Design of a Collaborative Knowledge Framework for Personalised Attention Deficit Hyperactivity Disorder (ADHD) Treatments
Abstract
:1. Introduction
2. Related Work
3. Research Methodology
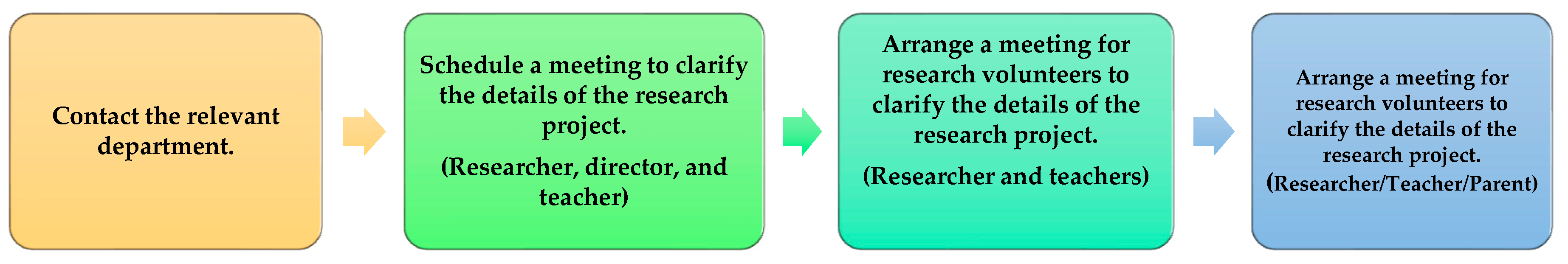
- Ban Rat Niyom School (Jor Prayoon Upatham) was contacted with detailed documents about research work. The documents related to research work were presented to the school’s director.
- After receiving approval from the school’s director, the researcher arranged a meeting to explain the details of the research process, activities, recruitment, and other information related to conducting research for the upcoming project.
- Volunteer recruitment for teachers was conducted. After that, an appointment was made to meet and clarify the research implementation requirements. Documents relevant to the study and the activities to take place were presented throughout the research project.
- The supervised teachers chose students. Then, they sent the parents the participant data sheet and consent letter. If the parents had any doubts regarding student participation, teachers could contact researchers to arrange meetings for clarification.
- (Inclusive criteria for teachers):
- Only homeroom teachers were selected, and they must have the following qualifications.
- The teachers must teach and supervise children of age 6–12 years old who study at the primary level (grade 1–6) at Ban Ratniyom School (Jorprayoon Upatham).
- The teachers have knowledge of and understand information about ADHD in children. They can assess and observe student behaviour in their supervising classes and are able to use a tool to screen behavioural/emotional problems, including the Strengths and Weaknesses Scale (SDQ, Teacher Student Behaviour Assessment Scale).
- (Inclusive criteria for students):
- Students must be 6–12 years old and study at the primary level (grade 1–6) at Ban Rat Niyom School (Jor Prayun Upatham). They are in the class of the teachers under the criteria stated above. The participating teachers selected students for this study.
- (Inclusive criteria for parents):
- Parents of the selected students, who were willing to participate, were included.
- Teachers who cannot participate in activities during the specified period of the research project were excluded.
- Teachers who could not assess and observe students’ behaviours in their supervised classes according to the specified criteria and within the duration of the research project were excluded.
- There were no exclusion criteria for students and parents.
3.1. Design and Development of the Proposed Collaborative Framework
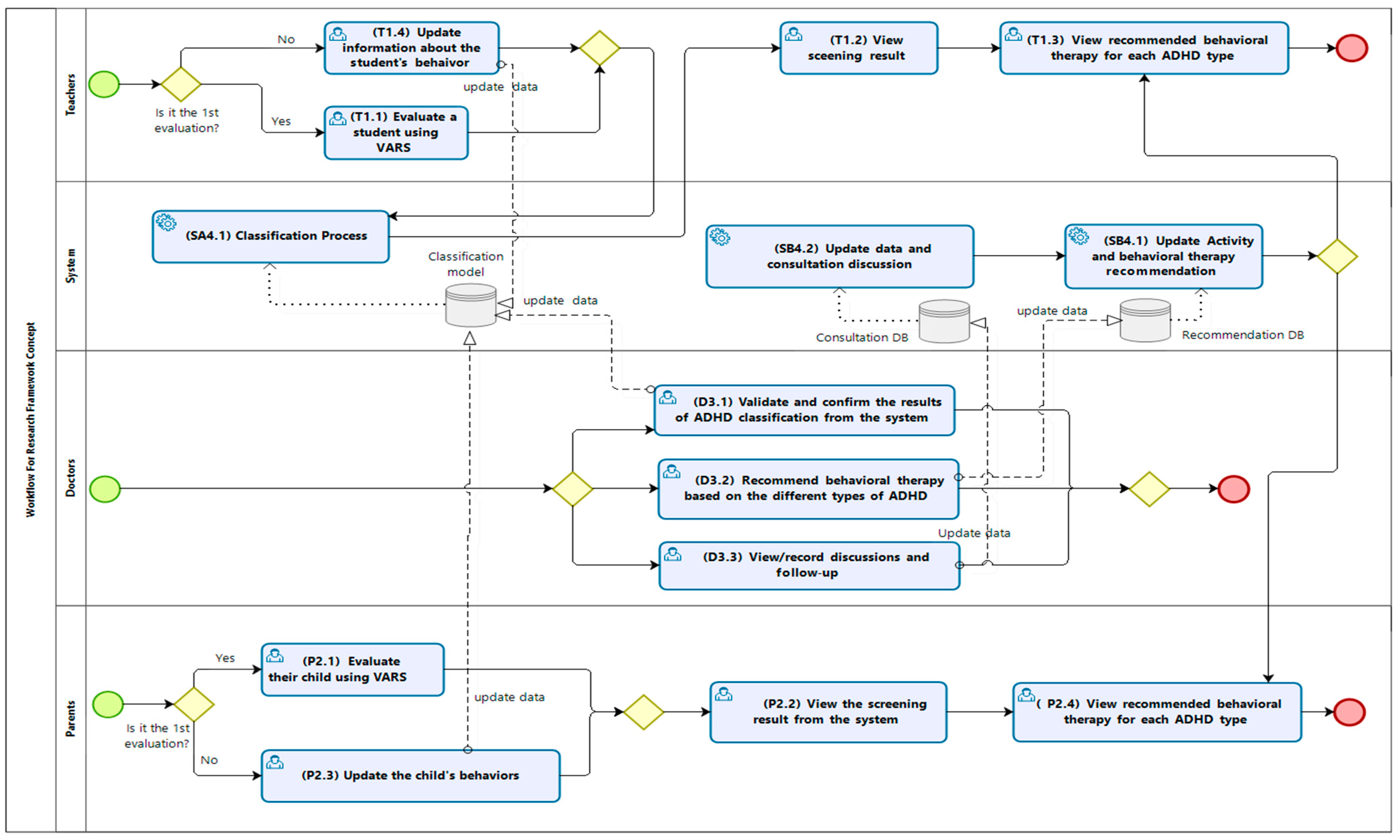
Workflow of the Collaborative Framework
