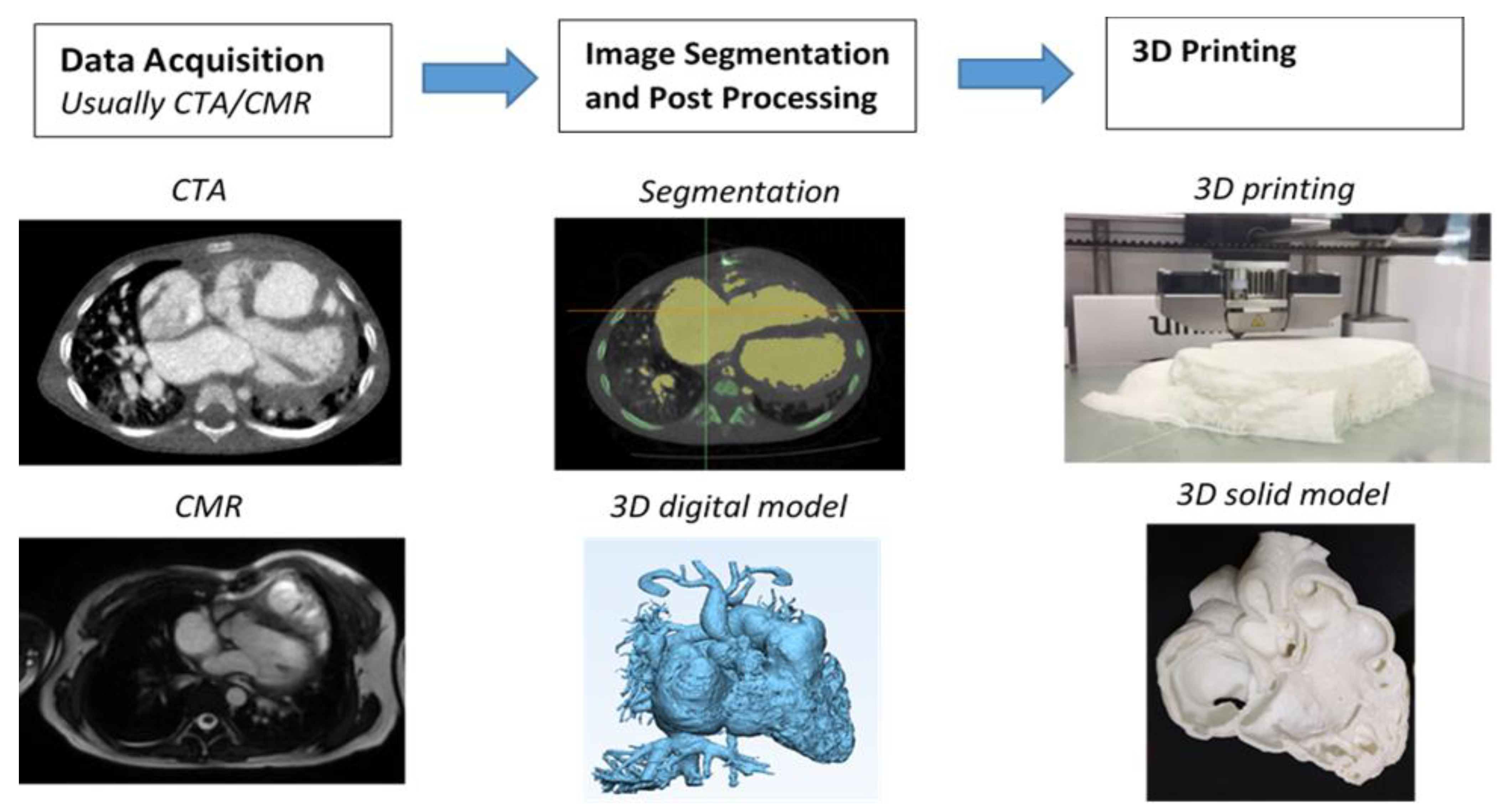
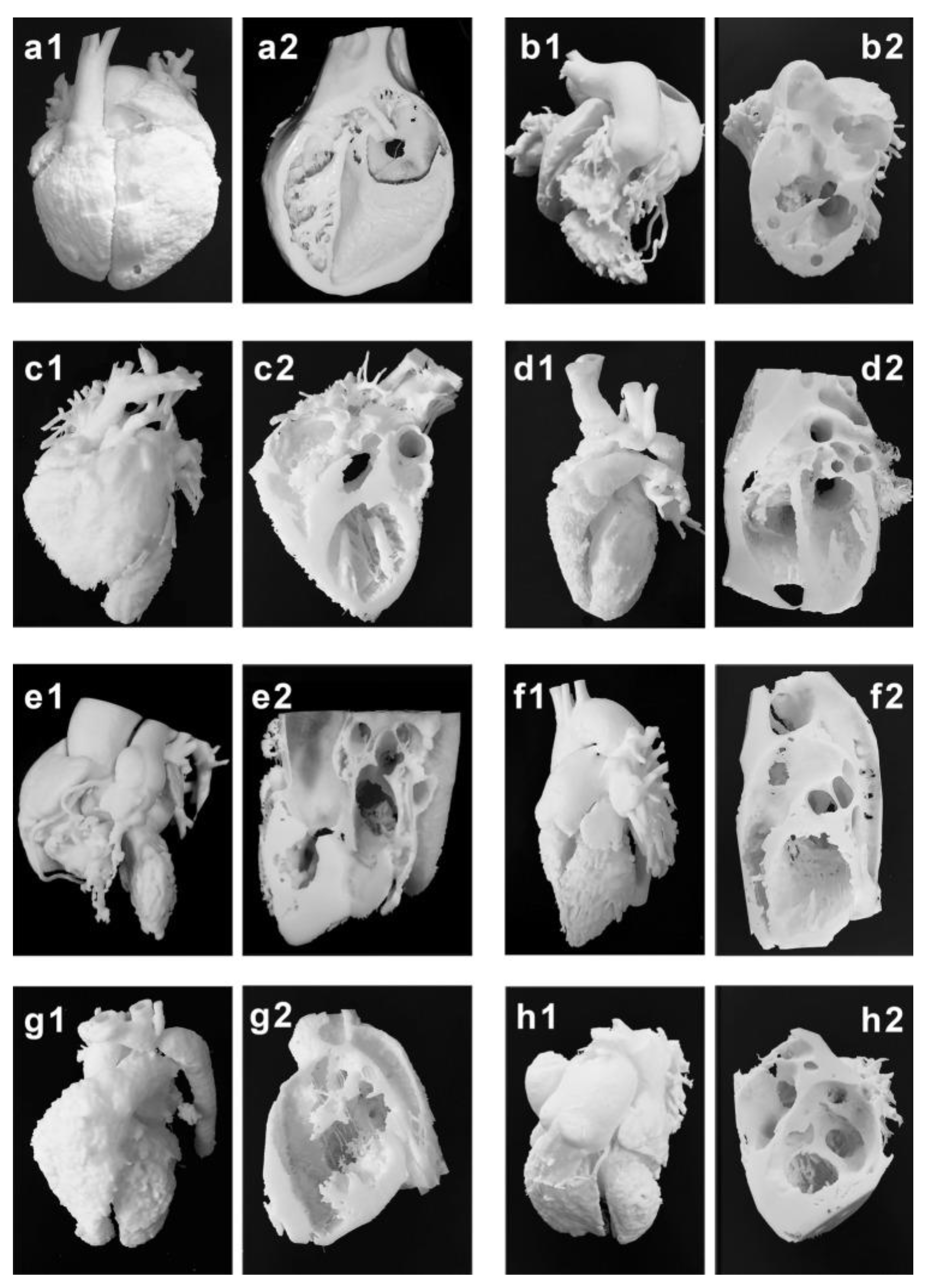
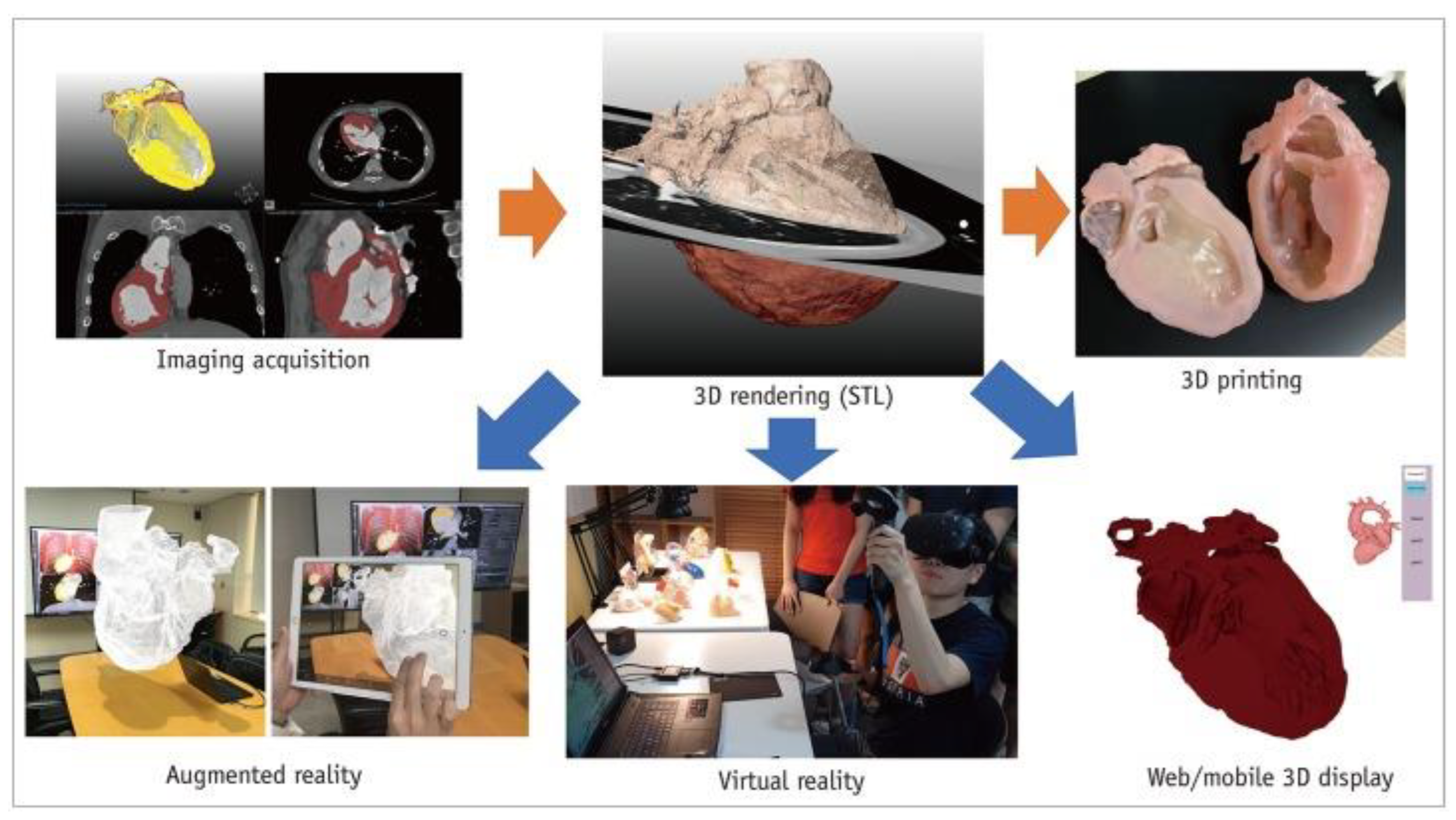
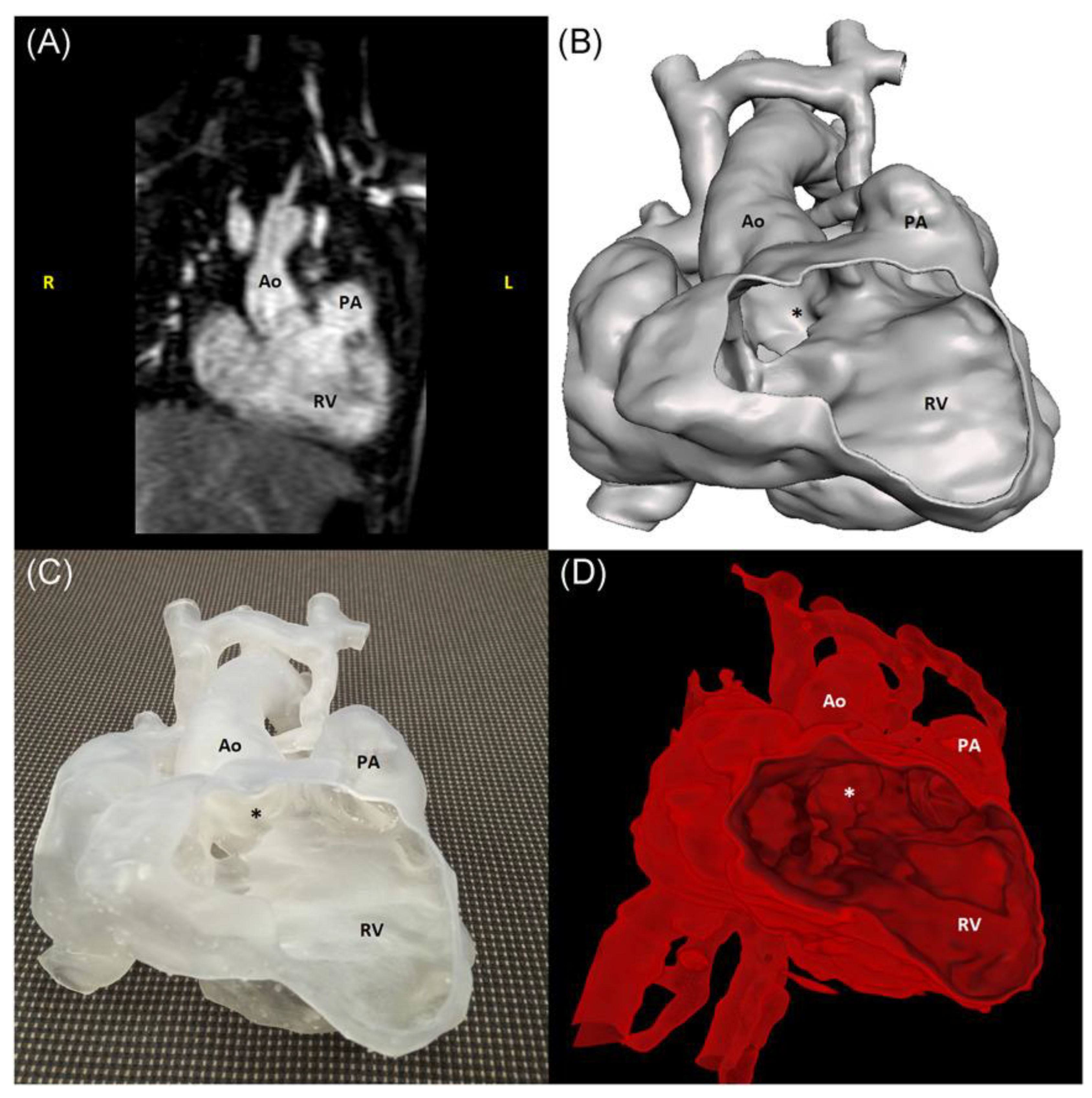
2. Generation of 3D-Printed Heart Models
3. Accuracy of 3D-Printed Heart Models Derived from Imaging Modalities
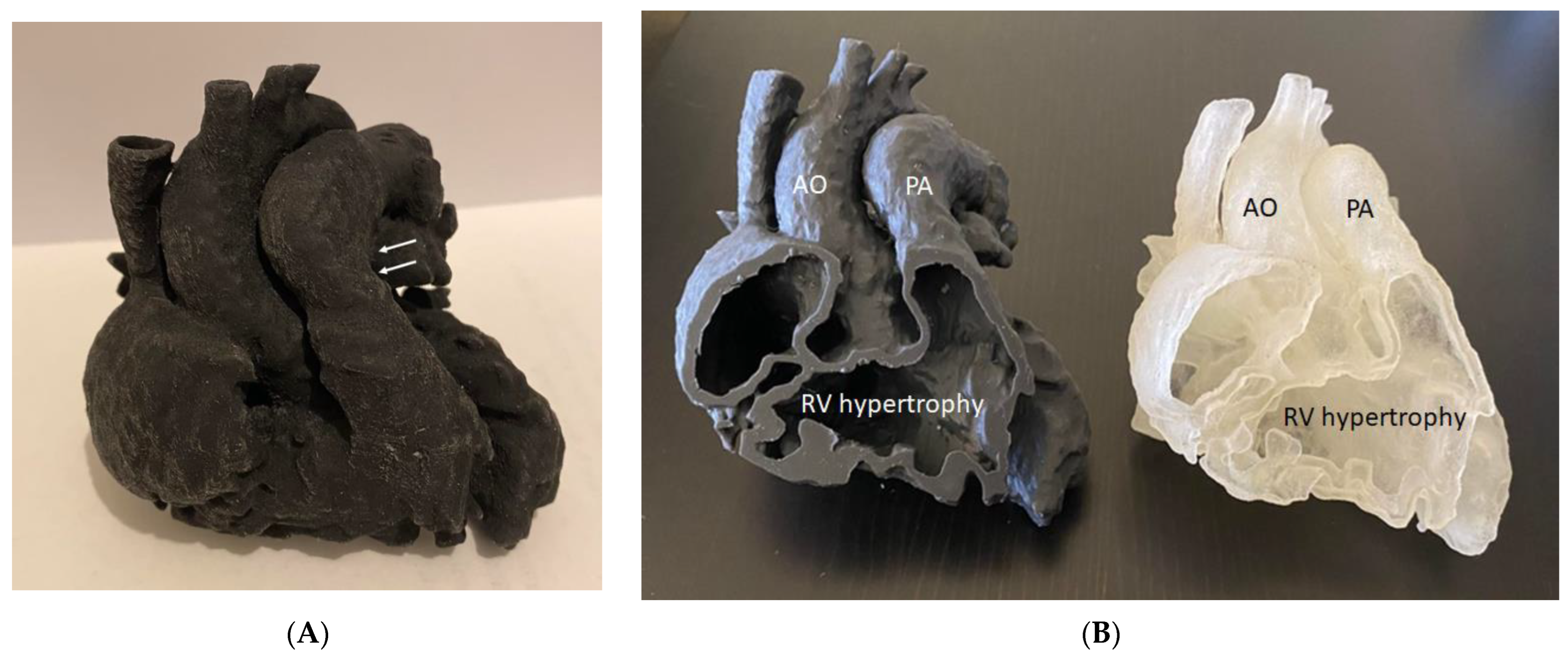
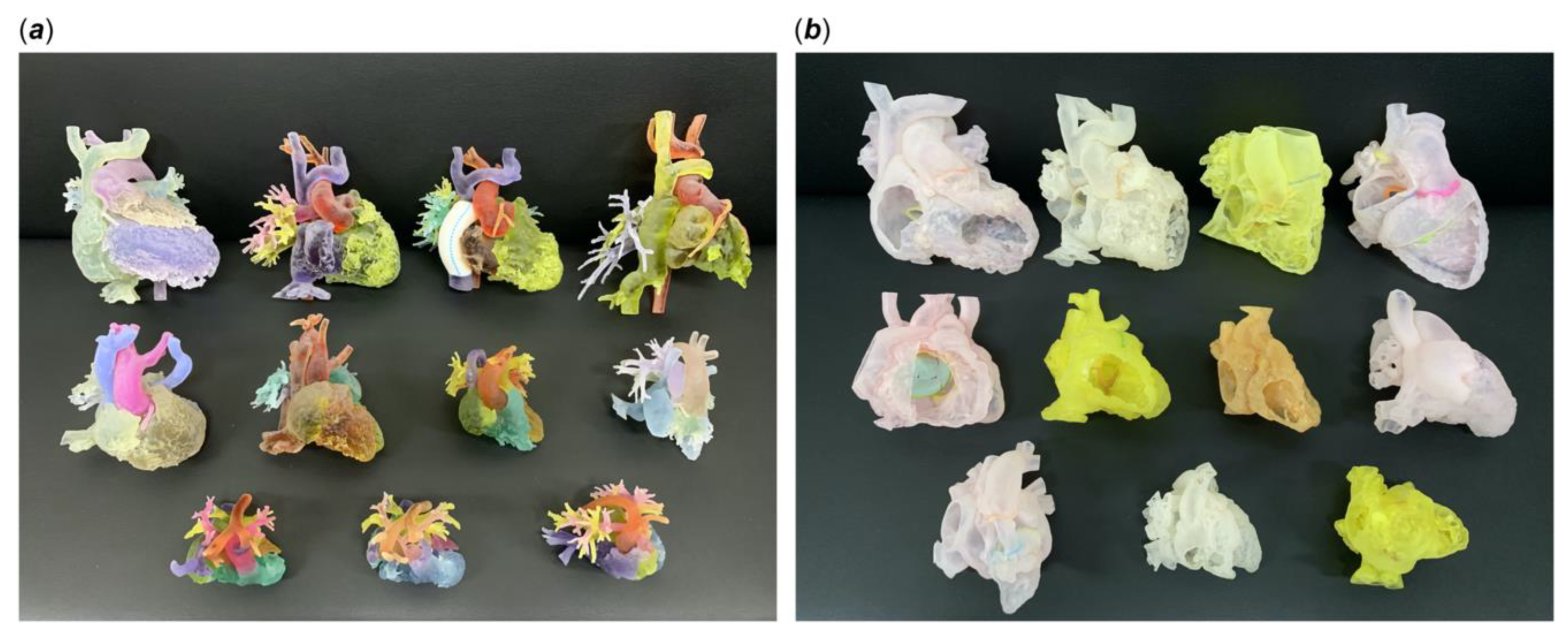
4. Three-Dimensional-Printing Materials for Printing Patient-Specific Models
5. Educational and Clinical Value of 3D-Printed Heart Models in CHD
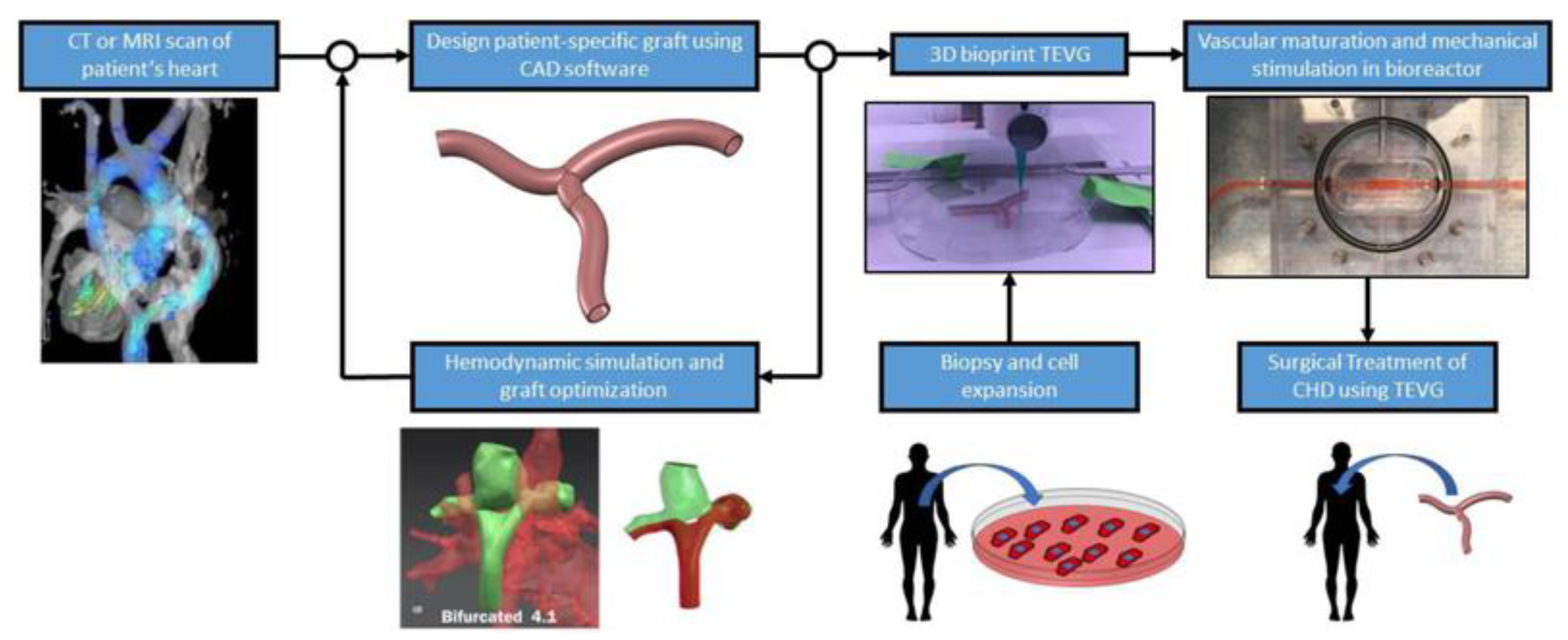
6. 3D-Printed Models in CHD: Clinical Applications
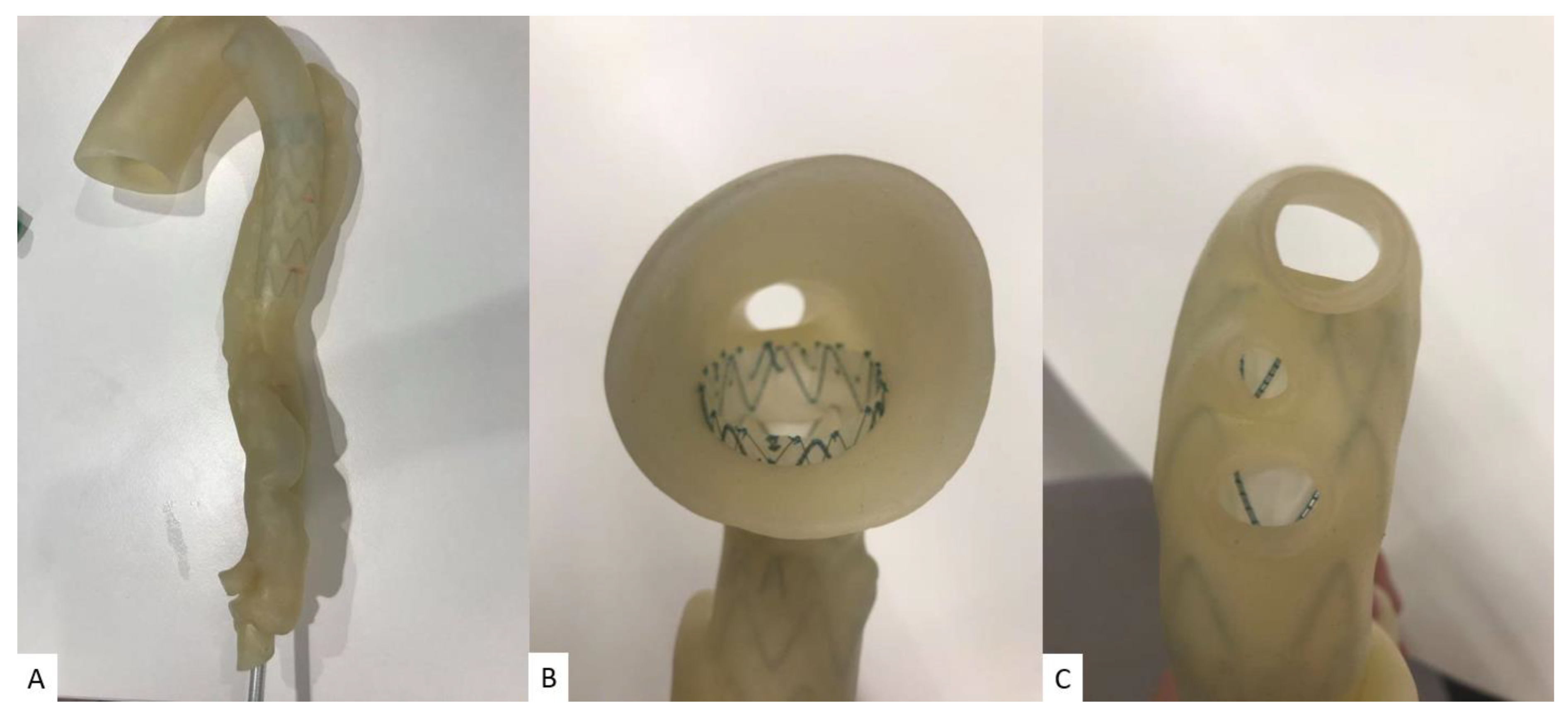
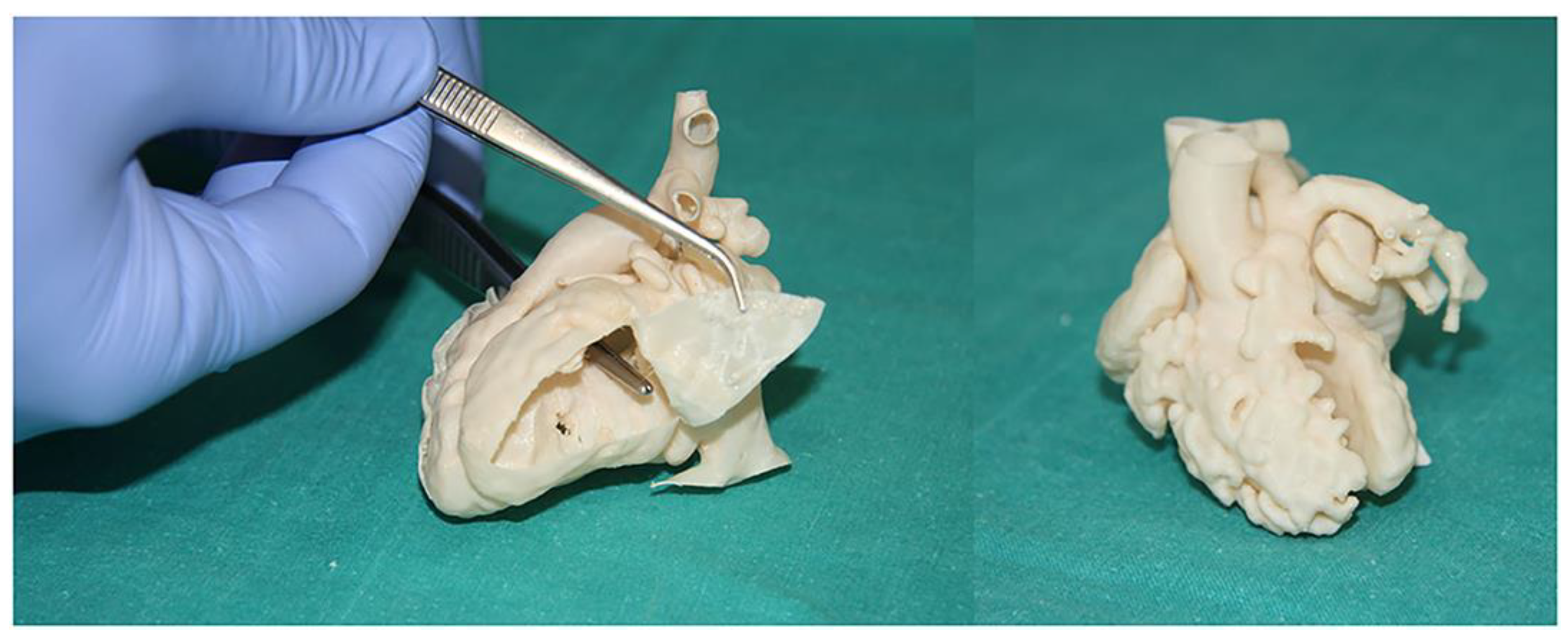
6.1. Pre-Surgical Planning of CHD Surgery
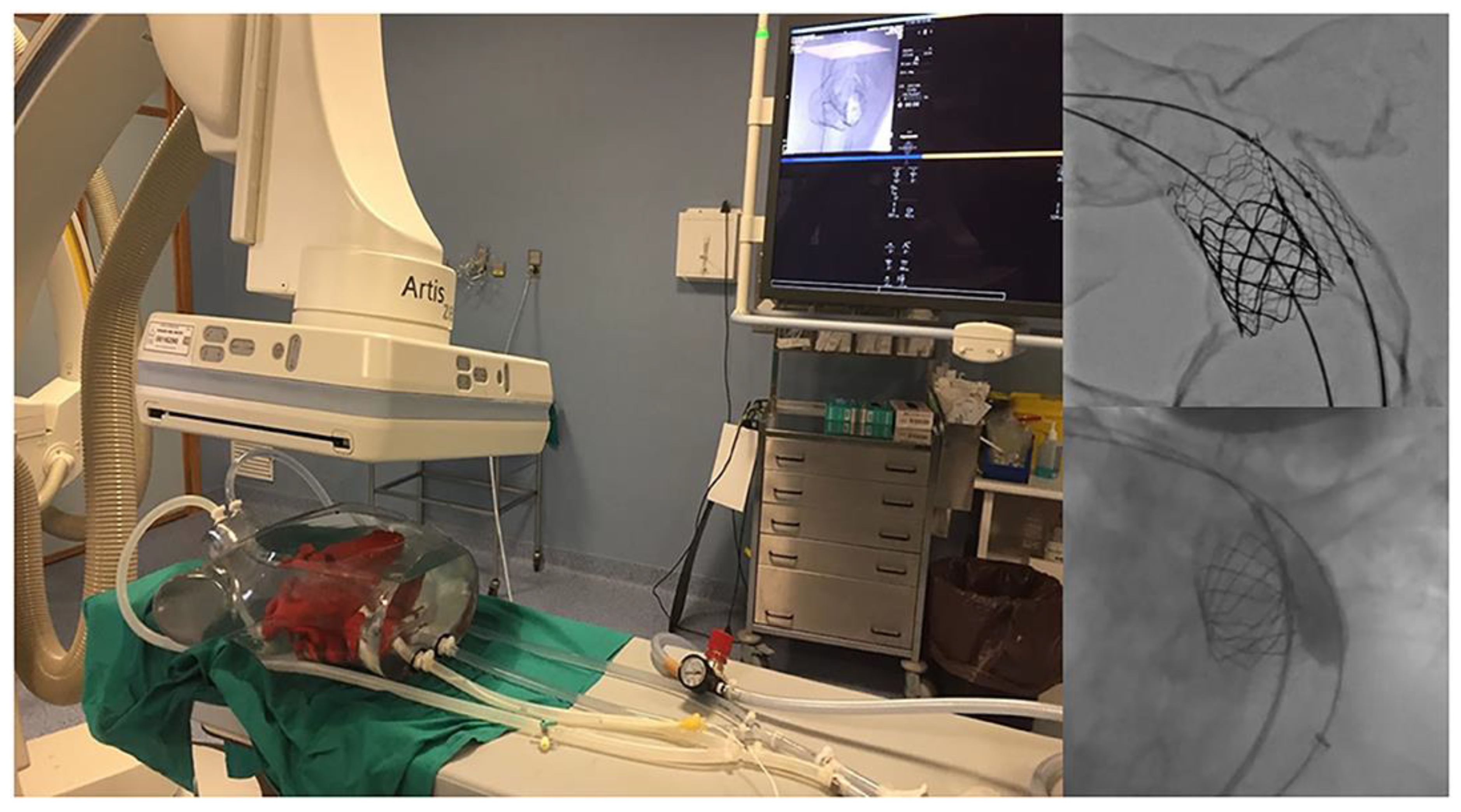
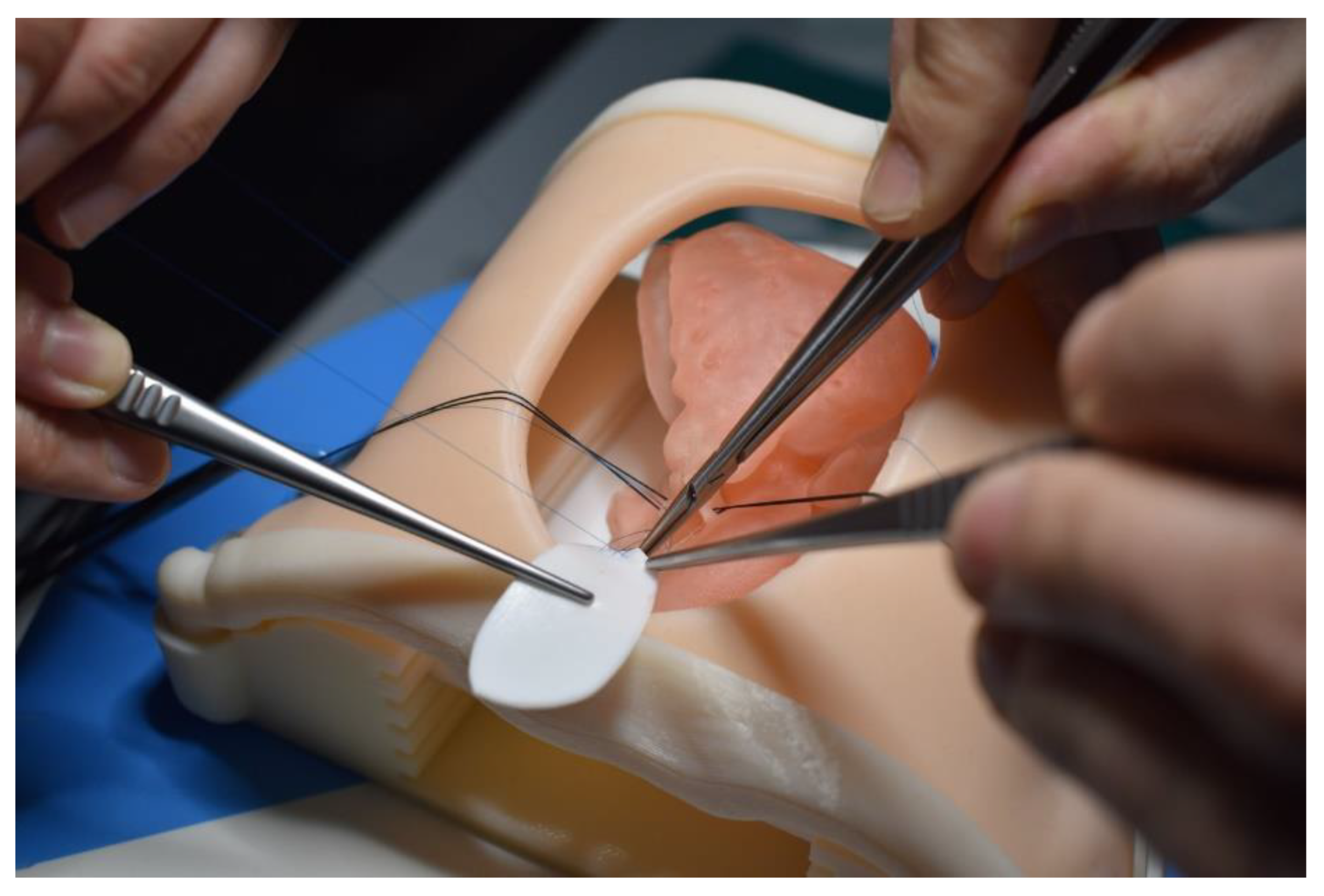
6.2. Hands-on Surgical Training for Congenital Heart Surgery Procedures and Medical Education
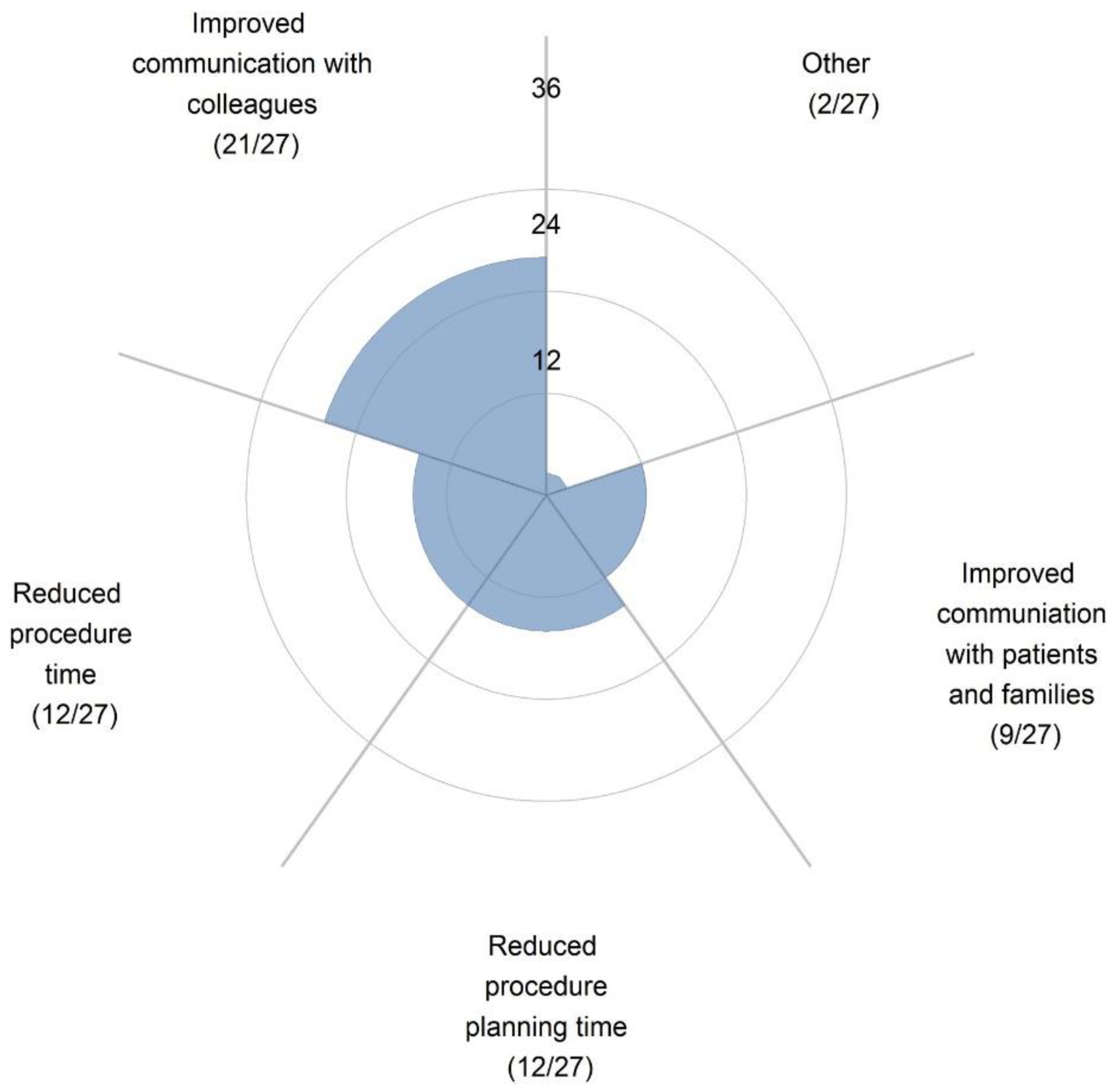
6.3. Improving Physician–Patient Communication/Facilitating Communication with Colleagues
7. Limitations, Challenges and Future Directions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Giannopoulos, A.A.; Steigner, M.L.; George, E.; Barile, M.; Hunsaker, A.R.; Rybicki, F.J.; Mitsouras, D. Cardiothoracic applications of 3-dimensional printing. J. Thorac. Imaging. 2016, 31, 253–272. [Google Scholar] [CrossRef]
- Witowski, J.; Wake, N.; Grochowska, A.; Sun, Z.; Budzyński, A.; Major, P.; Popiela, T.J.; Pędziwiatr, M. Investigating accuracy of 3D printed liver models with computed tomography. Quant. Imaging Med. Surg. 2019, 9, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Witowski, J.S.; Pędziwiatr, M.; Major, P.; Budzyński, A. Cost-effective, personalized, 3D-printed liver model for preoper-ative planning before laparoscopic liver hemihepatectomy for colorectal cancer metastases. Int. J. Comput. Assist. Radiol. Surg. 2017, 12, 2047–2054. [Google Scholar] [CrossRef]
- Costello, J.P.; Olivieri, L.; Krieger, A.; Thabit, O.; Marshall, M.B.; Yoo, S.-J.; Kim, P.C.; Jonas, R.A.; Nath, D.S. Utilizing Three-Dimensional Printing Technology to Assess the Feasibility of High-Fidelity Synthetic Ventricular Septal Defect Models for Simulation in Medical Education. World J. Pediatr. Congenit. Heart Surg. 2014, 5, 421–426. [Google Scholar] [CrossRef] [PubMed]
- Costello, J.P.; Olivieri, L.J.; Su, L.; Krieger, A.; Alfares, F.; Thabit, O.; Marshall, M.B.; Yoo, S.-J.; Kim, P.C.; Jonas, R.A.; et al. Incorporating Three-dimensional Printing into a Simulation-based Congenital Heart Disease and Critical Care Training Curriculum for Resident Physicians. Congenit. Heart Dis. 2014, 10, 185–190. [Google Scholar] [CrossRef] [PubMed]
- Javan, R.; Zeman, M.N. A Prototype Educational Model for Hepatobiliary Interventions: Unveiling the Role of Graphic Designers in Medical 3D Printing. J. Digit. Imaging 2017, 31, 133–143. [Google Scholar] [CrossRef] [PubMed]
- Sun, Z.; Lau, I.; Wong, Y.H.; Yeong, C.H. Personalized Three-Dimensional Printed Models in Congenital Heart Disease. J. Clin. Med. 2019, 8, 522. [Google Scholar] [CrossRef] [PubMed]
- Bagaria, V.; Bhansali, R.; Pawar, P. 3D printing-creating a blueprint for the future of orthopedics: Current concept review and the road ahead! J. Clin. Ortho. Trauma. 2018, 9, 207. [Google Scholar] [CrossRef]
- Skelley, N.W.; Hagerty, M.P.; Stannard, J.T.; Feltz, K.P.; Ma, R. Sterility of 3D-Printed Orthopedic Implants Using Fused Deposition Modeling. Orthopedics 2020, 43, 46–51. [Google Scholar] [CrossRef]
- Anwar, S.; Singh, G.K.; Miller, J.; Sharma, M.; Manning, P.; Billadello, J.J.; Eghtesady, P.; Woodard, P.K. 3D Printing is a Transformative Technology in Congenital Heart Disease. JACC Basic Transl. Sci. 2018, 3, 294–312. [Google Scholar] [CrossRef]
- Gallo, M.; D’Onofrio, A.; Tarantini, G.; Nocerino, E.; Remondino, F.; Gerosa, G. 3D-printing model for complex aortic transcatheter valve treatment. Int. J. Cardiol. 2016, 210, 139–140. [Google Scholar] [CrossRef] [PubMed]
- Ripley, B.; Kelil, T.; Cheezum, M.K.; Gonçalves, A.; Di Carli, M.F.; Rybicki, F.J.; Steigner, M.; Mitsouras, D.; Blankstein, R. 3D printing based on cardiac CT assists anatomic visualization prior to transcatheter aortic valve replacement. J. Cardiovasc. Comput. Tomogr. 2015, 10, 28–36. [Google Scholar] [CrossRef] [PubMed]
- Lau, I.; Sun, Z. Three-dimensional printing in congenital heart disease: A systematic review. J. Med. Radiat. Sci. 2018, 65, 226–236. [Google Scholar] [CrossRef]
- Bhatla, P.; Tretter, J.T.; Chikkabyrappa, S.; Chakravarti, S.; Mosca, R.S. Surgical planning for a complex double-outlet right ventricle using 3D printing. Echocardiography 2017, 34, 802–804. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Milano, E.G.; Capelli, C.; Wray, J.; Shearn, A.I.; Caputo, M.; Bucciarelli-Ducci, C.; Taylor, A.M.; Schievano, S. Three-dimensional printing in congenital heart disease: Considerations on training and clinical implementation from a teaching session. Int. J. Artif. Organs 2019, 42, 595–599. [Google Scholar] [CrossRef]
- Lau, I.W.W.; Sun, Z. Dimensional Accuracy and Clinical Value of 3D Printed Models in Congenital Heart Disease: A Systematic Review and Meta-Analysis. J. Clin. Med. 2019, 8, 1483. [Google Scholar] [CrossRef]
