The Ophthalmic Manifestations of Down Syndrome
Abstract
1. Introduction
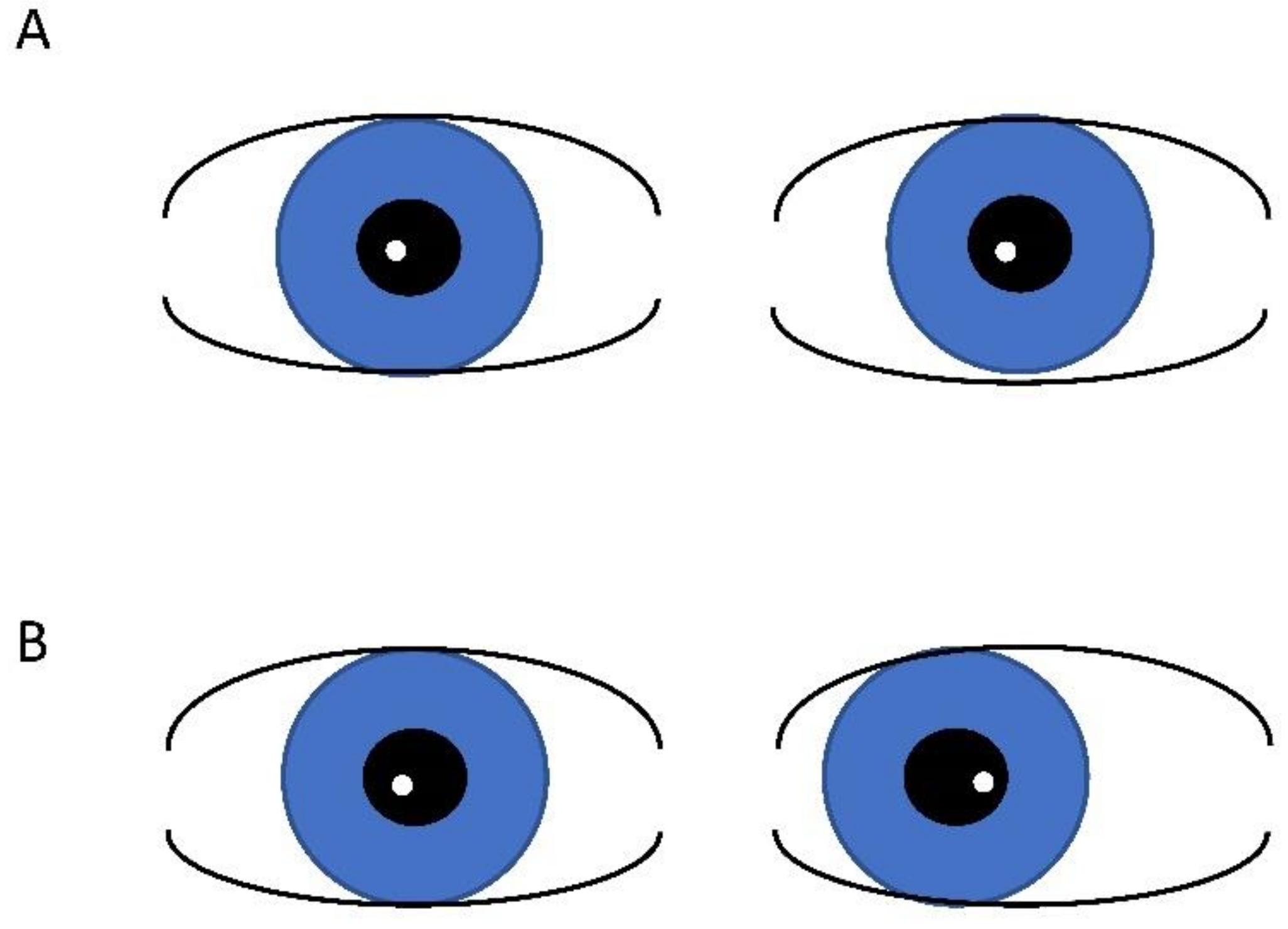
2. Strabismus
3. Amblyopia
4. Accommodation Defects
5. Refractive Error
6. Eyelid Abnormalities
7. Nasolacrimal Duct Obstruction
8. Nystagmus
9. Keratoconus
10. Iris
11. Cataracts
12. Retinal Abnormalities
13. Optic Nerve Abnormalities
14. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- Kazemi, M.; Salehi, M.; Kheirollahi, M. Down syndrome: Current status, challenges and future perspectives. Int. J. Mol. Cell. Med. 2016, 5, 125–133. [Google Scholar] [PubMed]
- Makateb, A.; Hashemi, H.; Farahi, A.; Mehravaran, S.; Khabazkhoob, M.; Asgari, S. Ocular alignment, media, and eyelid disorders in Down syndrome. Strabismus 2020, 28, 42–48. [Google Scholar] [CrossRef] [PubMed]
- Omobolanle, A.A.; Wajuihian, S.O. Ophthalmic manifestations of children with Down syndrome in Port Harcourt, Nigeria. Clin. Ophthalmol. 2012, 6, 1859–1864. [Google Scholar] [CrossRef] [PubMed]
- Liza-Sharmini, A.T.; Azlan, Z.N.; Zilfalil, B.A. Ocular findings in Malaysian children with Down syndrome. Singap. Med. J. 2006, 47, 14–19. [Google Scholar]
- Stephen, E.; Dickson, J.; Kindley, A.D.; Scott, C.C.; Charleton, P.M. Surveillance of vision and ocular disorders in children with Down syndrome. Dev. Med. Child Neurol. 2007, 49, 513–515. [Google Scholar] [CrossRef]
- Fimiani, F.; Iovine, A.; Carelli, R.; Pansini, M.; Sebastio, G.; Magli, A. Incidence of Ocular Pathologies in Italian Children with down Syndrome. Eur. J. Ophthalmol. 2007, 17, 817–822. [Google Scholar] [CrossRef]
- Ljubic, A.; Trajkovski, V.; Tesic, M.; Tojtovska, B.; Stankovic, B. Ophthalmic Manifestations in Children and Young Adults with Down Syndrome and Congenital Heart Defects. Ophthalmic Epidemiol. 2015, 22, 123–129. [Google Scholar] [CrossRef]
- Ugurlu, A.; Altinkurt, E. Ophthalmologic Manifestations and Retinal Findings in Children with Down Syndrome. J. Ophthalmol. 2020, 2020, 9726261-6. [Google Scholar] [CrossRef]
- Umfress, A.C.; Hair, C.D.; Donahue, S.P. Prevalence of Ocular Pathology on Initial Screening and Incidence of New Findings on Follow-up Examinations in Children With Trisomy 21. Am. J. Ophthalmol. 2019, 207, 373–377. [Google Scholar] [CrossRef]
- de Weger, C.; Boonstra, N.; Goossens, J. Bifocals reduce strabismus in children with Down syndrome: Evidence from a randomized controlled trial. Acta Ophthalmol. 2020, 98, 89–97. [Google Scholar] [CrossRef]