- The role of the teacher was to evaluate students using the VADRS (refer to T1.1 in the framework) and view the screening of the result (T1.2). The teacher could also view the recommended behavioural therapy for each type of ADHD from the system (T1.3). The teacher could consult with the doctor if he/she had any questions about how to apply the therapy or activity based on the recommendations from the system. After the teacher applied some therapies and/or treatment activities to the student, the teacher could update the information about the student’s behaviour in the system for further assessment (T1.4). The updated data would also be used for updating the classification model for improvement.
- The parents could evaluate their child using the same VADRS (P2.1) and view the screening result from the system (P2.2). The parents could update the child’s behaviour in the system for further assessment (P2.3) and view the recommended behavioural therapy for each type of ADHD from the system (P2.4).
- The doctors viewed and confirmed the results of the classification of ADHD that was returned by the system (D3.1) and recommended behavioural therapies based on the different types of ADHD (D3.2). They could view and record the discussions (D3.3) and give the teachers consultation from the system (D3.4) with follow-ups (D3.5).
- Our system consisted of three processes comprising the classification process (SA4.1), the update process for data and consultation discussion (SB4.1), and the update process for the activities and recommendations for behavioural therapy (SB4.2).
3.2. The Classification Process (SA4.1)
- (a)
- Data collection and analysis process
- (b)
- Model generation process
- Set SelectPercentile = N%.
- No. of the remaining attributes ≤ N%.
- Update the set of attributes based on the SelectPercentile.
- Return the attribute selection result.
- (c)
- Prediction process
- (d)
- Verification of the result of the predicted model
3.3. The Activity and Behavioural Therapy Recommendation Process (SB4.1)
- Mix-type is a symptom of the hyperactivity–impulsivity and inattention type of ADHD. The activities for this type focus on organisation and discipline activities (AOCD) and medication activities (AMOD).
- Hyperactivity is a symptom of a hyperactivity–impulsivity type of ADHD. The activities for this type include organisation and discipline activities (AOCD).
- Inattention is a symptom of a lack of concentration. The activities for the children involve increasing concentration (AIC).
- ODD is oppositional defiant disorder ADHD. The activities focus on those that can control behaviour (ACB).
- (a)
- Data collection and algorithm design
- (i)
- Questionnaires, interviews, focus group discussions, and social media were employed to collect the data sources from the parents, teachers, and doctors. This information was determined and used for designing the recommendation process and the algorithm used in the framework.
- (ii)
- (iii)
- We designed an algorithm to provide the appropriate recommendations for behavioural therapy and treatment activities based on the different types of ADHD. The verified information on the behavioural therapy and treatment activities was provided by the doctors, and it was pre-input into the system for the recommendation process.