- Anwar, S.; Rockefeller, T.; Raptis, D.A.; Woodard, P.K.; Eghtesady, P. 3D Printing Provides a Precise Approach in the Treatment of Tetralogy of Fallot, Pulmonary Atresia with Major Aortopulmonary Collateral Arteries. Curr. Treat. Options Cardiovasc. Med. 2018, 20, 5. [Google Scholar] [CrossRef]
- Gosnell, J.; Pietila, T.; Samuel, B.P.; Kurup, H.K.N.; Haw, M.P.; Vettukattil, J.J. Integration of Computed Tomography and Three-Dimensional Echocardiography for Hybrid Three-Dimensional Printing in Congenital Heart Disease. J. Digit. Imaging 2016, 29, 665–669. [Google Scholar] [CrossRef]
- Loke, Y.-H.; Harahsheh, A.S.; Krieger, A.; Olivieri, L.J. Usage of 3D models of tetralogy of Fallot for medical education: Impact on learning congenital heart disease. BMC Med. Educ. 2017, 17, 54–61. [Google Scholar] [CrossRef]
- Sun, Z. Clinical Applications of Patient-Specific 3D Printed Models in Cardiovascular Disease: Current Status and Future Directions. Biomolecules 2020, 10, 1577. [Google Scholar] [CrossRef]
- Gómez-Ciriza, G.; Gómez-Cía, T.; Rivas-González, J.A.; Forte, M.N.V.; Valverde, I. Affordable Three-Dimensional Printed Heart Models. Front. Cardiovasc. Med. 2021, 8, 642011. [Google Scholar] [CrossRef] [PubMed]
- Moore, R.A.; Riggs, K.W.; Kourtidou, S.; Schneider, K.; Szugye, N.; Troja, W.; D’Souza, G.; Rattan, M.; Bryant, R., 3rd; Taylor, M.D.; et al. Three-dimensional printing and virtual surgery for congenital heart procedural planning. Birth. Defects. Res. 2018, 110, 1082–1090. [Google Scholar] [CrossRef] [PubMed]
- Kiraly, L.; Shah, N.C.; Abdullah, O.; Al-Ketan, O.; Rowshan, R. Three-Dimensional Virtual and Printed Prototypes in Complex Congenital and Pediatric Cardiac Surgery—A Multidisciplinary Team-Learning Experience. Biomolecules 2021, 11, 1703. [Google Scholar] [CrossRef] [PubMed]
- Garas, M.; Vacccarezza, M.; Newland, G.; McVay-Doonbusch, K.; Hasani, J. 3D-printed speciamens as a valuable tool in anatomy education: A pilot study. Ann. Anat. 2018, 219, 57–64. [Google Scholar] [CrossRef]
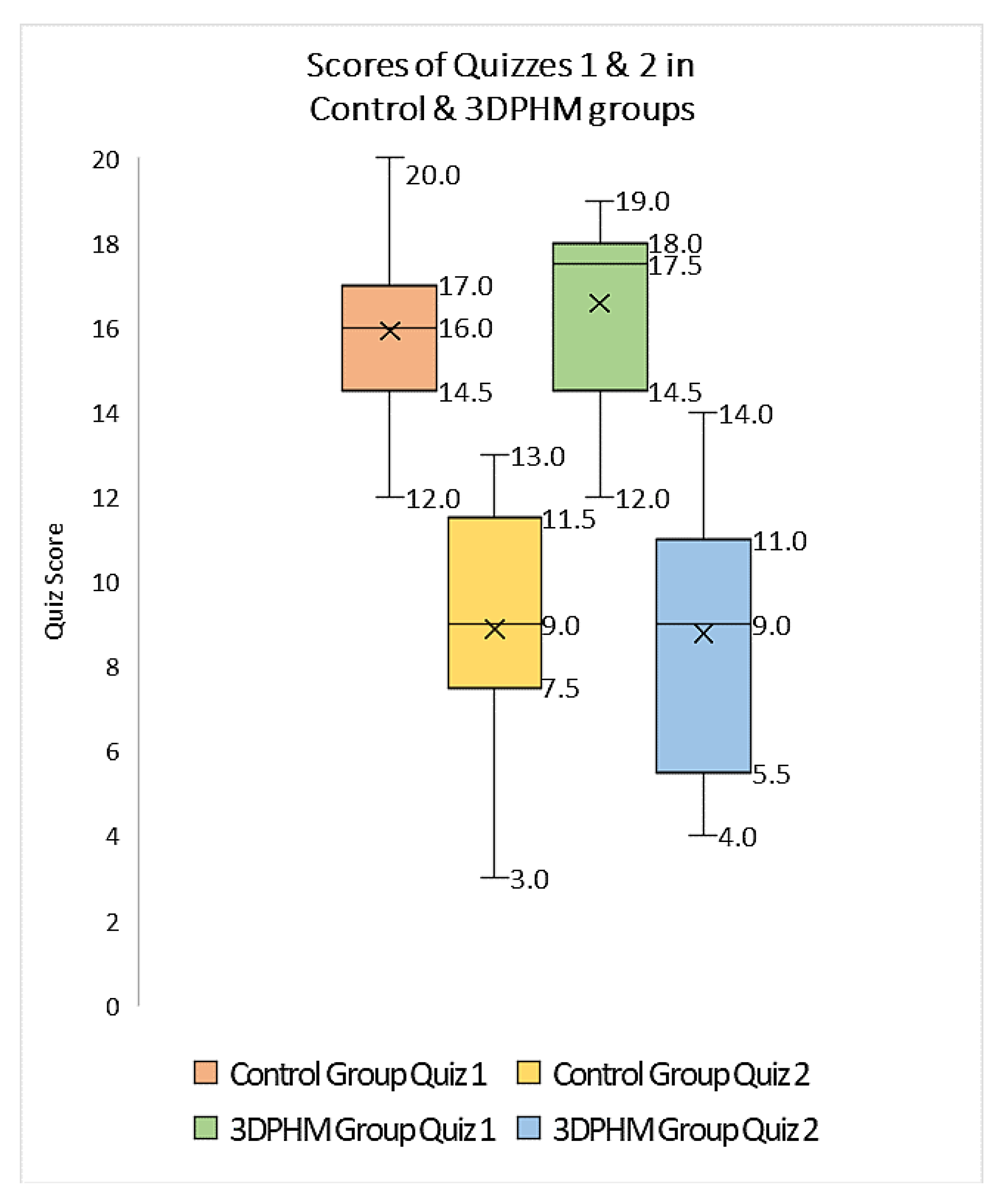
- Lau, I.; Sun, Z. The role of 3D printed heart models in immediate and long-term knowledge retention in medical education. Rev. Cardiovasc. Med. 2022, 23, 022. [Google Scholar] [CrossRef] [PubMed]
- Karsenty, C.; Guitarte, A.; Dulac, Y.; Briot, J.; Hascoet, S.; Vincent, R.; Delepaul, B.; Vignaud, P.; Djeddai, C.; Hadeed, K.; et al. The usefulness of 3D printed heart models for medical student education in congenital heart disease. BMC. Med. Edc. 2021, 21, 480. [Google Scholar] [CrossRef] [PubMed]
- Lim, K.H.A.; Loo, Z.Y.; Goldie, S.J.; Adams, J.W.; McMenamin, P.G. Use of 3D printed models in medical education: A randomized control trial comparing 3D prints versus cadaveric materials for learning external cardiac anatomy. Anat. Sci. Educ. 2015, 9, 213–221. [Google Scholar] [CrossRef] [PubMed]
- Smerling, J.; Marboe, C.C.; Lefkowitch, J.H.; Pavlicova, M.; Bacha, E.; Einstein, A.J.; Naka, Y.; Glickstein, J.; Farooqi, K.M. Utility of 3D Printed Cardiac Models for Medical Student Education in Congenital Heart Disease: Across a Spectrum of Disease Severity. Pediatr. Cardiol. 2019, 40, 1258–1265. [Google Scholar] [CrossRef] [PubMed]
- Su, W.; Xiao, Y.; He, S.; Huang, P.; Deng, X. Three-dimensional printing models in congenital heart disease education for medical students: A controlled comparative study. BMC Med. Educ. 2018, 18, 178. [Google Scholar] [CrossRef]
- Lau, I.; Gupta, A.; Sun, Z. Clinical Value of Virtual Reality versus 3D Printing in Congenital Heart Disease. Biomolecules 2021, 11, 884. [Google Scholar] [CrossRef] [PubMed]
- Jones, T.W.; Secker, M.D. Use of 3D models of vascular rings and slings to improve resident education. Congenit. Heart. Dis. 2017, 12, 578–582. [Google Scholar] [CrossRef] [PubMed]
- Krishnasamy, S.; Mokhtar, R.A.R.; Singh, R.; Sivallingam, S.; Abdul Aziz, Y.F.; Mathaneswaran, V. 3D rapid prototyping heart model validation for teaching and learning-A pilot project in a teaching institution. Braz. J. Cardiothorac. Surg. 2021, 36, 707–716. [Google Scholar]
- Valverde, I.; Gomez, G.; Byrne, N.; Anwar, S.; Cerpa, S.M.A.; Talavera, M.M.; Pushparajah, K.; Forte, V.M.N. Criss-cross heart three-dimensional printed models in medical education: A multicentre study on their value as a supporting tool to conventional imaging. Anat. Sci. Educ. 2022, 15, 719–730. [Google Scholar] [CrossRef] [PubMed]
- White, S.C.; Sedler, J.; Jones, T.W.; Seckeler, M. Utility of three-dimensional models in resident education on simple and complex intracardiac congenital heart defects. Congenit. Heart Dis. 2018, 13, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
- Tan, H.; Huang, E.; Deng, X.; Ouyang, S. Application of 3D printing technology combined with PBL teaching model in teaching clinical nursing in congenital heart surgery: A case-control study. Medicine 2021, 100, 20. [Google Scholar] [CrossRef] [PubMed]
- Cantinotti, M.; Valverde, I.; Kutty, S. Three-dimensional printed models in congenital heart disease. Int. J. Cardiovasc. Imaging 2017, 33, 137–144. [Google Scholar] [CrossRef]
- Sun, Z.; Wee, C. 3D Printed Models in Cardiovascular Disease: An Exciting Future to Deliver Personalized Medicine. Micromachines 2022, 13, 1575. [Google Scholar] [CrossRef]
- Liang, J.; Zhao, X.; Pan, G.; Zhang, G.; Zhao, D.; Xu, J.; Li, D.; Lu, B. Comparison of blood pool and myocardial 3D printing in the diagnosis of types of congenital heart disease. Sci. Rep. 2022, 12, 7136. [Google Scholar] [CrossRef]
