Comparative Analysis of Hematological and Biochemical Changes in Neonates among Women with and without COVID-19 Infection during Pregnancy
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Settings
2.2. Participants
2.3. Variables
2.4. Data Sources/Measurement
2.5. Reducing Bias
2.6. Statistical Analysis
3. Results
3.1. Baseline Characteristics
3.2. Investigating the Impact of Maternal COVID-19 Infection on Fetal Laboratory Test Results
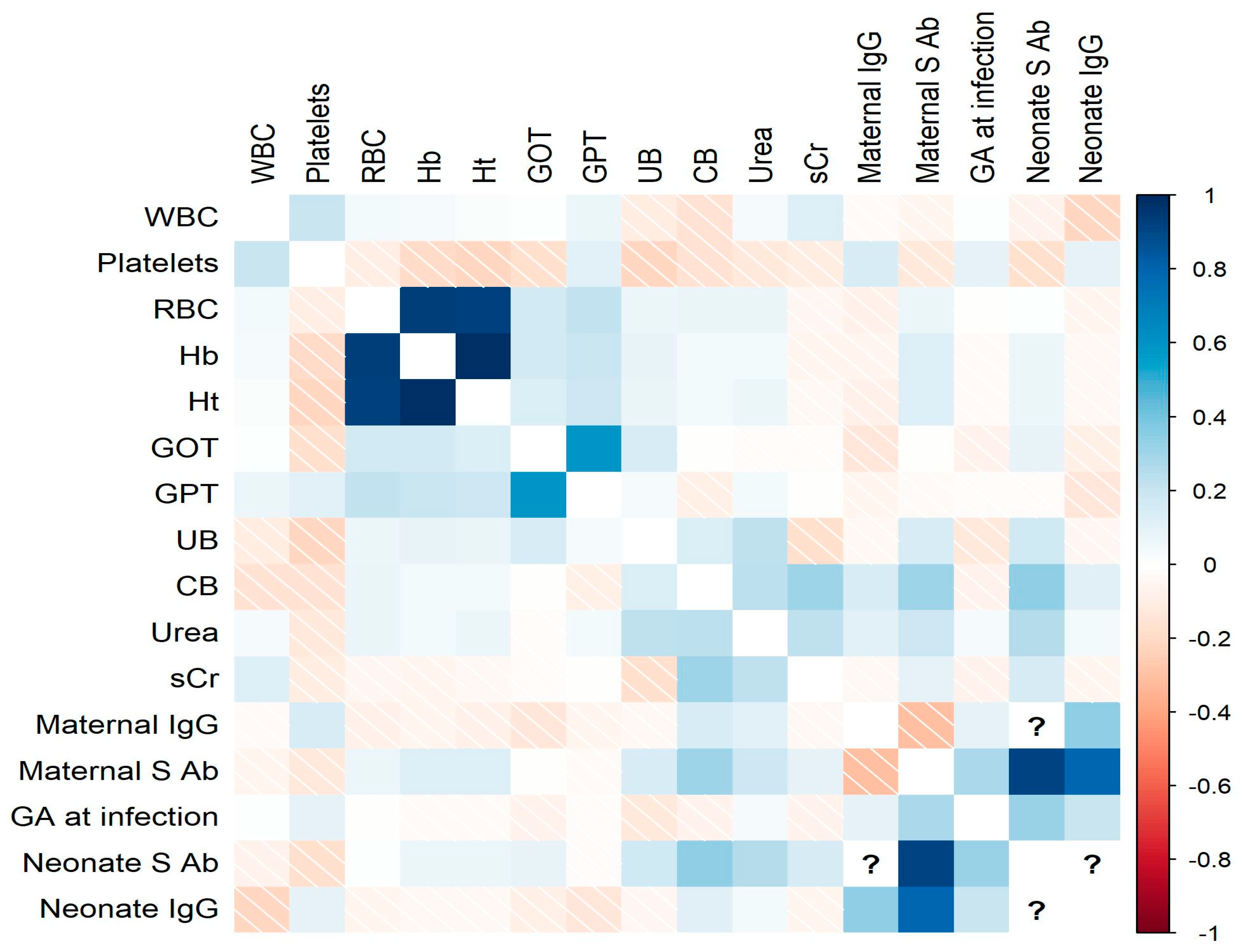
3.3. Hematological and Biochemical Profiles in Neonates of COVID-19-Positive Mothers
4. Discussion
4.1. Key Results
4.2. Limitations
4.3. Interpretation
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Abbreviation | Full Form |
|---|---|
| COVID-19 | Coronavirus disease |
| FGR | fetal growth restriction |
| GA | gestational age |
| GOT | glutamic oxaloacetic transaminase |
| GPT | glutamic pyruvic transaminase |
| GW | gestational weeks |
| IgG | Immunoglobulin G |
| IL-1β | interleukin-1β |
| IL-6 | interleukin-6 |
| NICU | neonatal intensive care unit |
| RBC | red blood cell |
| WBC | white blood cells |
References
- Sawicka, B.; Aslan, I.; Della Corte, V.; Periasamy, A.; Krishnamurthy, S.K.; Mohammed, A.; Tolba Said, M.M.; Saravanan, P.; Del Gaudio, G.; Adom, D.; et al. Chapter 14—The Coronavirus Global Pandemic and Its Impacts on Society. In Coronavirus Drug Discovery; Egbuna, C., Ed.; Drug Discovery Update; Elsevier: Amsterdam, The Netherlands, 2022; Volume 1, pp. 267–311. [Google Scholar] [CrossRef]
- The Impact of COVID-19 on Global Health Goals. Available online: https://www.who.int/news-room/spotlight/the-impact-of-covid-19-on-global-health-goals (accessed on 6 July 2023).
- Allotey, J.; Fernandez, S.; Bonet, M.; Stallings, E.; Yap, M.; Kew, T.; Zhou, D.; Coomar, D.; Sheikh, J.; Lawson, H.; et al. Clinical Manifestations, Risk Factors, and Maternal and Perinatal Outcomes of Coronavirus Disease 2019 in Pregnancy: Living Systematic Review and Meta-Analysis. BMJ 2020, 370, m3320. [Google Scholar] [CrossRef] [PubMed]
- Chaubey, I.; Vignesh, R.; Babu, H.; Wagoner, I.; Govindaraj, S.; Velu, V. SARS-CoV-2 in Pregnant Women: Consequences of Vertical Transmission. Front. Cell. Infect. Microbiol. 2021, 11, 717104. [Google Scholar] [CrossRef] [PubMed]
