Assessment of Five-Foot Plantar Morphological Pressure Points of Children with Cerebral Palsy Using or Not Dynamic Ankle Foot Orthosis
Abstract
1. Introduction
2. Methods
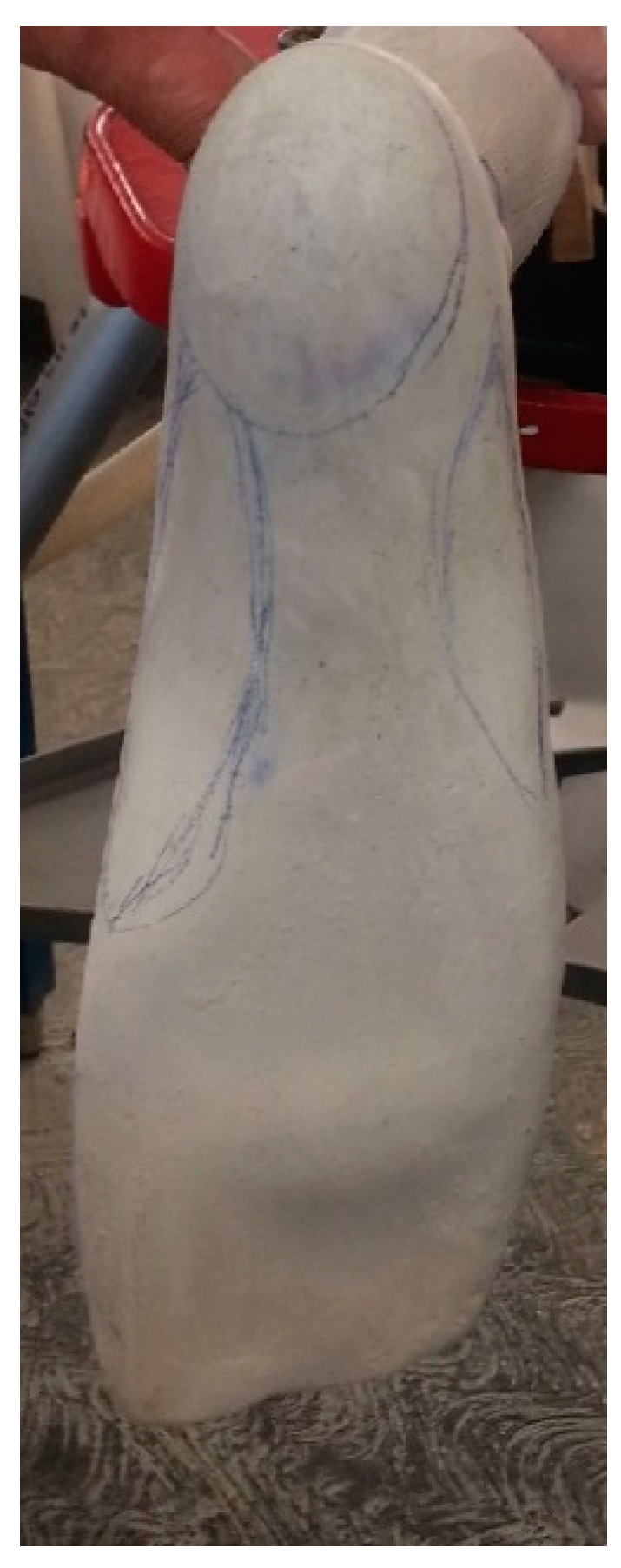
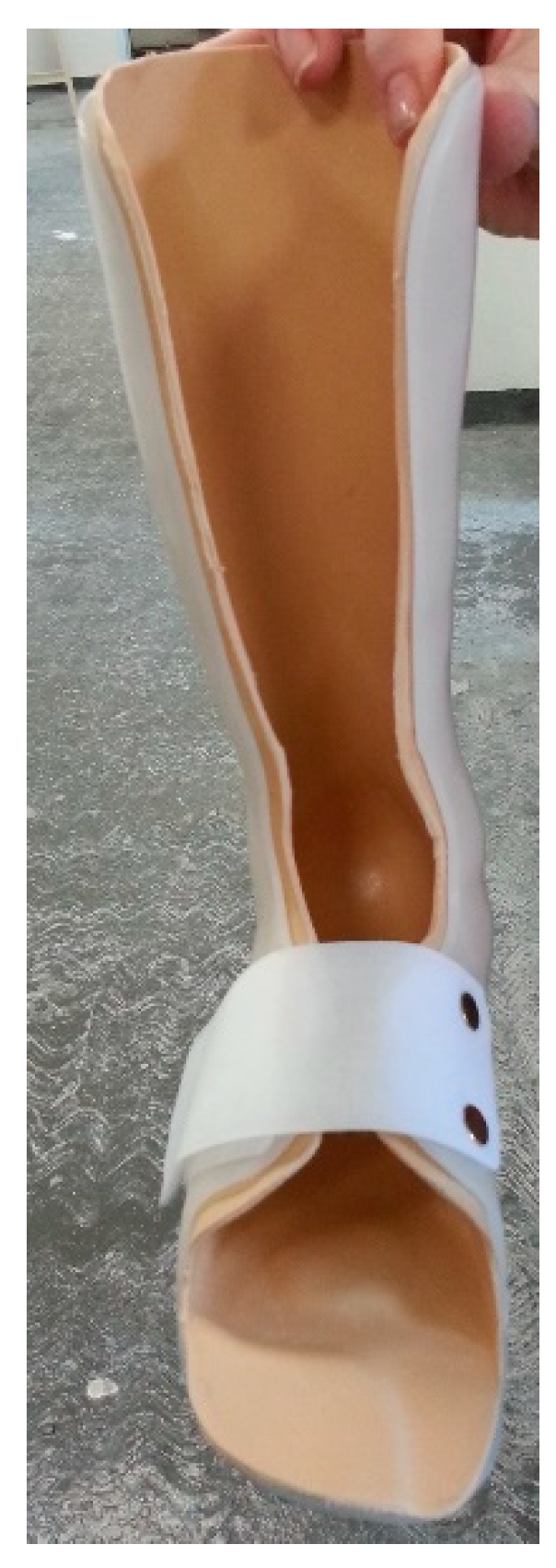
2.1. Orthoses Fabrication and Fitting
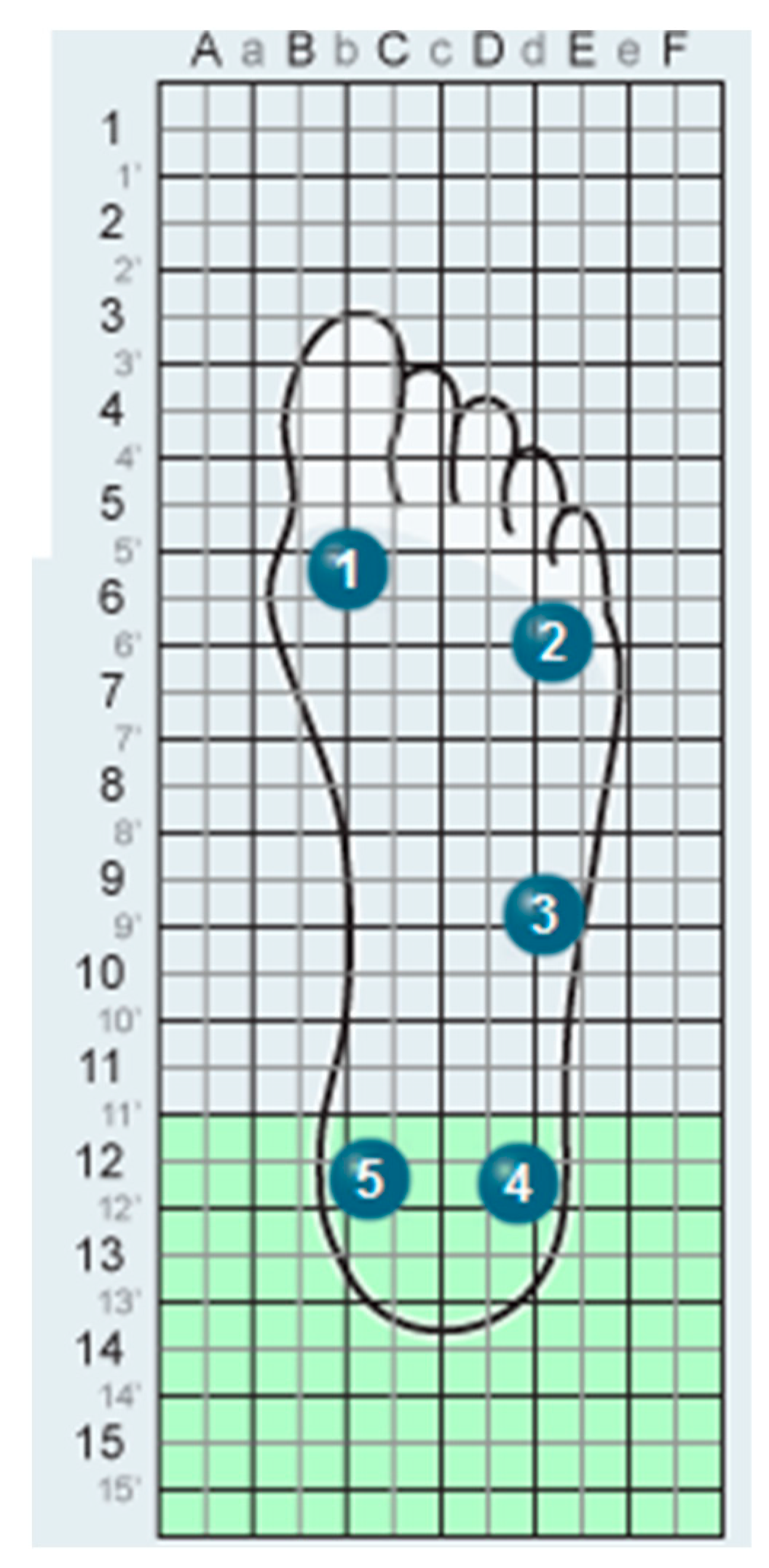
2.2. Plantar Pressure Distribution
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bax, M.; Goldstein, M.; Rosenbaum, P.; Leviton, A.; Paneth, N.; Dan, B.; Jacobsson, B.; Damiano, D. Proposed definition and classification of cerebral palsy. Dev. Med. Child Neurol. 2005, 47, 571–576. [Google Scholar] [PubMed]
- Carmick, J. Forefoot mobility in ankle and foot orthoses: Effect on gait of children with cerebral palsy. Pediatr. Phys. Ther. 2013, 25, 331–337. [Google Scholar] [CrossRef] [PubMed]
- Nahm, N.; Sohrweide, S.; Wervey, R.; Schwartz, M.; Novacheck, T. Surgical treatment of pes planovalgus in ambulatory children with cerebral palsy: Static and dynamic changes as characterized by multi-segment foot modeling, physical examination and radiographs. Gait Posture 2020, 76, 168–174. [Google Scholar] [CrossRef] [PubMed]
- Dieli, J.; Ayyappa, E.; Hornbeak, S. Effect of dynamic AFOs on three hemiplegic adults. J. Prosthet. Orthot. 1997, 9, 82–89. [Google Scholar] [CrossRef]
- Middleton, E.; Hurley, G.; McIlwain, J. The role of rigid and hinged polypropylene ankle-foot-orthoses in the management of cerebral palsy: A case study. Prosthet. Orthot. Int. 1988, 12, 129–135. [Google Scholar] [CrossRef]
- Brehm, M.; Harlaar, J.; Schwartz, M. Effect of ankle-foot orthoses on walking efficiency and gait in children with cerebral palsy. J. Rehabil. Med. 2008, 40, 529–534. [Google Scholar] [CrossRef] [PubMed]
- Hylton, N. Postural and functional impact of dynamic AFOs and FOs in a pediatric population. J. Prosthet. Orthot. 1989, 2, 40–53. [Google Scholar]
- Lima, D. Overview of the causes, treatment, and orthotic management of lower limb spasticity. J. Pediatr. Orthop. 1990, 2, 33–40. [Google Scholar]
