Lateral Humeral Condyle Fractures in Pediatric Patients
Abstract
1. Introduction
2. Epidemiology
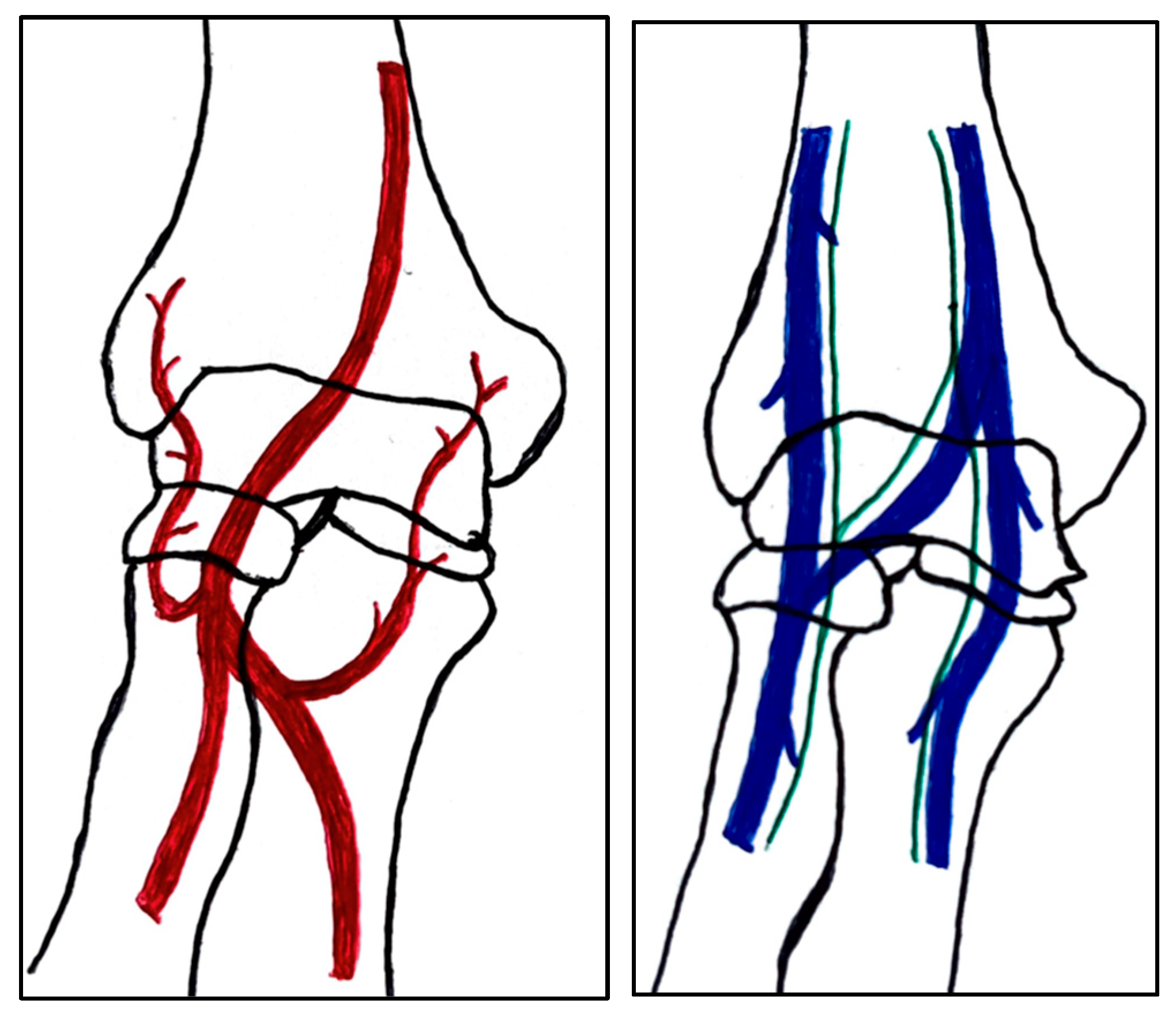
2.1. Anatomy
2.2. Trauma Mechanism and Associated Injuries
2.3. Classification of Fractures
| Classification | Type 1 (A) | Type 2 (B) | Type 3 (C) | Type 4 | Type 5 |
|---|---|---|---|---|---|
| Milch. [16] | 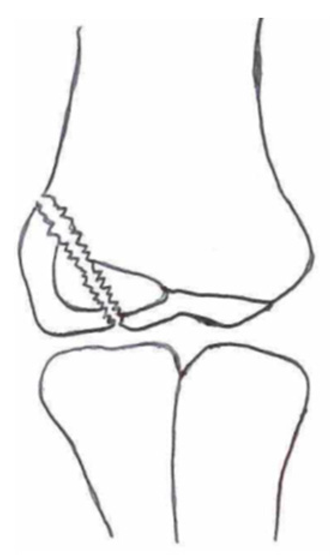 |  | |||
| Jacobs et al. [21] |  |  |  | ||
| Finnbogason et al. [22] |  |  |  | ||
| Weiss et al. [23] |  |  |  | ||
| Song et al. [4] |  |  |  |  |  |
2.4. Diagnosis
2.4.1. Medical History and Physical Examination
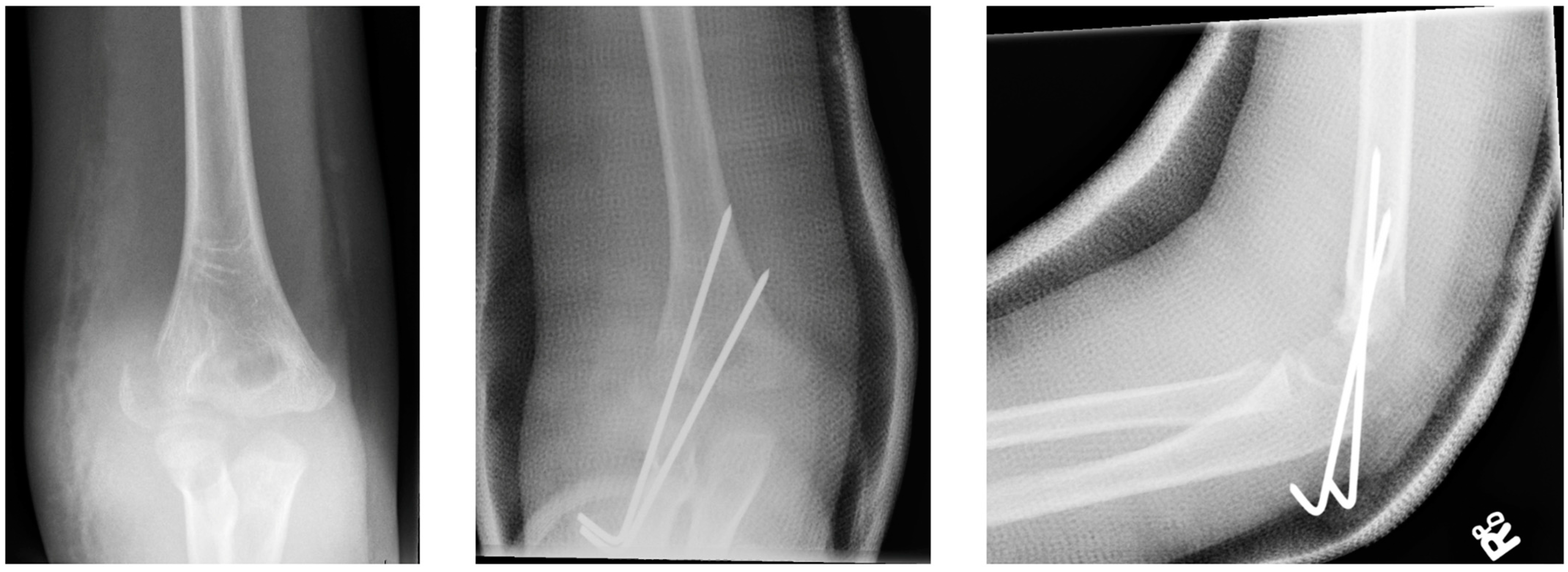
2.4.2. Diagnostic Imaging
3. Treatment Options
3.1. Non-Surgical/Operative Treatment Options: Plastered Cast Therapy
3.2. Surgical/Operative Treatment Options
3.2.1. Closed Reduction and Internal Fixation
3.2.2. Open Reduction and Internal Fixation
4. Complications
4.1. Lateral Overgrowth
4.2. Infections
4.3. Malunion and Non-Union
4.4. Avascular Necrosis
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Hedström, E.M.; Svensson, O.; Bergström, U.; Michno, P. Epidemiology of fractures in children and adolescents: Increased incidence over the past decade: A population-based study from northern Sweden. Acta Orthop. 2010, 81, 148–153. [Google Scholar] [CrossRef] [PubMed]
- Naranje, S.M.; Erali, R.A.; Warner, W.C.; Sawyer, J.R.; Kelly, D.M. Epidemiology of Pediatric Fractures Presenting to Emergency Departments in the United States. J. Pediatr. Orthop. 2016, 36, e45–e48. [Google Scholar] [CrossRef] [PubMed]
- Hussain, S.; Dar, T.; Beigh, A.Q.; Dhar, S.; Ahad, H.; Hussain, I.; Ahmad, S. Pattern and epidemiology of pediatric musculoskeletal injuries in Kashmir valley, a retrospective single-center study of 1467 patients. J. Pediatr. Orthop. Part B 2015, 24, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Hwan Koh, K.; Wook Seo, S.; Mu Kim, K.; Sup Shim, J. Clinical and Radiographic Results of Lateral Condylar Fracture of Distal Humerus in Children. J. Pediatr. Orthop. 2010, 30, 425–429. [Google Scholar]
- Landin, L.A.; Danielsson, L.G. Elbow fractures in children. Acta Orthop. Sand. 1986, 57, 309–312. [Google Scholar] [CrossRef]