- Haugen, O.H.; Høvding, G. Strabismus and binocular function in children with Down syndrome. A population-based, longitudinal study. Acta Ophthalmol. Scand. 2001, 79, 133–139. [Google Scholar] [CrossRef]
- Stewart, R.E.; Woodhouse, J.M.; Cregg, M.; Pakeman, V.H. Association Between Accommodative Accuracy, Hypermetropia, and Strabismus in Children with Down’s Syndrome. Optom. Vis. Sci. 2007, 84, 149–155. [Google Scholar] [CrossRef]
- Jaeger, E.A. Ocular findings in Down’s Syndrome. Trans. Am. Ophthalmol. Soc. 1980, 78, 808–845. [Google Scholar]
- Yurdakul, N.S.; Ugurlu, S.; Maden, A. Strabismus in Down Syndrome. J. Pediatr. Ophthalmol. Strabismus 2006, 43, 27–30. [Google Scholar] [CrossRef]
- Al-Mujaini, A.; AL Yahyai, M.; Ganesh, A. Congenital Eyelid Anomalies: What General Physicians Need to Know. Oman Med. J. 2021, 36, e279. [Google Scholar] [CrossRef]
- Harrison, A.; Allen, L.; O’Connor, A. Strabismus Surgery for Esotropia, Down Syndrome and Developmental Delay; Is an Altered Surgical Dose Required? A Literature Review. Br. Ir. Orthopt. J. 2020, 16, 4–12. [Google Scholar] [CrossRef]
- Hashemi, H.; Mehravaran, S.; Asgari, S.; Nasrabadi, F.D. Refractive and Vision Status in Down Syndrome: A Comparative Study. Turk. J. Ophthalmol. 2021, 51, 199–205. [Google Scholar] [CrossRef]
- Tsiaras, W.G.; Pueschel, S.; Keller, C.; Curran, R.; Giesswein, S. Amblyopia and visual acuity in children with Down's syndrome. Br. J. Ophthalmol. 1999, 83, 1112–1114. [Google Scholar] [CrossRef]
- Abdu, L.; Bawahab, N.; Hussain, R.W.M.; Qary, H.; Saeedi, A.; Alhibshi, N. Prevalence and Treatment Outcome of Nasolacrimal Duct Obstruction in Saudi Children with Down Syndrome. Cureus 2020, 12, e6672. [Google Scholar] [CrossRef]
- Miyazaki, E.A. The Orthoptics of Down Syndrome. Am. Orthopt. J. 2014, 64, 12–16. [Google Scholar] [CrossRef]
- Woodhouse, J.M.; Meades, J.S.; Leat, S.; Saunders, K. Reduced accommodation in children with Down syndrome. Investig. Opthalmology Vis. Sci. 1993, 34, 2382–2387. [Google Scholar]
- Doyle, L.; Saunders, K.J.; Little, J.-A. Determining the relative contribution of retinal disparity and blur cues to ocular accommodation in Down syndrome. Sci. Rep. 2017, 7, 39860. [Google Scholar] [CrossRef] [PubMed]
- Woodhouse, J.M.; Pakeman, V.H.; Saunders, K.; Parker, M.; Fraser, W.I.; Lobo, S.; Sastry, P. Visual acuity and accommodation in infants and young children with Down's syndrome. J. Intellect. Disabil. Res. 1996, 40, 49–55. [Google Scholar] [CrossRef] [PubMed]
