Feasibility and Effectiveness of Speech Intervention Implemented with a Virtual Reality System in Children with Developmental Language Disorders: A Pilot Randomized Control Trial
Abstract
:1. Introduction
2. Materials and Methods
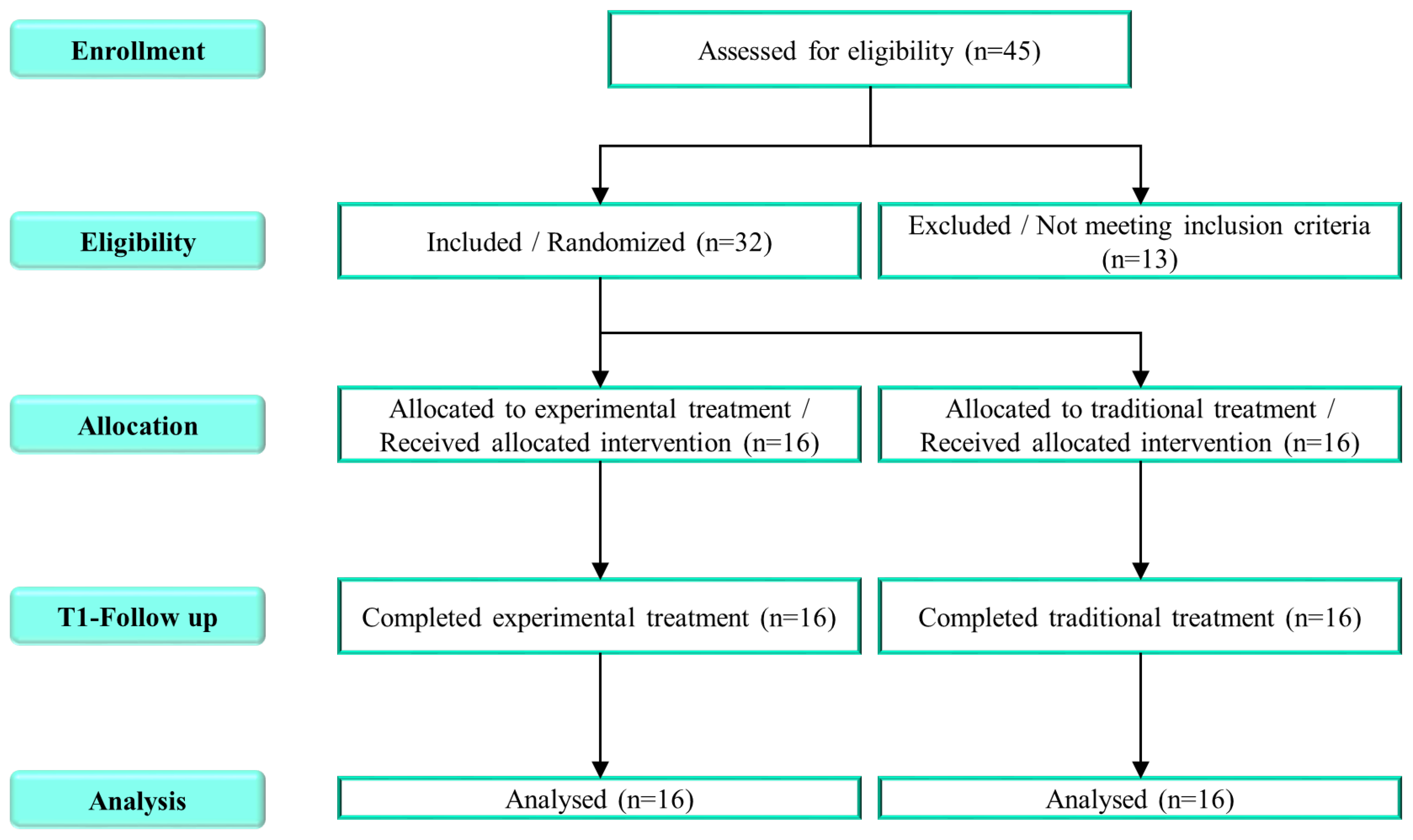
2.1. Population and Study Design
2.2. Neuropsychological Assessment
2.3. Intervention
2.4. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Publishing: Washington, DC, USA, 2013.
