Exergames to Limit Weight Gain and to Fight Sedentarism in Children and Adolescents with Obesity
Abstract
1. Introduction
2. Materials and Methods
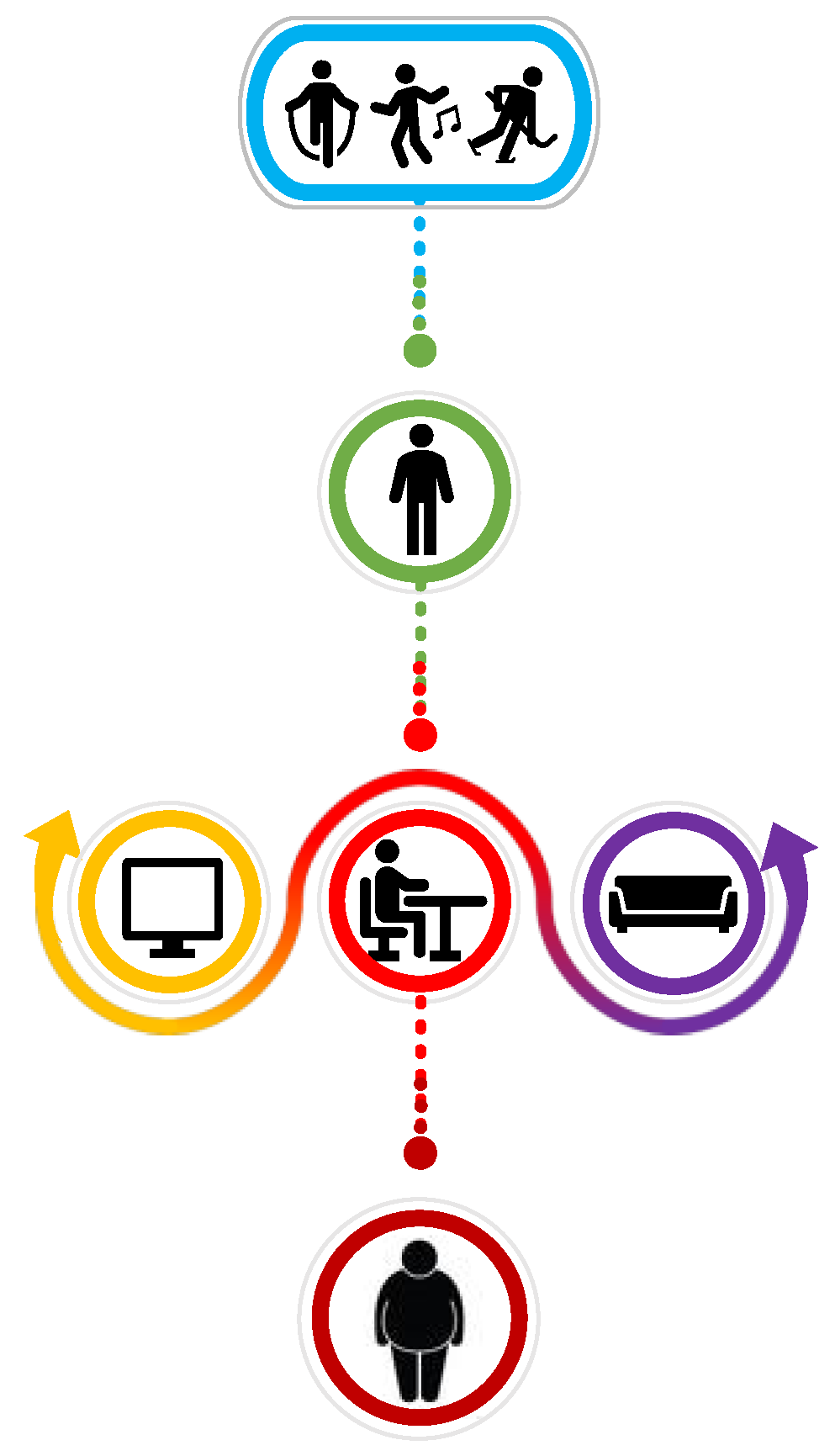
3. Physical Activity in Children and Adolescents with Obesity
4. Exergames
5. Exergames in Childhood Obesity
5.1. The Role of Exergames in Modifying Body Composition and Weight
5.2. Use of Exergames to Reduce Time Spent in Sedentary Behavior
6. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Van Biljon, A.; Longhurst, G.; Shaw, I.; Shaw, B.S. Role of Exergame Play on Cardiorespiratory Fitness and Body Composition in Overweight and Obese Children. Asian J. Sports Med. 2021, 12, e106782. [Google Scholar] [CrossRef]
- Gao, Z.; Chen, S. Are Field-Based Exergames Useful in Preventing Childhood Obesity? A Systematic Review: Exergame and Obesity. Obes. Rev. 2014, 15, 676–691. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Vandoni, M.; Rossi, V.; Berardo, C.; Grazi, R.; Cordaro, E.; Tranfaglia, V.; Carnevale Pellino, V.; Cereda, C.; Zuccotti, G. Use of Physical Activity and Exercise to Reduce Inflammation in Children and Adolescents with Obesity. Int. J. Environ. Res. Public Health 2022, 19, 6908. [Google Scholar] [CrossRef] [PubMed]
- Calcaterra, V.; Klersy, C.; Muratori, T.; Telli, S.; Caramagna, C.; Scaglia, F.; Cisternino, M.; Larizza, D. Prevalence of Metabolic Syndrome (MS) in Children and Adolescents with Varying Degrees of Obesity. Clin. Endocrinol. 2008, 68, 868–872. [Google Scholar] [CrossRef]
- Calcaterra, V.; Zuccotti, G. Physical Exercise as a Non-Pharmacological Intervention for Attenuating Obesity-Related Complications in Children and Adolescents. Int. J. Environ. Res. Public Health 2022, 19, 5046. [Google Scholar] [CrossRef]
- Owen, N.; Sparling, P.B.; Healy, G.N.; Dunstan, D.W.; Matthews, C.E. Sedentary Behavior: Emerging Evidence for a New Health Risk. Mayo Clin. Proc. 2010, 85, 1138–1141. [Google Scholar] [CrossRef]
- Valeriani, F.; Protano, C.; Marotta, D.; Liguori, G.; Romano Spica, V.; Valerio, G.; Vitali, M.; Gallè, F. Exergames in Childhood Obesity Treatment: A Systematic Review. Int. J. Environ. Res. Public Health 2021, 18, 4938. [Google Scholar] [CrossRef]
- Benzing, V.; Schmidt, M. Exergaming for Children and Adolescents: Strengths, Weaknesses, Opportunities and Threats. J. Clin. Med. 2018, 7, 422. [Google Scholar] [CrossRef]
- Graf, D.L.; Pratt, L.V.; Hester, C.N.; Short, K.R. Playing Active Video Games Increases Energy Expenditure in Children. Pediatrics 2009, 124, 534–540. [Google Scholar] [CrossRef]
- Bailey, B.W.; McInnis, K. Energy Cost of Exergaming: A Comparison of the Energy Cost of 6 Forms of Exergaming. Arch. Pediatr. Adolesc. Med. 2011, 165, 597–602. [Google Scholar] [CrossRef]
- Staiano, A.E.; Abraham, A.A.; Calvert, S.L. Adolescent Exergame Play for Weight Loss and Psychosocial Improvement: A Controlled Physical Activity Intervention. Obesity 2013, 21, 598–601. [Google Scholar] [CrossRef] [PubMed]
- Gregory, A.T.; Denniss, A.R. An Introduction to Writing Narrative and Systematic Reviews-Tasks, Tips and Traps for Aspiring Authors. Heart Lung Circ. 2018, 27, 893–898. [Google Scholar] [CrossRef] [PubMed]
- Baethge, C.; Goldbeck-Wood, S.; Mertens, S. SANRA—A Scale for the Quality Assessment of Narrative Review Articles. Res. Integr. Peer Rev. 2019, 4, 5. [Google Scholar] [CrossRef] [PubMed]
- Bethea, T.C.; Berry, D.; Maloney, A.E.; Sikich, L. Pilot Study of an Active Screen Time Game Correlates with Improved Physical Fitness in Minority Elementary School Youth. Games Health J. 2012, 1, 29–36. [Google Scholar] [CrossRef]
- Murphy, E.C.-S.; Carson, L.; Neal, W.; Baylis, C.; Donley, D.; Yeater, R. Effects of an Exercise Intervention Using Dance Dance Revolution on Endothelial Function and Other Risk Factors in Overweight Children. Int. J. Pediatr. Obes. 2009, 4, 205–214. [Google Scholar] [CrossRef]
- Ni Mhurchu, C.; Maddison, R.; Jiang, Y.; Jull, A.; Prapavessis, H.; Rodgers, A. Couch Potatoes to Jumping Beans: A Pilot Study of the Effect of Active Video Games on Physical Activity in Children. Int. J. Behav. Nutr. Phys. Act. 2008, 5, 8. [Google Scholar] [CrossRef]
- Staiano, A.E.; Marker, A.M.; Beyl, R.A.; Hsia, D.S.; Katzmarzyk, P.T.; Newton, R.L. A Randomized Controlled Trial of Dance Exergaming for Exercise Training in Overweight and Obese Adolescent Girls: Exergaming in Overweight Adolescent Girls. Pediatr. Obes. 2017, 12, 120–128. [Google Scholar] [CrossRef]