- Haugen, O.H.; Høvding, G.; Lundström, I. Refractive development in children with Down's syndrome: A population based, longitudinal study. Br. J. Ophthalmol. 2001, 85, 714–719. [Google Scholar] [CrossRef] [PubMed]
- Cregg, M.; Woodhouse, J.M.; Pakeman, V.H.; Saunders, K.; Gunter, H.L.; Parker, M.; Fraser, W.I.; Sastry, P. Accommodation and refractive error in children with Down syndrome: Cross-sectional and longitudinal studies. Investig. Opthalmology Vis. Sci. 2001, 42, 55–63. [Google Scholar]
- Nandakumar, K.; Leat, S. Bifocals in children with Down syndrome (BiDS)—Visual acuity, accommodation and early literacy skills. Acta Ophthalmol. 2010, 88, e196–e204. [Google Scholar] [CrossRef]
- Adyanthaya, R.; Isenor, S.; Muthusamy, B.; Irsch, K.; Guyton, D.L. Children with Down syndrome benefit from bifocals as evidenced by increased compliance with spectacle wear. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2014, 18, 481–484. [Google Scholar] [CrossRef]
- Nandakumar, K.; Evans, M.A.; Briand, K.; Leat, S. Bifocals in Down syndrome study (BiDS): Analysis of video recorded sessions of literacy and visual perceptual skills. Clin. Exp. Optom. 2011, 94, 575–585. [Google Scholar] [CrossRef]
- Bermudez, B.E.B.V.; Amaral, M.E.d.S.D.; Gomes, C.D.S.; Novadzki, I.M.; de Oliveira, C.M.; Serpe, C.C. Ophthalmological abnormalities in Down syndrome among Brazilian patients. Am. J. Med. Genet. Part A 2020, 182, 2641–2645. [Google Scholar] [CrossRef]
- Paudel, N.; Leat, S.; Adhikari, P.; Woodhouse, J.M.; Shrestha, J.B. Visual defects in Nepalese children with Down syndrome. Clin. Exp. Optom. 2010, 93, 83–90. [Google Scholar] [CrossRef]
- Watt, T.; Robertson, K.; Jacobs, R.J. Refractive error, binocular vision and accommodation of children with Down syndrome. Clin. Exp. Optom. 2015, 98, 3–11. [Google Scholar] [CrossRef]
- Afifi, H.H.; Azeem, A.A.A.; El-Bassyouni, H.T.; Gheith, M.E.; Rizk, A.; Bateman, J.B. Distinct Ocular Expression in Infants and Children With Down Syndrome in Cairo, Egypt. JAMA Ophthalmol 2013, 131, 1057–1066. [Google Scholar] [CrossRef]
- Muñoz-Ortiz, J.; Charry-Sánchez, J.D.; Bechara-Arango, I.; Blanco-Becerra, M.; Talero-Gutiérrez, C.; Gomez-Suarez, M.; De-La-Torre, A. Prevalence of ophthalmological manifestations in pediatric and adolescent populations with Down syndrome: A systematic review of the literature. Syst. Rev. 2022, 11, 75. [Google Scholar] [CrossRef]
- Purpura, G.; Bacci, G.M.; Bargagna, S.; Cioni, G.; Caputo, R.; Tinelli, F. Visual assessment in Down Syndrome: The relevance of early visual functions. Early Hum. Dev. 2019, 131, 21–28. [Google Scholar] [CrossRef]