- (b)
- Review the recommended information and algorithm
- Update data and consultation discussion (SB4.2)
4. Experiments and Results
4.1. Analysis of the Classification Results
4.2. Analysis of the Recommendation Process
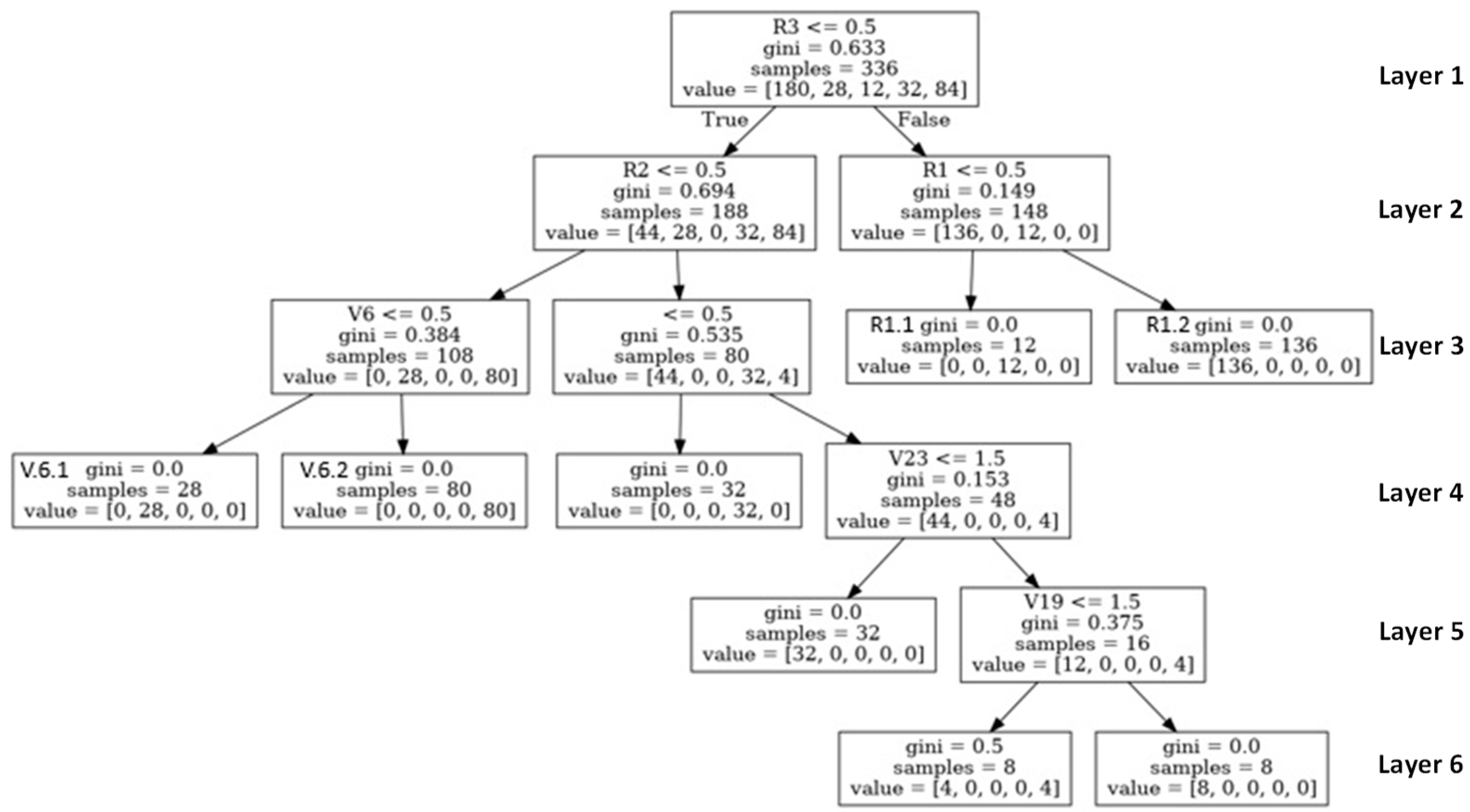
The Decision Tree Graph
- (1).
- The samples parameter is the number of data items compatible with that node, so as the decision moved down the depth of the tree, the number of samples of a node in each layer tended to decrease over time.
- (2).
- Gini indicates the “purity” of a node. Where Gini = 0, this infers that all the data items in the node belong to the same class. In comparison, Gini = 0.5 indicates that the data items in the node belong to two similar types, which represent the values, such as the value of R1 = [136, 0, 12 0, 0] in the child node to the right of the root node. This infers the 148 entries of 15 at this node condition. If the answer was false (child node left R1) and the value was [0, 0, 12, 0, 0], there would be 12 entries in the ODD classification. However, if the answer was true and the value was [136, 0, 0, 0, 0] (child node right R1), there would be 136 entries in the mix-type classification. This assumes that the data meeting this node’s condition is in the ODD and mix-type classifications.
- (3).
- Value is used to indicate the class of the predicted activities by the types of ADHD. The activities of the five classes were mix-type (index [0]), non-ADHD (index [1]), ODD (index [2]), hyperactivity (index [3]), and inattention (index [4]).