- Trost, S.G.; Sundal, D.; Foster, G.D.; Lent, M.R.; Vojta, D. Effects of a Pediatric Weight Management Program with and without Active Video Games a Randomized Trial. JAMA Pediatr. 2014, 168, 407–413. [Google Scholar] [CrossRef]
- Maddison, R.; Foley, L.; Ni Mhurchu, C.; Jiang, Y.; Jull, A.; Prapavessis, H.; Hohepa, M.; Rodgers, A. Effects of Active Video Games on Body Composition: A Randomized Controlled Trial. Am. J. Clin. Nutr. 2011, 94, 156–163. [Google Scholar] [CrossRef]
- Baranowski, T.; Abdelsamad, D.; Baranowski, J.; O’Connor, T.M.; Thompson, D.; Barnett, A.; Cerin, E.; Chen, T.-A. Impact of an Active Video Game on Healthy Children’s Physical Activity. Pediatrics 2012, 129, e636–e642. [Google Scholar] [CrossRef]
- Gao, Z.; Podlog, L. Urban Latino Children’s Physical Activity Levels and Performance in Interactive Dance Video Games: Effects of Goal Difficulty and Goal Specificity. Arch. Pediatr. Adolesc. Med. 2012, 166, 933–937. [Google Scholar] [CrossRef][Green Version]
- Martínez-López, E.J.; López-Serrano, S.; De La Torre-Cruz, M.; Ruiz-Ariza, A. Effects of the Augmented Reality Game Pokémon GO on Fitness and Fatness in Secondary School Students. Health Educ. J. 2022, 81, 54–68. [Google Scholar] [CrossRef]
- Schneider, E.F. Death with a Story: How Story Impacts Emotional, Motivational, and Physiological Responses to First-Person Shooter Video Games. Hum. Commun. Res. 2004, 30, 361–375. [Google Scholar] [CrossRef]
- Simons, M.; Brug, J.; Chinapaw, M.J.M.; de Boer, M.; Seidell, J.; de Vet, E. Replacing Non-Active Video Gaming by Active Video Gaming to Prevent Excessive Weight Gain in Adolescents. PLoS ONE 2015, 10, e0126023. [Google Scholar] [CrossRef]
- Graves, L.E.F.; Ridgers, N.D.; Atkinson, G.; Stratton, G. The Effect of Active Video Gaming on Children’s Physical Activity, Behavior Preferences and Body Composition. Pediatr. Exerc. Sci. 2010, 22, 535–546. [Google Scholar] [CrossRef]
- Wagener, T.L.; Fedele, D.A.; Mignogna, M.R.; Hester, C.N.; Gillaspy, S.R. Psychological Effects of Dance-Based Group Exergaming in Obese Adolescents. Pediatr. Obes. 2012, 7, e68–e74. [Google Scholar] [CrossRef]
- Maloney, A.E.; Threlkeld, K.A.; Cook, W.L. Comparative Effectiveness of a 12-Week Physical Activity Intervention for Overweight and Obese Youth: Exergaming with “Dance Dance Revolution”. Games Health J. 2012, 1, 96–103. [Google Scholar] [CrossRef]
- Staiano, A.E.; Beyl, R.A.; Hsia, D.S.; Katzmarzyk, P.T.; Newton, R.L. Twelve Weeks of Dance Exergaming in Overweight and Obese Adolescent Girls: Transfer Effects on Physical Activity, Screen Time, and Self-Efficacy. J. Sport Health Sci. 2017, 6, 4–10. [Google Scholar] [CrossRef]
- Maloney, A.E.; Bethea, T.C.; Kelsey, K.S.; Marks, J.T.; Paez, S.; Rosenberg, A.M.; Catellier, D.J.; Hamer, R.M.; Sikich, L. A Pilot of a Video Game (DDR) to Promote Physical Activity and Decrease Sedentary Screen Time. Obesity 2008, 16, 2074–2080. [Google Scholar] [CrossRef]
- Staiano, A.E.; Beyl, R.A.; Guan, W.; Hendrick, C.A.; Hsia, D.S.; Newton, R.L. Home-Based Exergaming among Children with Overweight and Obesity: A Randomized Clinical Trial. Pediatr. Obes. 2018, 13, 724–733. [Google Scholar] [CrossRef]
- Liang, Y.; Lau, P.W.C.; Jiang, Y.; Maddison, R. Getting Active with Active Video Games: A Quasi-Experimental Study. Int. J. Environ. Res. Public Health 2020, 17, 7984. [Google Scholar] [CrossRef] [PubMed]
- Christison, A.; Khan, H.A. Exergaming for Health: A Community-Based Pediatric Weight Management Program Using Active Video Gaming. Clin. Pediatr. 2012, 51, 382–388. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization (WHO). Physical Activity. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 30 April 2023).
- Nemet, D. Childhood Obesity, Physical Activity, and Exercise. Pediatr. Exerc. Sci. 2017, 29, 60–62. [Google Scholar] [CrossRef] [PubMed]
- García-Hermoso, A.; Ramírez-Vélez, R.; Ramírez-Campillo, R.; Peterson, M.D.; Martínez-Vizcaíno, V. Concurrent Aerobic plus Resistance Exercise versus Aerobic Exercise Alone to Improve Health Outcomes in Paediatric Obesity: A Systematic Review and Meta-Analysis. Br. J. Sports Med. 2018, 52, 161–166. [Google Scholar] [CrossRef]
- Calcaterra, V.; Verduci, E.; Vandoni, M.; Rossi, V.; Fiore, G.; Massini, G.; Berardo, C.; Gatti, A.; Baldassarre, P.; Bianchi, A.; et al. The Effect of Healthy Lifestyle Strategies on the Management of Insulin Resistance in Children and Adolescents with Obesity: A Narrative Review. Nutrients 2022, 14, 4692. [Google Scholar] [CrossRef]
