The Effectiveness of the Schroth Best Practice Program and Chêneau-Type Brace Treatment in Adolescent Idiopathic Scoliosis: Long-Term Follow-Up Evaluation Results
Abstract
:1. Introduction
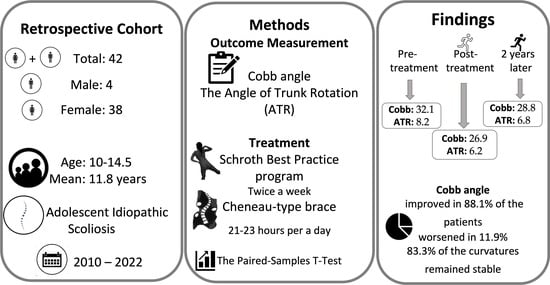
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Fadzan, M.; Bettany-Saltikov, J. Etiological Theories of Adolescent Idiopathic Scoliosis: Past and Present. Open Orthop. J. 2017, 11, 1466–1489. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Asher, M.A.; Burton, D.C. Adolescent idiopathic scoliosis: Natural history and long term treatment effects. Scoliosis 2006, 1, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lonstein, J. Idiopathic scoliosis. In Moe’s Textbook of Scoliosis and Other Spinal Deformities, 3rd ed.; Lonstein, J., Winter, R., Bradford, S., Ogilvie, J., Eds.; W. B. Saunders Ltd.: Philadelphia, PA, USA, 1995; pp. 219–256. [Google Scholar]
- MacLean, W.E., Jr.; Green, N.E.; Pierre, C.B.; Ray, D.C. Stress and coping with scoliosis: Psychological effects on adolescents and their families. J. Pediatr. Orthop. 1989, 9, 257–261. [Google Scholar] [CrossRef]
- Lonstein, J.E. Scoliosis: Surgical versus nonsurgical treatment. Clin. Orthop. Relat. Res. 2006, 443, 248–259. [Google Scholar] [CrossRef]
- Lonstein, J.E.; Carlson, J.M. The prediction of curve progression in untreated idiopathic scoliosis during growth. J. Bone Jt. Surg. 1984, 66, 1061–1071. [Google Scholar] [CrossRef] [Green Version]
- Bettany-Saltikov, J.; Weiss, H.R.; Chockalingam, N.; Taranu, R.; Srinivas, S.; Hogg, J.; Whittaker, V.; Kalyan, R.V.; Arnell, T. Surgical versus non-surgical interventions in people with adolescent idiopathic scoliosis. Cochrane Database Syst. Rev. 2015, 4, CD010663. [Google Scholar] [CrossRef] [Green Version]
- Kotwicki, T.; Chowanska, J.; Kinel, E.; Czaprowski, D.; Tomaszewski, M.; Janusz, P. Optimal management of idiopathic scoliosis in adolescence. Adolesc. Health Med. Ther. 2013, 4, 59–73. [Google Scholar] [CrossRef] [Green Version]
- Sy, N.; Bettany-Saltikov, J.; Moramarco, M. Evidence for Conservative Treatment of Adolescent Idiopathic Scoliosis—Update 2015 (Mini-Review). Curr. Pediatr. Rev. 2016, 12, 6–11. [Google Scholar] [CrossRef]
- Fang, M.Q.; Huang, X.L.; Wang, W.; Li, Y.A.; Xiang, G.H.; Yan, G.K.; Ke, C.R.; Mao, C.H.; Wu, Z.Y.; Pan, T.L.; et al. The efficacy of Schroth exercises combined with the Chêneau brace for the treatment of adolescent idiopathic scoliosis: A retrospective controlled study. Disabil. Rehabil. 2022, 44, 5060–5068. [Google Scholar] [CrossRef]
- Weiss, H.R.; Turnbull, D.; Seibel, S.; Kleban, A. First end-result of a prospective cohort with AIS treated with a CAD Chêneau style brace. J. Phys. Ther. Sci. 2019, 31, 983–991. [Google Scholar] [CrossRef] [Green Version]
- Kuru, T.; Yeldan, İ.; Dereli, E.E.; Özdinçler, A.R.; Dikici, F.; Çolak, İ. The efficacy of three-dimensional Schroth exercises in adolescent idiopathic scoliosis: A randomised controlled clinical trial. Clin. Rehabil. 2016, 30, 181–190. [Google Scholar] [CrossRef] [PubMed]
- Negrini, S.; Donzelli, S.; Lusini, M.; Minnella, S.; Zaina, F. The effectiveness of combined bracing and exercise in adolescent idiopathic scoliosis based on SRS and SOSORT criteria: A prospective study. BMC Musculoskelet. Disord. 2014, 15, 263. [Google Scholar] [CrossRef] [Green Version]
- Herring, J.A. Tachdjian’s Pediatric Orthopaedics, 3rd ed.; W. B. Saunders Company: New York, NY, USA, 2002; pp. 213–299. [Google Scholar]