- Houshian, S.; Mehdi, B.; Larsen, M.S. The epidemiology of elbow fracture in children: Analysis of 355 fractures, with special reference to supracondylar humerus fractures. J. Orthop. Sci. 2001, 6, 312–315. [Google Scholar] [CrossRef]
- Emery, K.H.; Zingula, S.N.; Anton, C.G.; Salisbury, S.R.; Tamai, J. Pediatric elbow fractures: A new angle on an old topic. Pediatr. Radiol. 2016, 46, 61–66. [Google Scholar] [CrossRef]
- Tan, S.H.S.; Dartnell, J.; Lim, A.K.S.; Hui, J.H. Paediatric lateral condyle fractures: A systematic review. Arch. Orthop. Trauma Surg. 2018, 138, 809–817. [Google Scholar] [CrossRef]
- James, V.; Chin, A.; Chng, C.; Lim, F.; Ting, M.; Chan, Y.H.; Ganapathy, S. Lateral Condyle Fracture of the Humerus Among Children Attending a Pediatric Emergency Department; A 10-Year Single-Center Experience. Pediatr. Emerg. Care 2021, 37, e1339–e1344. [Google Scholar] [CrossRef]
- Kwang, S.; Song, H.; Kang, B.; Woo, M.; Chul Bae, K.; Cho, C.H. Internal Oblique Radiographs for Diagnosis of Nondisplaced or Minimally Displaced Lateral Condylar Fractures of the Humérus in Children. J. Bone Jt. Surg. 2007, 89, 58–63. [Google Scholar]
- Hill, C.E.; Cooke, S. Common Paediatric Elbow Injuries. Open Orthop. J. 2017, 11, 1380–1393. [Google Scholar] [CrossRef] [PubMed]
- Shaerf, D.A.; Vanhegan, I.S.; Dattani, R. Diagnosis, management and complications of distal humerus lateral condyle fractures in children. Shoulder Elb. 2018, 10, 114–120. [Google Scholar] [CrossRef] [PubMed]
- Okubo, H.; Nakasone, M.; Kinjo, M.; Onaka, K.; Futenma, C.; Kanaya, F. Epidemiology of paediatric elbow fractures: A retrospective multi-centre study of 488 fractures. J. Child Orthop. 2019, 13, 516–521. [Google Scholar] [CrossRef] [PubMed]
- Rennie, L.; Court-Brown, C.M.; Mok, J.Y.Q.; Beattie, T.F. The epidemiology of fractures in children. Injury 2007, 38, 913–922. [Google Scholar] [CrossRef]
- Sananta, P.; Sintong, L.; Prasetio, B.; Putera, M.A.; Andarini, S.; Kalsum, U.; Dradjat, R.S. Elbow fracture in children at saiful anwar general hospital, nine years experiences. Open Access Maced. J. Med. Sci. 2019, 7, 4069–4071. [Google Scholar] [CrossRef]
- Milch, H. Fractures and fracture dislocations of the humeral condyles. J. Trauma 1964, 4, 592–607. [Google Scholar] [CrossRef] [PubMed]