- Lee, S.; Squelch, A.; Sun, Z. Quantitative Assessment of 3D Printed Model Accuracy in Delineating Congenital Heart Disease. Biomolecules 2021, 11, 270. [Google Scholar] [CrossRef]
- Valverde, I.; Gomez-Ciriza, G.; Hussain, T.; Suarez-Mejias, C.; Velasco-Forte, M.N.; Byrne, N.; Ordoñez, A.; Gonzalez-Calle, A.; Anderson, D.; Hazekamp, M.G.; et al. Three-dimensional printed models for surgical planning of complex congenital heart defects: An international multicentre study. Eur. J. Cardio-Thoracic Surg. 2017, 52, 1139–1148. [Google Scholar] [CrossRef]
- Olejník, P.; Nosal, M.; Havran, T.; Furdova, A.; Cizmar, M.; Slabej, M.; Thurzo, A.; Vitovic, P.; Klvac, M.; Acel, T. Utilisation of three-dimensional printed heart models for operative planning of complex congenital heart defects. Kardiol. Pol. 2017, 75, 495–501. [Google Scholar] [CrossRef]
- Olivieri, L.J.; Krieger, A.; Loke, Y.-H.; Nath, D.S.; Kim, P.C.; Sable, C.A. Three-Dimensional Printing of Intracardiac Defects from Three-Dimensional Echocardiographic Images: Feasibility and Relative Accuracy. J. Am. Soc. Echocardiogr. 2015, 28, 392–397. [Google Scholar] [CrossRef]
- Lau, I.W.W.; Liu, D.; Xu, L.; Fan, Z.; Sun, Z. Clinical value of patient-specific three-dimensional printing of congenital heart disease: Quantitative and qualitative assessments. PLoS ONE 2018, 13, e0194333. [Google Scholar] [CrossRef]
- Mowers, K.L.; Fullerton, J.B.; Hicks, D.; Singh, G.K.; Johnson, M.C.; Anwar, S. 3D echocardiography provides highly accurate 3D printed models in congenital heart disease. Pediatr. Cardiol. 2021, 42, 131–141. [Google Scholar] [CrossRef] [PubMed]
- Parimi, M.; Buelter, J.; Thanugundla, V.; Condoor, S.; Parkar, N.; Danon, S.; King, W. Feasibility and Validity of Printing 3D Heart Models from Rotational Angiography. Pediatr. Cardiol. 2018, 39, 653–658. [Google Scholar] [CrossRef]
- Wu, C.A.; Squelch, A.; Jansen, S.; Sun, Z. Optimization of computed tomography angiography protocols for follow-up type B aortic dissection patients by using 3D printed model. Appl. Sci. 2021, 11, 6844. [Google Scholar] [CrossRef]
- Valverde, I.; Gomez, G.; Gonzalez, A.; Suárez-Mejías, C.; Adsuar, A.; Coserria, J.F.; Uribe, S.; Gomez-Cia, T.; Hosseinpour, A.R. Three-dimensional patient-specific cardiac model for surgical planning in Nikaidoh procedure. Cardiol. Young 2014, 25, 698–704. [Google Scholar] [CrossRef] [PubMed]
- Garekar, S.; Bharati, A.; Chokhandre, M.; Mali, S.; Trivedi, B.; Changela, V.P.; Solanki, N.; Gaikwad, S.; Agarwal, V. Clinical Application and Multidisciplinary Assessment of Three Dimensional Printing in Double Outlet Right Ventricle with Remote Ventricular Septal Defect. World J. Pediatr. Congenit. Heart Surg. 2016, 7, 344–350. [Google Scholar] [CrossRef]
- Lau, I.; Wong, Y.H.; Yeong, C.H.; Aziz, Y.F.A.; Sari, N.A.; Hashim, S.A.; Sun, Z. Quantitative and qualitative comparison of low- and high-cost 3D-printed heart models. Quant. Imaging Med. Surg. 2019, 9, 107–114. [Google Scholar] [CrossRef]
- Illmann, C.F.; Hosking, M.; Harris, K.C. Utility and Access to 3-Dimensional Printing in the Context of Congenital Heart Disease: An International Physician Survey Study. CJC Open 2020, 2, 207–213. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Szary, J.; Luis, M.S.; Mikulski, S.; Patel, A.; Schulz, F.; Tretiakow, D.; Fercho, J.; Jaguszewska, K.; Frankiewicz, M.; Pawłowska, E.; et al. The Role of 3D Printing in Planning Complex Medical Procedures and Training of Medical Professionals—Cross-Sectional Multispecialty Review. Int. J. Environ. Res. Public Health 2022, 19, 3331. [Google Scholar] [CrossRef] [PubMed]
- Yamasaki, T.; Toba, S.; Sanders, S.P.; Carreon, C.K. Perfusion-distension fixation of heart specimens: A key step in immortalizing heart specimens for wax infiltration and generating 3D imaging data sets for reconstruction and printed 3D models. Cardiovasc. Pathol. 2022, 58, 107404. [Google Scholar] [CrossRef] [PubMed]
- Talanki, V.R.; Peng, Q.; Shamir, S.B.; Baete, S.H.; Duong, T.Q.; Wake, N. Three-dimensional printed anatomic models derived from magnetic resonance imaging data: Current state and image acquisition recommendations for appropriate clinical scenarios. J. Magn. Reson. Imaging. 2022, 55, 060–1081. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Capelli, C.; Koniordou, D.; Robertshaw, D.; Leaver, L.-K.; Schievano, S.; Taylor, A.M.; Wray, J. Use of 3D models of congenital heart disease as an education tool for cardiac nurses. Congenit. Heart Dis. 2016, 12, 113–118. [Google Scholar] [CrossRef]
- Lee, C.; Lee, J.Y. Utility of three-dimensional printed heart models for education on complex congenital heart diseases. Cardiol. Young 2020, 30, 1637–1642. [Google Scholar] [CrossRef]
- Sutherland, J.; Belec, J.; Sheikh, A.; Chepelev, L.; Althobaity, W.; Chow, B.J.W.; Mitsouras, D.; Christensen, A.; Rybicki, F.J.; La Russa, D.J. Applying Modern Virtual and Augmented Reality Technologies to Medical Images and Models. J. Digit. Imaging 2019, 32, 38–53. [Google Scholar] [CrossRef]
- Dhar, P.; Rocks, T.; Samarasinghe, R.M.; Stephenson, G.; Smith, C. Augmented reality in medical education: Students’ experience and learning outcomes. Med. Educ. Online 2021, 26, 1953953. [Google Scholar] [CrossRef] [PubMed]