- Eddison, N.; Chockalingam, N. The effect of tuning ankle foot orthoses-footwear combination on the gait parameters of children with cerebral palsy. Prosthet. Orthot. Int. 2012, 37, 95–107. [Google Scholar] [CrossRef]
- Singerman, R.; Hoy, D.; Mansour, J. Design changes in ankle foot orthoses intended to alter stiffness also alters orthosis kinematics. J. Prosthet. Orthot. 1999, 11, 48–56. [Google Scholar]
- Novacheck, T.; Beattie, C.; Rozumalski, A.; Gent, G.; Kroll, G. Quantifying the spring-like properties of ankle-foot orthoses (AFOs). J. Prosthet. Orthot. 2007, 19, 98–103. [Google Scholar] [CrossRef]
- Polliack, A.; Swanson, C.; Landsberger, S.; McNeal, D. Development of a testing apparatus for structural stiffness evaluation of ankle-foot orthoses. J. Prosthet. Orthot. 2001, 13, 74–82. [Google Scholar]
- El-Kafy, E. The clinical impact of orthotic correction of lower limb rotational deformities in children with cerebral palsy: A randomized controlled trial. Clin. Rehabil. 2014, 28, 1004–1014. [Google Scholar] [CrossRef]
- Ries, A.; Schwartz, M. Ground reaction and solid ankle-foot orthoses are equivalent for the correction of crouch gait in children with cerebral palsy. Dev. Med. Child Neurol. 2018, 61, 219–225. [Google Scholar] [CrossRef]
- Chui, K.; Jorge, M.; Yen, S.; Lusardi, M. Orthotics and Prosthetics in Rehabilitation, 4th ed.; Saunders Elsevier: St. Louis, MO, USA, 2020. [Google Scholar]
- Mueller, K.; Cornwall, M.; McPoil, T.; Mueller, D.; Barnwell, J. Effect of a tone-inhibiting dynamic ankle-foot orthosis on the foot-loading pattern of a hemiplegic adult: A preliminary study. J. Prosthet. Orthot. 1992, 4, 86–92. [Google Scholar] [CrossRef]
- Lam, W.; Leong, J.; Li, Y.; Hu, Y.; Lu, W. Biomechanical and electromyographic evaluation of ankle foot orthosis and dynamic ankle foot orthosis in spastic cerebral palsy. Gait Posture 2005, 22, 189–197. [Google Scholar] [CrossRef]
- Radtka, S.; Skinner, S.; Dixon, D.; Johanson, M. A comparison of gait with solid, dynamic, and no ankle-foot orthoses in children with spastic cerebral palsy. Phys. Ther. 1997, 77, 395–409. [Google Scholar] [CrossRef] [PubMed]