- Gomez, U.T.; Francisco, R.P.V.; Baptista, F.S.; Gibelli, M.A.B.C.; Ibidi, S.M.; Carvalho, W.B.D.; Paganoti, C.D.F.; Sabino, E.C.; Silva, L.C.D.O.D.; Jaenisch, T.; et al. Impact of SARS-CoV-2 on Pregnancy and Neonatal Outcomes: An Open Prospective Study of Pregnant Women in Brazil. Clinics 2022, 77, 100073. [Google Scholar] [CrossRef] [PubMed]
- Hamidi, O.P.; Lijewski, V.; Sheeder, J.; Powell, K.; Dolph, E.; Quayson, D.; Reeves, S. Adverse Perinatal Outcomes in Pregnancies Affected by Severe COVID-19 Infection. AJOG Glob. Rep. 2022, 2, 100118. [Google Scholar] [CrossRef]
- Malik, S.; Jain, D.; Bokade, C.M.; Savaskar, S.; Deshmukh, L.S.; Wade, P.; Madhura, A.D.; Suryawanshi, M.; Bandichhode, S.T.; Bodhgire, S.B.; et al. Outcomes in Neonates Born to Mothers with COVID-19 during the Second Wave in India. Eur. J. Pediatr. 2022, 181, 3537–3543. [Google Scholar] [CrossRef]
- Panda, S.K.; Mishra, A.; Pathak, M. Clinical Outcome of Neonates Born to SARS-CoV-2 Positive Mothers in India: A Systematic Review and Meta-Analysis. Cureus 2022, 14, e22958. [Google Scholar] [CrossRef]
- Sánchez-Luna, M.; Fernández Colomer, B.; De Alba Romero, C.; Alarcón Allen, A.; Baña Souto, A.; Camba Longueira, F.; Cernada Badía, M.; Galve Pradell, Z.; González López, M.; López Herrera, M.C.; et al. Neonates Born to Mothers With COVID-19: Data from the Spanish Society of Neonatology Registry. Pediatrics 2021, 147, e2020015065. [Google Scholar] [CrossRef]
- Yoon, S.H.; Kang, J.-M.; Ahn, J.G. Clinical Outcomes of 201 Neonates Born to Mothers with COVID-19: A Systematic Review. Eur. Rev. Med. Pharmacol. Sci. 2020, 24, 7804–7815. [Google Scholar] [CrossRef]
- Birol Ilter, P.; Prasad, S.; Mutlu, M.A.; Tekin, A.B.; O’Brien, P.; Von Dadelszen, P.; Magee, L.A.; Tekin, S.; Tug, N.; Kalafat, E.; et al. Maternal and Perinatal Outcomes of SARS-CoV-2 Infection in Unvaccinated Pregnancies during Delta and Omicron Waves. Ultrasound Obstet. Gynecol. 2022, 60, 96–102. [Google Scholar] [CrossRef]
- Torche, F.; Nobles, J. The Unequal Impact of the COVID-19 Pandemic on Infant Health. Demography 2022, 59, 2025–2051. [Google Scholar] [CrossRef]
- Patberg, E.T.; Adams, T.; Rekawek, P.; Vahanian, S.A.; Akerman, M.; Hernandez, A.; Rapkiewicz, A.V.; Ragolia, L.; Sicuranza, G.; Chavez, M.R.; et al. Coronavirus Disease 2019 Infection and Placental Histopathology in Women Delivering at Term. Am. J. Obstet. Gynecol. 2021, 224, 382.e1–382.e18. [Google Scholar] [CrossRef] [PubMed]
- Shanes, E.D.; Mithal, L.B.; Otero, S.; Azad, H.A.; Miller, E.S.; Goldstein, J.A. Placental Pathology in COVID-19. Am. J. Clin. Pathol. 2020, 154, 23–32. [Google Scholar] [CrossRef] [PubMed]