- Chilosi, A.M.; Brovedani, P.; Cipriani, P.; Casalini, C. Sex differences in early language delay and in developmental language disorder. J. Neurosci. Res. 2023, 101, 654–667. [Google Scholar] [CrossRef]
- Norbury, C.F.; Gooch, D.; Baird, G.; Charman, T.; Simonoff, E.; Pickles, A. Younger children experience lower levels of language competence and academic progress in the first year of school: Evidence from a population study. J. Child Psychol. Psychiatry 2016, 57, 65–73. [Google Scholar] [CrossRef] [Green Version]
- Tomblin, J.B.; Smith, E.; Zhang, X. Epidemiology of specific language impairment: Prenatal and perinatal risk factors. J. Commun. Disord. 1997, 30, 325–343. [Google Scholar] [CrossRef]
- Sharp, H.M.; Hillenbrand, K. Speech and language development and disorders in children. Pediatr. Clin. N. Am. 2008, 55, 1159–1173. [Google Scholar] [CrossRef] [PubMed]
- Fisher, E.L. A Systematic Review and Meta-Analysis of Predictors of Expressive-Language Outcomes Among Late Talkers. J. Speech Lang. Hear. Res. 2017, 60, 2935–2948. [Google Scholar] [CrossRef]
- Friend, M.; Schmitt, S.A.; Simpson, A.M. Evaluating the predictive validity of the computerized comprehension task: Comprehension predicts production. Dev. Psychol. 2012, 48, 136–148. [Google Scholar] [CrossRef] [PubMed]
- Feldman, H.M. How young children learn language and speech. Pediatr. Rev. 2019, 40, 398–411. [Google Scholar] [CrossRef] [PubMed]
- Redmond, S.M. Clinical intersections among idiopathic language disorder, social (pragmatic) communication disorder, and attention-deficit/hyperactivity disorder. J. Speech Lang. Hear. Res. 2020, 63, 3263–3276. [Google Scholar] [CrossRef]
- Yew, S.G.K.; O’Kearney, R. Emotional and behavioural outcomes later in childhood and adolescence for children with specific language impairments: Meta-analyses of controlled prospective studies. J. Child. Psychol. Psychiatry 2013, 54, 516–524. [Google Scholar] [CrossRef] [PubMed]
- O’Hare, A. Wayward words and watchful waiting: Should clinicians be more proactive for the preschooler with ‘uncomplicated’ expressive language delay? Arch Dis. Child 2009, 94, 80–82. [Google Scholar] [CrossRef]
- Desmarais, C.; Sylvestre, A.; Meyer, F.; Bairati, I.; Rouleau, N. Three profiles of language abilities in toddlers with an expressive vocabulary delay: Variations on a theme. J. Speech Lang. Hear. Res. 2010, 53, 699–709. [Google Scholar] [CrossRef]
- Young, A.R.; Beitchman, J.H.; Johnson, C.; Douglas, L.; Atkinson, L.; Escobar, M.; Wilson, B. Young adult academic outcomes in a longitudinal sample of early identified language impaired and control children. J. Child Psychol. Psychiatry 2002, 43, 635–645. [Google Scholar] [CrossRef]
- Conti-Ramsden, G.; Botting, N. Emotional health in adolescents with and without a history of specific language impairment (SLI). J. Child Psychol. Psychiatry 2008, 49, 516–525. [Google Scholar] [CrossRef]
- Law, J.; Rush, R.; Schoon, I.; Parsons, S. Modeling developmental language difficulties from school entry into adulthood: Literacy, mental health, and employment outcomes. J. Speech Lang. Hear. Res. 2009, 52, 1401–1416. [Google Scholar] [CrossRef] [Green Version]
- O’Hare, A.; Bremner, L. Management of developmental speech and language disorders: Part 1. Arch. Dis. Child. 2016, 101, 272–277. [Google Scholar] [CrossRef]