- Patel, N.; Costa, A.; Sanders, S.P.; Ezon, D. Stereoscopic virtual reality does not improve knowledge retention of congenital heart disease. Int. J. Cardiovasc. Imaging 2021, 37, 2283–2290. [Google Scholar] [CrossRef]
- Maresky, H.S.; Oikonomou, A.; Ali, I.; Ditkofsky, N.; Pakkal, M.; Ballyk, B. Virtual reality and cardiac anatomy: Exploring immersive three-dimensional cardiac imaging, a pilot study in undergraduate medical anatomy education. Clin. Anat. 2019, 32, 238–243. [Google Scholar] [CrossRef]
- Goo, H.W.; Park, S.J.; Yoo, S.J. Advanced medical use of three-dimensional imaging in congenital heart disease: Augmented reality, mixed reality, virtual reality and three-dimensional printing. Korean. J. Radiol. 2020, 21, 133–145. [Google Scholar] [CrossRef]
- Barteit, S.; Lanfermann, L.; Barnighausen, T.; Neuhann, F.; Beiersmann, C. Aug-mentted reality, mixed and virtual reality-based head-mounted devices for medical education: Systematic review. JMIR. Serious Games 2021, 9, e29080. [Google Scholar] [CrossRef]
- Raimondi, F.; Vida, V.; Godard, C.; Bertelli, F.; Reffo, E.; Boddaert, N.; El Beheiry, M.; Masson, J.B. Fast-track virtual reality for cardiac imaging in congenital heart disease. J. Card. Surg. 2021, 36, 2598–2602. [Google Scholar] [CrossRef]
- Cen, J.; Liufu, R.; Wen, S.; Qiu, H.; Liu, X.; Chen, X.; Yuan, H.; Huang, M.; Zhuang, J. Three-Dimensional Printing, Virtual Reality and Mixed Reality for Pulmonary Atresia: Early Surgical Outcomes Evaluation. Heart Lung Circ. 2020, 30, 296–302. [Google Scholar] [CrossRef] [PubMed]
- Guo, H.; Wang, Y.; Dai, J.; Ren, C.; Li, J.; Lai, Y. Application of 3D printing in the surgical planning of hypertrophic obstructive cardiomyopathy and physician-patient communication: A preliminary study. J. Thorac. Dis. 2018, 10, 867–873. [Google Scholar] [CrossRef] [PubMed]
- Ryan, J.; Plasencia, J.; Richardson, R.; Velez, D.; Nigro, J.J.; Pophal, S.; Frakes, D. 3D printing for congenital heart disease: A single site’s initial three-year experience. 3D. Print. Med. 2018, 4, 10. [Google Scholar] [CrossRef]
- Zhao, L.; Zhou, S.; Fan, T.; Li, B.; Liang, W.; Dong, H. Three-dimensional printing enhances preparation for repair of double outlet right ventricular surgery. J. Card. Surg. 2018, 33, 24–27. [Google Scholar] [CrossRef]
- Ghosh, R.M.; Jolley, M.A.; Mascio, C.E.; Chen, J.M.; Fuller, S.; Rome, J.J.; Silvestro, E.; Whitehead, K.K. Clinical 3D modeling to guide pediatric cardiothoracic sur-gery and intervention using 3D printed anatomic models, computer aided design and virtual reality. 3D. Pring. Med. 2022, 8, 11. [Google Scholar] [CrossRef]
- Yoo, S.J.; Spray, T.; Austin, E.H.; Yun, T.J.; van Arsdell, G.S. Hands-on surgical training of congenital heart surgery suing 3-dimensional print models. J. Thorac. Cardiovasc. Surg. 2017, 153, 15301–15540. [Google Scholar] [CrossRef] [PubMed]
- Hussein, N.; Honjo, O.; Haller, C.; Coles, J.G.; Hua, Z.; Van Arsdell, G.; Yoo, S.-J. Quantitative assessment of technical performance during hands-on surgical training of the arterial switch operation using 3-dimensional printed heart models. J. Thorac. Cardiovasc. Surg. 2020, 160, 1035–1042. [Google Scholar] [CrossRef]
- Hussein, N.; Lim, A.; Honji, O.; Haller, C.; Coles, J.G.; Van Arsdell, G.; Yoo, S.J. Development and validation of a procedure-specific assessment tool for hands-on surgical training in congenital heart surgery. J. Thorac. Cardiovasc. Surg. 2020, 160, 229–240. [Google Scholar] [CrossRef]
- Averkin, I.I.; Grehov, E.V.; Pervunina, T.M.; Komlichenko, E.V.; Vasichkina, E.S.; Zaverza, V.M.; Nikiforov, V.G.; Latipova, M.L.; Govorov, I.E.; Kozyrev, I.A.; et al. 3D-printing in preoperative planning in neonates with complex congenital heart defects. J. Matern. Fetal. Neonatal Med. 2022, 35, 2020–2024. [Google Scholar] [CrossRef] [PubMed]
- Betancourt, L.G.; Wong, S.H.; Singh, H.R.; Nento, D.; Agarwal, A. Utility of three-dimensional printed model in biventricular repair of complex congenital cardiac defects: Case report and review of literature. Children 2022, 9, 184. [Google Scholar] [CrossRef] [PubMed]
- Brüning, J.; Kramer, P.; Goubergrits, L.; Schulz, A.; Murin, P.; Solowjowa, N.; Kuehne, T.; Berger, F.; Photiadis, J.; Weixler, V.H.-M. 3D modeling and printing for complex biventricular repair of double outlet right ventricle. Front. Cardiovasc. Med. 2022, 9, 1024053. [Google Scholar] [CrossRef]
- Liang, J.; Lu, B.; Zhao, X.; Wang, J.; Zhao, D.; Zhang, G.; Zhu, B.; Ma, Q.; Pan, G.; Li, D. Feasibility analyses of virtual models and 3D printing for surgical simulation of the double-outlet right ventricle. Med. Biol. Eng. Comput. 2022, 60, 3029–3040. [Google Scholar] [CrossRef]
- Spanaki, A.; Kabir, S.; Stephenson, N.; van Poppel, M.P.M.; Benetti, V.; Simpson, J. 3D Approaches in Complex CHD: Where Are We? Funny Printing and Beautiful Images, or a Useful Tool? J. Cardiovasc. Dev. Dis. 2022, 9, 269. [Google Scholar] [CrossRef]
- Yoo, S.-J.; Hussein, N.; Barron, D.J. Congenital Heart Surgery Skill Training Using Simulation Models: Not an Option but a Necessity. J. Korean Med. Sci. 2022, 37, e293. [Google Scholar] [CrossRef] [PubMed]
- Bernhard, B.; Illi, J.; Gloeckler, M.; Pilgrim, T.; Praz, F.; Windecker, S.; Haeberlin, A.; Gräni, C. Imaging-based, patient-specific three-dimensional printing to plan, train, and guide cardiovascular tnterventions: A systematic review and meta-analysis. Heart. Lung. Circ. 2022, 31, 1203–1218. [Google Scholar] [CrossRef] [PubMed]
