Orthodontic Approaches in the Management of Mandibular Fractures: A Scoping Review
Abstract
1. Introduction
2. Materials and Methods
2.1. Searching Strategies
2.2. Article Selection
3. Results
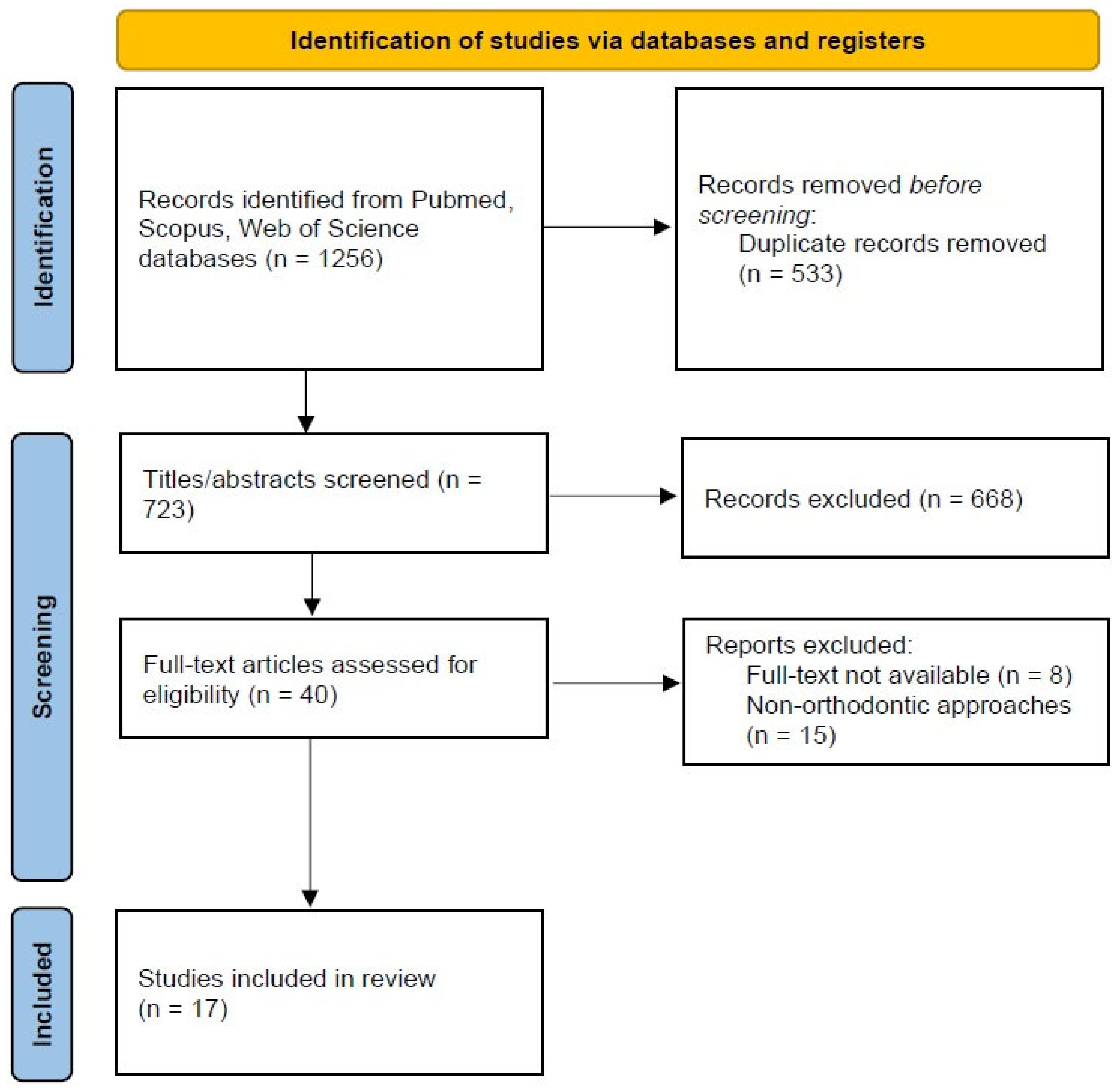
3.1. Study Selection
3.2. Description of the Included Studies
3.3. Mandibular Fracture Management
3.3.1. Removable and Cemented Acrylic Splints
3.3.2. Hybrid Protocols and Rigid Orthodontic Splints
3.3.3. Intermaxillary Fixation with Orthodontic Brackets and Mini-Screws
| Study | Aim | Sample | Design of the Study | Site of the Mandibular Fracture | Approach | Main Findings |
|---|---|---|---|---|---|---|
| Agarwal RM et al. (2014) [56] | To present a variety of therapeutic techniques for pediatric mandibular fractures. | 19 subjects (3–12 y) | Case series | symphysis/parasymphysis (9), body (4), parasymphysis + condylar (4), body + condyle (1), and body + parasymphysis (1) | Acrylic cap splint (with circummandibular wiring or cemented) or Erich arch bar | Given the ages and anatomical diversity of children, managing pediatric mandibular fractures is difficult. Symphysis/parasymphysis fractures were the most prevalent kind of mandibular fracture in this case series, accounting for 42% of all fractures. Pediatric dentists play a crucial role in treating children who have such fractures. If the right guidelines are followed, children should obtain satisfactory results with the least amount of discomfort. |
| Aizendbud D et al. (2008) [57] | To describe the production of the orthodontic fixation device, treatment concerns, and long-term follow-up results (10 y). | 1 subject (5 y) | Case report with 10 y follow-up | Parasymphysis with minimal displacement | Cemented rigid modified orthodontic splint appliance | Growth may be affected in an unforeseen way if the mandible’s periosteal envelope is compromised. Therefore, a closed reduction is preferred in children who need help. In this instance, the 10-year follow-up showed that the orthodontic fixation splint approach, which is noninvasive, can offer a superior and effective treatment for mandibular fracture in young children. |
| Boffano P et al. (2012) [58] | To present conservative measures as options for treating subjects with mixed dentition who had a series of unilateral displaced condylar fractures. | 25 subjects (6–12 y) | Non-controlled prospective study with 1 y follow-up | Unilateral condylar with displacement | Fixed orthodontic appliances, acrylic splints, rubber bands, and functional exercises | At 12 months of follow-up, a conservative treatment of displaced unilateral condylar fractures in children with mixed dentition produced good functional results. The correct reconstruction of the condyles was guided by a splint that was progressively modified, allowing the fractured process to regain its normal forms and heights. Condylar fractures in kids between the ages of 6 and 13 can still be treated non-surgically, which is still the best option to preserve healthy growth and function. |
| Cazzolla AP et al. (2018) [59] | To present the therapeutic option of a condylar neck fracture in an 11-year-old boy. | 1 subject (11 y) | Case report with 1 y follow-up | condylar neck with minimal displacement | Removable acrylic splint and functional exercises | With a lower-resin splint, a non-surgical treatment for a child’s condylar neck fracture can restore mandibular motions and appearance. After a year of treatment, facial growth was normal. In certain circumstances with a mildly displaced condyle, a conservative treatment may be recommended for children. |
| Chen CY et al. (2010) [60] | To propose an innovative method, the direct bonding technique, as an alternative to intermaxillary fixation with arch bars or looped wires. | 2 subjects (19–28 y) | Case series with 3-month follow-up | Condylar or condylar + parasymphysis and body | Bonding of brackets and wires + elastics | This novel approach did not require the insertion of interdental wires in the typical manner. The removal of challenges, time requirements, and penetration risk thereby benefits the practitioner. Compared to arch bars or looped wires, it also lessens pain and tension for the patient, and dental hygiene is much improved. |