- DA Cunha, R.P.; Moreira, J.B.D.C. Ocular Findings in Down's Syndrome. Am. J. Ophthalmol. 1996, 122, 236–244. [Google Scholar] [CrossRef]
- Wagner, R.S.; Caputo, A.R.; Reynolds, R.D. Nystagmus in Down Syndrome. Ophthalmology 1990, 97, 1439–1444. [Google Scholar] [CrossRef]
- Roizen, N.J.; Mets, M.B.; Blondis, T.A. OPHTHALMIC DISORDERS IN CHILDREN WITH DOWN SYNDROME. Dev. Med. Child Neurol. 1994, 36, 594–600. [Google Scholar] [CrossRef]
- Woodhouse, J.M.; Pakeman, V.H.; Cregg, M.; Saunders, K.J.; Parker, M.; Fraser, W.I.; Sastry, P.; Lobo, S. Refractive Errors in Young Children with Down Syndrome. Optom. Vis. Sci. 1997, 74, 844–851. [Google Scholar] [CrossRef]
- Cregg, M.; Woodhouse, J.M.; Stewart, R.E.; Pakeman, V.H.; Bromham, N.R.; Gunter, H.L.; Trojanowska, L.; Parker, M.; Fraser, W.I. Development of Refractive Error and Strabismus in Children with Down Syndrome. Investig. Opthalmology Vis. Sci. 2003, 44, 1023–1030. [Google Scholar] [CrossRef]
- Coats, D.K.; McCreery, K.M.; Plager, D.A.; Bohra, L.; Kim, D.S.; Paysse, E.A. Nasolacrimal outflow drainage anomalies in down’s syndrome. Ophthalmology 2003, 110, 1437–1441. [Google Scholar] [CrossRef]
- Haseeb, A.; Huynh, E.; ElSheikh, R.H.; ElHawary, A.S.; Scelfo, C.; Ledoux, D.M.; Maidana, D.E.; Elhusseiny, A.M. Down syndrome: A review of ocular manifestations. Ther. Adv. Ophthalmol. 2022, 14. [Google Scholar] [CrossRef] [PubMed]
- Al-Faky, Y.H.; Mousa, A.; Alkhiary, H.T.; Al-Mosallam, A.R. Management of Unilateral Versus Bilateral Lacrimal Drainage System Dysfunction in Down Syndrome. J. Pediatr. Ophthalmol. Strabismus 2012, 49, 109–113. [Google Scholar] [CrossRef] [PubMed]
- Lueder, G.T. Treatment of nasolacrimal duct obstruction in children with trisomy 21. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2000, 4, 230–232. [Google Scholar] [CrossRef] [PubMed]
- Postolache, L. Abnormalities of the Optic Nerve in Down Syndrome and Associations with Visual Acuity. Front. Neurol. 2019, 10, 633. [Google Scholar] [CrossRef]
- Oladiwura, D.; Shweikh, Y.; Roberts, C.; Theodorou, M. Nystagmus in Down Syndrome—A Retrospective Notes Review. Br. Ir. Orthopt. J. 2022, 18, 48–56. [Google Scholar] [CrossRef]
- Averbuch-Heller, L.; Dell'Osso, L.F.; Jacobs, J.B.; Remler, B.F. Latent and Congenital Nystagmus in Down Syndrome. J. Neuro-Ophthalmology 1999, 19, 166–172. [Google Scholar] [CrossRef]
- Zahidi, A.A.A.; McIlreavy, L.; Erichsen, J.T.; Woodhouse, J.M. Visual and Refractive Status of Children with Down's Syndrome and Nystagmus. Investig. Opthalmology Vis. Sci. 2022, 63, 28. [Google Scholar] [CrossRef]