- Ebbels, S.H.; McCartney, E.; Slonims, V.; Dockrell, J.E.; Norbury, C.F. Evidence-based pathways to intervention for children with language disorders. International. J. Lang. Commun. Disord. 2019, 54, 3–19. [Google Scholar] [CrossRef]
- Lowe, H.; Henry, L.; Joffe, V.L. The Effectiveness of Classroom Vocabulary Intervention for Adolescents with Language Disorder. J. Speech Lang. Hear. Res. 2019, 62, 2829–2846. [Google Scholar] [CrossRef] [PubMed]
- Martins, S.; Cavaco, S. Customizable Serious Speech Therapy Games with Dynamic Difficulty Adjustment for Children with Sigmatism. MEDINFO 2022, 2021, 924–928. [Google Scholar]
- De Luca, R.; Calabrò, R.S.; Bramanti, P. Cognitive rehabilitation after severe acquired brain injury: Current evidence and future directions. Neuropsychol. Rehabil. 2018, 28, 879–898. [Google Scholar] [CrossRef]
- Moreno, J.M.M.; Sánchez, J.S.; Carrion, R.S.; Palmero, S.G.; González, P.S.; Pérez, C.G.; Aguilera, E.J.G. Monitoring visual attention on a neurorehabilitation environment based on Interactive Video. In Proceedings of the International Conference on Recent Advances on Neurorehabilitation (ICRAN 2013), Valencia, Spain, 7–8 March 2013. [Google Scholar]
- Martini, G.; Beani, E.; Filogna, S.; Menici, V.; Cioni, G.; Battini, R.; Sgandurra, G. New Technological Approach for the Evaluation of Postural Control Abilities in Children with Developmental Coordination Disorder. Children 2022, 9, 957. [Google Scholar] [CrossRef] [PubMed]
- Leonardi, S.; Maggio, M.G.; Russo, M.; Bramanti, A.; Arcadi, F.A.; Naro, A.; Calabrò, R.S.; De Luca, R. Cognitive recovery in people with relapsing/remitting multiple sclerosis: A randomized clinical trial on virtual reality-based neurorehabilitation. Clin. Neurol. Neurosurg. 2021, 208, 106828. [Google Scholar] [CrossRef]
- Ravi, D.K.; Kumar, N.; Singhi, P. Effectiveness of virtual reality rehabilitation for children and adolescents with cerebral palsy: An updated evidence-based systematic review. Physiotherapy 2017, 103, 245–258. [Google Scholar]
- Alemanno, F.; Houdayer, E.; Emedoli, D.; Locatelli, M.; Mortini, P.; Mandelli, C.; Raggi, A.; Iannaccone, S. Efficacy of virtual reality to reduce chronic low back pain: Proof-of-concept of a non-pharmacological approach on pain, quality of life, neuropsychological and functional outcome. PLoS ONE 2019, 14, e0216858. [Google Scholar] [CrossRef] [Green Version]
- Maresca, G.; Maggio, M.G.; Buda, A.; La Rosa, G.; Manuli, A.; Bramanti, P.; Luca, R.D.; Calabrò, R.S. A novel use of virtual reality in the treatment of cognitive and motor deficit in spinal cord injury: A case report. Medicine 2018, 97, e13559. [Google Scholar] [CrossRef] [PubMed]
- Laver, K.; George, S.; Thomas, S.; Deutsch, J.E.; e Crotty, M. Realtà virtuale per la riabilitazione dell’ictus: Una versione ridotta di una revisione Cochrane. Riv. Eur. Di Med. Fis. E Riabil. 2015, 51, 497–506. [Google Scholar]
- Maresca, G.; Leonardi, S.; De Cola, M.C.; Giliberto, S.; Di Cara, M.; Corallo, F.; Quartarone, A.; Pidalà, A. Use of Virtual Reality in Children with Dyslexia. Children 2022, 9, 1621. [Google Scholar] [CrossRef] [PubMed]
- Patel, R.; Salata, A. Using computer games to mediate caregiver–child communication for children with severe dysarthria. J. Med. Speech Lang. Pathol. 2006, 14, 279–284. [Google Scholar]