| Choubey S et al. (2014) [61] | To highlight the benefits of a vacuum-formed splint that was selected as a viable and successful conservative therapy strategy for the management of maxillofacial injuries. | 1 subject (9 y) | Case report with 2 y follow-up | Parasymphysis with displacement | Cemented vacuum-formed splint | Compared to fractures in the adult population, pediatric maxillofacial traumas necessitate different therapeutic treatment approaches. The prognoses for many dentoalveolar injuries can be considerably improved with prompt and adequate care. The most crucial element, time, determines the course of treatment and its result. |
| Kocaaslan BK et al. (2022) [62] | To compare conservative treatment modalities for condylar fractures and determine the best option using CT images. | 24 subjects (18–48 y) | Retrospective study with 6-month follow-up | condylar neck (bilateral or unilateral) | Bracketing, arch bar, or mini-screw (+ eventual occlusal splint) | No statistically significant differences were detected between the treatment modalities in the condylar length difference (affected side vs. unaffected side). An acceptable and more conservative form of treatment is intermaxillary fixation with an occlusal splint, as opposed to an open reduction. |
| Qadri GW et al. (2008) [63] | In order to reduce the risk of complications, a case of a juvenile mandibular fracture treated with direct interdental wire and an acrylic splint instead of absorbable plates and screws was discussed. | 1 subject (14 y) | Case report with 6-month follow-up | Symphysis with minimal displacement | Interdental wiring (0.5 mm stainless-steel wire) + cemented acrylic splint | With the use of an acrylic splint and direct interdental wiring, the subject was successfully treated. |
| Sabbagh HT et al. (2022) [64] | To evaluate and monitor the progress of a conservative treatment strategy using a functional orthodontic appliance for the treatment of mandibular condyle fractures in young patients. | 8 subjects (mean age: 8.3 y) | Retrospective study (follow-up not specified) | Condyle (bilateral or unilateral) | Functional removable appliance | The concept of a conservative functional approach in growing patients is supported by the positive functional and morphologic outcomes of functional orthodontic treatment. When treating growing patients with conservative measures for mandibular condyle fractures, functional adjunctive therapy should be taken into account. |
| Saskianti T et al. (2022) [65] | To aid pediatric dentists in managing this distinct and highly specialized area of traumatology by providing them with better knowledge on how to treat mandibular fractures in children. | 1 subject (9 y) | Case report with 2-month follow-up | Symphysis/parasymphysis | Cemented closed-cap acrylic splint | Pediatric mandibular fractures treated with modified closed-cap splints, particularly those in the symphysis/parasymphysis region, are safe and successful. |
| Tehranchi A et al. (2013) [66] | To provide a case of a young subject who had maxillofacial trauma and needed cautious multidisciplinary care after suffering severe injuries in a plane crash. | 1 subject (25 y) | Case report with 6-month follow-up | Symphysis and greenstick fracture at the anterior border of the ramus | Mini-screw and elastics + orthodontic brackets and wire | The proposed technique could constitute an adjunctive treatment to assist in the management of complex and multidisciplinary cases. |