- Kim, J.H.; Hwang, J.-M.; Kim, H.J.; Yu, Y.S. Characteristic ocular findings in Asian children with Down syndrome. Eye 2002, 16, 710–714. [Google Scholar] [CrossRef]
- Weiss, A.H.; Kelly, J.P.; Phillips, J.O. Infantile Nystagmus and Abnormalities of Conjugate Eye Movements in Down Syndrome. Investig. Opthalmology Vis. Sci. 2016, 57, 1301. [Google Scholar] [CrossRef]
- Kristianslund, O.; Drolsum, L. Prevalence of keratoconus in persons with Down syndrome: A review. BMJ Open Ophthalmol. 2021, 6, e000754. [Google Scholar] [CrossRef]
- Alio, J.L.; Vega-Estrada, A.; Sanz, P.; Osman, A.A.; Kamal, A.M.; Mamoon, A.; Soliman, H. Corneal Morphologic Characteristics in Patients With Down Syndrome. JAMA Ophthalmol 2018, 136, 971–978. [Google Scholar] [CrossRef]
- Kristianslund, O.; Hagem, A.M.; Thorsrud, A.; Drolsum, L. Prevalence and incidence of keratoconus in Norway: A nationwide register study. Acta Ophthalmol. 2021, 99, e694–e699. [Google Scholar] [CrossRef]
- Vincent, A.L.; Weiser, B.A.; Cupryn, M.; Stein, R.M.; Abdolell, M.; Levin, A.V. Clinical Science. Computerized corneal topography in a paediatric population with Down syndrome. Clin. Exp. Ophthalmol. 2005, 33, 47–52. [Google Scholar] [CrossRef]
- Imbornoni, L.M.; Wise, R.E.; Taravella, M.J.; Hickey, F.; McCourt, E.A. Keratoconus and corneal morphology in patients with Down syndrome at a pediatric hospital. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2020, 24, 140.e1–140.e5. [Google Scholar] [CrossRef]
- Evereklioglu, C.; Yilmaz, K.; Bekir, N.A. Decreased Central Corneal Thickness in Children with Down Syndrome. J. Pediatr. Ophthalmol. Strabismus 2002, 39, 274–277. [Google Scholar] [CrossRef]
- Aslan, L.; Aslankurt, M.; Yüksel, E.; Özdemir, M.; Aksakal, E.; Gümüşalan, Y.; Özdemir, G. Corneal thickness measured by Scheimpflug imaging in children with Down syndrome. J. Am. Assoc. Pediatr. Ophthalmol. Strabismus 2013, 17, 149–152. [Google Scholar] [CrossRef]
- Karakucuk, Y.; Altinkaynak, H.; Comez, A.; Beyoglu, A. Objective evaluation of corneal and lens densitometry in children with Down syndrome. J. Français D'ophtalmologie 2020, 43, 884–890. [Google Scholar] [CrossRef] [PubMed]
- Haargaard, B. Down's syndrome and early cataract. Br. J. Ophthalmol. 2006, 90, 1024–1027. [Google Scholar] [CrossRef] [PubMed]
- Igersheimer, J.; Mautner, H. About the significance of lenticular changes in mongolism. Ann. Paediatr. Int. Rev. Pediatr. 1953, 181, 34–44. [Google Scholar] [PubMed]