5. Discussion and Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Al-Ghannami, S.S.; Al-Adawi, S.; Ghebremeskel, K.; Cramer, M.T.; Hussein, I.S.; Min, Y.; Jeyaseelan, L.; Al-Sibani, N.; Al-Shammakhi, S.M.; Al-Mamari, F.; et al. Attention Deficit Hyperactivity Disorder and Parental Factors in School Children Aged Nine to Ten Years in Muscat, Oman. Oman Med. J. 2018, 33, 193–199. [Google Scholar] [CrossRef] [PubMed]
- Posner, J.; Polanczyk, G.V.; Sonuga-Barke, E. Attention-deficit hyperactivity disorder. Lancet 2020, 395, 450–462. [Google Scholar] [CrossRef]
- Rohde, L.; Buitelaar, J.K.; Gerlach, M.; Faraone, S.V.; Coghill, D. The world federation of ADHD guide. Porto Alegre Artmed 2019, 66–70. [Google Scholar]
- Swanson, J.M.; Wigal, T.; Lakes, K. DSM-V and the future diagnosis of attention-deficit/hyperactivity disorder. Curr. Psychiatry Rep. 2009, 11, 399–406. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Association: Washington, DC, USA, 2013. [Google Scholar]
- Sonne, T.; Marshall, P.; Obel, C.; Thomsen, P.H.; Grønbæk, K. An assistive technology design framework for ADHD. In Proceedings of the 28th Australian Conference on Computer-Human Interaction–OzCHI’16, Launceston, Australia, 29 November–2 December 2016. [Google Scholar]
- Dreyer, B.P. The Diagnosis and Management of Attention-Deficit/Hyperactivity Disorder in Preschool Children: The State of Our Knowledge and Practice. Curr. Probl. Pediatr. Adolesc. Health Care 2006, 36, 6–30. [Google Scholar] [CrossRef]
- Gallo, E.F.; Posner, J. Moving towards causality in attention-deficit hyperactivity disorder: Overview of neural and genetic mechanisms. Lancet Psychiatry 2016, 3, 555–567. [Google Scholar] [CrossRef] [Green Version]
- Sibley, M.H.; Pelham Jr, W.E.; Molina, B.S.; Gnagy, E.M.; Waschbusch, D.A.; Garefino, A.C.; Kuriyan, A.B.; Babinski, D.E.; Karch, K.M. Diagnosing ADHD in adolescence. J. Consult. Clin. Psychol. 2012, 80, 139. [Google Scholar] [CrossRef] [Green Version]
- Jain, R.A. To Study the Attention Deficit Hyperactivity Disorder (ADHD) and to Evaluate the Cognitive, Hyperactive and Impulsive Behavior against 6-OHDA Hbr Lesioned Sprague Dawley Neonates Using Hyperaxe, Curcumin & Quercetin; CL Baid Metha College of Pharmacy: Chennai, India, 2017. [Google Scholar]
- Kalaman, C.R.; Ibrahim, N.; Shaker, V.; Cham, C.Q.; Ho, M.C.; Visvalingam, U.; Shahabuddin, F.A.; Rahman, F.N.A.; Halim, M.R.T.A.; Kaur, M.; et al. Parental Factors Associated with Child or Adolescent Medication Adherence: A Systematic Review. Healthcare 2023, 11, 501. [Google Scholar] [CrossRef]
- Mick, E.; Biederman, J.; Faraone, S.V.; Sayer, J.; Kleinman, S. Case-Control Study of Attention-Deficit Hyperactivity Disorder and Maternal Smoking, Alcohol Use, and Drug Use During Pregnancy. J. Am. Acad. Child Adolesc. Psychiatry 2002, 41, 378–385. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Perrin, J.M.; Stein, M.T.; Amler, R.W.; Blondis, T.A.; Feldman, H.; Meyer, B.; Shaywitz, B.; Wolraich, M. Clinical practice guideline: Treatment of the school-aged child with attention-deficit/hyperactivity disorder. Pediatrics 2001, 108, 1033–1044. [Google Scholar]
- Wender, P.H.; Tomb, D.A. Attention-Deficit Hyperactivity Disorder in Adults: An Overview. Atten.-Deficit Hyperact. Disord. (ADHD) Adults 2010, 176, 258447. [Google Scholar] [CrossRef]
- Alamuti, E. Mohammadi, M.R. Comparison of Child and Parent Cognitive Behaviour Therapy on Reduction of Attention Deficit Hyperactivity Disorder Symptoms in Children. J. Child Adolesc. Behav. 2016, 4, 285. [Google Scholar] [CrossRef]
- Chu, S. Occupational Therapy for Children with Attention Deficit Hyperactivity Disorder: A Survey on the Level of Involvement and Training Needs of Therapists. Br. J. Occup. Ther. 2003, 66, 209–218. [Google Scholar] [CrossRef]
- Barbaresi, W.J.; Colligan, R.C.; Weaver, A.L.; Voigt, R.G.; Killian, J.M.; Katusic, S.K.; Chawla, A.; Sprinz, P.G.; Welch, J.; Heeney, M.; et al. Mortality, ADHD, and Psychosocial Adversity in Adults With Childhood ADHD: A Prospective Study. Pediatrics 2013, 131, 637–644. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Fogler, J.M.; Weaver, A.L.; Katusic, S.; Voigt, R.G.; Barbaresi, W.J. Recalled Experiences of Bullying and Victimization in a Longitudinal, Population-Based Birth Cohort: The Influence of ADHD and Co-Occurring Psychiatric Disorder. J. Atten. Disord. 2020, 26, 15–24. [Google Scholar] [CrossRef] [PubMed]
- Singh, I. A Framework for Understanding Trends in ADHD Diagnoses and Stimulant Drug Treatment: Schools and Schooling as a Case Study. Biosocieties 2006, 1, 439–452. [Google Scholar] [CrossRef]
- Lahey, B.B.; Pelham, W.E.; Loney, J.; Lee, S.S.; Willcutt, E. Instability of the DSM-IV Subtypes of ADHD From Preschool through Elementary School. Arch. Gen. Psychiatry 2005, 62, 896–902. [Google Scholar] [CrossRef]
- Paholpak, S.; Arunpongpaisal, S.; Krisanaprakornkit, T.; Khiewyoo, J. Validity and reliability study of the Thai version of WHO schedules for clinical assessment in neuropsychiatry: Sections on psychotic disorders. J. Med. Assoc. Thail. 2008, 91, 408. [Google Scholar]
- Minor, E.C.; Porter, A.C.; Murphy, J.; Goldring, E.B.; Cravens, X.; Elloitt, S.N. A known group analysis validity study of the Vanderbilt Assessment of Leadership in Education in US elementary and secondary schools. Educ. Assess. Eval. Acc. 2014, 26, 29–48. [Google Scholar] [CrossRef]
- Health, M.O.P. Thai Children are more likely to Have ADHD than One Year ago. 2008. Available online: https://www.dmh.go.th/newsdmh/ (accessed on 27 March 2023).