- Negrini, S.; Donzelli, S.; Aulisa, A.G.; Czaprowski, D.; Schreiber, S.; de Mauroy, J.C.; Diers, H.; Grivas, T.B.; Knott, P.; Kotwicki, T.; et al. 2016 SOSORT guidelines: Orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord. 2018, 13, 3. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Akçay, B.; Çolak, T.K.; Apti, A.; Çolak, İ.; Kızıltaş, Ö. The reliability of the augmented Lehnert-Schroth and Rigo classification in scoliosis management. S. Afr. J. Physiother. 2021, 77, 1568. [Google Scholar] [CrossRef]
- Weiss, H.R.; Lehnert-Schroth, C.; Moramarco, M. Schroth Therapy: Advances in Conservative Scoliosis Treatment; LAP Lambert Academic Publishing: Saarbruecken, Germany, 2015. [Google Scholar]
- Risser, J.C. The Iliac apophysis; an invaluable sign in the management of scoliosis. Clin. Orthop. 1958, 11, 111–119. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotwicki, T. Risser sign: The value of the lateral spinal radiograph to assess the excursion of the iliac apophysis. Stud. Health Technol. Inform. 2008, 140, 44–47. [Google Scholar]
- Marshall, W.A.; Tanner, J.M. Variations in the pattern of pubertal changes in boys. Arch. Dis. Child. 1970, 45, 13–23. [Google Scholar] [CrossRef] [Green Version]
- Marshall, W.A.; Tanner, J.M. Variations in pattern of pubertal changes in girls. Arch. Dis. Child. 1969, 44, 291–303. [Google Scholar] [CrossRef] [Green Version]
- Amendt, L.E.; Ause-Ellias, K.L.; Eybers, J.L.; Wadsworth, C.T.; Nielsen, D.H.; Weinstein, S.L. Validity and reliability testing of the Scoliometer. Phys. Ther. 1990, 70, 108–117. [Google Scholar] [CrossRef]
- Moramarco, M.; Borysov, M.; Ng, S.Y.; Weiss, H.R. Schroth’s Textbook of Scoliosis and Other Spinal Deformities; Cambridge Scholars Publishing: Newcastle, UK, 2020. [Google Scholar]
- Berdishevsky, H.; Lebel, V.A.; Bettany-Saltikov, J.; Rigo, M.; Lebel, A.; Hennes, A.; Romano, M.; Białek, M.; M’Hango, A.; Betts, T.; et al. Physiotherapy scoliosis-specific exercises—A comprehensive review of seven major schools. Scoliosis Spinal Disord. 2016, 11, 20. [Google Scholar] [CrossRef] [Green Version]
- Weiss, H.R.; Çolak, T.K.; Lay, M.; Borysov, M. Brace treatment for patients with scoliosis: State of the art. S. Afr. J. Physiother. 2021, 77, 1573. [Google Scholar] [CrossRef] [PubMed]
- Richards, B.S.; Bernstein, R.M.; D’Amato, C.R.; Thompson, G.H. Standardization of criteria for adolescent idiopathic scoliosis brace studies: SRS Committee on Bracing and Nonoperative Management. Spine 2005, 30, 2068–2077. [Google Scholar] [CrossRef] [Green Version]
- Weiss, H.R.; Tournavitis, N.; Seibel, S.; Kleban, A. A Prospective Cohort Study of AIS Patients with 40° and More Treated with a Gensingen Brace (GBW): Preliminary Results. Open Orthop. J. 2017, 11, 1558–1567. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Aulisa, A.G.; Guzzanti, V.; Falciglia, F.; Giordano, M.; Galli, M.; Aulisa, L. Brace treatment of Idiopathic Scoliosis is effective for a curve over 40 degrees, but is the evaluation of Cobb angle the only parameter for the indication of treatment? Eur. J. Phys. Rehabil. Med. 2019, 55, 231–240. [Google Scholar] [CrossRef]
- Rigo, M.; Jelačić, M. Brace technology thematic series: The 3D Rigo Chêneau-type brace. Scoliosis Spinal Disord. 2017, 12, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Negrini, S.; Atanasio, S.; Fusco, C.; Zaina, F. Effectiveness of complete conservative treatment for adolescent idiopathic scoliosis (bracing and exercises) based on SOSORT management criteria: Results according to the SRS criteria for bracing studies—SOSORT Award 2009 Winner. Scoliosis 2009, 4, 19. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kotwicki, T. Improved accuracy in Risser sign grading with lateral spinal radiography. Eur. Spine J. 2008, 17, 1676–1685. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Little, D.G.; Sussman, M.D. The Risser sign: A critical analysis. J. Pediatr. Orthop. 1994, 14, 569–575. [Google Scholar] [CrossRef]