| Trupthi DV et al. (2014) [67] | To assess the clinical effectiveness of arch bars against vacuum-produced splints in the management of mildly displaced mandibular fractures. | 40 subjects (18–55 y) | Non-randomized comparative prospective study: group 1 (cemented vacuum-formed splint + elastics) vs. group 2 (arch bar), with 2-month follow-up | Minimally displaced mandibular fractures | Cemented vacuum-formed splint + elastics and arch bar | Regarding chair-side time, periodontal health, patient compliance with maintaining oral hygiene, mastication, and speech, vacuum-produced splints are superior to arch bars. Needlestick injuries are prevented by using vacuum-formed splints. Therefore, they can be applied to minimally displaced mandibular fractures for intermaxillary fixation. |
| Tuna EB et al. (2012) [68] | To clinically and radiologically review the results of the conservative approach of a 10-year-old subject who had a unilateral greenstick fracture for the previous 2.5 years. | 1 subject (10 y) | Case report with 2.5 y follow-up | Unilateral greenstick condylar fracture | Removable acrylic mandibular splint | Children with unilateral fractures of the mandibular condyle may avoid deformation in future growth by using a non-surgical functional approach. Condylar growth could occur continuously and simultaneously during the growing period as a result of the proliferation in the chondrocyte layer, which promotes new bone formation in the fragmented condyle. |
| Utley DS et al. (1998) [69] | To evaluate the efficacy, ease of use, and safety profile of orthodontic direct bonded bracket fixation. | 32 subjects (16–42 y) | Non-controlled prospective study with 44.4 ± 51.6-week follow-up (MMF/DDB or MMF/DDB + ORIF or arch bars) | Symphysis, angle, condylar neck, coronoid, and body. | Orthodontic brackets + elastics (with eventual ORIF) or arch bars | For less complicated subcondylar, angle, body, and symphyseal mandibular fractures, MMF/DBB is effective as the sole treatment strategy. In more difficult fractures, MMF/DBB is a useful preoperative addition to ORIF. |
| Wu Y et al. (2012) [70] | To assess the viability and safety of using an occlusal splint with a specially developed screw-based semi-rigid intermaxillary fixation in the conservative management of pediatric mandibular condylar fractures. | 13 subjects (<12 y) | Retrospective study with 28.6-month mean follow-up | Condyle with displacement | Mini-screw and elastics + vacuum-formed occlusal splint | This approach may be a secure, simple, and efficient way to treat condylar fractures in children. |
| Xu YH et al. (2016) [71] | To describe a variant of the conservative fixed orthodontic treatment that was added to help a child with a bilateral condylar fracture heal. | 1 subject (10 y) | Case report with 49-month follow-up | Condyle with displacement and symphysis | Bracket with 0.018 in Australian wire and elastics | A mandibular fracture can be treated conservatively with fixed orthodontics, which is an effective treatment approach that is generally simple, affordable, and acceptable to patients. |
| Zhao YM et al. (2014) [72] | To assess how a removable occlusal splint affects the treatment of condylar fractures in children and adolescents. | 40 subjects (3–16 y) | Retrospective study with 14 months to 4 years of follow-up | Condyle | Removable occlusal splint | Condylar fractures in children can be successfully treated with conservative measures. A potential method for treating condylar fractures in children and teenagers is a removable occlusal splint. |
4. Discussion
4.1. Management of Mandibular Fractures in Adults
4.1.1. Minimally Displaced Mandibular Body Fractures in Adults
4.1.2. Minor Condylar Fractures in Adults
4.2. Management of Mandibular Fractures in Children
4.2.1. Condylar Fractures in Children
4.2.2. Minor mandibular Body Fractures in Children
4.3. Limitations and Future Directions
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Koshy, J.C.; Feldman, E.M.; Chike-Obi, C.J.; Bullocks, J.M. Pearls of mandibular trauma management. Semin. Plast. Surg. 2010, 24, 357–374. [Google Scholar] [CrossRef]