- Marson, E.C.; Delevatti, R.S.; Prado, A.K.G.; Netto, N.; Kruel, L.F.M. Effects of Aerobic, Resistance, and Combined Exercise Training on Insulin Resistance Markers in Overweight or Obese Children and Adolescents: A Systematic Review and Meta-Analysis. Prev. Med. 2016, 93, 211–218. [Google Scholar] [CrossRef]
- Stodden, D.F.; Goodway, J.D.; Langendorfer, S.J.; Roberton, M.A.; Rudisill, M.E.; Garcia, C.; Garcia, L.E. A Developmental Perspective on the Role of Motor Skill Competence in Physical Activity: An Emergent Relationship. Quest 2008, 60, 290–306. [Google Scholar] [CrossRef]
- Romero-Pérez, E.M.; González-Bernal, J.J.; Soto-Cámara, R.; González-Santos, J.; Tánori-Tapia, J.M.; Rodríguez-Fernández, P.; Jiménez-Barrios, M.; Márquez, S.; de Paz, J.A. Influence of a Physical Exercise Program in the Anxiety and Depression in Children with Obesity. Int. J. Environ. Res. Public. Health 2020, 17, 4655. [Google Scholar] [CrossRef]
- Vandoni, M.; Carnevale Pellino, V.; Gatti, A.; Lucini, D.; Mannarino, S.; Larizza, C.; Rossi, V.; Tranfaglia, V.; Pirazzi, A.; Biino, V.; et al. Effects of an Online Supervised Exercise Training in Children with Obesity during the COVID-19 Pandemic. Int. J. Environ. Res. Public. Health 2022, 19, 9421. [Google Scholar] [CrossRef]
- Pancar, Z.; Özdal, M.; Çinar, V. The Effect of 4-Weekly Low Intensity Physical Activity Program in Thyroid Hormone Levels in Obese and Overweight Children. Eur. J. Phys. Educ. Sport. Sci. 2017, 3, 11. [Google Scholar] [CrossRef]
- Pienaar, A.E.; Du Toit, D.; Truter, L. The Effect of a Multidisciplinary Physical Activity Intervention on the Body Composition and Physical Fitness of Obese Children. J. Sports Med. Phys. Fitness 2013, 53, 415–427. [Google Scholar]
- Alberga, A.S.; Prud’homme, D.; Sigal, R.J.; Goldfield, G.S.; Hadjiyannakis, S.; Phillips, P.; Malcolm, J.; Ma, J.; Doucette, S.; Gougeon, R.; et al. Effects of Aerobic Training, Resistance Training, or Both on Cardiorespiratory and Musculoskeletal Fitness in Adolescents with Obesity: The HEARTY Trial. Appl. Physiol. Nutr. Metab. 2016, 41, 255–265. [Google Scholar] [CrossRef]
- Molina-Garcia, P.; Mora-Gonzalez, J.; Migueles, J.H.; Rodriguez-Ayllon, M.; Esteban-Cornejo, I.; Cadenas-Sanchez, C.; Plaza-Florido, A.; Gil-Cosano, J.J.; Pelaez-Perez, M.A.; Garcia-Delgado, G.; et al. Effects of Exercise on Body Posture, Functional Movement, and Physical Fitness in Children with Overweight/Obesity. J. Strength Cond. Res. 2020, 34, 2146–2155. [Google Scholar] [CrossRef]
- Bouamra, M.; Zouhal, H.; Ratel, S.; Makhlouf, I.; Bezrati, I.; Chtara, M.; Behm, D.G.; Granacher, U.; Chaouachi, A. Concurrent Training Promotes Greater Gains on Body Composition and Components of Physical Fitness Than Single-Mode Training (Endurance or Resistance) in Youth with Obesity. Front. Physiol. 2022, 13, 869063. [Google Scholar] [CrossRef]
- Paduano, S.; Greco, A.; Borsari, L.; Salvia, C.; Tancredi, S.; Pinca, J.; Midili, S.; Tripodi, A.; Borella, P.; Marchesi, I. Physical and Sedentary Activities and Childhood Overweight/Obesity: A Cross-Sectional Study among First-Year Children of Primary Schools in Modena, Italy. Int. J. Environ. Res. Public. Health 2021, 18, 3221. [Google Scholar] [CrossRef]
- Bull, F.C.; Al-Ansari, S.S.; Biddle, S.; Borodulin, K.; Buman, M.P.; Cardon, G.; Carty, C.; Chaput, J.-P.; Chastin, S.; Chou, R.; et al. World Health Organization 2020 Guidelines on Physical Activity and Sedentary Behaviour. Br. J. Sports Med. 2020, 54, 1451–1462. [Google Scholar] [CrossRef]
- Smith, K.L.; Straker, L.M.; McManus, A.; Fenner, A.A. Barriers and Enablers for Participation in Healthy Lifestyle Programs by Adolescents Who Are Overweight: A Qualitative Study of the Opinions of Adolescents, Their Parents and Community Stakeholders. BMC Pediatr. 2014, 14, 53. [Google Scholar] [CrossRef]
- Stodden, D.F.; Gao, Z.; Goodway, J.D.; Langendorfer, S.J. Dynamic Relationships between Motor Skill Competence and Health-Related Fitness in Youth. Pediatr. Exerc. Sci. 2014, 26, 231–241. [Google Scholar] [CrossRef]
- Harter, S.; Bukowski, W.M. The Construction of the Self: Developmental and Sociocultural Foundations; Distinguished Contributions in Psychology; Guilford Publications: New York, NY, USA, 2012; ISBN 978-1-4625-0297-4. [Google Scholar]
- Lovecchio, N.; Zago, M. Fitness Differences According to BMI Categories: A New Point of View. J. Sports Med. Phys. Fitness 2019, 59, 298–303. [Google Scholar] [CrossRef]
- Calcaterra, V.; Larizza, D.; Codrons, E.; De Silvestri, A.; Brambilla, P.; Abela, S.; Arpesella, M.; Vandoni, M. Improved Metabolic and Cardiorespiratory Fitness during a Recreational Training Program in Obese Children. J. Pediatr. Endocrinol. Metab. 2013, 26, 271–276. [Google Scholar] [CrossRef]