- Bryant, L.; Brunner, M.; Hemsley, B. A review of virtual reality technologies in the field of communication disability: Implications for practice and research. Disabil. Rehabil. Assist. Technol. 2020, 15, 365–372. [Google Scholar] [CrossRef]
- Eldridge, S.M.; Chan, C.L.; Campbell, M.J.; Bond, C.M.; Hopewell, S.; Thabane, L.; Lancaster, G.A. PAFS consensus group. CONSORT 2010 statement: Extension to randomised pilot and feasibility trials. BMJ 2016, 355, i5239. [Google Scholar] [CrossRef] [Green Version]
- Cianchetti, C.; Fancello, G.S. Test TVL. Test di valutazione del linguaggio. In Livello Prescolare; Edizioni Erickson: Trento, Italy, 1997; Volume 16. [Google Scholar]
- Majorano, M.; Lavelli, M. The use of sophisticated words with children with specific language impairment during shared book reading. J. Commun. Disord. 2015, 53, 1–16. [Google Scholar] [CrossRef]
- Panesi, S.; Morra, S. The relation between drawing and language in preschoolers: The role of working Memory and executive functions. Cogn. Dev. 2022, 61, 101142. [Google Scholar] [CrossRef]
- Nicastri, M.; Giallini, I.; Amicucci, M.; Mariani, L.; de Vincentiis, M.; Greco, A.; Guerzoni, L.; Cuda, D.; Ruoppolo, G.; Mancini, P. Variables influencing executive functioning in preschool hearing-impaired children implanted within 24 months of age: An observational cohort study. Eur. Arch. Oto-Rhino-Laryngol. 2021, 278, 2733–2743. [Google Scholar]
- Angelillo, N.; Di Costanzo, B.; Barillari, U. Speech-language evaluation and rehabilitation treatment in Floating-Harbor syndrome: A case study. J. Commun. Disord. 2010, 43, 252–260. [Google Scholar] [CrossRef]
- Montirosso, R.; Giusti, L.; Del Prete, A.; Zanini, R.; Bellù, R.; Borgatti, R. Language outcomes at 36 months in prematurely born children is associated with the quality of developmental care in NICUs. J. Perinatol. 2016, 36, 768–774. [Google Scholar] [CrossRef]
- Roid, G.H.; Pomplun, M.; Martin, J. Nonverbal intellectual assessment with the Leiter-R. In A Practitioner’s Guide to Assessment of Intelligence Achievement; Naglieri, J., Goldstein, S., Eds.; Wiley: New York, NY, USA, 2013; pp. 265–290. [Google Scholar]
- Wechsel, D. Wechsler Preschool and Primary Scale of Intelligence-Fourth Edition (WPPSI-IV) dt. Bearbeitung von F.Petermann M. Daseking; Pearson Assessment: Frankfurt, Germany, 2018. [Google Scholar]
- Wechsler, D. Wechsler Intelligence Scale for Children, 4th Edition (WISC-IV); Psychological Corporation: San Antonio, TX, USA, 2003. [Google Scholar]
- Contrada, M.; Arcuri, F.; Tonin, P.; Pignolo, L.; Mazza, T.; Nudo, G.; Pignataro, M.L.; Quintieri, M.; Iozzi, A.; Cerasa, A. Stroke Telerehabilitation in Calabria: A Health Technology Assessment. Front. Neurol. 2022, 12, 2333. [Google Scholar] [CrossRef]
- De Luca, R.; Bonanno, M.; Rifici, C.; Pollicino, P.; Caminiti, A.; Morone, G.; Calabrò, R.S. Does Non-Immersive Virtual Reality Improve Attention Processes in Severe Traumatic Brain Injury? Encouraging Data from a Pilot Study. Brain Sci. 2022, 12, 1211. [Google Scholar] [CrossRef] [PubMed]
- Turolla, A.; Dam, M.; Ventura, L.; Tonin, P.; Agostini, M.; Zucconi, C.; Kiper, P.; Cagnin, A.; Piron, L. Virtual reality for the rehabilitation of the upper limb motor function after stroke: A prospective controlled trial. J. Neuroeng. Rehabil. 2013, 10, 1–9. [Google Scholar] [CrossRef]