- Abzug, J.M.; Dua, K.; Kozin, S.H.; Herman, M.J. Current Concepts in the Treatment of Lateral Condyle Fractures in Children. J. Am. Acad. Orthop. Surg. 2020, 28, E9–E19. [Google Scholar] [CrossRef]
- Herdea, A.; Ulici, A.; Toma, A.; Voicu, B.; Charkaoui, A. The relationship between the dominant hand and the occurrence of the supracondylar humerus fracture in pediatric orthopedics. Children 2021, 8, 51. [Google Scholar] [CrossRef]
- Bryce, C.D.; Armstrong, A.D. Anatomy and Biomechanics of the Elbow. Orthop. Clin. N. Am. 2008, 39, 141–154. [Google Scholar] [CrossRef]
- Paulsen, F.; Waschke, J. (Eds.) Sobotta Atlas of Human Anatomy, 15th ed.; Elsevier: Amsterdam, The Netherlands, 2011. [Google Scholar]
- Jakob, R.; Fowles, J.V.; Rang, M.; Kassab, M.T. Observations concerning fractures of the lateral humeral condyle in children. J. Bone Jt. Surg. Br. 1975, 57, 430–436. [Google Scholar] [CrossRef]
- Finnbogason, T.; Karlsson, G.; Lindberg, L.; Mortensson, W. Nondisplaced and minimally displaced fractures of the lateral humeral condyle in children: A prospective radiographic investigation of fracture stability. J. Pediatr. Orthop. 1995, 15, 422–425. [Google Scholar] [CrossRef] [PubMed]
- Weiss, J.M.; Graves, S.; Yang, S.; Mendelsohn, E.; Kay, R.M.; Skaggs, D.L. A new classification system predictive of complications in surgically treated pediatric humeral lateral condyle fractures. J. Pediatr. Orthop. 2009, 29, 602–605. [Google Scholar] [CrossRef] [PubMed]
- Mirsky, E.C.; Karas, E.H.; Weiner, L.S. Lateral condyle fractures in children: Evaluation of classification and treatment. J. Orthop. Trauma 1997, 11, 117–120. [Google Scholar] [CrossRef]
- Pennington, R.G.C.; Corner, J.A.; Brownlow, H.C. Milch’s classification of paediatric lateral condylar mass fractures: Analysis of inter- and intraobserver reliability and comparison with operative findings. Injury 2009, 40, 249–252. [Google Scholar] [CrossRef]
- Ramo, B.A.; Funk, S.S.; Elliott, M.E.; Jo, C.H. The Song Classification Is Reliable and Guides Prognosis and Treatment for Pediatric Lateral Condyle Fractures: An Independent Validation Study with Treatment Algorithm. J. Pediatric Orthop. 2020, 40, E203–E209. [Google Scholar] [CrossRef] [PubMed]