- Mattus, M.S.; Ralph, T.B.; Keller, S.M.P.; Waltz, A.L.; Bramlet, M.T. Creation of patient-specific silicone cardiac models with ap-plications in presurgical plans and hands-on training. J. Vis. Exp. 2022, 10, 180. [Google Scholar]
- Peel, B.; Lee, W.; Hussein, N.; Yoo, S.-J. State-of-the-art silicone molded models for simulation of arterial switch operation: Innovation with parting-and-assembly strategy. JTCVS Tech. 2022, 12, 132–142. [Google Scholar] [CrossRef]
- Qiu, H.; Wen, S.; Ji, E.; Chen, T.; Liu, X.; Li, X.; Teng, Y.; Zhang, Y.; Liufu, R.; Zhang, J.; et al. A novel 3D visualized operative procedure in the single-stage complete repair with unifocalization of pulmonary aresia with ventricular septal defect and major aortopulmonary collateral arteries. Front. Cardiovasc. Med. 2022, 9, 836200. [Google Scholar] [CrossRef]
- Magagna, P.; Caprioglio, F.; Gallo, M.; Salvador, L. 3D printing to manage postinfarct ventricular septal defect. J. Card. Surg. 2021, 37, 449–450. [Google Scholar] [CrossRef] [PubMed]
- Wei, L.; Sun, G.; Wu, Q.; Zhang, W.; Tang, M.; Zhao, T.; Hu, S. Case Report: Three-Dimensional Printing–Assisted Surgical Treatment of Complex Body Vein Ectopic Drainage. Front. Cardiovasc. Med. 2022, 9, 782601. [Google Scholar] [CrossRef]
- Longinotti, L.; Castaldi, B.; Bertelli, F.; Vida, V.L.; Padalino, M.A. Three-dimensional Printing for Hybrid Closure of Complex Muscular Ventricular Septal Defects. Ann. Thorac. Surg. 2021, 113, e129–e132. [Google Scholar] [CrossRef]
- Hussein, N.; Honjo, O.; Haller, C.; Hickey, E.; Coles, J.G.; Williams, W.G.; Yoo, S.-J. Hands-On Surgical Simulation in Congenital Heart Surgery: Literature Review and Future Perspective. Semin. Thorac. Cardiovasc. Surg. 2020, 32, 98–105. [Google Scholar] [CrossRef]
- Hussein, N.; Honjo, O.; Barron, D.J.; Haller, C.; Coles, J.G.; Yoo, S.-J. The Incorporation of Hands-On Surgical Training in a Congenital Heart Surgery Training Curriculum. Ann. Thorac. Surg. 2020, 112, 1672–1680. [Google Scholar] [CrossRef]
- Scanlan, A.B.; Nguyen, A.V.; Ilina, A.; Lasso, A.; Cripe, L.; Jegatheeswaran, A.; Sil-vestro, E.; McGowan, F.X.; Mascio, C.E.; Fuller, S.; et al. Comparison of 3D echocardiography-derived 3D printed valve models to molded models for simulated repair of pediatric atrioventricular valve. Pediatr. Cardiol. 2018, 39, 538–547. [Google Scholar] [CrossRef]
- Brunner, B.S.; Thierij, A.; Jakob, A.; Tengler, A.; Grab, M.; Thierfelder, N.; Leuner, C.J.; Haas, N.A.; Hopfner, C. 3D-printed heart models for hands-on training in pediatric cardiology-the future of modern learning and teaching? GMS. J. Med. Educ. 2022, 39, Doc23. [Google Scholar]
- Hoashi, T.; Ichikawa, H.; Nakata, T.; Shimada, M.; Ozawa, H.; Higashida, A.; Kurosaki, K.; Kanzaki, S.; Shiraishi, I. Utility of a super-flexible three-dimensional printed heart model in congenital heart surgery†. Interact. Cardiovasc. Thorac. Surg. 2018, 27, 749–755. [Google Scholar] [CrossRef] [PubMed]
- Hon, N.W.L.; Hussein, N.; Honjo, O.; Yoo, S.-J. Evaluating the Impact of Medical Student Inclusion Into Hands-On Surgical Simulation in Congenital Heart Surgery. J. Surg. Educ. 2020, 78, 207–213. [Google Scholar] [CrossRef]
- Olivieri, L.J.; Su, L.; Hynes, C.F.; Krieger, A.; Alfares, F.A.; Ramakrishnan, K.; Zurakowski, D.; Marshall, M.B.; Kim, P.C.W.; Jonas, R.A.; et al. “Just-In-Time” Simulation Training Using 3-D Printed Cardiac Models After Congenital Cardiac Surgery. World J. Pediatr. Congenit. Heart Surg. 2016, 7, 164–168. [Google Scholar] [CrossRef] [PubMed]
- Stewart, M.A. Effective physician-patient communication and health outcomes: A review. Can. Med. Assoc. J. 1995, 152, 1423–1433. [Google Scholar]
- Pratt, M.; Searles, G.E. Using Visual Aids to Enhance Physician-Patient Discussions and Increase Health Literacy. J. Cutan. Med. Surg. 2017, 21, 497–501. [Google Scholar] [CrossRef] [PubMed]
- Traynor, G.; Shearn, A.I.U.; Milano, E.G.; Ordonez, M.V.; Forte, M.N.V.; Caputo, M.; Schievano, S.; Mustard, H.; Wray, J.; Biglino, G. The use of 3D-printed models in patient communication: A scoping review. J. 3D Print. Med. 2022, 6, 13–23. [Google Scholar] [CrossRef]
- Biglino, G.; Koniordou, D.; Gasparini, M.; Capelli, C.; Leaver, L.K.; Khambadkone, S.; Schievano, S.; Taylor, A.M.; Wray, J. Piloting the use of patient-specific cardiac models as a novel tool to facilitate communication during clinical consultations. Pediatr. Cardiol. 2017, 38, 813–818. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Capelli, C.; Wray, J.; Schievano, S.; Leaver, L.-K.; Khambadkone, S.; Giardini, A.; Derrick, G.; Jones, A.; Taylor, A.M. 3D-manufactured patient-specific models of congenital heart defects for communication in clinical practice: Feasibility and acceptability. BMJ Open 2015, 5, e007165. [Google Scholar] [CrossRef] [PubMed]
- Biglino, G.; Moharem-Elgamal, S.; Lee, M.; Tulloh, R.; Caputo, M. The Perception of a Three-Dimensional-Printed Heart Model from the Perspective of Different Stakeholders: A Complex Case of Truncus Arteriosus. Front. Pediatr. 2017, 5, 209. [Google Scholar] [CrossRef]