- Agostini, M.; Garzon, M.; Benavides-Varela, S.; De Pellegrin, S.; Bencini, G.; Rossi, G.; Rosadoni, S.; Mancuso, M.; Turolla, A.; Meneghello, F.; et al. Telerehabilitation in poststroke anomia. BioMed Res. Int. 2014, 2014, 706909. [Google Scholar] [CrossRef]
- Maresca, G.; Maggio, M.G.; Latella, D.; Cannavò, A.; De Cola, M.C.; Portaro, S.; Stagnitti, M.C.; Silvestri, G.; Torrisi, M.; Bramanti, A.; et al. Toward improving poststroke aphasia: A pilot study on the growing use of telerehabilitation for the continuity of care. J. Stroke Cerebrovasc. Dis. 2019, 28, 104303. [Google Scholar] [CrossRef] [PubMed]
- Menici, V.; Barzacchi, V.; Filogna, S.; Beani, E.; Tinelli, F.; Cioni, G.; Sgandurra, G. Tele-Rehabilitation for Postural Control by Means of Virtual Reality Rehabilitation System in an Adolescent with Motor Disorder: A Case Study. Front. Psychol. 2021, 12, 720677. [Google Scholar] [PubMed]
- Stanica, I.C.; Moldoveanu, F.; Portelli, G.P.; Dascalu, M.I.; Moldoveanu, A.; Ristea, M.G. Flexible virtual reality system for neurorehabilitation and quality of life improvement. Sensors 2020, 20, 6045. [Google Scholar] [CrossRef] [PubMed]
- Chen, F.; Wang, L.; Peng, G.; Yan, N.; Pan, X. Development and evaluation of a 3-D virtual pronunciation tutor for children with autism spectrum disorders. PLoS ONE 2019, 14, e0210858. [Google Scholar] [CrossRef] [Green Version]
- Halabi, O.; El-Seoud, S.A.; Alja’am, J.M.; Alpona, H.; Al-Hemadi, M.; Al-Hassan, D. Design of immersive virtual reality system to improve communication skills in individuals with autism. Int. J. Emerg. Technol. Learn. 2017, 12, 50–64. [Google Scholar] [CrossRef] [Green Version]
- Zhao, J.; Zhang, X.; Lu, Y.; Wu, X.; Zhou, F.; Yang, S.; Wang, L.; Wu, X.; Fei, F. Virtual reality technology enhances the cognitive and social communication of children with autism spectrum disorder. In Frontiers in Public Health. Frontiers Media SA. 2022, 10, 1029392. [Google Scholar] [CrossRef]
- Zhao, H.; Swanson, A.R.; Weitlauf, A.S.; Warren, Z.E.; Sarkar, N. Hand-in-hand: A communication-enhancement collaborative virtual reality system for promoting social interaction in children with autism spectrum disorders. IEEE Trans. Hum. Mach. Syst. 2018, 48, 136–148. [Google Scholar]
- Lorenzo, G.; Pomares, J.; Lledó, A. Inclusion of immersive virtual learning environments and visual control systems to support the learning of students with Asperger syndrome. Comput. Educ. 2013, 62, 88–101. [Google Scholar] [CrossRef]
- Frolli, A.; Savarese, G.; Di Carmine, F.; Bosco, A.; Saviano, E.; Rega, A.; Carotenuto, M.; Ricci, M.C. Children on the autism spectrum and the use of virtual reality for supporting social skills. Children 2022, 9, 181. [Google Scholar] [CrossRef]
- Brundage, S.B.; Hancock, A.B. Real enough: Using virtual public speaking environments to evoke feelings and behaviors targeted in stuttering assessment and treatment. Am. J. Speech-Lang. Pathol. 2015, 24, 139–149. [Google Scholar] [CrossRef]
- Almudhi, A. Evaluating adaptation effect in real versus virtual reality environments with people who stutter. Expert Rev. Med. Devices 2022, 19, 75–81. [Google Scholar] [CrossRef]