- Appelboam, A.; Reuben, A.D.; Benger, J.R.; Beech, F.; Dutson, J.; Haig, S.; Higginson, I.; Klein, J.A.; Le Roux, S.; Saranga, S.S.; et al. Elbow extension test to rule out elbow fracture: Multicentre, prospective validation and observational study of diagnostic accuracy in adults and children. BMJ 2009, 338, 31–33. [Google Scholar] [CrossRef] [PubMed]
- Knutsen, A.; Avoian, T.; Borkowski, S.L.; Ebramzadeh, E.; Zionts, L.E.; Sangiorgio, S.N. Accuracy of radiographs in assessment of displacement in lateral humeral condyle fractures. J. Child Orthop. 2014, 8, 83–89. [Google Scholar] [CrossRef]
- Soon Song, K.; Woon Shin, Y.; Wug, C.O.; Choer Bae, K.; Hyun Cho, C. Closed Reduction and Internal Fixation of Completely Displaced and Rotated Lateral Condyle Fractures of the Humerus in Children. J. Orthop. Trauma 2010, 24, 434–438. [Google Scholar] [CrossRef]
- Poppelaars, M.A.; Eygendaal, D.; The, B.; van Oost, I.; van Bergen, C.J.A. Diagnosis and Treatment of Children with a Radiological Fat Pad Sign without Visible Elbow Fracture Vary Widely: An International Online Survey and Development of an Objective Definition. Children 2022, 9, 950. [Google Scholar] [CrossRef]
- Kappelhof, B.; Roorda, B.L.; Poppelaars, M.A.; The, B.; Eygendaal, D.; Mulder, P.G.H.; Van Bergen, C.J. Occult Fractures in Children with a Radiographic Fat Pad Sign of the Elbow: A Meta-Analysis of 10 Published Studies. JBJS Rev. 2022, 10, e22. [Google Scholar] [CrossRef]
- Chapman, V.M.; Grottkau, B.E.; Albright, M.; Salamipour, H.; Jaramillo, D. Multidetector computed tomography of pediatric lateral condylar fractures. J. Comput. Assist. Tomogr. 2005, 29, 842–846. [Google Scholar] [CrossRef] [PubMed]
- Knapik, D.M.; Gilmore, A.; Liu, R.W. Conservative Management of Minimally Displaced (≤2 mm) Fractures of the Lateral Humeral Condyle in Pediatric Patients: A Systematic Review. J. Pediatr. Orthop. 2017, 37, e83–e87. [Google Scholar] [CrossRef] [PubMed]
- Marcheix, P.S.; Vacquerie, V.; Longis, B.; Peyrou, P.; Fourcade, L.; Moulies, D. Distal humerus lateral condyle fracture in children: When is the conservative treatment a valid option? Orthop. Traumatol. Surg. Res. 2011, 97, 304–307. [Google Scholar] [CrossRef]
- Zhang, S.; Tan, S.H.S.; Lim, A.K.S.; Hui, J.H.P. Surgical outcomes in paediatric lateral condyle non-union: A systematic review and meta-analysis. Orthop. Traumatol. Surg. Res. 2022, 108, 102933. [Google Scholar] [CrossRef]