- Biglino, G.; Capelli, C.; Leaver, L.K.; Schievano, S.; Taylor, A.M.; Wray, J. Involving patient, family and medical staff in the evaluation of 3D printing models of congenital heart disease. Common. Med. 2015, 12, 157–169. [Google Scholar] [CrossRef] [PubMed]
- Lau, I.; Gupta, A.; Ihdayhid, A.; Sun, Z. Clinical Applications of Mixed Reality and 3D Printing in Congenital Heart Disease. Biomolecules 2022, 12, 1548. [Google Scholar] [CrossRef] [PubMed]
- Deng, X.; He, S.; Huang, P.; Luo, J.; Yang, G.; Zhou, B.; Xiao, Y. A three-dimensional printed model in preoperative consent for ventricular septa defect repair. J. Cardiothorac. Surg. 2021, 16, 229. [Google Scholar] [CrossRef] [PubMed]
- Chessa, M.; Van De Bruaene, A.; Farooqi, K.; Valverde, I.; Jung, C.; Votta, E.; Sturla, F.; Paul Diller, G.; Brida, M.; Sun, Z.; et al. Three-dimensional printing, holograms, computational modelling, and artificial intelligence for adult congenital heart disease care: An exciting future. Eur. Heart. J. 2022, 43, 2672–2684. [Google Scholar]
- Alonzo, M.; AnilKumar, S.; Roman, B.; Tasnim, N.; Joddar, B. 3D Bioprinting of cardiac tissue and cardiac stem cell therapy. Transl. Res. 2019, 211, 64–83. [Google Scholar] [CrossRef]
- Zhang, J.; Wehrle, E.; Rubert, M.; Muller, R. 3D bioprinting of human tissues: Biofabrication, bioinks and bioreactors. Int. J. Mol. Sci. 2021, 22, 3971. [Google Scholar] [CrossRef]
- Wang, Z.; Lee, S.J.; Cheng, H.-J.; Yoo, J.J.; Atala, A. 3D bioprinted functional and contractile cardiac tissue constructs. Acta Biomater. 2018, 70, 48–56. [Google Scholar] [CrossRef] [PubMed]
- Kato, B.; Wisser, G.; Agrawal, D.K.; Wood, T.; Thankam, F.G. 3D bioprinting of cardiac tissue: Current challenges and perspectives. J. Mater. Sci. Mater. Med. 2021, 32, 54. [Google Scholar] [CrossRef] [PubMed]
- Jiang, S.; Feng, W.; Chang, C.; Li, G. Modeling human heart development and congenital defects using organoids: How close are we? J. Cardiovasc. Dev. Dis. 2022, 9, 125. [Google Scholar] [CrossRef] [PubMed]
- Lee, A.; Hudson, A.R.; Shiwarski, D.J.; Tashman, J.W.; Hinton, T.J.; Yerneni, S.; Bliley, J.M.; Campbell, P.G.; Feinberg, A.W. 3D bioprinting of collagen to rebuild components of the human heart. Science 2019, 365, 482–487. [Google Scholar] [CrossRef] [PubMed]
- Lee, W.; Hong, Y.; Dai, G. 3D bioprinting of vascular conduits for pediatric congenital heart repairs. Transl. Res. 2019, 211, 35–45. [Google Scholar] [CrossRef]
- Bliley, J.; Tashman, J.; Stang, M.; Coffin, B.; Shiwarski, D.; Lee, A.; Hinton, T.; Feinberg, A. FRESH 3D bioprinting a con-tractile heart tube using human stem cell-derived cardiomyocytes. Biofabrication 2022, 14, 024106. [Google Scholar] [CrossRef]
- Mirdamadi, E.; Tashman, J.W.; Shiwarski, D.J.; Palchesko, R.N.; Feinberg, A.W. FRESH 3D Bioprinting a Full-Size Model of the Human Heart. ACS Biomater. Sci. Eng. 2020, 6, 6453–6459. [Google Scholar] [CrossRef]


| Studies | No. of 3D-Printed Models | Comparisons | Mean Difference (mm) | Analysis Method |
|---|---|---|---|---|
| Lee et al. [39] | 3 | 3D model vs. original CT 3D model vs. CT of 3D model 3D model vs. STL files Original CT images vs. STL files | 0.21 ± 0.37 mm −0.11 ± 0.47 mm 0.1 ± 0.28/ 0.17 ± 0.48 mm 0.12 ± 0.23/ 0.12 ± 0.25 mm | Pearson’s correlation/ Bland–Altman plot |
| Valverde et al. [40] | 40 (20 selected for accuracy comparison) | 3D model vs. both CT and MRI 3D model vs. original CT 3D model vs. original MRI | 0.27 ± 0.73 mm −0.16 ± 0.85 mm −0.30 ± 0.67 mm | Bland–Altman plot |
| Olejník et al. [41] | 8 | CT images vs. STL | 0.19 ± 0.38 mm | Bland–Altman plot |
| 3D model vs. in vivo | 0.13 ± 0.26 mm | |||
| Olivieri et al. [42] | 9 | 3D model vs. echo | 0.4 ± 0.9 mm | Pearson’s correlation/ Bland–Altman plot |
| Lau et al. [43] | 1 | 3D model vs. CT | 0.23 mm | Pearson’s correlation |
| Mowers et al. [44] | 5 | 2D echo vs. digital 3D | 0 mm | Pearson’s correlation/ Bland–Altman plot |
| 2D echo vs. 3D model | 0.3 mm | |||
| Parimi et al. [45] | 5 | 3D model vs. rotational angiography | No significant difference between 3D models and biplane angiography measurements (p = 0.14) | Pearson’s correlation/ Bland–Altman plot |
| Author | Study Design | Sample Size and Participants | Original Data Source | Application in CHD | Key Findings |
|---|---|---|---|---|---|
| Lau & Sun [25] | Cohort study | 53 medical students | CT | ASD, VSD, ToF and DORV. | Slightly higher scores were achieved in the 3D-printed model group than those in the control group (7.79 ± 2.63 vs. 7.04 ± 2.64, p > 0.05), while 3D-printed models did not improve knowledge acquisition. |
| Karsenty et al. [26] | RCT | 347 medical students | CT | CHD including ASD, VSD, CoA and ToF. | Use of 3D printing improved objective knowledge when compared to the control group (p < 0.0001). |
| Smerling et al. [28] | Cross-sectional study | 45 medical students | CT | Three-dimensional-printed heart models including pulmonic stenosis (PS), ASD, ToF, d-TGA, CoA and HLHS. | Three-dimensional-printed models significantly enhanced students’ knowledge for all of these cardiac pathologies (p < 0.001). |
| Su et al. [29] | RCT | 63 medical students | CT | Three-dimensional-printed VSD models: perimembranous, subarterial and muscular VSD. | Three-dimensional-printed models significantly improved VSD learning when compared to the control group (p < 0.05). |