- Van Vuuren, S.; Cherney, L.R. A virtual therapist for speech and language therapy. In Proceedings of the Intelligent Virtual Agents: 14th International Conference, IVA 2014, Boston, MA, USA, 27–29 August 2014; Springer International Publishing: Berlin/Heidelberg, Germany, 2014; pp. 438–448. [Google Scholar]
- O’Connor, S. Virtual reality and avatars in health care. Clin. Nurs. Res. 2019, 28, 523–528. [Google Scholar] [CrossRef] [Green Version]
- Moro, C.; Štromberga, Z.; Raikos, A.; Stirling, A. The effectiveness of virtual and augmented reality in health sciences and medical anatomy. Anat. Sci. Educ. 2017, 10, 549–559. [Google Scholar] [CrossRef] [Green Version]
- Karamians, R.; Proffitt, R.; Kline, D.; Gauthier, L.V. Effectiveness of virtual reality-and gaming-based interventions for upper extremity rehabilitation poststroke: A meta-analysis. Arch. Phys. Med. Rehabil. 2020, 101, 885–896. [Google Scholar] [CrossRef]
- Giachero, A.; Calati, M.; Pia, L.; La Vista, L.; Molo, M.; Rugiero, C.; Fornaro, C.; Marangolo, P. Conversational therapy through semi-immersive virtual reality environments for language recovery and psychological well-being in post stroke aphasia. Behav. Neurol. 2020, 2020, 15. [Google Scholar] [CrossRef]
- Sultan, N.; Khushnood, K.; Qureshi, S.; Altaf, S.; Khan, M.K.; Malik, A.N.; Mehmood, R.; Awan, M.M.A. Effects of Virtual Reality Training Using Xbox Kinect on Balance, Postural Control, and Functional Independence in Subjects with Stroke. In Games for Health Journal; Mary Ann Liebert Inc.: Larchmont, NY, USA, 2023. [Google Scholar] [CrossRef]
- Manjari, K.; Verma, M.; Singal, G. A survey on assistive technology for visually impaired. Internet Things 2020, 11, 100188. [Google Scholar] [CrossRef]
- Feng, H.; Li, C.; Liu, J.; Wang, L.; Ma, J.; Li, G.; Gan, L.; Shang, X.; Wu, Z. Virtual reality rehabilitation versus conventional physical therapy for improving balance and gait in Parkinson’s disease patients: A randomized controlled trial. Med. Sci. Monit. Int. Med. J. Exp. Clin. Res. 2019, 25, 4186. [Google Scholar]
- Arane, K.; Behboudi, A.; Goldman, R.D. Virtual reality for pain and anxiety management in children. Can. Fam. Physician 2017, 63, 932–934. [Google Scholar] [PubMed]
- Coad, J.; Harding, S.; Hambly, H.; Parker, N.; Morgan, L.; Marshall, J.; Roulstone, S. Perspectives of preschool children in England with speech and language needs in the development of evidence-based activities. Child Care Health Dev. 2020, 46, 283–293. [Google Scholar] [CrossRef]
- Parsons, T.D.; Riva, G.; Parsons, S.; Mantovani, F.; Newbutt, N.; Lin, L.; Venturini, E.; Hall, T. Virtual reality in pediatric psychology. Pediatrics 2017, 140 (Suppl. S2), S86–S91. [Google Scholar] [CrossRef] [Green Version]
- Cavalcante Neto, J.L.; Steenbergen, B.; Tudella, E. Motor intervention with and without Nintendo® Wii for children with developmental coordination disorder: Protocol for a randomized clinical trial. Trials 2019, 20, 1–12. [Google Scholar]
- Bellani, M.; Fornasari, L.; Chittaro, L.; Brambilla, P. Virtual reality in autism: State of the art. Epidemiol. Psychiatr. Sci. 2011, 20, 235–238. [Google Scholar] [CrossRef] [Green Version]
- Shorey, S.; Ang, E.; Ng, E.D.; Yap, J.; Lau, L.S.T.; Chui, C.K. Communication skills training using virtual reality: A descriptive qualitative study. Nurse Educ. Today 2020, 94, 104592. [Google Scholar] [CrossRef] [PubMed]