- Eckhoff, M.D.; Tadlock, J.C.; Nicholson, T.C.; Wells, M.E.; Garcia, E.s.J.; Hennessey, T.A. Open reduction of pediatric lateral condyle fractures: A systematic review. Shoulder Elb. 2022, 14, 317–325. [Google Scholar] [CrossRef] [PubMed]
- Trisolino, G.; Antonioli, D.; Gallone, G.; Stallone, S.; Zarantonello, P.; Tanzi, P.; Olivotto, E.; Stilli, L.; Di Gennaro, G.L.; Stilli, S. Neglected fractures of the lateral humeral condyle in children; which treatment for which condition? Children 2021, 8, 56. [Google Scholar] [CrossRef]
- Prakash, J.; Mehtani, A. Open reduction versus in-situ fixation of neglected lateral condyle fractures: A comparative study. J. Pediatr. Orthop. Part B 2018, 27, 134–141. [Google Scholar] [CrossRef]
- Pace, J.L.; Arkader, A.; Sousa, T.; Broom, A.M.; Shabtai, L. Incidence, Risk Factors, and Definition for Nonunion in Pediatric Lateral Condyle Fractures. J. Pediatr. Orthop. 2018, 38, e257–e261. [Google Scholar] [CrossRef]
- Shabtai, L.; Lightdale-Miric, N.; Rounds, A.; Arkader, A.; Pace, J.L. Incidence, risk factors and outcomes of avascular necrosis occurring after humeral lateral condyle fractures. J. Pediatr. Orthop. Part B 2020, 29, 145–148. [Google Scholar] [CrossRef]
- Pirker, M.E.; Weinberg, A.M.; Höllwarth, M.E.; Haberlik, A. Subsequent displacement of initially nondisplaced and minimally displaced fractures of the lateral humeral condyle in children. J. Trauma Inj. Infect. Crit. Care 2005, 58, 1202–1207. [Google Scholar] [CrossRef]
- Gaston, M.S.; Irwin, G.J.; Huntley, J.S. Lateral condyle fracture of a child’s humerus: The radiographic features may be subtle. Scott Med. J. 2012, 57, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Wendling-Keim, D.S.; Teschemacher, S.; Dietz, H.G.; Lehner, M. Lateral Condyle Fracture of the Humerus in Children: Kirschner Wire or Screw Fixation? Eur. J. Pediatr. Surg. 2021, 31, 374–379. [Google Scholar] [CrossRef] [PubMed]
- Li, X.; Shen, X.; Wu, X.; Wang, S. Ultrasound-assisted closed reduction and percutaneous pinning for displaced and rotated lateral condylar humeral fractures in children. J. Shoulder Elbow Surg. 2021, 30, 2113–2119. [Google Scholar] [CrossRef] [PubMed]