| Lau et al. [30] | Cross-sectional study | 29 participants (radiologists, sonographers and radiographers) | CT | ASD, VSD, ToF and DORV. | Both 3D-printed models and VR were useful in education and pre-operative planning when compared to conventional visualisations. |
| Jones & Seckeler [31] | RCT | 36 pediatric medical students | CT & MRI | Three-dimensional-printed models of vascular rings and pulmonary artery slings. | Three-dimensional-printed models significantly enhanced participants’ knowledge in learning anatomy and pathology (p < 0.01). |
| Loke et al. [19] | RCT | 35 pediatric residents | CT, MRI and 3D echocardiography | Three-dimensional-printed models: A normal infant heart, an adult repaired ToF and an infant unrepaired ToF. | Higher satisfaction scores were achieved with 3D-printed models (p = 0.03). |
| Valverde et al. [33] | Non-RCT | 127 participants | Echocardiography and CMR. | Value of 3D-printed models on medical education in criss-cross hearts. | Three-dimensional-printed models significantly increased knowledge in learning criss-cross heart anatomy (p < 0.001). |
| White et al. [34] | RCT | 60 pediatric and emergency medicine residents | NA | Three-dimensional-printed models of four cases including VSD and ToF. | The 3D printing group scored significantly higher than the control group (p = 0.037) on ToF postlecture test, while the control group scored higher on the VSD postlecture test (p = 0.012). |
| Tan et al. [35] | RCT | 132 nursing students | NA | Three-dimensional-printed model of a ASD case in teaching clinical nursing in congenital heart surgery. | Use of Three-dimensional-printed models significantly improved clinical nurses in learning congenital heart surgery. |
| Biglino et al. [54] | Cross-sectional study | 100 cardiac nurses | NA | Nine 3D-printed models: a heathy heart, and other types of CHD. | Three-dimensional-printed models serve as useful tools in training adult and pediatric cardiac nurses for learning and understanding CHD. |
| Liang et al. [38] | Cross-sectional study | Expert group (n = 40 with 20 cardiac surgeons and 20 sonographers) and student group (40 postgraduate medical students) | CT | Eight types of CHD: PDA, CoA, VSD ccTGA, DORV, WA, CAF and ToF. | 3D-printed models significantly improved the CHD diagnosis in both the expert and student groups (p = 0.000–0.001). Three-dimensional printing was found to be more important in the diagnosis of more complex CHD than simple CHD (p = 0.000). |
| Lee C and Lee J [55] | Cross-sectional study | 74 participants including 41 residents, 14 physicians, 10 nurses and 9 perfusionists. | CT | Eleven complex CHD cases included ToF, AVSD, DORV, single ventricle with DILV/BCPA. | Subjective improvements were found in all learning categories post-seminar scores when compared with pre-seminar scores: understanding anatomy (8.4 ± 1.1 vs. 4.8 ± 2.1), 3D structure (8.9 ± 1.0 vs. 4.6 ± 2.2), pathophysiology (8.5 ± 1.0 vs. 4.8 ± 2.2), and surgery (8.8 ± 0.9 vs. 4.9 ± 2.3), with all p < 0.001 respectively. |
| Author | Study Design | Sample Size and Participants | Original Data Source | Application in CHD | Key Findings |
|---|---|---|---|---|---|
| Valverde et al. [40] | Prospective multicenter study | Forty patients with complex CHD. | CT and MRI | Three-dimensional-printed models of 19 DORV and 21 other types of CHD. | The surgical decision was changed in 47.5% cases with aid of 3D-printed models. |
| Chen et al. [63] | Cross-sectional study | Five patients with (PA with VSD or MAPCA | Echocardiography and CT | Three-dimensional-printed models and VR/MR in surgical outcomes. | Three-dimensional-printed models assisted surgeons to pre-operatively analyse surgery plans, while VR facilitated understanding of intracardiac structures. |
| Gomez-Ciriza et al. [21] | Cross-sectional study | Forty-three participants | CT and MRI | One hundred thirty-eight low-cost 3D-printed models were developed for surgical planning and interventional simulations. | Use of 3D-printed models has a positive impact on CHD surgery with initial surgical plan modified in 47.5% of the cases after reviewing the models. |
| Guo et al. [64] | Cross-sectional study | Surgeon, patients and nonmedical professionals | CT | Seven HOCM models were printed for surgical management and pre-operative conversation. | Three-dimensional-printed models were useful for surgical planning and pre-operative communication. |
| Kiraly et al [23] | Cross-sectional study | Single center team learning experience of 3D-printed models in pediatric surgeries | CT | Fifteen models of pediatric patients with CHD and their impact on complex CHD surgeries. | Three-dimensional-printed models significantly contributed to improved surgical plans with intracardiac repair modified in 13 out of 15 cases. |
| Ryan et al. [65] | Cross-sectional study | Single center experience of 3D-printed models in CHD | CT and MRI | One hundred sixty-four models were printed for various purposes. | Three-dimensional-printed models contributed to a mean reduction in overall time when compared with standard of care, although the reductions did not reach significant differences. |
| Zhao et al. [66] | Cross-sectional study | Twenty-five patients with DORV | CT | Use of 3D-printed models in pre-operative repair of complex DORV. | Three-dimensional-printed models significantly reduced operating time and improved postoperative outcomes (p < 0.05). |