- Comeras-Chueca, C.; Villalba-Heredia, L.; Perez-Lasierra, J.L.; Marín-Puyalto, J.; Lozano-Berges, G.; Matute-Llorente, Á.; Vicente-Rodríguez, G.; Gonzalez-Aguero, A.; Casajús, J.A. Active Video Games Improve Muscular Fitness and Motor Skills in Children with Overweight or Obesity. Int. J. Environ. Res. Public. Health 2022, 19, 2642. [Google Scholar] [CrossRef] [PubMed]
- Benzing, V.; Schmidt, M. The Effect of Exergaming on Executive Functions in Children with ADHD: A Randomized Clinical Trial. Scand. J. Med. Sci. Sports 2019, 29, 1243–1253. [Google Scholar] [CrossRef] [PubMed]
- Lima, J.L.; Axt, G.; Teixeira, D.S.; Monteiro, D.; Cid, L.; Yamamoto, T.; Murillo-Rodriguez, E.; Machado, S. Exergames for Children and Adolescents with Autism Spectrum Disorder: An Overview. Clin. Pract. Epidemiol. Ment. Health 2020, 16, 1–6. [Google Scholar] [CrossRef] [PubMed]
- Kracht, C.L.; Joseph, E.D.; Staiano, A.E. Video Games, Obesity, and Children. Curr. Obes. Rep. 2020, 9, 1–14. [Google Scholar] [CrossRef] [PubMed]
- Abd-alrazaq, A.; Alajlani, M.; Alhuwail, D.; Schneider, J.; Akhu-Zaheya, L.; Ahmed, A.; Househ, M. The Effectiveness of Serious Games in Alleviating Anxiety: Systematic Review and Meta-Analysis. JMIR Serious Games 2022, 10, e29137. [Google Scholar] [CrossRef]
- Comeras-Chueca, C.; Marin-Puyalto, J.; Matute-Llorente, A.; Vicente-Rodriguez, G.; Casajus, J.A.; Gonzalez-Aguero, A. The Effects of Active Video Games on Health-Related Physical Fitness and Motor Competence in Children and Adolescents with Healthy Weight: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 6965. [Google Scholar] [CrossRef]
- O’Neil, O.; Fernandez, M.M.; Herzog, J.; Beorchia, M.; Gower, V.; Gramatica, F.; Starrost, K.; Kiwull, L. Virtual Reality for Neurorehabilitation: Insights From 3 European Clinics. PM&R 2018, 10, S198–S206. [Google Scholar] [CrossRef]
- Smits-Engelsman, B.; Bonney, E.; Ferguson, G. Effects of Graded Exergames on Fitness Performance in Elementary School Children with Developmental Coordination Disorder. Front. Sports Act. Living 2021, 3, 653851. [Google Scholar] [CrossRef]
- Vandoni, M.; Codella, R.; Pippi, R.; Carnevale Pellino, V.; Lovecchio, N.; Marin, L.; Silvestri, D.; Gatti, A.; Magenes, V.C.; Regalbuto, C.; et al. Combatting Sedentary Behaviors by Delivering Remote Physical Exercise in Children and Adolescents with Obesity in the COVID-19 Era: A Narrative Review. Nutrients 2021, 13, 4459. [Google Scholar] [CrossRef]
- Lee, I.-M.; Shiroma, E.J.; Lobelo, F.; Puska, P.; Blair, S.N.; Katzmarzyk, P.T. Effect of Physical Inactivity on Major Non-Communicable Diseases Worldwide: An Analysis of Burden of Disease and Life Expectancy. Lancet 2012, 380, 219–229. [Google Scholar] [CrossRef]
- Hwang, J.; Lee, I.-M.; Fernandez, A.M.; Hillman, C.H.; Lu, A.S. Exploring Energy Expenditure and Body Movement of Exergaming in Children of Different Weight Status. Pediatr. Exerc. Sci. 2019, 31, 438–447. [Google Scholar] [CrossRef]
- Biro, F.M.; Wien, M. Childhood Obesity and Adult Morbidities. Am. J. Clin. Nutr. 2010, 91, S1499–S1505. [Google Scholar] [CrossRef]
- Benjamin, R.M. The Surgeon General’s Vision for a Healthy and Fit Nation. Public Health Rep. 2010, 125, 514–515. [Google Scholar] [CrossRef]
- McGuire, S. Institute of Medicine. 2012. Accelerating Progress in Obesity Prevention: Solving the Weight of the Nation. Washington, DC: The National Academies Press. Adv. Nutr. 2012, 3, 708–709. [Google Scholar] [CrossRef]
- Uys, M.; Bassett, S.; Draper, C.E.; Micklesfield, L.; Monyeki, A.; de Villiers, A.; Lambert, E.V. Results from South Africa’s 2016 Report Card on Physical Activity for Children and Youth. J. Phys. Act. Health 2016, 13, S265–S273. [Google Scholar] [CrossRef]
- Piercy, K.L.; Troiano, R.P.; Ballard, R.M.; Carlson, S.A.; Fulton, J.E.; Galuska, D.A.; George, S.M.; Olson, R.D. The Physical Activity Guidelines for Americans. JAMA 2018, 320, 2020. [Google Scholar] [CrossRef]
- Strasburger, V.C.; Council on Communications and Media. Children, Adolescents, Obesity, and the Media. Pediatrics 2011, 128, 201–208. [Google Scholar] [CrossRef]
- Katzmarzyk, P.T.; Denstel, K.D.; Beals, K.; Bolling, C.; Wright, C.; Crouter, S.E.; McKenzie, T.L.; Pate, R.R.; Saelens, B.E.; Staiano, A.E.; et al. Results from the United States of America’s 2016 Report Card on Physical Activity for Children and Youth. J. Phys. Act. Health 2016, 13, S307–S313. [Google Scholar] [CrossRef]