- Choopun, K.; Boonlue, N. Attention Deficit Hyperactivity Disorder in Primary School Chiang Mai, Thailand. Int. J. Child Dev. Ment. Health 2022, 10. [Google Scholar]
- Ayano, G.; Yohannes, K.; Abraha, M. Epidemiology of attention-deficit/hyperactivity disorder (ADHD) in children and ado-lescents in Africa: A systematic review and meta-analysis. Ann. Gen. Psychiatry 2020, 19, 21. [Google Scholar] [CrossRef] [Green Version]
- Danielson, M.L.; Bitsko, R.H.; Ghandour, R.M.; Holbrook, J.R.; Kogan, M.D.; Blumberg, S.J. Prevalence of Parent-Reported ADHD Diagnosis and Associated Treatment Among U.S. Children and Adolescents, 2016. J. Clin. Child Adolesc. Psychol. 2018, 47, 199–212. [Google Scholar] [CrossRef]
- Hoang, H.H.; Tran, A.T.N.; Nguyen, V.H.; Nguyen, T.T.B.; Le, D.D.; Jatho, A.; Onchonga, D.; Van Duong, T.; Nguyen, M.T.; Tran, B.T. Attention Deficit Hyperactivity Disorder (ADHD) and Associated Factors Among First-Year Elementary School Students. J. Multidiscip. Health 2021, 14, 997–1005. [Google Scholar] [CrossRef] [PubMed]
- Rissanen, M. Translational health technology and system schemes: Enhancing the dynamics of health informatics. Health Inf. Sci. Syst. 2020, 8, 39. [Google Scholar] [CrossRef] [PubMed]
- Albahar, F.; Abu-Farha, R.K.; Alshogran, O.Y.; Alhamad, H.; Curtis, C.E.; Marriott, J.F. Healthcare Professionals’ Perceptions, Barriers, and Facilitators towards Adopting Computerised Clinical Decision Support Systems in Antimicrobial Stewardship in Jordanian Hospitals. Healthcare 2023, 11, 836. [Google Scholar] [CrossRef]
- De Silva, S.; Dayarathna, S.; Ariyarathne, G.; Meedeniya, D.; Jayarathna, S.; Michalek, A.M.P. Computational Decision Support System for ADHD Identification. Int. J. Autom. Comput. 2020, 18, 233–255. [Google Scholar] [CrossRef]
- Bard, D.E.; Wolraich, M.L.; Neas, B.; Doffing, M.; Beck, L. The Psychometric Properties of the Vanderbilt Attention-Deficit Hyperactivity Disorder Diagnostic Parent Rating Scale in a Community Population. J. Dev. Behav. Pediatr. 2013, 34, 72–82. [Google Scholar] [CrossRef]
- Becker, S.P.M.; Langberg, J.M.; Vaughn, A.J.; Epstein, J.N. Clinical Utility of the Vanderbilt ADHD Diagnostic Parent Rating Scale Comorbidity Screening Scales. J. Dev. Behav. Pediatr. 2012, 33, 221–228. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kądziela-Olech, H. The measurement of the symptoms of ADHD in the NICHQ Vanderbilt Assessment Scale for Parent (VADPRS) and for Teacher (VADTRS). Psychiatr. I Psychol. Klin. 2014, 14, 277–283. [Google Scholar] [CrossRef]
- Murphy, J.F.; Goldring, E.B.; Cravens, X.C.; Elliott, S.N.; Porter, A.C. The Vanderbilt assessment of leadership in education: Measuring learning-centered leadership. J. East China Norm. Univ. 2007, 29, 1–10. [Google Scholar]
- Porter, A.C.; Polikoff, M.S.; Goldring, E.B.; Murphy, J.; Elliott, S.N.; May, H. Investigating the Validity and Reliability of the Vanderbilt Assessment of Leadership in Education. Elem. Sch. J. 2010, 111, 282–313. [Google Scholar] [CrossRef]
- Saputra, D.C.E.; Sunat, K.; Ratnaningsih, T. A New Artificial Intelligence Approach Using Extreme Learning Machine as the Potentially Effective Model to Predict and Analyze the Diagnosis of Anemia. Healthcare 2023, 11, 697. [Google Scholar] [CrossRef] [PubMed]
- Ferdous, M.; Debnath, J.; Chakraborty, N.R. Machine Learning Algorithms in Healthcare: A Literature Survey. In Proceedings of the 2020 11th International Conference on Computing, Communication and Networking Technologies (ICCCNT), Kharagpur, India, 1–3 July 2020. [Google Scholar] [CrossRef]
- Shobana, G.; Umamaheswari, K. Prediction of Liver Disease using Gradient Boost Machine Learning Techniques with Feature Scaling. In Proceedings of the 2021 5th International Conference on Computing Methodologies and Communication (ICCMC), Erode, India, 8–10 April 2021; IEEE: Piscataway Township, NJ, USA; pp. 1223–1229. [Google Scholar] [CrossRef]
- Zahoor, S.; Shoaib, U.; Lali, I.U. Breast Cancer Mammograms Classification Using Deep Neural Network and Entropy-Controlled Whale Optimization Algorithm. Diagnostics 2022, 12, 557. [Google Scholar] [CrossRef] [PubMed]