- Breeland, G.; Aktar, A.; Patel, B.C. Anatomy, head and neck, mandible. In StatPearls; StatPearls Publishing: St. Petersburg, FL, USA, 2022. [Google Scholar]
- Ngeow, W.C.; Chai, W.L. The clinical anatomy of accessory mandibular canal in dentistry. Clin. Anat. 2020, 33, 1214–1227. [Google Scholar] [CrossRef]
- Iwanaga, J.; Shiromoto, K.; Kato, T.; Tanaka, T.; Ibaragi, S.; Tubbs, R.S. Anatomy of the mandibular canal and surrounding structures. Part II: Cancellous pattern of the mandible. Ann. Anat.-Anat. Anz. 2020, 232, 151583. [Google Scholar] [CrossRef] [PubMed]
- Xie, L.; Li, T.; Chen, J.; Yin, D.; Wang, W.; Xie, Z. Cone-beam CT assessment of implant-related anatomy landmarks of the anterior mandible in a Chinese population. Surg. Radiol. Anat. 2019, 41, 927–934. [Google Scholar] [CrossRef] [PubMed]
- Vallabh, R.; Zhang, J.; Fernandez, J.; Dimitroulis, G.; Ackland, D.C. The morphology of the human mandible: A computational modelling study. Biomech. Model. Mechanobiol. 2020, 19, 1187–1202. [Google Scholar] [CrossRef] [PubMed]
- Calloway, D.M.; Anton, M.A.; Jacobs, J.S. Changing concepts and controversies in the management of mandibular fractures. Clin. Plast. Surg. 1992, 19, 59–69. [Google Scholar] [CrossRef]
- Trivedi, B.; Kesterke, M.J.; Bhattacharjee, R.; Weber, W.; Mynar, K.; Reddy, L.V. Craniofacial injuries seen with the introduction of bicycle-share electric scooters in an urban setting. J. Oral Maxillofac. Surg. 2019, 77, 2292–2297. [Google Scholar] [CrossRef]
- Blomberg, S.N.F.; Rosenkrantz, O.C.M.; Lippert, F.; Christensen, H.C. Injury from electric scooters in Copenhagen: A retrospective cohort study. BMJ Open 2019, 9, e033988. [Google Scholar] [CrossRef]
- Lalloo, R.; Lucchesi, L.R.; Bisignano, C.; Castle, C.D.; Dingels, Z.V.; Fox, J.T.; Hamilton, E.B.; Liu, Z.; Roberts, N.L.; Sylte, D.O. Epidemiology of facial fractures: Incidence, prevalence and years lived with disability estimates from the Global Burden of Disease 2017 study. Inj. Prev. 2020, 26, i27–i35. [Google Scholar] [CrossRef]
- Olding, J.; Zisman, S.; Olding, C.; Fan, K. Penetrating trauma during a global pandemic: Changing patterns in interpersonal violence, self-harm and domestic violence in the Covid-19 outbreak. Surgeon 2021, 19, e9–e13. [Google Scholar] [CrossRef]
- Høye, A. Bicycle helmets–To wear or not to wear? A meta-analyses of the effects of bicycle helmets on injuries. Accid. Anal. Prev. 2018, 117, 85–97. [Google Scholar] [CrossRef]
- Vandoros, S. COVID-19, lockdowns and motor vehicle collisions: Empirical evidence from Greece. Inj. Prev. 2022, 28, 81–85. [Google Scholar] [CrossRef] [PubMed]
- Erdmann, D.; Follmar, K.E.; DeBruijn, M.; Bruno, A.D.; Jung, S.-H.; Edelman, D.; Mukundan, S.; Marcus, J.R. A retrospective analysis of facial fracture etiologies. Ann. Plast. Surg. 2008, 60, 398–403. [Google Scholar] [CrossRef]
- Ellis, E., III; Moos, K.F.; El-Attar, A. Ten years of mandibular fractures: An analysis of 2,137 cases. Oral Surg. Oral Med. Oral Pathol. 1985, 59, 120–129. [Google Scholar] [CrossRef]
- Furr, A.M.; Schweinfurth, J.M.; May, W.L. Factors associated with long-term complications after repair of mandibular fractures. Laryngoscope 2006, 116, 427–430. [Google Scholar] [CrossRef] [PubMed]
- Fadl, S.A.; Sandstrom, C.K. Pattern recognition: A mechanism-based approach to injury detection after motor vehicle collisions. RadioGraphics 2019, 39, 857–876. [Google Scholar] [CrossRef] [PubMed]
- Diab, J.; Flapper, W.J.; Anderson, P.J.; Moore, M.H. Patterns of mandibular fractures in South Australia: Epidemiology, treatment, and clinical outcomes. J. Craniofacial Surg. 2022, 33, 1018–1022. [Google Scholar] [CrossRef]
- Hesham, A.; Geiger, J.; Alshamrani, Y.; Sawatari, Y. Can the mechanism of injury impact the location of a mandibular fracture? A systematic review. J. Maxillofac. Oral Surg. 2022, 2022, 1–8. [Google Scholar] [CrossRef]
