Effect of Culturally Adapted Dental Visual Aids on Anxiety Levels in Children with Autism Spectrum Disorder: A Randomized Clinical Trial †
Abstract
:1. Introduction
2. Materials and Methods
2.1. Ethical Approval
2.2. Sample Size
2.3. Participants’ Eligibility Criteria
2.4. Inclusion Criteria
2.5. Exclusion Criteria
2.6. Study Design
2.7. Blinding and Randomization
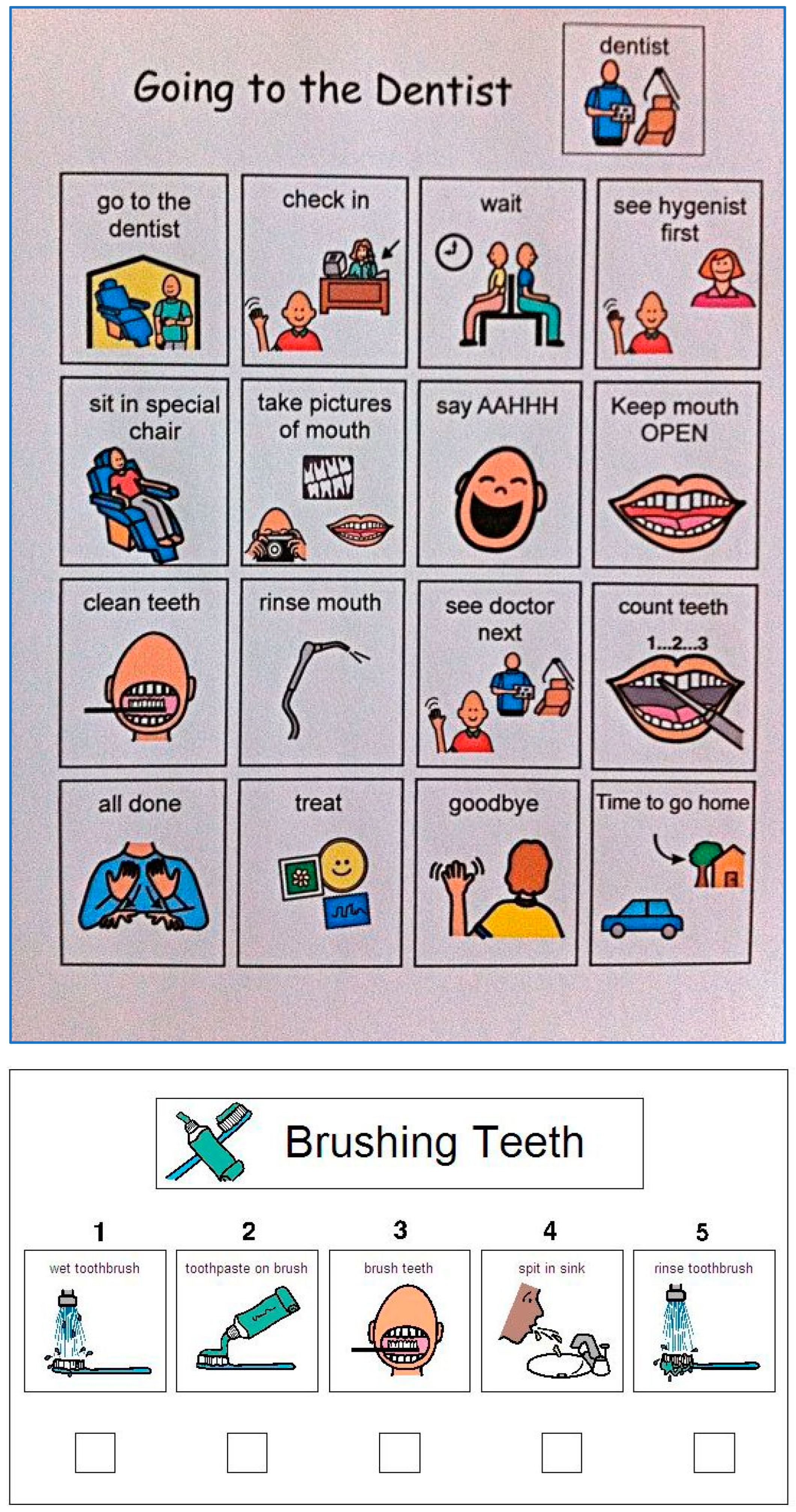
2.8. Interventions (Dental Visual Aids)
2.9. Preparatory Visit
2.10. Pre-Test Questionnaire
2.11. First Dental Assessment Visit
2.12. Second Dental Assessment Visit
2.13. Anxiety Level Scale
2.14. Calibration and Reliability
2.15. Statistical Analysis
3. Results
3.1. Characteristics of the Participants
3.2. Anxiety Scale for Children with ASD
3.2.1. Intragroup Comparison
3.2.2. Comparison between the Groups
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A. Ethical Approval

Appendix B. Anxiety Scale for Children with Autism Spectrum Disorder—Parent Version


References
- American Psychiatric Association (APA). Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; Text Revision (DSM-V-TR); American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Murshid, E.Z. Effectiveness of a preparatory aid in facilitating oral assessment in a group of Saudi children with autism spectrum disorders in Central Saudi Arabia. Saudi Med. J. 2017, 28, 533–540. [Google Scholar] [CrossRef] [PubMed]
- Isong, I.A.; Rao, S.R.; Holifield, C.; Iannuzzi, D.; Hanson, E.; Ware, J.; Nelson, L.P. Addressing Dental Fear in Children with Autism Spectrum Disorders: A Randomized Controlled Pilot Study Using Electronic Screen Media. Clin. Paediatr. 2014, 53, 230–237. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Gu, Z.; Wang, Y.; Wu, Q.; Chen, V.; Xu, X.; Zhou, X. Effect of audiovisual distraction on the management of dental anxiety in children: A systematic review. Int. J. Paediatr. Dent. 2019, 29, 14–21. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yildirim, T.T.; Dundar, S.; Bozoglan, A.; Karaman, T.; Dildes, N.; Kaya, F.A.; Altintas, E.; Oztekin, F.; Atas, O.; Alan, H. Is there a relation between dental anxiety, fear and general psychological status? PeerJ 2017, 5, 2978. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mah, J.W.; Tsang, P. Visual Schedule System in Dental Care for Patients with Autism: A Pilot Study. J. Clin. Paediatr. Dent. 2016, 40, 393–399. [Google Scholar] [CrossRef] [PubMed]