- Bjornson, K.; Schmale, G.; Adamczyk-Foster, A.; McLaughlin, J. The effect of Dynamic Ankle Foot Orthoses on function in children with cerebral palsy. J Pediatr Orthop. 2006, 26, 773–776. [Google Scholar] [CrossRef] [PubMed]
- Stuberg, W. The aims of lower limb orthotic management of cerebral palsy: A critical review of the literature. In Report of a Consensus Conference on the Lower Limb Orthotic Management of Cerebral Palsy; Meadows, C.B., Condie, D.N., Eds.; International Society of Prosthetics and Orthotics: Copenhagen, Denmark, 1994; pp. 27–34. [Google Scholar]
- Morris, C. Orthotic management of children with cerebral palsy. J. Prosthet. Orthot. 2002, 14, 150–158. [Google Scholar] [CrossRef]
- Jagadamma, K.C.; Coutts, F.J.; Mercer, T.H.; Herman, J.; Yirrell, J.; Forbes, L.; van der Linden, M.L. Optimising the effects of rigid ankle foot orthoses on the gait of children with cerebral palsy (CP)-an exploratory trial. Disabil. Rehabil. Assist. Technol. 2015, 10, 445–451. [Google Scholar] [CrossRef] [PubMed]
- Uckun, A.C.; Celik, C.; Ucan, H.; Gokkaya, N.K.O. Comparison of effects of lower extremity orthoses on energy expenditure in patients with cerebral palsy. Dev. Neurorehabil. 2014, 17, 388–392. [Google Scholar]
- Vanwala, J.; Diwan, S.; Shah, S.; Vyas, N. Effect of ankle foot orthosis on energy expenditure index and gait speed in spastic cerebral palsy children: An observational study. Int. J. Contemp. Pediatr. 2014, 1, 17. [Google Scholar] [CrossRef]
- Hayek, S.; Hemo, Y.; Chamis, S.; Bat, R.; Segev, E.; Wientroub, S.; Yzhar, Z. The effect of community-prescribed ankle-foot orthoses on gait parameters in children with spastic cerebral palsy. J. Child. Orthop. 2007, 1, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Lucareli, P.; Lima, M.; Lucarelli, J.; Lima, F. Changes in joint kinematics in children with cerebral palsy while walking with and without a floor reaction ankle-foot orthosis. Clinics 2007, 62, 63–68. [Google Scholar] [CrossRef] [PubMed]