- Piasecki, J.H.; Gutowski, K.A.; Lahvis, G.P.; Moreno, K.I. An experimental model for improving fat graft viability and purity. Plast. Reconstr. Surg. 2007, 119, 1571–1583. [Google Scholar] [CrossRef]
- Reddy, L.; Lee, D.; Vincent, A.; Shokri, T.; Sokoya, M.; Ducic, Y. Secondary management of mandible fractures. Facial Plast. Surg. 2019, 35, 627–632. [Google Scholar] [CrossRef]
- Saccomanno, S.; Quinzi, V.; D’Andrea, N.; Albani, A.; Paskay, L.C.; Marzo, G. Traumatic Events and Eagle Syndrome: Is There Any Correlation? A Systematic Review. Healthcare 2021, 9, 825. [Google Scholar] [CrossRef]
- Stone, N.; Corneman, A.; Sandre, A.R.; Farrokhyar, F.; Thoma, A.; Cooper, M.J. Treatment delay impact on open reduction internal fixation of mandibular fractures: A systematic review. Plast. Reconstr. Surg. Glob. Open 2018, 6, e1829. [Google Scholar] [CrossRef]
- Elsayed, S.A.; Abdullah, A.A.B.; Dar-Odeh, N.; Altaweel, A.A. Intraoral Wound Dehiscence After Open Reduction Internal Fixation of Mandibular Fractures: A Retrospective Cohort Study. Wounds Compend. Clin. Res. Pract. 2021, 33, 60–64. [Google Scholar]
- Zhang, B.; Yang, M.; Zhou, Q.; Liu, Q. Delayed open reduction and single screw internal fixation as a treatment option in cases of failed non-surgical treatment of bilateral condylar head fractures with fragmentation. J. Craniomaxillofac. Surg. 2016, 44, 1655–1661. [Google Scholar] [CrossRef] [PubMed]
- Barry, R.G.; Wolbert, T.T.; Gress, T.W.; Ray, P.D.; Mozaffari, F.B. Outcomes after open reduction with internal fixation of mandible fractures. J. Craniofacial. Surg. 2018, 29, 1237–1240. [Google Scholar] [CrossRef]
- Stone, I.E.; Dodson, T.B.; Bays, R.A. Risk factors for infection following operative treatment of mandibular fractures: A multivariate analysis. Plast. Reconstr. Surg. 1993, 91, 64–68. [Google Scholar] [CrossRef] [PubMed]
- Bansal, A.; Yadav, P.; Bhutia, O.; Roychoudhury, A.; Bhalla, A.S. Comparison of outcome of open reduction and internal fixation versus closed treatment in pediatric mandible fractures-a retrospective study. J. Cranio-Maxillofac. Surg. 2021, 49, 196–205. [Google Scholar] [CrossRef] [PubMed]
- Ravikumar, C.; Bhoj, M. Evaluation of postoperative complications of open reduction and internal fixation in the management of mandibular fractures: A retrospective study. Indian J. Dent. Res. 2019, 30, 94. [Google Scholar]
- Cillo Jr, J.E.; Godwin, S.; Becker, E.; Schorr, R. Neurosensory recovery following mental nerve skeletonization in intraoral open reduction and internal fixation of mandible fractures. J. Oral Maxillofac. Surg. 2021, 79, 183–191. [Google Scholar] [CrossRef]
- Chen, C.-C.; Yang, C.-H.; Chang, Y.-J.; Wu, C.-C.; Chang, L.-R.; Lai, J.-P. Repairing Facial Fractures with Interrupted Maxillary-mandibular Arches by Computer-assisted Reverse Planning Model Surgery. Plast. Reconstr. Surg. Glob. Open 2022, 10, e4149. [Google Scholar] [CrossRef]
- Choi, J.-W.; Kim, H.B.; Jeong, W.S.; Kim, S.C.; Koh, K.S. Comparison between intermaxillary fixation with screws and an arch bar for mandibular fracture. J. Craniofacial Surg. 2019, 30, 1787–1789. [Google Scholar] [CrossRef]
- Kumar, S.; Gupta, P.; Singh, D.; Sharma, A. Modified Treatment Protocol for Managing Mandibular Fracture With Orthodontic Brackets and Elastics-A Rare Case Report. J. Indira Gandhi Inst. Med. Sci. 2020, 6, 169. [Google Scholar]
- Bonetti, G.A.; Parenti, S.I.; Gracco, A. Passive Archwires for Intermaxillary Fixation in Surgical Cases: A Clinical Report. J. Can. Dent. Assoc. 2011, 77, b159. [Google Scholar]
- Roccia, F.; Sobrero, F.; Raveggi, E.; Rabufetti, A.; Scolozzi, P.; Dubron, K.; Politis, C.; Ganasouli, D.; Zanakis, S.N.; Jelovac, D. European multicenter prospective analysis of the use of maxillomandibular fixation for mandibular fractures treated with open reduction and internal fixation. J. Stomatol. Oral Maxillofac. Surg. 2022, 124, 101376. [Google Scholar] [CrossRef]