- Beerekamp, M.S.H.; Sulkers, G.S.I.; Ubbink, D.T.; Maas, M.; Schep, N.W.L.; Goslings, J.C. Accuracy and consequences of 3D-fluoroscopy in upper and lower extremity fracture treatment: A systematic review. Eur. J. Radiol. 2012, 81, 4019–4028. [Google Scholar] [CrossRef]
- Colton, C.; Monsell, F.; Slongo, T. AO General K-Wires Principles. 2023. Available online: https://surgeryreference.aofoundation.org/orthopedic-trauma/pediatric-trauma/basic-technique/general-k-wire-principles (accessed on 23 May 2023).
- Hasler, C.C.; von Laer, L. Prevention of growth disturbances after fractures of the lateral humeral condyle in children. J. Pediatr. Orthop. B 2001, 10, 123–130. [Google Scholar]
- Pribaz, J.R.; Bernthal, N.M.; Wong, T.C.; Silva, M. Lateral spurring (overgrowth) after pediatric lateral condyle fractures. J. Pediatr. Orthop. 2012, 32, 456–460. [Google Scholar] [CrossRef]
- Ganeshalingam, R.; Donnan, A.; Evans, O.; Hoq, M.; Camp, M.; Donnan, L. Lateral condylar fractures of the humerus in children: Does the type of fixation matter? Bone Jt. J. 2018, 100-B, 387–395. [Google Scholar] [CrossRef]
- Leonidou, A.; Chettiar, K.; Graham, S.; Akhbari, P.; Antonis, K.; Tsiridis, E.; Leonidou, O. Open reduction internal fixation of lateral humeral condyle fractures in children. A series of 105 fractures from a single institution. Strateg. Trauma Limb Reconstr. 2014, 9, 73–78. [Google Scholar] [CrossRef]
- Pennock, A.T.; Salgueiro, L.; Upasani, V.V.; Bastrom, T.P.; Newton, P.O.; Yaszay, B. Closed Reduction and Percutaneous Pinning Versus Open Reduction and Internal Fixation for Type II Lateral Condyle Humerus Fractures in Children Displaced >2 mm. J. Pediatr. Orthop. 2016, 36, 780–786. [Google Scholar] [CrossRef]
- Thomas, J.D.; Kehoe, J.L. Bone Nonunion; StatPearls: Tampa, FL, USA, 2023. [Google Scholar]
- Launay, F.; Leet, A.I.; Jacopin, S.; Jouve, J.-L.; Bollini, G.; Sponseller, P.D. Lateral humeral condyle fractures in children: A comparison of two approaches to treatment. J. Pediatr. Orthop. 2004, 24, 385–391. [Google Scholar] [CrossRef]
- Toh, S.; Tsubo, K.; Nishikawa, S.; Inoue, S.; Nakamura, R.; Narita, S. Osteosynthesis for Nonunion of the Lateral Humeral Condyle. Clin. Orthop. Relat. Res. 2002, 405, 230–241. [Google Scholar] [CrossRef]