- Sween, J.; Wallington, S.F.; Sheppard, V.; Taylor, T.; Llanos, A.A.; Adams-Campbell, L.L. The Role of Exergaming in Improving Physical Activity: A Review. J. Phys. Act. Health 2014, 11, 864–870. [Google Scholar] [CrossRef]
- Guy, S.; Ratzki-Leewing, A.; Gwadry-Sridhar, F. Moving Beyond the Stigma: Systematic Review of Video Games and Their Potential to Combat Obesity. Int. J. Hypertens. 2011, 2011, 1–13. [Google Scholar] [CrossRef]
- Daley, A.J. Can Exergaming Contribute to Improving Physical Activity Levels and Health Outcomes in Children? Pediatrics 2009, 124, 763–771. [Google Scholar] [CrossRef] [PubMed]
- Foley, L.; Maddison, R. Use of Active Video Games to Increase Physical Activity in Children: A (Virtual) Reality? Pediatr. Exerc. Sci. 2010, 22, 7–20. [Google Scholar] [CrossRef] [PubMed]
- Biddiss, E.; Irwin, J. Active Video Games to Promote Physical Activity in Children and Youth: A Systematic Review. Arch. Pediatr. Adolesc. Med. 2010, 164, 664–672. [Google Scholar] [CrossRef] [PubMed]
- Gao, Z.; Zeng, N. Exergaming and Obesity in Youth: Current Perspectives. Int. J. Gen. Med. 2016, 9, 275–284. [Google Scholar] [CrossRef]
- Anderson, N.; Steele, J.; O’Neill, L.-A.; Harden, L.A. Pokémon Go: Mobile App User Guides. Br. J. Sports Med. 2017, 51, 1505–1506. [Google Scholar] [CrossRef]
- Serino, M.; Cordrey, K.; McLaughlin, L.; Milanaik, R.L. Pokémon Go and Augmented Virtual Reality Games: A Cautionary Commentary for Parents and Pediatricians. Curr. Opin. Pediatr. 2016, 28, 673–677. [Google Scholar] [CrossRef]
- Jakobsson, M. The Achievement Machine: Understanding Xbox 360 Achievements in Gaming Practices. Game Stud. 2011, 11. [Google Scholar]
- Warburton, D.E.R.; Bredin, S.S.D.; Horita, L.T.L.; Zbogar, D.; Scott, J.M.; Esch, B.T.A.; Rhodes, R.E. The Health Benefits of Interactive Video Game Exercise. Appl. Physiol. Nutr. Metab. 2007, 32, 655–663. [Google Scholar] [CrossRef]
- Smits-Engelsman, B.C.M.; Jelsma, L.D.; Ferguson, G.D. The Effect of Exergames on Functional Strength, Anaerobic Fitness, Balance and Agility in Children with and without Motor Coordination Difficulties Living in Low-Income Communities. Hum. Mov. Sci. 2017, 55, 327–337. [Google Scholar] [CrossRef]
- Chin, A.; Paw, M.J.M.; Jacobs, W.M.; Vaessen, E.P.G.; Titze, S.; van Mechelen, W. The Motivation of Children to Play an Active Video Game. J. Sci. Med. Sport 2008, 11, 163–166. [Google Scholar] [CrossRef]
- Liang, Y.; Lau, P.W.C. Effects of Active Videogames on Physical Activity and Related Outcomes Among Healthy Children: A Systematic Review. Games Health J. 2014, 3, 122–144. [Google Scholar] [CrossRef]
- Lu, A.S. Narrative in Exergames: Thoughts on Procedure, Mechanism, and Others. Games Health J. 2015, 4, 19–24. [Google Scholar] [CrossRef]
- Lu, A.S.; Thompson, D.; Baranowski, J.; Buday, R.; Baranowski, T. Story Immersion in a Health Videogame for Childhood Obesity Prevention. Games Health J. 2012, 1, 37–44. [Google Scholar] [CrossRef]
- Caroli, M.; Argentieri, L.; Cardone, M.; Masi, A. Role of Television in Childhood Obesity Prevention. Int. J. Obes. Relat. Metab. Disord. 2004, 28, S104–S108. [Google Scholar] [CrossRef]
- Nelson, M.C.; Neumark-Stzainer, D.; Hannan, P.J.; Sirard, J.R.; Story, M. Longitudinal and Secular Trends in Physical Activityand Sedentary Behavior during Adolescence. Pediatrics 2006, 118, e1627–e1634. [Google Scholar] [CrossRef]
- Foley, L.S.; Maddison, R.; Jiang, Y.; Olds, T.; Ridley, K. It’s Not Just the Television: Survey Analysis of Sedentary Behaviour in New Zealand Young People. Int. J. Behav. Nutr. Phys. Act. 2011, 8, 132. [Google Scholar] [CrossRef]
- Marshall, S.J.; Biddle, S.J.H.; Gorely, T.; Cameron, N.; Murdey, I. Relationships between Media Use, Body Fatness and Physical Activity in Children and Youth: A Meta-Analysis. Int. J. Obes. Relat. Metab. Disord. 2004, 28, 1238–1246. [Google Scholar] [CrossRef]
- Vandewater, E.A.; Shim, M.; Caplovitz, A.G. Linking Obesity and Activity Level with Children’s Television and Video Game Use. J. Adolesc. 2004, 27, 71–85. [Google Scholar] [CrossRef]
- Chaput, J.-P.; Visby, T.; Nyby, S.; Klingenberg, L.; Gregersen, N.T.; Tremblay, A.; Astrup, A.; Sjödin, A. Video Game Playing Increases Food Intake in Adolescents: A Randomized Crossover Study. Am. J. Clin. Nutr. 2011, 93, 1196–1203. [Google Scholar] [CrossRef]
- Janz, K.F.; Levy, S.M.; Burns, T.L.; Torner, J.C.; Willing, M.C.; Warren, J.J. Fatness, Physical Activity, and Television Viewing in Children during the Adiposity Rebound Period: The Iowa Bone Development Study. Prev. Med. 2002, 35, 563–571. [Google Scholar] [CrossRef]