- Dashtipour, K.; Taylor, W.; Ansari, S.; Zahid, A.; Gogate, M.; Ahmad, J.; Assaleh, K.; Arshad, K.; Imran, M.A.; Abbasi, Q. Detecting Alzheimer’s disease using machine learning methods. In Proceedings of the Body Area Networks. Smart IoT and Big Data for Intelligent Health Management: 16th EAI International Conference, BODYNETS 2021, Virtual Event, 25–26 October 2021; Springer: Berlin/Heidelberg, Germany, 2022; pp. 89–100. [Google Scholar]
- Krishnaveni, K.; Radhamani, E. Diagnosis and evaluation of ADHD using Naïve Bayes and J48 classifiers. In Proceedings of the 2016 3rd International Conference on Computing for Sustainable Global Development (INDIACom), New Delhi, India, 16–18 March 2016; IEEE: Piscataway Township, NJ, USA; pp. 1809–1814. [Google Scholar]
- Kuang, D.; He, L. Classification on ADHD with Deep Learning. In Proceedings of the 2014 International Conference on Cloud Computing and Big Data, Wuhan, China, 12–14 November 2014. [Google Scholar]
- Oztoprak, H.; Toycan, M.; Alp, Y.K.; Arikan, O.; Dogutepe, E.; Karakas, S. Machine-based learning system: Classification of ADHD and non-ADHD participants. In Proceedings of the 2017 25th Signal Processing and Communications Applications Conference (SIU), Antalya, Turkey, 15–18 May 2017; IEEE: Piscataway Township, NJ, USA; pp. 1–4. [Google Scholar] [CrossRef]
- Miao, B.; Zhang, Y. A feature selection method for classification of ADHD. In Proceedings of the 2017 4th International Conference on Information, Cybernetics and Computational Social Systems (ICCSS), Dalian, China, 24–26 July 2017; IEEE: Piscataway Township, NJ, USA; pp. 21–25. [Google Scholar] [CrossRef]
- Khanna, S.; Das, W. A Novel Application for the Efficient and Accessible Diagnosis of ADHD Using Machine Learning. In Proceedings of the 2020 IEEE/ITU International Conference on Artificial Intelligence for Good (AI4G), Geneva, Switzerland, 21–25 September 2020; IEEE: Piscataway Township, NJ, USA; pp. 51–54. [Google Scholar] [CrossRef]
- Peng, J.; Debnath, M.; Biswas, A.K. Efficacy of novel Summation-based Synergetic Artificial Neural Network in ADHD diagnosis. Mach. Learn. Appl. 2021, 6, 100120. [Google Scholar] [CrossRef]
- Cordova, M.; Shada, K.; Demeter, D.V.; Doyle, O.; Miranda-Dominguez, O.; Perrone, A.; Schifsky, E.; Graham, A.; Fombonne, E.; Langhorst, B.; et al. Heterogeneity of executive function revealed by a functional random forest approach across ADHD and ASD. NeuroImage Clin. 2020, 26, 102245. [Google Scholar] [CrossRef]
- Radhamani, E.; Krishnaveni, K. Diagnosis and Evaluation of ADHD using MLP and SVM Classifiers. Indian J. Sci. Technol. 2016, 9, 93853. [Google Scholar] [CrossRef] [Green Version]
- Parashar, A.; Kalra, N.; Singh, J.; Goyal, R.K. Machine Learning Based Framework for Classification of Children with ADHD and Healthy Controls. Intell. Autom. Soft Comput. 2021, 28, 669–682. [Google Scholar] [CrossRef]
- Shao, L.; Xu, Y.; Fu, D. Classification of ADHD with bi-objective optimization. J. Biomed. Informatics 2018, 84, 164–170. [Google Scholar] [CrossRef]
- Felt, B.T.; Biermann, B.; Christner, J.G.; Kochhar, P.; Van Harrison, R. Diagnosis and management of ADHD in children. Am. Fam. Physician 2014, 90, 456–464. [Google Scholar]
- Pfiffner, L.J.; Mikami, A.Y.; Huang-Pollock, C.; Easterlin, B.; Zalecki, C.; McBurnett, K. A randomized, controlled trial of integrated home-school behavioral treatment for ADHD, predominantly inattentive type. J. Am. Acad. Child Adolesc. Psychiatry 2007, 46, 1041–1050. [Google Scholar] [CrossRef]
- McVoy, M.; Findling, R.L. Clinical Manual of Child and Adolescent Psychopharmacology; American Psychiatric Pub: Washington, DC, USA, 2017. [Google Scholar]
- Sokolova, M.; Lapalme, G. A systematic analysis of performance measures for classification tasks. Inf. Process. Manag. 2009, 45, 427–437. [Google Scholar] [CrossRef]
| No | Classification Technique | Description | Pros | Cons |
|---|---|---|---|---|
| 1 | Decision Tree | A Decision Tree is a supervised learning technique that can be used for both classification and regression problems, but mostly it is preferred for solving classification problems. |
|
|