- Murphy, C.A.; O’Reilly, D.P.; Edebiri, O.; Weiss, L.; Cullivan, S.; EL-Khuffash, A.; Doyle, E.; Donnelly, J.C.; Malone, F.D.; Ferguson, W.; et al. Haematological Parameters and Coagulation in Umbilical Cord Blood Following COVID-19 Infection in Pregnancy. Eur. J. Obstet. Gynecol. Reprod. Biol. 2021, 266, 99–105. [Google Scholar] [CrossRef]
- Koupenova, M.; Freedman, J.E. Platelets and Immunity: Going Viral. Arterioscler. Thromb. Vasc. Biol. 2020, 40, 1605–1607. [Google Scholar] [CrossRef]
- Nori, W.; Hameed, B.H.; Thamir, A.R.; Fadhil, A. COVID-19 in Pregnancy: Implication on Platelets and Blood Indices. Rev. Bras. Ginecol. E Obs. RBGO Gynecol. Obstet. 2021, 43, 595–599. [Google Scholar] [CrossRef] [PubMed]
- Montazersaheb, S.; Hosseiniyan Khatibi, S.M.; Hejazi, M.S.; Tarhriz, V.; Farjami, A.; Ghasemian Sorbeni, F.; Farahzadi, R.; Ghasemnejad, T. COVID-19 Infection: An Overview on Cytokine Storm and Related Interventions. Virol. J. 2022, 19, 92. [Google Scholar] [CrossRef]
- Stark, K.; Massberg, S. Interplay between Inflammation and Thrombosis in Cardiovascular Pathology. Nat. Rev. Cardiol. 2021, 18, 666–682. [Google Scholar] [CrossRef]
- Cunin, P.; Nigrovic, P.A. Megakaryocytes as Immune Cells. J. Leukoc. Biol. 2019, 105, 1111–1121. [Google Scholar] [CrossRef]
- Agnello, L.; Giglio, R.V.; Bivona, G.; Scazzone, C.; Gambino, C.M.; Iacona, A.; Ciaccio, A.M.; Lo Sasso, B.; Ciaccio, M. The Value of a Complete Blood Count (CBC) for Sepsis Diagnosis and Prognosis. Diagnostics 2021, 11, 1881. [Google Scholar] [CrossRef]
- Khanduja, P.C.; Agarwal, K.N.; Bhatt, I.; Taneja, P.N. Haematological and Biochemical Values in First Year of Life under Optimal Nutritional Conditions. Indian J. Med. Res. 1967, 55, 435–442. [Google Scholar]
- Letícia De Oliveira Toledo, S.; Sousa Nogueira, L.; Das Graças Carvalho, M.; Romana Alves Rios, D.; De Barros Pinheiro, M. COVID-19: Review and Hematologic Impact. Clin. Chim. Acta 2020, 510, 170–176. [Google Scholar] [CrossRef]
- Zhang, C.; Chu, H.; Pei, Y.V.; Zhang, J. Laboratory Effects of COVID-19 Infection in Pregnant Women and Their Newborns: A Systematic Review and Meta-Analysis. Front. Glob. Women’s Health 2021, 2, 647072. [Google Scholar] [CrossRef]