- Balaban, B.; Yasar, E.; Dal, U.; Yazicioglu, K.; Mohur, H.; Kalyon, T. The effect of hinged ankle-foot orthosis on gait and energy expenditure in spastic hemiplegic cerebral palsy. Disabil. Rehabil. 2007, 29, 139–144. [Google Scholar] [CrossRef]
- Zhao, X.; Xiao, N.; Li, H.; Du, S. Day vs. day-night use of ankle-foot orthoses in young children with spastic diplegia: A randomized controlled study. Am. J. Phys. Med. Rehabil. 2013, 92, 905–911. [Google Scholar] [CrossRef] [PubMed]
- Lintanf, M.; Bourseul, J.; Houx, L.; Lempereur, M.; Brochard, S.; Pons, C. Effect of ankle-foot orthoses on gait, balance and gross motor function in children with cerebral palsy: A systematic review and meta-analysis. Clin. Rehabil. 2018, 32, 1175–1188. [Google Scholar]
- Aboutorabi, A.; Arazpour, M.; Bani, M.A.; Saeedi, H.; Head, J.S. Efficacy of ankle foot orthoses types on walking in children with cerebral palsy: A systematic review. Ann. Phys. Rehabil. Med. 2017, 60, 393–402. [Google Scholar] [CrossRef]
- Wren, T.A.L.; Dryden, J.W.; Mueske, N.M.; Dennis, S.W.; Healy, B.S.; Rethlefsen, S.A. Comparison of 2 Orthotic Approaches in Children with Cerebral Palsy. Pediatr. Phys. Ther. 2015, 27, 218–226. [Google Scholar] [CrossRef]
- Leunkeu, A.; Lelard, T.; Shephard, R.; Doutrellot, P.; Ahmaidi, S. Gait cycle and plantar pressure distribution in children with cerebral palsy: Clinically useful outcome measures for management and rehabilitation. NeuroRehabilitation 2014, 35, 657–663. [Google Scholar] [CrossRef] [PubMed]
- Galli, M.; Cimolin, V.; Pau, M.; Leban, B.; Brunner, R.; Albertini, G. Foot pressure distribution in children with cerebral palsy while standing. Res. Dev. Disabil. 2015, 41, 52–57. [Google Scholar] [CrossRef] [PubMed]
- Palisano, R.; Rosenbaum, P.; Walter, S.; Russell, D.; Wood, E.; Galuppi, B. Development and reliability of a system to classify grossmotor function in children with cerebral palsy. Dev. Med. ChildNeurol. 1997, 39, 214–223. [Google Scholar]
- Wren, T.; Rethlefsen, S.; Kay, R. Prevalence of specific gait abnormalities in children with cerebral palsy: Influence of cerebral palsy subtype, age, and previous surgery. J. Pediatr. Orthop. 2005, 25, 79–83. [Google Scholar] [PubMed]