| 2 | Naïve Bay | The KNN algorithm classifies data by comparing information of interest to others. The algorithm returns a result based on the information that is most similar to the information of interest. |
|
|
| 3 | KNN | The Naive Bay algorithm is a data mining classifier. The technique was developed based on the principle of Probably Naïve Bayesian Classification. It is used to analyze the probability of an unprecedented event from occurred events. |
|
|
| 4 | Neural Network | This algorithm is one of the data mining techniques. It is a mathematical model for processing information with a connected computation (Connectionist). The algorithm is used to simulate the functioning of neural networks in the human brain to create a tool capable of learning pattern recognition, knowledge extraction (Knowledge Extraction), and the human brain capabilities. |
|
|
| No | ADHD Type | Activities | Description | Example for Activities |
|---|---|---|---|---|
| 1 | Mix-type | AOCD and AMOD | Organization and Discipline Activities and Medication Activities | Play toys or games that require concentration. Training the child to play with one toy at a time will help the child to concentrate on playing longer and Listen—play good music for concentration. |
| 2 | hyperactivity | AOCD | Activities Organization/Discipline Activities | Activities that require calmness, such as building blocks of wood or making towers of coins, Feed the eggs with a spoon. |
| 3 | inattention | AMOD | Activities Medication Activities | Activities that use distance, such as throwing a ball into the basket, threading the needle, stringing the beads, or stringing the garland, |
| 4 | ODD | ACB | Activities Control Behavioral | Create a daily schedule of activities, such as doing homework before play. |
| 5 | Non-ADHD | NO-Activities | Non-ADHD | General activities that increase concentration, such as reading stories. |
| No | Type of ADHD | Data | Number of Data | % | All Data |
|---|---|---|---|---|---|
| 0 | Mix -Type | train | 188 | 80 | 235 |
| test | 47 | 20 | |||
| 1 | Non-ADHD | train | 28 | 80 | 35 |
| test | 7 | 20 | |||
| 2 | ODD | train | 12 | 80 | 15 |
| test | 3 | 20 | |||
| 3 | hyperactivity | train | 32 | 80 | 40 |
| test | 8 | 20 | |||
| 4 | inattention | train | 76 | 80 | 95 |
| test | 19 | 20 |
| No | Type of ADHD | Test | Decision Tree | KNN | Naive Bayes | Neural Network | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Cor | % | Inc | % | Cor | % | Inc | % | Cor | % | Inc | % | Cor | % | Inc | % | |||
| 0 | Mix-type | 47 | 46 | 97.87 | 1 | 2.13 | 44 | 93.62 | 3 | 6.38 | 34 | 72.34 | 13 | 27.66 | 46 | 97.87 | 1.00 | 2.13 |
| 1 | Non-ADHD | 7 | 7 | 100.00 | 0 | 0.00 | 7 | 100.00 | 0 | 0.00 | 7 | 100.00 | 0 | 0.00 | 7 | 100.00 | 0.00 | 0.00 |
| 2 | ODD | 3 | 3 | 100.00 | 0 | 0.00 | 3 | 100.00 | 0 | 0.00 | 3 | 100.00 | 0 | 0.00 | 3 | 100.00 | 0.00 | 0.00 |
| 3 | hyperactivity | 8 | 8 | 100.00 | 0 | 0.00 | 8 | 100.00 | 0 | 0.00 | 8 | 100.00 | 0 | 0.00 | 8 | 100.00 | 0.00 | 0.00 |
| 4 | inattention | 19 | 19 | 100.00 | 0 | 0.00 | 19 | 100.00 | 0 | 0.00 | 19 | 100.00 | 0 | 0.00 | 19 | 100.00 | 0.00 | 0.00 |
| Total (case) | 84 | 99.57 | 0.43 | 98.72 | 1.28 | 94.47 | 5.53 | 99.57 | 0.43 | |||||||||
| % Total Cases | 99.57 | 98.72 | 94.47 | 99.57 | ||||||||||||||
| No | Type of ADHD | Decision Tree | KNN | Naive Bayes | Neural Network | ||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| TPR | TNR | PR | RC | AC | F1 | TPR | TNR | PR | RC | AC | F1 | TPR | TNR | PR | RC | AC | F1 | TPR | TNR | PR | RC | AC | F1 | ||
| 0 | Mix-type | 0.98 | 0 | 1 | 0.98 | 0.99 | 0.99 | 0.94 | 0 | 1 | 0.94 | 0.96 | 0.97 | 0.72 | 0 | 1 | 0.72 | 0.85 | 0.84 | 0.98 | 0 | 1 | 0.98 | 0.99 | 0.99 |
| 1 | Non-ADHD | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 |
| 2 | ODD | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 |
| 3 | hyperactivity | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 1 | 0 | 1 | 1 | 1 | 1 |
| 4 | inattention | 1 | 0.02 | 0.95 | 1 | 0.99 | 0.97 | 1 | 0.05 | 0.86 | 1 | 0.96 | 0.93 | 1 | 0.2 | 0.59 | 1 | 0.85 | 0.75 | 1 | 0.02 | 0.95 | 1 | 0.99 | 0.97 |
| Average Accuracy | 0.996 | 0.984 | 0.94 | 0.996 | |||||||||||||||||||||
| No. | Computation Time | |