- Little, D.G.; Song, K.M.; Katz, D.; Herring, J.A. Relationship of peak height velocity to other maturity indicators in idiopathic scoliosis in girls. J. Bone Jt. Surg. 2000, 82, 685–693. [Google Scholar] [CrossRef]
- Hoppenfeld, S.; Lonner, B.; Murthy, V.; Gu, Y. The rib epiphysis and other growth centers as indicators of the end of spinal growth. Spine 2004, 29, 47–50. [Google Scholar] [CrossRef]
- Weiss, H.R.; Weiss, G.; Schaar, H.J. Conservative management in patients with scoliosis--does it reduce the incidence of surgery? Stud. Health Technol. Inform. 2002, 91, 342–347. [Google Scholar] [PubMed]
- Zaina, F.; Negrini, S.; Atanasio, S.; Fusco, C.; Romano, M.; Negrini, A. Specific exercises performed in the period of brace weaning can avoid loss of correction in Adolescent Idiopathic Scoliosis (AIS) patients: Winner of SOSORT’s 2008 Award for Best Clinical Paper. Scoliosis 2009, 4, 8. [Google Scholar] [CrossRef] [PubMed] [Green Version]



| Variables | Mean ± SD Median (min–max) |
|---|---|
| Age (years) | 11.8 ± 1.3 11 (10–14.5) |
| Risser grade | 0.2 ± 0.5 0 (0–2) |
| Tanner stage | 1.9 ± 1 2 (0–4) |
| Height (cm) | 153.7 ± 11.4 (121–175) |
| Weight (kg) | 42.5 ± 9.6 (23–62) |
| BMI (kg/m2) | 18.1 ± 2.8 (12.7–23.6) |
| Reached maximum daily brace wearing time (hours) | 20.4 ± 2.4 (12–23) |
| Total duration of brace use (months) | 35.1 ± 17.4 29.5 (18–87) |
| Start of the Treatment Mean ± SD (min–max) | End of the Treatment Mean ± SD (min–max) | Last Follow-Up Mean ± SD (min–max) | p Value | Mean Change | |
|---|---|---|---|---|---|
| Cobb angle | 32.1 ± 7.3 (20–47) | 26.9 ± 9.9 (10–48) | 28.8 ± 10.1 (12–48) | * 0.000 | C1 −5.1 ± 7.3 (−17–12) |
| ** 0.013 | C2 −3 ± 7.4 (−17–15) | ||||
| *** 0.007 | C3 1.9 ± 4.7 (−13–18) | ||||
| ATR | 8.2 ± 3.7 (2–17) | 6.2 ± 3.1 (1–13) | 6.8 ± 3 (1–16) | * 0.001 | C1 −1.7 ± 3.6 (−11–6) |
| ** 0.113 | C2 −1.1 ± 3.4 (−8–6) | ||||
| *** 0.014 | C3 0.6 ± 2.5 (−6–9) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuru Çolak, T.; Akçay, B.; Apti, A.; Çolak, İ. The Effectiveness of the Schroth Best Practice Program and Chêneau-Type Brace Treatment in Adolescent Idiopathic Scoliosis: Long-Term Follow-Up Evaluation Results. Children 2023, 10, 386. https://doi.org/10.3390/children10020386
Kuru Çolak T, Akçay B, Apti A, Çolak İ. The Effectiveness of the Schroth Best Practice Program and Chêneau-Type Brace Treatment in Adolescent Idiopathic Scoliosis: Long-Term Follow-Up Evaluation Results. Children. 2023; 10(2):386. https://doi.org/10.3390/children10020386
Chicago/Turabian StyleKuru Çolak, Tuğba, Burçin Akçay, Adnan Apti, and İlker Çolak. 2023. "The Effectiveness of the Schroth Best Practice Program and Chêneau-Type Brace Treatment in Adolescent Idiopathic Scoliosis: Long-Term Follow-Up Evaluation Results" Children 10, no. 2: 386. https://doi.org/10.3390/children10020386
APA StyleKuru Çolak, T., Akçay, B., Apti, A., & Çolak, İ. (2023). The Effectiveness of the Schroth Best Practice Program and Chêneau-Type Brace Treatment in Adolescent Idiopathic Scoliosis: Long-Term Follow-Up Evaluation Results. Children, 10(2), 386. https://doi.org/10.3390/children10020386