- Mathan, J.J.; Simkin, S.K.; Gokul, A.; McGhee, C.N.J. Down syndrome and the eye: Ocular characteristics and ocular assessment. Surv. Ophthalmol. 2022, 67, 1631–1646. [Google Scholar] [CrossRef]
- Saifee, M.; Kong, L.; Yen, K.G. Outcomes of Cataract Surgery in Children with Down Syndrome. J. Ophthalmic Vis. Res. 2017, 12, 243–244. [Google Scholar] [CrossRef]
- Gardiner, C.; Lanigan, B.; O'Keefe, M. Postcataract surgery outcome in a series of infants and children with Down syndrome. Br. J. Ophthalmol. 2008, 92, 1112–1116. [Google Scholar] [CrossRef]
- Tataru, C.I.; Voinea, L.M.; Tataru, C.P.; Sima, G. Clinical and therapeutic particularities of congenital cataracts in pediatric patients with Down Syndrome. Rom. J. Ophthalmol. 2020, 64, 168–175. [Google Scholar] [CrossRef]
- Santoro, S.L.; Atoum, D.; Hufnagel, R.B.; Motley, W.W. Surgical, medical and developmental outcomes in patients with Down syndrome and cataracts. SAGE Open Med. 2017, 5, 2050312117715583. [Google Scholar] [CrossRef]
- Sherk, M.C.; Williams, T.D. Disc Vascularity in Downʼs Syndrome. Optom. Vis. Sci. 1979, 56, 509–511. [Google Scholar] [CrossRef]
- Ahmad, A.; Pruett, R.C. The Fundus in Mongolism. Arch. Ophthalmol. 1976, 94, 772–776. [Google Scholar] [CrossRef]
- AlAhmadi, B.O.; Alsulaiman, S.M.; Arevalo, J.F. Retinal Detachment in Down Syndrome: Characteristics and Surgical Outcomes. J. Ophthalmol. 2016, 2016, 6971591. [Google Scholar] [CrossRef]
- Satgé, D. Are Patients with Down Syndrome Predisposed to Retinal Neoplasms? Ophthalmic Genet. 2009, 30, 155. [Google Scholar] [CrossRef]
- Schneier, A.J.; Heidary, G.; Ledoux, D.M. Optic Nerve Appearance in Patients with Down Syndrome. J. Pediatr. Ophthalmol. Strabismus 2013, 50, 60. [Google Scholar] [CrossRef]
- Esmaili, N.; Bradfield, Y.S. Pseudotumor Cerebri in Children with Down Syndrome. Ophthalmology 2007, 114, 1773–1778. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Sun, E.; Kraus, C.L. The Ophthalmic Manifestations of Down Syndrome. Children 2023, 10, 341. https://doi.org/10.3390/children10020341
Sun E, Kraus CL. The Ophthalmic Manifestations of Down Syndrome. Children. 2023; 10(2):341. https://doi.org/10.3390/children10020341
Chicago/Turabian StyleSun, Emily, and Courtney L. Kraus. 2023. "The Ophthalmic Manifestations of Down Syndrome" Children 10, no. 2: 341. https://doi.org/10.3390/children10020341
APA StyleSun, E., & Kraus, C. L. (2023). The Ophthalmic Manifestations of Down Syndrome. Children, 10(2), 341. https://doi.org/10.3390/children10020341