|---|---|---|
| Decision Tree Model | Neural Network | |
| 1 | 0.031229 | 1.040929 |
| 2 | 0.055537 | 1.110908 |
| 3 | 0.061133 | 1.175104 |
| 4 | 0.051996 | 2.634261 |
| 5 | 0.074594 | 1.068259 |
| 6 | 0.052359 | 1.24145 |
| 7 | 0.050016 | 1.313238 |
| 8 | 0.047997 | 1.392138 |
| 9 | 0.073211 | 1.600991 |
| 10 | 0.078132 | 2.092879 |
| 11 | 0.058697 | 1.389741 |
| 12 | 0.057674 | 1.334164 |
| 13 | 0.062324 | 1.848112 |
| 14 | 0.082012 | 1.639582 |
| 15 | 0.091128 | 1.899683 |
| 16 | 0.070998 | 1.397739 |
| 17 | 0.044996 | 1.257645 |
| 18 | 0.058901 | 1.204572 |
| 19 | 0.045997 | 1.127632 |
| 20 | 0.056571 | 1.180286 |
| 21 | 0.049337 | 1.2724 |
| 22 | 0.063612 | 1.046959 |
| 23 | 0.064478 | 1.25124 |
| 24 | 0.063231 | 1.501523 |
| 25 | 0.063992 | 3.656594 |
| 26 | 0.083996 | 1.15601 |
| 27 | 0.058533 | 1.216549 |
| 28 | 0.050994 | 1.071333 |
| 29 | 0.048935 | 1.203264 |
| 30 | 0.048 | 1.352984 |
| 31 | 0.047018 | 1.296979 |
| 32 | 0.081719 | 1.195881 |
| 33 | 0.045019 | 1.038161 |
| 34 | 0.052759 | 1.117537 |
| 35 | 0.048993 | 1.120578 |
| 36 | 0.063812 | 1.11737 |
| 37 | 0.053889 | 1.229534 |
| 38 | 0.054619 | 1.55222 |
| 39 | 0.050994 | 1.119644 |
| 40 | 0.060458 | 1.255233 |
| 41 | 0.051103 | 1.493202 |
| 42 | 0.050003 | 1.005049 |
| 43 | 0.05909 | 1.304165 |
| 44 | 0.052995 | 1.251586 |
| 45 | 0.061735 | 1.457659 |
| 46 | 0.050007 | 1.086125 |
| 47 | 0.052067 | 1.379029 |
| 48 | 0.051687 | 1.133587 |
| 49 | 0.050996 | 1.049925 |
| 50 | 0.044999 | 1.177412 |
| 51 | 0.064901 | 1.06846 |
| 52 | 0.056602 | 0.970769 |
| 53 | 0.051998 | 1.345009 |
| 54 | 0.046708 | 1.189245 |
| 55 | 0.047584 | 1.125525 |
| 56 | 0.089003 | 1.555476 |
| 57 | 0.0625 | 2.134213 |
| 58 | 0.086094 | 2.15842 |
| 59 | 0.068346 | 1.812286 |
| 60 | 0.059886 | 1.31289 |
| 61 | 0.0644 | 1.274483 |
| 62 | 0.053056 | 1.663544 |
| 63 | 0.077142 | 1.632083 |
| 64 | 0.084134 | 2.141111 |
| 65 | 0.074552 | 1.464199 |
| 66 | 0.057663 | 1.094026 |
| 67 | 0.048291 | 1.640016 |
| 68 | 0.044992 | 1.486279 |
| 69 | 0.049449 | 1.069333 |
| 70 | 0.046227 | 1.450437 |
| 71 | 0.063584 | 1.509127 |
| 72 | 0.075065 | 1.465219 |
| 73 | 0.047998 | 1.345517 |
| 74 | 0.047002 | 1.229406 |
| 75 | 0.056996 | 1.622626 |
| 76 | 0.048608 | 1.10312 |
| 77 | 0.046375 | 1.286845 |
| 78 | 0.047895 | 1.19502 |
| 79 | 0.054994 | 1.117199 |
| 80 | 0.074998 | 1.395097 |
| 81 | 0.05399 | 1.271263 |
| 82 | 0.053778 | 1.882056 |
| 83 | 0.065562 | 1.208384 |
| 84 | 0.055619 | 1.22781 |
| 85 | 0.047999 | 1.047544 |
| 86 | 0.048203 | 1.251664 |
| 87 | 0.04885 | 1.160577 |
| 88 | 0.050631 | 0.874186 |
| 89 | 0.055177 | 1.260275 |
| 90 | 0.049021 | 1.201123 |
| 91 | 0.044018 | 1.254685 |
| 92 | 0.046995 | 1.244649 |
| 93 | 0.047016 | 1.05943 |
| 94 | 0.052024 | 0.944234 |
| 95 | 0.042279 | 1.299954 |
| 96 | 0.059698 | 1.503714 |
| 97 | 0.047133 | 1.13383 |
| 98 | 0.060916 | 1.063454 |
| 99 | 0.047019 | 0.98657 |
| 100 | 0.05708 | 1.087645 |
| Average computation time | 0.057146 | 1.348791 |
| No | Type of ADHD | Decision Tree | |||||
|---|---|---|---|---|---|---|---|
| TPR | TNR | PR | RC | AC | F1 | ||
| 0 | Mix-type (AOCD + AMOD + ACB) | 0.98 | 0 | 1 | 0.98 | 0.99 | 0.99 |
| 1 | hyperactivity (AOCD) | 1 | 0 | 1 | 1 | 1 | 1 |
| 2 | inattention (AIC) | 1 | 0 | 1 | 1 | 1 | 1 |
| 3 | ODD (ACB) | 1 | 0 | 1 | 1 | 1 | 1 |
| 4 | Non-ADHD (No) | 1 | 0.02 | 0.95 | 1 | 0.99 | 0.97 |
| Accuracy average | 0.996 | ||||||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Chatpreecha, P.; Usanavasin, S. Design of a Collaborative Knowledge Framework for Personalised Attention Deficit Hyperactivity Disorder (ADHD) Treatments. Children 2023, 10, 1288. https://doi.org/10.3390/children10081288
Chatpreecha P, Usanavasin S. Design of a Collaborative Knowledge Framework for Personalised Attention Deficit Hyperactivity Disorder (ADHD) Treatments. Children. 2023; 10(8):1288. https://doi.org/10.3390/children10081288
Chicago/Turabian StyleChatpreecha, Pornsiri, and Sasiporn Usanavasin. 2023. "Design of a Collaborative Knowledge Framework for Personalised Attention Deficit Hyperactivity Disorder (ADHD) Treatments" Children 10, no. 8: 1288. https://doi.org/10.3390/children10081288