- Maloney, K.; Rutner, T. Virtual surgical planning and hardware fabrication prior to open reduction and internal fixation of atrophic edentulous mandible fractures. Craniomaxillofacial Trauma Reconstr. 2019, 12, 156–162. [Google Scholar] [CrossRef]
- Vatsa, P.; Siddaraju, A. A comparative clinical study on self-drilling screws and Erich arch bars in mandibular fractures. Int. J. Appl. Dent. Sci. 2018, 4, 212–217. [Google Scholar]
- Mittal, H.C.; Yadav, S.; Shekhawat, H. Conservative management of pediatric mandibular distal fractures—A retrospective study. Dent. Traumatol. 2021, 37, 321–329. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Taneja, S.; Rai, A. What is a better modality of maxillomandibular fixation: Bone-supported arch bars or Erich arch bars? A systematic review and meta-analysis. Br. J. Oral Maxillofac. Surg. 2021, 59, 858–866. [Google Scholar] [CrossRef]
- Stähli, C.; Eliades, T.; Papageorgiou, S.N. Functional appliance treatment for mandibular fractures: A systematic review with meta-analyses. J. Oral Rehabil. 2021, 48, 945–954. [Google Scholar] [CrossRef]
- Bell, R.B.; Thompson, L.; Amundson, M. Contemporary management of mandibular fractures. In Peterson’s Principles of Oral and Maxillofacial Surgery; Springer: Cham, Switzerlands, 2022; pp. 581–647. [Google Scholar]
- Konaş, E.; Tunçbilek, G.; Kayikçioğlu, A.; Akcan, C.A.; Kocadereli, I.; Mavili, M.E. Splint-assisted reduction of comminuted or complex maxillofacial fractures. J. Craniofac. Surg. 2011, 22, 1471–1475. [Google Scholar] [CrossRef]
- Satpute, A.S.; Mohiuddin, S.A.; Doiphode, A.M.; Kulkarni, S.S.; Qureshi, A.A.; Jadhav, S.B. Comparison of Erich arch bar versus embrasure wires for intraoperative intermaxillary fixation in mandibular fractures. Oral Maxillofac. Surg. 2018, 22, 419–428. [Google Scholar] [CrossRef]
- Glazer, M.; Joshua, B.Z.; Woldenberg, Y.; Bodner, L. Mandibular fractures in children: Analysis of 61 cases and review of the literature. Int. J. Pediatr. Otorhinolaryngol. 2011, 75, 62–64. [Google Scholar] [CrossRef]
- Zimmermann, C.; Troulis, M.; Kaban, L. Pediatric facial fractures: Recent advances in prevention, diagnosis and management. Int. J. Oral Maxillofac. Surg. 2005, 34, 823–833. [Google Scholar] [CrossRef] [PubMed]
- Zhou, W.; An, J.; He, Y.; Zhang, Y. Analysis of pediatric maxillofacial trauma in North China: Epidemiology, pattern, and management. Injury 2020, 51, 1561–1567. [Google Scholar] [CrossRef] [PubMed]
- Țenț, P.A.; Juncar, R.I.; Moca, A.E.; Moca, R.T.; Juncar, M. The Etiology and Epidemiology of Pediatric Facial Fractures in North-Western Romania: A 10-Year Retrospective Study. Children 2022, 9, 932. [Google Scholar] [CrossRef] [PubMed]
- Cleveland, C.N.; Kelly, A.; DeGiovanni, J.; Ong, A.A.; Carr, M.M. Maxillofacial trauma in children: Association between age and mandibular fracture site. Am. J. Otolaryngol. 2021, 42, 102874. [Google Scholar] [CrossRef] [PubMed]
- Morisada, M.V.; Tollefson, T.T.; Said, M.; Hwang, J.; Hsieh, T.Y.; Funamura, J.L. Pediatric Mandible Fractures: Mechanism, Pattern of Injury, Fracture Characteristics, and Management by Age. Facial Plast. Surg. Aesthet. Med. 2022, 24, 375–381. [Google Scholar] [CrossRef]
- Khatri, A.; Kalra, N. A conservative approach to pediatric mandibular fracture management: Outcome and advantages. Indian J. Dent. Res. 2011, 22, 873. [Google Scholar] [CrossRef] [PubMed]
- Eppley, B.L. Use of resorbable plates and screws in pediatric facial fractures. J. Oral Maxillofac. Surg. 2005, 63, 385–391. [Google Scholar] [CrossRef]
- Yesantharao, P.S.; Lopez, J.; Reategui, A.; Najjar, O.; Jason, W.Y.; Pourtaheri, N.; Redett, R.J.; Manson, P.N.; Dorafshar, A. Open reduction, internal fixation of isolated mandible angle fractures in growing children. J. Craniofacial Surg. 2020, 31, 1946–1950. [Google Scholar] [CrossRef]
- Fernández, E.C.; Moreira, E.M.; Martínez, A.P. Mandible fracture in children: A case report. South Sudan Med. J. 2020, 13, 116–119. [Google Scholar]