- Healy, A.; Burgess-Walker, P.; Naemi, R.; Chockalingam, N. Repeatability of WalkinSense® in shoe pressure measurement system: A preliminary study. Foot 2012, 22, 35–39. [Google Scholar] [CrossRef]
- Patar, A.; Jamlus, N.; Makhtar, K.; Mahmud, J.; Komeda, T. Development of Dynamic Ankle Foot Orthosis for Therapeutic Application. Procedia Eng. 2012, 41, 1432–1440. [Google Scholar] [CrossRef][Green Version]
- Abel, M.; Juhl, G.; Vaughan, C.; Damiano, D. Gait assessment of fixed ankle foot orthoses in children with spastic diplegia. Arch. Phys. Med. Rehabil. 1998, 79, 126–133. [Google Scholar] [CrossRef] [PubMed]
- Carlson, W.; Vaughan, C.; Damiano, D.; Abel, M. Orthotic management of gait in spastic diplegia. Am. J. Phys. Med. Rehabil. 1997, 76, 219–225. [Google Scholar]
- Buckon, C.; Thomas, S.; Jakobson-Huston, S.; Sussman, M.; Aiona, M. Comparison of three ankle-foot orthosis configurations for children with spastic hemiplegia. Dev. Med. Child. Neurol. 2001, 43, 371–378. [Google Scholar] [PubMed]
- Romkes, J.; Brunner, R. Comparison of a dynamic and a hinged ankle foot orthosis by gait analysis in patients with hemiplegic cerebral palsy. Gait Posture 2002, 15, 18–24. [Google Scholar] [CrossRef]
- Schwarze, M.; Horoba, L.; Block, J.D.I.; Putz, C.; Alimusaj, M.D.I.; Salami, F.; Wolf, S.I.D.; Dreher, T. Additional Effects of Shank Adaptations in Children with Bilateral Spastic Cerebral Palsy. J. Prosthet. Orthot. 2021, 33, 125–132. [Google Scholar] [CrossRef]
- Everaert, L.; Papageorgiou, E.; Van Campenhout, A.; Labey, L.; Desloovere, K. The influence of ankle-foot orthoses on gait pathology in children with cerebral palsy: A retrospective study. Gait Posture 2023, 100, 149–156. [Google Scholar] [PubMed]
- Theologis, T. Lever arm dysfunction in cerebral palsy gait. J. Child. Orthop. 2013, 7, 379–382. [Google Scholar] [CrossRef] [PubMed]
- Yoon, H.; Park, K.; Roh, J.; Park, H.; Chi, H.; Kim, H. Extraarticular subtalar arthrodesis for pes planovalgus: An interim result of 50 feet in patients with spastic diplegia. Clin. Orthop. Surg. 2010, 2, 13–21. [Google Scholar] [CrossRef] [PubMed]