- Salem, Y.; Elokda, A. Use of virtual reality gaming systems for children who are critically ill. J. Pediatr. Rehabil. Med. 2014, 7, 273–276. [Google Scholar] [CrossRef] [PubMed]
- Voinescu, A.; Sui, J.; Fraser, D.S. Virtual reality in neurorehabilitation: An umbrella review of meta-analyses. J. Clin. Med. 2021, 10, 1478. [Google Scholar] [CrossRef] [PubMed]
| Exercise | Game | Language Domain |
|---|---|---|
| Phrase Selection | Select the phrase representing the video shown. | Comprehension |
| Identify Action | Write the action performed in the video. | Comprehension |
| Semantic Recognition | Recognize the object among the images depicted | Comprehension |
| Image Recognition Acoustic Reference | Recognize the object among the images represented with acoustic reference. | Comprehension |
| Similar Word Recognition | Recognize the object among the similar words represented. | Comprehension |
| Separate by Color | Click on objects in the same category to divide them. | Comprehension |
| Separates by Shape | Drag and drop objects into the correct category. | Comprehension |
| Separate by Semantic Group | Drag and drop objects into the correct category. | Comprehension |
| Spatial Perceptual Orientation Front/Back | Drag the objects into the correct category by means of the verbal prose in front and behind. | Comprehension |
| Recognize One Object Among Many | Select from the list the identical item to be indicated. | Comprehension |
| Select Phrase | Repetition of sentences with picture help. | Repetition |
| Tachistoscope Pictures | Repeat the images depicted in a period of a few seconds. | Repetition |
| Tachistoscope Words | Repeat the words represented in a period of a few seconds. | Repetition |
| Farm | Repeat and select animals equal to those represented in the box. | Repetition |
| Advanced Point Connection | Join the dots ordered numerically and alphabetically. | Denomination |
| Tachistoscope Images | Name the images depicted in a period of a few seconds. | Denomination |
| Tachistoscope Words | Name the words represented in a few seconds. | Denomination |
| Reorder the Syllable Count | Rearrange the syllables to reconstruct the word. | Verbal Production |
| Select the Syllable Count | Select the first syllable belonging to the indicated image. | Verbal Production |
| Select Images | Select from multiple images represented. | Verbal Production |
| Subdivide Images | Divide between several images represented. | Verbal Production |
| Identify Action | Write down the action performed in the video. | Verbal Production |
| Identify Sentence | Write the completed sentence in the video. | Verbal Production |
| EG | CG | Total Sample | ||||
|---|---|---|---|---|---|---|
| N | Mean ± SD or % | N | Mean ± SD or % | N | Mean ± SD or % | |
| Participants | 16 | 50% | 16 | 50% | 32 | |
| Age (years) | 4.9 ± 1.3 | 4.7 ± 1.0 | 4.8 ± 1.1 | |||
| Gender | ||||||
| Male | 13 | 81.3% | 13 | 81.3% | 26 | 81.3% |
| Female | 3 | 18.7% | 3 | 18.7% | 6 | 18.7% |
| M:F Ratio | 4.3:1 | 4.3:1 | 4.3:1 | |||
| Comorbid Neurodevelopmental Disorders | ||||||
| ADHD | 3 | 18.7% | 3 | 18.7% | 6 | 18.7% |
| DCD | 1 | 6.3% | 1 | 6.3% | 2 | 6.3% |
| Clinical Assessment | Experimental Group | p-Value | Control Group | p-Value | ||
|---|---|---|---|---|---|---|