- Eamsobhana, P.; Kaewpornsawan, K. Should we repair nonunion of the lateral humeral condyle in children? Int. Orthop. 2015, 39, 1579–1585. [Google Scholar] [CrossRef]
- Park, H.; Hwang, J.H.; Kwon, Y.U.; Kim, H.W. Osteosynthesis In Situ for Lateral Condyle Nonunion in Children. J. Pediatr. Orthop. 2015, 35, 334–340. [Google Scholar] [CrossRef]
- Salgueiro, L.; Roocroft, J.H.; Bastrom, T.P.; Edmonds, E.W.; Pennock, A.T.; Upasani, V.V.; Yaszay, B. Rate and Risk Factors for Delayed Healing Following Surgical Treatment of Lateral Condyle Humerus Fractures in Children. J. Pediatr. Orthop. 2017, 37, 1–6. [Google Scholar] [CrossRef]
- Silva, M.; Cooper, S.D. Closed Reduction and Percutaneous Pinning of Displaced Pediatric Lateral Condyle Fractures of the Humerus. J. Pediatr. Orthop. 2015, 35, 661–665. [Google Scholar] [CrossRef]
- Eygendaal, D.; Bain, G.; Pederzini, L.; Poehling, G. Osteochondritis dissecans of the elbow: State of the art. J. ISAKOS 2017, 2, 47–57. [Google Scholar] [CrossRef]

| 1 (A) | 2 (B) | 3 (C) | 4 | 5 | |
|---|---|---|---|---|---|
| Milch [16] | Cast/CRPP | CRPP/ORIF | - | - | - |
| Jakobs [21] | Cast/CRPP | CRPP | ORIF | - | - |
| Finnbogason [22] | Cast/CRPP | CRPP | CRPP/ORIF | - | - |
| Weiss [23] | Cast/CRPP | CRPP | ORIF | - | - |
| Song [29] | Cast | Cast/CRPP | CRPP | CRPP | ORIF |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Saris, T.F.F.; Eygendaal, D.; The, B.; Colaris, J.W.; van Bergen, C.J.A. Lateral Humeral Condyle Fractures in Pediatric Patients. Children 2023, 10, 1033. https://doi.org/10.3390/children10061033
Saris TFF, Eygendaal D, The B, Colaris JW, van Bergen CJA. Lateral Humeral Condyle Fractures in Pediatric Patients. Children. 2023; 10(6):1033. https://doi.org/10.3390/children10061033
Chicago/Turabian StyleSaris, Tim F. F., Denise Eygendaal, Bertram The, Joost W. Colaris, and Christiaan J. A. van Bergen. 2023. "Lateral Humeral Condyle Fractures in Pediatric Patients" Children 10, no. 6: 1033. https://doi.org/10.3390/children10061033
APA StyleSaris, T. F. F., Eygendaal, D., The, B., Colaris, J. W., & van Bergen, C. J. A. (2023). Lateral Humeral Condyle Fractures in Pediatric Patients. Children, 10(6), 1033. https://doi.org/10.3390/children10061033