- Al-Matary, A.; Almatari, F.; Al-Matary, M.; AlDhaefi, A.; Alqahtani, M.H.S.; Alhulaimi, E.A.; AlOtaiby, S.; Almehiny, K.; John, L.S.; Alanazi, F.S.; et al. Clinical Outcomes of Maternal and Neonate with COVID-19 Infection—Multicenter Study in Saudi Arabia. J. Infect. Public Health 2021, 14, 702–708. [Google Scholar] [CrossRef]
- Kosmeri, C.; Koumpis, E.; Tsabouri, S.; Siomou, E.; Makis, A. Hematological Manifestations of SARS-CoV-2 in Children. Pediatr. Blood Cancer 2020, 67. [Google Scholar] [CrossRef] [PubMed]
- Qiu, H.; Wu, J.; Hong, L.; Luo, Y.; Song, Q.; Chen, D. Clinical and Epidemiological Features of 36 Children with Coronavirus Disease 2019 (COVID-19) in Zhejiang, China: An Observational Cohort Study. Lancet Infect. Dis. 2020, 20, 689–696. [Google Scholar] [CrossRef]
- Miller, J.; Cantor, A.; Zachariah, P.; Ahn, D.; Martinez, M.; Margolis, K.G. Gastrointestinal Symptoms as a Major Presentation Component of a Novel Multisystem Inflammatory Syndrome in Children That Is Related to Coronavirus Disease 2019: A Single Center Experience of 44 Cases. Gastroenterology 2020, 159, 1571–1574.e2. [Google Scholar] [CrossRef] [PubMed]
- Mao, R.; Qiu, Y.; He, J.-S.; Tan, J.-Y.; Li, X.-H.; Liang, J.; Shen, J.; Zhu, L.-R.; Chen, Y.; Iacucci, M.; et al. Manifestations and Prognosis of Gastrointestinal and Liver Involvement in Patients with COVID-19: A Systematic Review and Meta-Analysis. Lancet Gastroenterol. Hepatol. 2020, 5, 667–678. [Google Scholar] [CrossRef] [PubMed]
- Stolfi, I.; Conti, M.G.; Marciano, A.; Dito, L.; Natale, F.; Bartolucci, M.; Cellitti, R.; Regoli, D.; Ticchiarelli, A.; Pangallo, I.; et al. Liver Involvement in SARS-CoV-2 Vertically Infected Newborn: A Case Report. Front. Pediatr. 2021, 9, 701722. [Google Scholar] [CrossRef]
- Benoit, J.L.; Benoit, S.W.; Oliveira, M.H.S.; Lippi, G.; Henry, B.M. Anemia and COVID-19: A Prospective Perspective. J. Med. Virol. 2021, 93, 708–711. [Google Scholar] [CrossRef]
- Tao, Z.; Xu, J.; Chen, W.; Yang, Z.; Xu, X.; Liu, L.; Chen, R.; Xie, J.; Liu, M.; Wu, J.; et al. Anemia Is Associated with Severe Illness in COVID-19: A Retrospective Cohort Study. J. Med. Virol. 2021, 93, 1478–1488. [Google Scholar] [CrossRef]
- Bergamaschi, G.; Borrelli De Andreis, F.; Aronico, N.; Lenti, M.V.; Barteselli, C.; Merli, S.; Pellegrino, I.; Coppola, L.; Cremonte, E.M.; Croce, G.; et al. Anemia in Patients with COVID-19: Pathogenesis and Clinical Significance. Clin. Exp. Med. 2021, 21, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Kaur, M. Maternal Anaemia and Neonatal Outcome: A Prospective Study on Urban Pregnant Women. J. Clin. Diagn. Res. 2015, 9. [Google Scholar] [CrossRef] [PubMed]