- Femery, V.; Moretto, P.; Renaut, H.; Lensel, G.; Thevenon, A. Asymmetries in dynamic plantar pressure distribution measurement in able-bodied gait: Application to the study of the gait asymmetries in children with hemiplegic cerebral palsy. Ann. Readapt. Med. Phys. 2002, 45, 114–122. [Google Scholar] [PubMed]
- Zhang, C.; Pan, S.; Qi, Y.; Yang, Y. A Footprint Extraction and Recognition Algorithm Based on Plantar Pressure. Traitement Du Signal 2019, 36, 419–424. [Google Scholar] [CrossRef]
- Pauk, J.; Ihnatouski, M.; Daunoraviciene, K.; Laskhousky, U.; Griskevicius, J. Research of the spatial-temporal gait parameters and pressure characteristic in spastic diplegia children. Acta Bioeng. Biomech. 2016, 18, 121–129. [Google Scholar] [PubMed]


| Case | Age | Sex | Diagnosis | Type of Orthosis | Total Ankle ROM (Extended Knee) | Total Ankle ROM (Flexed Knee) | İnitial Contact (without Orthosis) | İnitial Contact (with the Orthosis) | Max Knee Extension in the Stance Phase |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 12 | M | Spastic Diplegia | DAFO3 | 30° | 38° | İnitial ground contact made with forefoot | İnitial ground contact made with both the forefoot and hindfoot | Hyperextension |
| 2 | 5 | F | Spastic Diplegia | DAFO4 | 48° | 55° | İnitial ground contact made with both the forefoot and hindfoot | İnitial ground contact made with both the forefoot and hindfoot | Not Hyperextension |
| 3 | 12 | M | Spastic Diplegia | DAFO3 | 35° | 42° | İnitial ground contact made with forefoot | İnitial ground contact made with both the forefoot and hindfoot | Hyperextension |
| 4 | 4 | M | Spastic Diplegia | DAFO3 | 40° | 47° | İnitial ground contact made with both the forefoot and hindfoot | İnitial ground contact made with both the forefoot and hindfoot | Hyperextension |
| 5 | 10 | F | Spastic Diplegia | DAFO3 | 34° | 40° | İnitial ground contact made with forefoot | İnitial ground contact made with both the forefoot and hindfoot | Hyperextension |