- American Academy of Pediatric Dentistry. Behavior guidance for the pediatric dental patient. In The Reference Manual of Pediatric Dentistry. Chicago, III: American Academy of Pediatric Dentistry; American Academy of Pediatric Dentistry: Chicago, IL, USA, 2022; pp. 321–339. [Google Scholar]
- Afif, I.Y.; Manik, A.R.; Munthe, K.; Maula, M.I.; Ammarullah, M.I.; Jamari, J.; Winarni, T.I. Physiological Effect of Deep Pressure in Reducing Anxiety of Children with ASD during Traveling: A Public Transportation Setting. Bioengineering 2022, 9, 157. [Google Scholar] [CrossRef] [PubMed]
- Afif, I.Y.; Farkhan, M.; Kurdi, O.; Maula, M.I.; Ammarullah, M.I.; Setiyana, B.; Jamari, J.; Winarni, T.I. Effect of Short-Term Deep-Pressure Portable Seat on Behavioral and Biological Stress in Children with Autism Spectrum Disorders: A Pilot Study. Bioengineering 2022, 9, 48. [Google Scholar] [CrossRef] [PubMed]
- Nilchian, F.; Shakibaei, F.; Jarah, Z.T. Evaluation of Visual Pedagogy in Dental Checkups and Preventive Practices among 6–12-Year-Old Children with Autism. J. Autism Dev. Disord. 2017, 47, 858–864. [Google Scholar] [CrossRef] [PubMed]
- Fakhruddin, K.S.; El Batawi, H.Y. Effectiveness of audiovisual distraction in behavior modification during dental caries assessment and sealant placement in children with autism spectrum disorder. Dent. Res. J. 2017, 14, 177–182. [Google Scholar] [CrossRef] [PubMed]
- Schopler, E.; Reichler, R.J.; DeVellis, R.F.; Daly, K. Toward objective classification of childhood autism: Childhood Autism Rating Scale (CARS). J. Autism Dev. Disord. 1980, 10, 91–103. [Google Scholar] [CrossRef] [PubMed]
- Centralstat. Central Department of Statistics and Information, Kingdom of Saudi Arabia. Spending and Household Income. Available online: http://cdsi.gov.sa/English/ (accessed on 12 January 2019).