- Kohli, U.A.; Rajput, M.; Venkatesan, S. Association of Maternal Hemoglobin and Iron Stores with Neonatal Hemoglobin and Iron Stores. Med. J. Armed Forces India 2021, 77, 158–164. [Google Scholar] [CrossRef] [PubMed]
- Ornoy, A.; Diavcitrin, O. Fetal Effects of Primary and Secondary Cytomegalovirus Infection in Pregnancy. Reprod. Toxicol. 2006, 21, 399–409. [Google Scholar] [CrossRef] [PubMed]
- Rausen, A.R.; Richter, P.; Tallal, L.; Cooper, L.Z. Hematologic Effects of Intrauterine Rubella. JAMA 1967, 199, 75–78. [Google Scholar] [CrossRef] [PubMed]
- Giorgio, E.; De Oronzo, M.A.; Iozza, I.; Di Natale, A.; Cianci, S.; Garofalo, G.; Giacobbe, A.M.; Politi, S. Parvovirus B19 during Pregnancy: A Review. J. Prenat. Med. 2010, 4, 63–66. [Google Scholar]
- Rohlfing, A.-K.; Rath, D.; Geisler, T.; Gawaz, M. Platelets and COVID-19. Hämostaseologie 2021, 41, 379–385. [Google Scholar] [CrossRef]
- Sagara, A.; Yamaguchi, M.; Yoshimura, S.; Kodera, C.; Ohba, T.; Kondoh, E. Maternal Thrombocytopenia Due to Inflammatory Changes in the Placenta Precedes Fetal Death Associated with COVID-19. Placenta 2022, 128, 131. [Google Scholar] [CrossRef]
- Schwartz, D.A.; Avvad-Portari, E.; Babál, P.; Baldewijns, M.; Blomberg, M.; Bouachba, A.; Camacho, J.; Collardeau-Frachon, S.; Colson, A.; Dehaene, I.; et al. Placental Tissue Destruction and Insufficiency From COVID-19 Causes Stillbirth and Neonatal Death From Hypoxic-Ischemic Injury. Arch. Pathol. Lab. Med. 2022, 146, 660–676. [Google Scholar] [CrossRef]
- Kotlyar, A.M.; Grechukhina, O.; Chen, A.; Popkhadze, S.; Grimshaw, A.; Tal, O.; Taylor, H.S.; Tal, R. Vertical Transmission of Coronavirus Disease 2019: A Systematic Review and Meta-Analysis. Am. J. Obstet. Gynecol. 2021, 224, 35–53.e3. [Google Scholar] [CrossRef]
- Fathi Najafi, T.; Dashti, S.; Bahri, N. Vertical Transmission of COVID-19: A Systematic Review. Arch. Pediatr. Infect. Dis. 2020, 9, e108769. [Google Scholar] [CrossRef]



| Parameter | Overall | Group 1 (n = 167/45.50%) | Group 2 (n = 200/54.50%) | p-Value |
|---|---|---|---|---|
| Maternal Characteristics | ||||
| Age | 33 (6) | 32 (5) | 33 (6) | 0.06 |
| Gestation | 2 (1) | 2(1) | 1 (1) | 0.39 |
| Parity | 1 (1) | 1 (1) | 1 (1) | 0.12 |
| Diabetes | 2 (0.54%) | 0 | 2 | NA |
| Hypertension | 2 (0.54%) | 0 | 2 | NA |