| 6 | 9 | M | Spastic Diplegia | DAFO4 | 47° | 55° | İnitial ground contact made with both the forefoot and hindfoot | İnitial ground contact made with both the forefoot and hindfoot | Not Hyperextension |
| 7 | 9 | M | Spastic Diplegia | DAFO3 | 37° | 45° | İnitial ground contact made with forefoot | İnitial ground contact made with both the forefoot and hindfoot | Hyperextension |
| 8 | 11 | F | Spastic Diplegia | DAFO3 | 32° | 38° | İnitial ground contact made with forefoot | İnitial ground contact made with both the forefoot and hindfoot | Hyperextension |
| Stance Phase Plantar Pressure Distributions | Only Shoes | DAFO with Shoes | p |
|---|---|---|---|
| Maximum pressure kg/cm2 | 1.99 | 1.71 | 0.123 |
| Maximum pressure sensor | 2 | 3 | 0.037 * |
| 1 sensor activation % | 92 | 24.5 | 0.028 * |
| 2 sensor activation % | 89.2 | 56 | 0.161 |
| 3 sensor activation % | 81 | 88 | 0.161 |
| 4 sensor activation % | 58 | 90 | 0.036 * |
| 5 sensor activation % | 60 | 80 | 0.161 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Guner, S.; Alsancak, S.; Güven, E.; Özgün, A.K. Assessment of Five-Foot Plantar Morphological Pressure Points of Children with Cerebral Palsy Using or Not Dynamic Ankle Foot Orthosis. Children 2023, 10, 722. https://doi.org/10.3390/children10040722
Guner S, Alsancak S, Güven E, Özgün AK. Assessment of Five-Foot Plantar Morphological Pressure Points of Children with Cerebral Palsy Using or Not Dynamic Ankle Foot Orthosis. Children. 2023; 10(4):722. https://doi.org/10.3390/children10040722
Chicago/Turabian StyleGuner, Senem, Serap Alsancak, Enver Güven, and Ali Koray Özgün. 2023. "Assessment of Five-Foot Plantar Morphological Pressure Points of Children with Cerebral Palsy Using or Not Dynamic Ankle Foot Orthosis" Children 10, no. 4: 722. https://doi.org/10.3390/children10040722
APA StyleGuner, S., Alsancak, S., Güven, E., & Özgün, A. K. (2023). Assessment of Five-Foot Plantar Morphological Pressure Points of Children with Cerebral Palsy Using or Not Dynamic Ankle Foot Orthosis. Children, 10(4), 722. https://doi.org/10.3390/children10040722