- Rodgers, J.; Wigham, S.; McConachie, H.; Freeston, M.; Honey, E.; Parr, J.R. Development of the Anxiety Scale for children with Autism Spectrum Disorder (ASC-ASD). Autism Res. 2016, 9, 1205–1215. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- World Health Organization (WHO). Oral Health Surveys Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013. [Google Scholar]
- Cagetti, M.G.; Mastroberardino, S.; Campus, G.; Olivari, B.; Faggioli, R.; Lenti, C.; Strohmenger, L. Dental care protocol based on visual supports for children with autism spectrum disorders. Med. Oral Patol. Oral Cir. Bucal. 2015, 20, e598–e604. [Google Scholar] [CrossRef] [PubMed]
- Aljubour, A.A.; Al-Sehaibany, F. Characteristics of primary dentition occlusion among preschool children with autism spectrum disorder. J. Dent Health Oral Disord Ther. 2018, 9, 262–266. [Google Scholar]
- Villabø, M.A.; Gere, M.K.; Torgersen, S.; Marchand, G.H.; Kendall, P.C. Measuring anxiety in youth: A systematic review of assessment instruments. Psychol. Assess. 2021, 33, 631–652. [Google Scholar] [CrossRef]
- Rekha, C.V.; Arangannal, P.; Shahed, H. Oral health status of children with autistic disorder in Chennai. Eur. Arch. Paediatr. Dent. 2012, 13, 126–131. [Google Scholar] [CrossRef] [PubMed]
- Sallam, A.M.; Badr, S.B.Y.; Rashed, M.A. Effectiveness of audiovisual modeling on the behavioral change toward oral and dental care in children with autism. Indian J. Dent. 2013, 4, 184–190. [Google Scholar] [CrossRef]
- Jaber, M.A. Dental caries experience, oral health status and treatment needs of dental patients with autism. J. Appl. Oral Sci. 2011, 19, 212–217. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zink, A.G.; Diniz, M.B.; Rodrigues Dos Santos, M.T.B.; Guaré, R.O. Use of a Picture Exchange Communication System for preventive procedures in individuals with autism spectrum disorder: Pilot study. Spec. Care Dentist 2016, 36, 254–259. [Google Scholar] [CrossRef] [PubMed]
- Orellana, L.M.; Silvestre, F.J.; Martinez-Sanchis, S.; Martinez-Mihi, V.; Bautista, D. Oral manifestations in a group of adults with autism spectrum disorder. Med. Oral Patol. Oral Cir. Bucal. 2021, 17, 415–419. [Google Scholar] [CrossRef] [Green Version]
- Aljubour, A.A.; AbdElBaki, M.A.; El Meligy, O.A.; Al Jabri, B.A.; Sabbagh, H.J. Effectiveness of dental visual aids in behavior management of children with autism spectrum disorder: A systematic review. J. Child. Health Care 2021, 50, 83–107. [Google Scholar] [CrossRef]


| Group | Mean | SD | MED | p-Value | ||
|---|---|---|---|---|---|---|
| Total Anxiety Score | Test | Before | 22.090 | 11.650 | 19.500 | <0.001 * |
| After | 13.840 | 8.600 | 13.500 | |||
| Control | Before | 18.060 | 10.540 | 17.500 | 0.532 | |
| After | 18.060 | 12.160 | 14.00 | |||
| Performance Anxiety | Test | Before | 3.440 | 2.970 | 3.00 | 0.001 * |
| After | 1.940 | 2.200 | 1.00 | |||
| Control | Before | 3.000 | 3.210 | 2.500 | 0.259 | |
| After | 2.625 | 3.170 | 1.500 | |||
| Anxious Arousal | Test | Before | 3.690 | 2.290 | 3.00 | <0.001 * |
| After | 2.125 | 1.720 | 2.00 | |||
| Control | Before | 3.310 | 2.670 | 2.00 | 0.583 | |
| After | 3.500 | 2.910 | 2.500 | |||
| Separation Anxiety | Test | Before | 6.720 | 4.200 | 7.00 | 0.002 * |
| After | 4.375 | 2.485 | 4.00 | |||
| Control | Before | 5.090 | 2.720 | 5.00 | 0.692 | |
| After | 5.030 | 3.050 | 5.00 | |||
| Uncertainty | Test | Before | 8.250 | 5.435 | 8.500 | <0.001 * |
| After | 5.440 | 4.370 | 4.00 | |||
| Control | Before | 6.660 | 4.190 | 6.00 | 0.522 | |
| After | 7.190 | 4.770 | 8.00 |
| Test Group | Control Group | p-Value | |
|---|---|---|---|
| Anxiety Level | Mean | Mean | |
| Total Anxiety Score | −8.25 | 0.00 | <0.001 * |
| Performance Anxiety | −0.15 | −0.38 | 0.026 * |
| Anxious Arousal | −1.56 | 1.88 | <0.001 * |
| Separation Anxiety | −2.34 | −0.063 | 0.003 * |
| Uncertainty | −2.813 | 0.53 | <0.001 * |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Aljubour, A.; AbdElBaki, M.; El Meligy, O.; Al-Jabri, B.; Sabbagh, H. Effect of Culturally Adapted Dental Visual Aids on Anxiety Levels in Children with Autism Spectrum Disorder: A Randomized Clinical Trial. Children 2023, 10, 1040. https://doi.org/10.3390/children10061040
Aljubour A, AbdElBaki M, El Meligy O, Al-Jabri B, Sabbagh H. Effect of Culturally Adapted Dental Visual Aids on Anxiety Levels in Children with Autism Spectrum Disorder: A Randomized Clinical Trial. Children. 2023; 10(6):1040. https://doi.org/10.3390/children10061040
Chicago/Turabian StyleAljubour, Ala, Medhat AbdElBaki, Omar El Meligy, Basma Al-Jabri, and Heba Sabbagh. 2023. "Effect of Culturally Adapted Dental Visual Aids on Anxiety Levels in Children with Autism Spectrum Disorder: A Randomized Clinical Trial" Children 10, no. 6: 1040. https://doi.org/10.3390/children10061040
APA StyleAljubour, A., AbdElBaki, M., El Meligy, O., Al-Jabri, B., & Sabbagh, H. (2023). Effect of Culturally Adapted Dental Visual Aids on Anxiety Levels in Children with Autism Spectrum Disorder: A Randomized Clinical Trial. Children, 10(6), 1040. https://doi.org/10.3390/children10061040