- Kao, R.; Rabbani, C.C.; Patel, J.M.; Parkhurst, S.M.; Mantravadi, A.V.; Ting, J.Y.; Sim, M.W.; Koehler, K.; Shipchandler, T.Z. Management of Mandible Fracture in 150 Children Across 7 Years in a US Tertiary Care Hospital. JAMA Facial Plast. Surg. 2019, 21, 414–418. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: Explanation and elaboration. Ann. Intern. Med. 2009, 151, W-65–W-94. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, R.M.; Yeluri, R.; Singh, C.; Chaudhry, K.; Munshi, A.K. Management of pediatric mandibular fracture: A case series. Compend. Contin. Educ. Dent. 2014, 35, 578–582. [Google Scholar]
- Aizenbud, D.; Emodi, O.; Rachmiel, A. Nonsurgical orthodontic splinting of mandibular fracture in a young child: 10-year follow-up. J. Oral Maxillofac. Surg. 2008, 66, 575–577. [Google Scholar] [CrossRef] [PubMed]
- Boffano, P.; Roccia, F.; Schellino, E.; Baietto, F.; Gallesio, C.; Berrone, S. Conservative Treatment of Unilateral Displaced Condylar Fractures in Children With Mixed Dentition. J. Craniofacial Surg. 2012, 23, E376–E378. [Google Scholar] [CrossRef]
- Cazzolla, A.P.; Montaruli, G.; Testa, N.F.; Favia, G.; Lacaita, M.G.; Lo Muzio, L.; Ciavarella, D. Non-surgical Treatment of Condylar Fracture in an 11-Year-Old Patient: A Case Report. J. Oral. Maxillofac. Res. 2018, 9, e5. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.Y.; Chang, L.R.; Chen, W.H.; Lin, L.W. Reduction of mandible fractures with direct bonding technique and orthodontic appliances: Two case reports. Dent. Traumatol. 2010, 26, 204–209. [Google Scholar] [CrossRef]
- Choubey, S.; Shigli, A.; Banda, N.; Vyawahare, S. Vacuum formed splints: Novel method for managing oro-facial trauma. J. Indian Soc. Pedod. Prev. Dent. 2014, 32, 353–356. [Google Scholar] [CrossRef]
- Kocaaslan, N.D.; Unal, B.K.; Ozkan, M.C.; Karadede, B.; Celebiler, O. Comparison of different treatment techniques in the mandibular condyle fracture. Turk. J. Trauma Emerg. Surg. 2022, 28, 99–106. [Google Scholar] [CrossRef]
- Qadri, G.W.; Mokhtar, S.M. Paediatric mandibular fractures: Report of a case. Dent. Traumatol. 2008, 24, 67–70. [Google Scholar] [CrossRef] [PubMed]
- Sabbagh, H.; Nikolova, T.; Kakoschke, S.C.; Wichelhaus, A.; Kakoschke, T.K. Functional Orthodontic Treatment of Mandibular Condyle Fractures in Children and Adolescent Patients: An MRI Follow-Up. Life 2022, 12, 1596. [Google Scholar] [CrossRef] [PubMed]
- Saskianti, T.; Marwah, A.; Tedjosasongko, U.; Dewi, A.M.; Maulani, B.; Rahmawati, L. Modified Closed Cap Splint for Symphysis/Parasymphysis Mandibular Fracture Management: A Case Report. J. Int. Dent. Med. Res. 2022, 15, 1320–1325. [Google Scholar]
- Tehranchi, A.; Behnia, H.; Younessian, F.; Ghochani, M.S. Rapid, conservative, multidisciplinary miniscrew-assisted approach for treatment of mandibular fractures following plane crash. Dent. Res. J. 2013, 10, 678–684. [Google Scholar]
- Trupthi, D.V.; Chowdhury, S.; Shah, A.; Singh, M. Treatment of Mandibular Fractures Using Intermaxillary Fixation and Vacuum Forming Splints: A Comparative Study. J. Maxillofac. Oral Surg. 2014, 13, 519–524. [Google Scholar] [CrossRef]
- Tuna, E.B.; Dündar, A.; Cankaya, A.B.; Gençay, K. Conservative approach to unilateral condylar fracture in a growing patient: A 2.5-year follow up. Open Dent. J. 2012, 6, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Utley, D.S.; Utley, J.D.; Koch, R.J.; Goode, R.L. Direct bonded orthodontic brackets for maxillomandibular fixation. Laryngoscope 1998, 108, 1338–1345. [Google Scholar] [CrossRef]
- Wu, Y.; Long, X.; Fang, W.; Li, B.; Cheng, Y.; Deng, M.; Cai, H.; Gong, Z. Management of paediatric mandibular condylar fractures with screw-based semi-rigid intermaxillary fixation. Int. J. Oral Maxillofac. Surg. 2012, 41, 55–60. [Google Scholar] [CrossRef]
- Xu, Y.H.; Gong, S.G.; Zhu, F.Y.; Li, M.; Biao, X. Conservative orthodontic fixed appliance management of pediatric mandibular bilateral condylar fracture. Am. J. Orthod. Dentofac. Orthop. 2016, 150, 181–187. [Google Scholar] [CrossRef]