| T0 | T1 | T0 | T1 | |||
| COMP.WORDS | 3.5 | 9.0 | 0.011 | 5.0 | 5.5 | 0.036 |
| (2.0–7.0) | (3.0–10.0) | (1.5–7.5) | (3.8–10.0) | |||
| COMP.SENT | 2.0 | 7.0 | 0.004 | 3.0 | 5.0 | 0.059 |
| (3.0–10.0) | (2.0–10.0) | (0.0–5.3) | (3.0–7.0) | |||
| COMP.TOTAL | 3.5 | 9.0 | 0.004 | 4.5 | 5.5 | 0.022 |
| (2.0–5.5) | (3.0–10.0) | (1.5–5.3) | (3.0–10.0) | |||
| REPETITION | 2.0 | 4.5 | 0.004 | 2.5 | 3.5 | 0.003 |
| (0.0–10.0) | (2.8–7.0) | (0.0–4.0) | (2.0–5.3) | |||
| NAMING.BODY | 2.5 | 6.5 | 0.033 | 2.5 | 5.0 | 0.009 |
| (0.0–7.0) | (3.8–9.3) | (0.0–5.3) | (3.0–9.0) | |||
| NAMING.OBJ | 6.5 | 9.0 | 0.011 | 4.0 | 5.0 | 0.009 |
| (0.0–9.3) | (5.3–10.0) | (0.0–6.0) | (3.0–9.3) | |||
| NAMING.TOTAL | 3.0 | 6.5 | 0.029 | 3.5 | 5.0 | 0.004 |
| (0.0–7.0) | (2.8–10.0) | (0.0–5.0) | (3.0–9.3) | |||
| ACCURACY.PHONO | 0.0 | 3.5 | 0.009 | 1.0 | 2.5 | 0.002 |
| (0.0–3.3) | (2.0–6.0) | (0.0–3.0) | (2.0–6.3) | |||
| ACCURACY.MORPH | 2.0 | 6.5 | 0.012 | 3.0 | 4.5 | 0.033 |
| (0.0–5.5) | (3.8–10.0) | (0.0–7.5) | (2.0–10.0) | |||
| CONS.SENT | 0.0 | 5.0 | 0.005 | 2.5 | 6.0 | 0.002 |
| (0.0–4.3) | (2.0–9.3) | (0.0–4.5) | (2.80–10.0) | |||
| CONS.PERIOD | 0.0 | 2.5 | 0.030 | 3.0 | 6.0 | 0.002 |
| (0.0–3.3) | (2.0–6.8) | (0.0–6.0) | (2.8–10.0) | |||
| CONS.MLU | 1.0 | 5.0 | 0.013 | 2.5 | 4.0 | 0.039 |
| (0.0–4.5) | (2.0–9.3) | (0.0–5.0) | (1.5–9.3) | |||
| CONS.STYLE | 2.5 | 6.5 | 0.006 | 2.0 | 4.0 | 0.090 |
| (0.0–6.0) | (2.8–7.5) | (0.0–4.3) | (0.0–6.0) | |||
| CONS.SPONT | 2.0 | 3.5 | 0.031 | 3.0 | 4.5 | 0.071 |
| (1.5–4.3) | (2.0–6.3) | (0.0–4.0) | (2.0–5.0) | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Cappadona, I.; Ielo, A.; La Fauci, M.; Tresoldi, M.; Settimo, C.; De Cola, M.C.; Muratore, R.; De Domenico, C.; Di Cara, M.; Corallo, F.; et al. Feasibility and Effectiveness of Speech Intervention Implemented with a Virtual Reality System in Children with Developmental Language Disorders: A Pilot Randomized Control Trial. Children 2023, 10, 1336. https://doi.org/10.3390/children10081336
Cappadona I, Ielo A, La Fauci M, Tresoldi M, Settimo C, De Cola MC, Muratore R, De Domenico C, Di Cara M, Corallo F, et al. Feasibility and Effectiveness of Speech Intervention Implemented with a Virtual Reality System in Children with Developmental Language Disorders: A Pilot Randomized Control Trial. Children. 2023; 10(8):1336. https://doi.org/10.3390/children10081336
Chicago/Turabian StyleCappadona, Irene, Augusto Ielo, Margherita La Fauci, Maria Tresoldi, Carmela Settimo, Maria Cristina De Cola, Rosalia Muratore, Carmela De Domenico, Marcella Di Cara, Francesco Corallo, and et al. 2023. "Feasibility and Effectiveness of Speech Intervention Implemented with a Virtual Reality System in Children with Developmental Language Disorders: A Pilot Randomized Control Trial" Children 10, no. 8: 1336. https://doi.org/10.3390/children10081336
APA StyleCappadona, I., Ielo, A., La Fauci, M., Tresoldi, M., Settimo, C., De Cola, M. C., Muratore, R., De Domenico, C., Di Cara, M., Corallo, F., Tripodi, E., Impallomeni, C., Quartarone, A., & Cucinotta, F. (2023). Feasibility and Effectiveness of Speech Intervention Implemented with a Virtual Reality System in Children with Developmental Language Disorders: A Pilot Randomized Control Trial. Children, 10(8), 1336. https://doi.org/10.3390/children10081336