- Fisher, A.; Reilly, J.J.; Montgomery, C.; Kelly, L.A.; Williamson, A.; Jackson, D.M.; Paton, J.Y.; Grant, S. Seasonality in Physical Activity and Sedentary Behavior in Young Children. Pediatr. Exerc. Sci. 2005, 17, 31–40. [Google Scholar] [CrossRef]
- Colley, R.C.; Garriguet, D.; Janssen, I.; Craig, C.L.; Clarke, J.; Tremblay, M.S. Physical Activity of Canadian Children and Youth: Accelerometer Results from the 2007 to 2009 Canadian Health Measures Survey. Health Rep. 2011, 22, 15–23. [Google Scholar] [PubMed]
- Sardinha, L.B.; Andersen, L.B.; Anderssen, S.A.; Quitério, A.L.; Ornelas, R.; Froberg, K.; Riddoch, C.J.; Ekelund, U. Objectively Measured Time Spent Sedentary Is Associated with Insulin Resistance Independent of Overall and Central Body Fat in 9- to 10-Year-Old Portuguese Children. Diabetes Care 2008, 31, 569–575. [Google Scholar] [CrossRef] [PubMed]
- Strauss, R.S.; Rodzilsky, D.; Burack, G.; Colin, M. Psychosocial Correlates of Physical Activity in Healthy Children. Arch. Pediatr. Adolesc. Med. 2001, 155, 897–902. [Google Scholar] [CrossRef]
- Fullerton, S.; Taylor, A.W.; Dal Grande, E.; Berry, N. Measuring Physical Inactivity: Do Current Measures Provide an Accurate View of “Sedentary” Video Game Time? J. Obes. 2014, 2014, 287013. [Google Scholar] [CrossRef]
- Lamboglia, C.M.G.F.; da Silva, V.T.B.L.; de Vasconcelos Filho, J.E.; Pinheiro, M.H.N.P.; da Silva Munguba, M.C.; Silva Júnior, F.V.I.; de Paula, F.A.R.; da Silva, C.A.B. Exergaming as a Strategic Tool in the Fight against Childhood Obesity: A Systematic Review. J. Obes. 2013, 2013, 438364. [Google Scholar] [CrossRef][Green Version]

| Author, Year | Study Design | Subjects (n°/Age) | Setting | Intervention Group (AVG/Frequency) | Control Group | Follow-Up |
|---|---|---|---|---|---|---|
| Bethea et al., 2012 [14] | Pilot study | IG: 34 CG: 28 9.9 ± 0.7 years | After school/Home | PlayStation 2®, DDR Extreme game®, dance mats up to 3 days/week for approximately 30 min during school and unlimited access at home | None | 30 weeks |
| Murphy et al., 2009 [15] | RCT | IG: 23; 10.21 ± 1.67 years CG: 12; 7–12 years | Home | DDR 5 days per week | None | 12 weeks |
| Ni Mhurchu et al., 2008 [16] | RCT | IG: 10 CG: 10 12 ± 1.5 years | Home | PlayStation Eye-Toy, and dance mat. Unspecified | Yes | 12 weeks |
| Staiano et al., 2013 [11] | RCT | IG: 54 15–19 years CG: 16; 15–19 years | Home | Nintendo Wii Active exergame 30–60 min every school day during the lunch period or after school | Yes | 12 weeks |
| Staiano et al., 2017 [17] | RCT | IG: 22 14–18 years CG: 19 14–18 years | Research laboratory | Dance exergaming Kinect for Xbox 360 (Microsoft Corporation, Redmond, WA, USA) 1 h of exergaming sessions per week | Yes | 12 weeks |
| Trost et al., 2014 [18] | Randomized study | IG: 34; 10.1 ± 1.9 years CG: 41; 9.9 ± 1.5 years | Clinic | Kinect and Xbox 360 (Kinect sports) Unspecified | No active games | 16 weeks |
| Maddison et al., 2011 [19] | RCT | IG: 160 10–14 years CG: 162 10–14 years | Home | PlayStation EyeToy (Sony), USB motion-capture camera, dance mat, and a selection of active video games (e.g., Play3, Kinetic, Sport, and Dance Factory; Sony) 60 min of moderate-to-vigorous physical activity on most days of the week | No active games | 24 weeks |
| Baranowski et al., 2012 [20] | RCT | IG: 41 9–12 years CG: 43 9–12 years | Home | Wii console 30 min per day, 5 days per week | No active games | 12 weeks |
| Gao et al., 2012 [21] | RCT | IG: 70 9–12 years CG: 33 9–12 years | Home | Dance Dance Revolution [DDR]; Konami Corporation Unspecified | No active games | 8 weeks |
| Martínez-López et al., 2022 [22] | Quantitative longitudinal study | IG: 78 12–15 years CG: 86 12–15 years | Outdoor | Pokémon GO®; Unspecified | Yes | 8 weeks |
| Author, Year | Outcome | Tool | Results | p-Value |
|---|---|---|---|---|
| Bethea et al., 2012 [14] | Physical activity/physical fitness/use of home Dance Dance Revolution/safety and acceptability/anthropometric/fasting metabolic profile at baseline, 12 weeks, and 30 weeks | FitnessGram®, a standardized physical fitness test battery. | IG were more active than CG | Significant |
| Murphy et al., 2009 [15] | Endothelial function and other risk factors in overweight children | Brachial artery flow-mediated dilatation (FMD), dual-energy X-ray absorptiometry, blood pressure measurement, fasting blood samples, insulin sensitivity index via oral glucose tolerance test, and physical fitness testing | IG had improved endothelial function and decreased body mass index, waist circumference, and systolic blood pressure than did CG | Significant |