| Ghosh et al. [67] | Cross-sectional study | Single center three-year experience with 112 3D-printed CHD models for pre-operative planning. | MRI and CT | Use of 3D-printed models in pre-procedural planning of CHD. | Demand for the use of 3D-printed models in clinical practice has tripled over a three-year period. Incorporation of 3D printing technology into pre-procedural care of pediatric CHD surgeries is feasible. |
| Author | Study Design | Sample Size and Participants | Original Data Source | Application in CHD | Image Processing Software | 3D Printer | 3D Printing Material | Key Findings |
|---|---|---|---|---|---|---|---|---|
| Yoo et al. [68] | Cross-sectional study | Fifty participants (surgeons and surgical trainees) participated in the survey. | CT and MRI | HOST using 3D-printed CHD models. | Mimics (Materalise, Belgium) Average cost per model: $60 | Objet Connex 260 printer. | TangoPlus FullCure resin and VeroWhite | HOST serves as a valuable surgical simulation platform for practicing congenital heart surgery on 3D-printed models. |
| Hussein et al [85] | Cross-sectional study | Seven trainees completed 12 sessions through HOST program for congenital heart surgery. | NA | Twelve 3D-printed heart models were incorporated into year long currciulum. | NA | Polyjet (Stratasys J750, Eden Prairie, MN, USA). | Agilus30 | Ninety-one percent of procedural times were improved by a mean of 25% (p < 0.001). Eighty-four percent of trainees’ mean time improved between the two attempts with an improvement of 23% (p = 0.002). |
| Scanlan et al [86] | Cross-sectional study | Four physicians and four pediatric cardiac surgery fellows assessed suitability of 3D-printed models for simulation of tricuspid valve annuloplasty and atrioventricular canal repair procedures. | Echocardiograpy | Three valve models (MV, TV and CAV) were printed with different materials for simulation of congenital heart valve procedures. | 3D Slicer Directly printed model: $7.90 Molded: $45 | Object 500 Connex (Stratasys, Eden Prairie, MN, USA) | Valve models printed in TangoPlus FLX 930, while valve mold printed in VeroGray RDG850 or VeroBlue GDG840 | Surgeon assessment showed that the molded valve models were more realistic for cutting and suturing than directly printed models (p < 0.01). Complete atrioventricular canal repair was highly rated by surgeons using the molded valves compared with the directly printed valves (p < 0.01). |
| Hoashi et al. [88] | Cross-sectional study | Twenty models of CHD were created for surgical simulation with all operations performed by a young consultant surgeon. | NA | Understanding the relationship between intraventricular communications and great vessels and utility of 3D models for simulations of intracardiac procedures. | NA $2000–3000 per model | Stereolithography (SOUP2, 600GS, Japan) | Super flexible polyurethan resins | The median cardiopulmonary bypass time and cross-clamp time was 345 (110–570) min and 114 (35–293) min, respectively. No mortality was observed during the median follow-up of 1.3 (0.1–2.5) years. |
| Brunner et al. [87] | Cross-sectional study | Nineteen medical students and doctors participated in the hands-on training program. | CT | Hands-on training on simulation of interventional cardiology procedures on common CHD models. | Mimics (Materalise, Belgium) | Agilista 3200W Polyjet 3D printer | Silicone rubber | Practicing on 3D-printed models significantly reduced the mean fluoroscopy time and increased confidence in interventions on real patients. |
| Hon et al. [89] | Cross-sectional study | Fifteen preclinical medical students participated in the HOST course. | NA | Medical students rehearsed their knot-typing and simple suturing skills on 3D printed models. | NA | NA | Agilus30 (Stratasys, Eden Prairie, MN, USA) | All students were highly satisfied with 3D-printed models helping their understanding of CHD (4.80 ± 0.41) and learning complex anatomy (4.87 ± 0.35), with training sessions improving their assisting skills (4.93 ± 0.26). |
| Olivieri et al. [90] | Cross-sectional study | Seventy participants enrolled in the study including 22 physicians, 38 critical care nurses and 10 ancillary providers. | CT or MRI | Ten CHD cases were selected for cardiac surgery simulation. | Mimics (Materalise, Belgium) | Objet500 Connext (Stratays, Eden, Prairie, MN, USA) | Rigid plastic materials. | Three-dimensional-printed models were scored more useful (8.4 out of 10) than standard hands-off with 90% of participants scoring 8 out of 10 or higher. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the author. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, Z. Patient-Specific 3D-Printed Models in Pediatric Congenital Heart Disease. Children 2023, 10, 319. https://doi.org/10.3390/children10020319
Sun Z. Patient-Specific 3D-Printed Models in Pediatric Congenital Heart Disease. Children. 2023; 10(2):319. https://doi.org/10.3390/children10020319
Chicago/Turabian StyleSun, Zhonghua. 2023. "Patient-Specific 3D-Printed Models in Pediatric Congenital Heart Disease" Children 10, no. 2: 319. https://doi.org/10.3390/children10020319
APA StyleSun, Z. (2023). Patient-Specific 3D-Printed Models in Pediatric Congenital Heart Disease. Children, 10(2), 319. https://doi.org/10.3390/children10020319