| Cardiovascular disease | 2 (0.54%) | 2 (1.19%) | 0 | NA |
| Hepatitis | 6 (1.63%) | 2 (1.19%) | 4 (2.0%) | 0.84 |
| Trimester of infection | ||||
| 1st trimester | - | 37 (22.3%) | ||
| 2nd trimester | - | 73 (44%) | ||
| 3rd trimester | - | 56 (33.7%) | ||
| Pregnancy Complications | ||||
| C-section | 267 (75.7%) | 128 (76.64%) | 139 (69.5%) | 0.15 |
| Preeclampsia | 17 (4.63%) | 9 (5.39%) | 8 (4.0%) | 0.70 |
| FGR | 27 (7.35%) | 11 (6.58%) | 16 (8.0%) | 0.75 |
| Preterm Birth | 16 (4.36%) | 7 (4.19%) | 9 (4.50%) | 0.99 |
| Neonatal Characteristics | ||||
| Gender (male) | 200 (54.5%) | 90 (53.89%) | 110 (55.0%) | 0.01 |
| GA at birth | 39 (1) | 39 (1) | 39 (1) | 0.23 |
| Weight | 3340 (520) | 3380 (510.0) | 3295 (507.5) | 0.07 |
| Length | 51 (1.5) | 51 (2) | 50 (1) | 0.12 |
| Head Circumference | 34 (2) | 35 (3) | 34 (2) | 0.45 |
| APGAR score | 9 (0) | 9 (1) | 9 (0) | 0.05 |
| Parameter | Overall | Group 1 | Group 2 | p-Value |
|---|---|---|---|---|
| Maternal | ||||
| WBC | 9.82 (3.13) | 9.69 (2.69) | 10.04 (3.19) | 0.84 |
| Platelets | 233 (75) | 237.0 (73.0) | 229.5 (81.5) | 0.01 |
| Hemoglobin | 11.7 (1.4) | 11.6 (1.4) | 11.8 (1.4) | 0.33 |
| Hematocrit | 34.6 (3.7) | 34.6 (3.90) | 34.5 (3.62) | 0.53 |
| Red Blood Cells | 3.96 (0.455) | 3.97 (0.45) | 3.94 (0.45) | 0.91 |
| GOT | 15.8 (5.45) | 15.70 (5.85) | 15.95 (5.22) | 0.45 |
| GPT | 10.4 (5.8) | 10.20 (5.25) | 10.85 (6.12) | 0.25 |
| Neonatal | ||||
| WBC | 20.01 (5.86) | 20.46 (5.86) | 19.69 (6.04) | 0.04 |
| Platelets | 302.00 (74.50) | 303 (74.50) | 302 (71.75) | 0.85 |
| Red Blood Cells | 4.54 (0.78) | 4.500 (0.70) | 4.595 (0.82) | 0.40 |
| Hemoglobin | 16.30 (2.50) | 16.10 (2.55) | 16.35 (2.65) | 0.22 |
| Hematocrit | 47.10 (7.25) | 47.0 (6.95) | 47.3 (7.37) | 0.53 |
| GOT | 46.70 (20.60) | 48.30 (19.95) | 44.85 (19.57) | 0.08 |
| GPT | 13.90 (7.95) | 14.0 (9.65) | 13.6 (7.42) | 0.09 |
| Unconjugated bilirubine | 6.30 (2.45) | 6.3 (2.40) | 6.2 (2.42) | 0.95 |
| Conjugated bilirubine | 0.40 (0.20) | 0.4 (0.1) | 0.4 (0.2) | 0.9 |
| Urea | 12.50 (6.80) | 12.70 (6.20) | 12.25 (6.97) | 0.26 |
| Creatinine | 0.60 (0.10) | 0.6 (0.2) | 0.5 (0.2) | 0.54 |
| Group 1 | Group 2 | p-Value (OR; 95%CI) | |
|---|---|---|---|
| Neonatal Anemia | 19 (11.4%) | 15 (7.5%) | 0.21 (1.58; 0.73–3.46) |
| Neonatal Leukocytosis | 9 (5.39%) | 6 (3.0%) | 0.29 (1.83; 0.57–6.41) |
| Neonatal Thrombocytopenia | 1 (0.59%) | - | NA |