| Ni Mhurchu et al., 2008 [16] | PA levels | Actigraph e PAQ-C | IG were more active than were CG | Significant |
| Staiano et al., 2013 [11] | Primary outcome: weight loss. Secondary outcomes: changes in BMI, self-esteem, and perceived physical competence. | Anthropometric measures, self-reported questionnaires, and physical fitness tests | IG had better weight loss and improved BMI, self-esteem, and perceived physical competence | Significant |
| Staiano et al., 2017 [17] | Body composition physical fitness, daily physical activity, sedentary time, dietary intake, and psychosocial well-being | Anthropometry, dual-energy X-ray absorptiometry, and magnetic resonance imaging to assess body composition. Youth Physical Activity Questionnaire, the Block Food Frequency Questionnaire, and the Pediatric Quality of Life Inventory | IG had significantly improved body composition, physical fitness, daily physical activity, and decreased sedentary time compared to CG. There were no significant differences in dietary intake or psychosocial well-being between IG and CG. | Significant |
| Trost et al., 2014 [18] | Sedentary behavior change | Actigraph | IG had decreases sedentary time compared to CG | Significant |
| Maddison et al., 2011 [19] | Changes in body composition (BMI, fat mass, waist circumference) | BIA, Actigraph | IG had decreased BMI, fat mass, and waist circumference compared to CG | Significant |
| Baranowski et al., 2012 [20] | Physical activity level | Actigraph GT33 x accelerometers | IG were not more active in general, or at any time, than were CG | Nonsignificant |
| Gao et al., 2012 [21] | Physical activity level | Actigraph accelerometer and AVG performance scores | IG had higher physical activity levels than did CG | Significant |
| Martínez-López et al., 2021 [23] | Physical fitness and fatness | Measures of physical fitness (CRF, S/A, MS) were assessed using the ALPHA health-related fitness test battery for youth. Measures of fatness were BMI (assessed through height, measured by ASIMED® B-type-class III (Guayaquil, Ecuador), and weight, measured through a portable height meter SECA 214® Ltd., Reinach, Switzerland), BIA (measured through Biospace InBody 720 bioelectrical impedance analyzer) and waist and hip circumferences (measured with tape measure) | IG had greater improvement for CRF, BMI, and %BF than did CG | Physical fitness: significant for CRF but not significant for S/A or MS; Fatness: significant for BMI and %BF but not significant for WHI |
| Author, Year | Study Design | Subjects (n°/Age) | Setting | Intervention Group (AVG/Frequency) | Control Group | Follow-Up |
|---|---|---|---|---|---|---|
| Ni Mhurchu et al., 2008 [16] | RCT | IG: 10 CG: 10 12 ± 1.5 years | Home | PlayStation Eye-Toy, and dance mat. Unspecified | No active games | 12 weeks |
| Simons et al., 2015 [24] | RCT | IG: 134; 13.7 ± 1.3 years CG: 126; 14.1 ± 1.3 years | Home | PlayStation Move (Sport Champions, Move Fitness, Start the Party, Medieval Moves, Dance Star Party and Sorcery) At least one hour a week | None | 40 weeks |
| Graves et al., 2010 [25] | RCT | IG: 22 CG:29 9.2 ± 0.5 years | Home | PlayStation 2 and 3 and Nintendo Wii; jOG packing Unspecified | None | 12 weeks |
| Wagener et al., 2012 [26] | RCT | IG: 21 CG: 20 12–18 years | Clinic | Exergames based on supervised group dance. 3 times a week; 2 × 15’ for the first session; 10’ rest between sets 4 × 15’ for subsequent sessions; 5’ rest between sets | None | 10 weeks |
| Maloney et al., 2012 [27] | RCT | IG: 33; 12.9 ± 2.36 years CG: 31; 11.73 ± 2.38 years | Home | PlayStation 2 (DDR). Average of 89’ per week | None | 12 weeks |
| Staiano et al., 2017 [28] | Original article | IG: 19 girls; 15.3 ± 1.3 years CG: 18 girls; 16.1 ± 1.3 years | Research laboratory | Dance exergaming Kinect for Xbox 360 (Microsoft Corporation, Redmond, WA, USA) Thirty-six 60 min sessions | None | 12 weeks |
| Trost et al., 2014 [18] | Randomized study | IG: 34; 10.1 ± 1.9 years CG: 41; 9.9 ± 1.5 years | Clinic | Kinect and Xbox 360 (Kinect ports) Unspecified | No active games | 16 weeks |
| Maloney et al., 2008 [29] | Pilot study | IG: 40; 7.5 ± 0.5 years CG: 20; 7.6 ± 0.5 years | Home | PlayStation2 game console DDR MAX2 game (Konami of America, Redwood City, CA, USA), 120 min per week of DDR, preferably divided over four sessions | Wait-list control (10-week delay) | 28 weeks |