- Zhao, Y.M.; Yang, J.; Bai, R.C.; Ge, L.H.; Zhang, Y. A retrospective study of using removable occlusal splint in the treatment of condylar fracture in children. J. Cranio-Maxillofac. Surg. 2014, 42, 1078–1082. [Google Scholar] [CrossRef]
- Hassanein, A.G. Trends and outcomes of management of mandibular fractures. J. Craniofacial Surg. 2019, 30, 1245–1251. [Google Scholar] [CrossRef] [PubMed]
- Dergin, G.; Emes, Y.; Aybar, B. Evaluation and management of mandibular fracture. In Trauma in Dentistry; IntechOpen: London, UK, 2019. [Google Scholar]
- Sankar, H.; Rai, S.; Jolly, S.S.; Rattan, V. Comparison of Efficacy and Safety of Hybrid Arch Bar with Erich Arch Bar in the Management of Mandibular Fractures: A Randomized Clinical Trial. Craniomaxillofacial Trauma Reconstr. 2022, 19433875221080019. [Google Scholar] [CrossRef]
- Pathak, P.; Thomas, S.; Bhargava, D.; Beena, S. A prospective comparative clinical study on modified screw retained arch bar (SRAB) and conventional Erich’s arch bar (CEAB). Oral Maxillofac. Surg. 2019, 23, 285–289. [Google Scholar] [CrossRef] [PubMed]
- Sharma, A.; Patidar, D.C.; Gandhi, G.; Soodan, K.S.; Patidar, D. Mandibular fracture in children: A new approach for management and review of literature. Int. J. Clin. Pediatr. Dent. 2019, 12, 356. [Google Scholar] [PubMed]
- Chakravarthy, C.; Gupta, N.C.; Patil, R. A simplified digital workflow for the treatment of pediatric mandibular fractures using three-dimensional (3D) printed cap splint: A case report. Craniomaxillofacial Trauma Reconstr. Open 2019, 3, e67–e70. [Google Scholar] [CrossRef]
- Gupta, S.; Verma, R.; Sahu, N. Various approaches for the management of mandibular fracture in pediatric patients: A case series. J. Adv. Clin. Res. Insights 2022, 9, 16–19. [Google Scholar]
- Chocron, Y.; Azzi, A.J.; Davison, P. Management of pediatric mandibular fractures using resorbable plates. J. Craniofacial Surg. 2019, 30, 2111–2114. [Google Scholar] [CrossRef]
- Nilesh, K.; Sawant, A.; Taur, S.; Parkar, M. Management of multiple mandibular fractures in a child with osteogenesis imperfecta using arch bar retained thermoformed splints: A novel technique. J. Clin. Pediatr. Dent. 2016, 40, 322–327. [Google Scholar] [CrossRef]

| Database | Boolean Operators | Results |
|---|---|---|
| PubMed | Mandibular fracture AND (direct bonded brackets OR direct bonding technique OR splint) | 552 |
| Scopus | (“Mandibular fracture” OR “intermaxillary fixation”) AND (“direct bonded brackets” OR “direct bonding technique” OR “splint”) | 497 |
| Web of Science | Mandibular fracture AND (direct bonded brackets OR direct bonding technique OR splint) | 207 |
| Total | 1256 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Polizzi, A.; Ronsivalle, V.; Lo Giudice, A.; Isola, G.; Bianchi, A.; Santonocito, S.; Leonardi, R.; Mummolo, S. Orthodontic Approaches in the Management of Mandibular Fractures: A Scoping Review. Children 2023, 10, 605. https://doi.org/10.3390/children10030605
Polizzi A, Ronsivalle V, Lo Giudice A, Isola G, Bianchi A, Santonocito S, Leonardi R, Mummolo S. Orthodontic Approaches in the Management of Mandibular Fractures: A Scoping Review. Children. 2023; 10(3):605. https://doi.org/10.3390/children10030605
Chicago/Turabian StylePolizzi, Alessandro, Vincenzo Ronsivalle, Antonino Lo Giudice, Gaetano Isola, Alberto Bianchi, Simona Santonocito, Rosalia Leonardi, and Stefano Mummolo. 2023. "Orthodontic Approaches in the Management of Mandibular Fractures: A Scoping Review" Children 10, no. 3: 605. https://doi.org/10.3390/children10030605
APA StylePolizzi, A., Ronsivalle, V., Lo Giudice, A., Isola, G., Bianchi, A., Santonocito, S., Leonardi, R., & Mummolo, S. (2023). Orthodontic Approaches in the Management of Mandibular Fractures: A Scoping Review. Children, 10(3), 605. https://doi.org/10.3390/children10030605