| Staiano et al., 2018 [30] | RCT | IG: 23 CG: 23 11.2 ± 0.8 years | Home | Kinect and Xbox 360 (Your Shape: Fitness Evolved 2012, Just Dance 3, Disneyland Adventures, and Kinect Sports Season 2) One hour per session, 3 times a week + weekly/bi-weekly video chat sessions with an athletic trainer | None | 24 weeks |
| Liang et al., 2020 [31] | RCT | IG: 30 CG: 57 10.5 ± 0.8 years | School | Xbox 360 Kinect Two 1-h sessions per week. | None | 8 weeks |
| Christison et al., 2012 [32] | Prospective observational pilot study | IG: 48 8–16 years | Home | DDR, exerbike XG, Nintendo Wii 10 weekly 1 h facilitated activity sessions: 5 one-hour exergaming sessions; 5 one-hour combined exergaming/traditional exercise sessions | None | 18 months |
| Author, Year | Outcome | Tool | Results | p-Value |
|---|---|---|---|---|
| Ni Mhurchu et al., 2008 [16] | PA levels | Actigraph e Paq-c | IG more active than CG | Significant |
| Simons et al., 2015 [24] | Energy expenditure | Actigraph | IG > CG | Nonsignificant |
| Graves et al., 2010 [25] | Perceived competence to exercise/relations with parents/self-esteem | Perceived Competence Scale (PCS)/Parent Rating Scales-Adolescent version (PRS-A)/Adolescent Self-Report Scales (SRP-A) | IG had an increase in perceived competence and relationships with parents | Significant |
| Wagener et al., 2012 [26] | Screen time | Actigraph | IG < CG | Significant |
| Maloney et al., 2012 [27] | Total sedentary screen time/self-reported nonactive videogame time | Flemish Physical Activity Computerized Questionnaire (FPACQ) | IG had a reduction in screen time and passive video game participation | Significant |
| Staiano et al., 2017 [28] | PA levels | Actigraph | IG had improved self-efficacy during intervention compared to GC | Non Significant |
| Trost et al., 2014 [18] | Sedentary behavior change | Actigraph | IG had decrease sedentary time compared to GC | Significant |
| Maloney et al., 2008 [29] | Screen time/self-esteem/PA time | Self-perception profile for children (SPPC)/healthy style questionnaire | IG had reduced screen time and increased motor activity hours and self-esteem | Significant |
| Staiano et al., 2018 [30] | PA levels | Actigraph | IG had increased levels of moderate-to-vigorous motor activity compared with CG | Significant |
| Liang et al., 2020 [31] | PA/PA during leisure time/self-efficacy toward PA/screen time/intrinsic motivation | Accelerometry (ActiGraph GT3X+; ActiGraph Inc., FortWalton Beach, FL, USA)/Godin-Shephard Leisure-Time Physical Activity Questionnaire/13-item self-report survey/NHANES/IMI | IG self-reported an increase in PA (p = 0.035) and fewer hours watching television or videos (p = 0.01) after the intervention; significantly improved self-efficacy toward PA (p = 0.028); and highly rated intrinsic motivation toward exergaming. | Significant |
| Christison et al., 2012 [32] | PA/SST (sedentary screen time) | ActiGraph accelerometer (MTI Health Systems, Ft. Walton Beach, FL, USA)/jointly self-reported measure | Increase in vigorous PA and reduction in light PA/decrease in SST of –1.2 ± 3.7 h per week (hpw) | Significant |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Calcaterra, V.; Vandoni, M.; Marin, L.; Carnevale Pellino, V.; Rossi, V.; Gatti, A.; Patanè, P.; Cavallo, C.; Re, F.; Albanese, I.; et al. Exergames to Limit Weight Gain and to Fight Sedentarism in Children and Adolescents with Obesity. Children 2023, 10, 928. https://doi.org/10.3390/children10060928
Calcaterra V, Vandoni M, Marin L, Carnevale Pellino V, Rossi V, Gatti A, Patanè P, Cavallo C, Re F, Albanese I, et al. Exergames to Limit Weight Gain and to Fight Sedentarism in Children and Adolescents with Obesity. Children. 2023; 10(6):928. https://doi.org/10.3390/children10060928
Chicago/Turabian StyleCalcaterra, Valeria, Matteo Vandoni, Luca Marin, Vittoria Carnevale Pellino, Virginia Rossi, Alessandro Gatti, Pamela Patanè, Caterina Cavallo, Fabio Re, Ilaria Albanese, and et al. 2023. "Exergames to Limit Weight Gain and to Fight Sedentarism in Children and Adolescents with Obesity" Children 10, no. 6: 928. https://doi.org/10.3390/children10060928
APA StyleCalcaterra, V., Vandoni, M., Marin, L., Carnevale Pellino, V., Rossi, V., Gatti, A., Patanè, P., Cavallo, C., Re, F., Albanese, I., Silvestri, D., De Nunzio, A., & Zuccotti, G. (2023). Exergames to Limit Weight Gain and to Fight Sedentarism in Children and Adolescents with Obesity. Children, 10(6), 928. https://doi.org/10.3390/children10060928