| Elevated GOT level | 127 (76.04%) | 136 (68%) | 0.10 (1.49; 0.91–2.44) |
| Elevated GPT level | 1 (0.59%) | 1 (1.0%) | 0.99 (0.59; 0.01–11.56) |
| Elevated Conjugated hyperbilirubinemia | 1 (0.59%) | - | NA |
| Elevated creatinine | 1 (0.59%) | - | NA |
| Outcomes | Asymptomatic COVID-19 | Hospitalization during COVID-19 | ||||
|---|---|---|---|---|---|---|
| Yes | No | p | Yes | No | p | |
| Neonatal Anemia | - | 19 (13.2%) | NA | 2 (22.2%) | 17 (10.7%) | 0.27 |
| Neonatal Leukocytosis | 1 (4.34%) | 8 (5.55%) | 0.99 | - | 9 (5.69%) | NA |
| Neonatal Thrombocytopenia | - | 1 (0.69%) | NA | - | 1/0.63% | NA |
| Conjugated Hyperbilirubinemia | - | 1 (0.69%) | NA | - | 1/0.63% | NA |
| Elevated GOT Level | 18/78.2% | 107/74.3% | 0.8 | 8/88.8% | 117/74.0% | 0.45 |
| Elevated GPT level | - | 1/0.69% | NA | - | 1/0.63% | NA |
| Elevated creatinine | - | 1/0.69% | NA | - | 1/0.63% | NA |
| Outcomes | Maternal SARS-CoV-2 Immunopositivity | Neonatal SARS-CoV-2 Immunopositivity | ||||
|---|---|---|---|---|---|---|
| Yes | No | p | Yes | No | p | |
| Neonatal Anemia | 13 (10.7%) | 6 (13.3%) | 0.59 | 9/10.3% | 10/12.5% | 0.80 |
| Neonatal Leukocytosis | 5 (4.09%) | 4 (8.88%) | 0.25 | 3/3.45 | 6/7.5% | 0.31 |
| Neonatal Thrombocytopenia | 1/0.81% | - | NA | 1/1.1% | - | NA |
| Conjugated Hyperbilirubinemia | - | 1/2.2% | NA | - | 1/1.3% | NA |
| Elevated GOT Level | 89/73.0% | 36/80.0% | 0.42 | 65/74.7% | 60/75.0% | 0.96 |
| Elevated GPT level | 1/0.81% | - | NA | 1/1.1% | - | NA |
| Elevated creatinine | - | 1/2.2% | NA | - | 1/1.3% | NA |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Popescu, D.-E.; Cerbu, S.; Rosca, I.; Lungu, N.; Trușculescu, A.A.; Belengeanu, V.; Manea, A.M.; Dima, M.A.; Gorun, F.; Popa, Z.L.; et al. Comparative Analysis of Hematological and Biochemical Changes in Neonates among Women with and without COVID-19 Infection during Pregnancy. Children 2023, 10, 1370. https://doi.org/10.3390/children10081370
Popescu D-E, Cerbu S, Rosca I, Lungu N, Trușculescu AA, Belengeanu V, Manea AM, Dima MA, Gorun F, Popa ZL, et al. Comparative Analysis of Hematological and Biochemical Changes in Neonates among Women with and without COVID-19 Infection during Pregnancy. Children. 2023; 10(8):1370. https://doi.org/10.3390/children10081370
Chicago/Turabian StylePopescu, Daniela-Eugenia, Simona Cerbu, Ioana Rosca, Nicoleta Lungu, Ana Adriana Trușculescu, Valerica Belengeanu, Aniko Maria Manea, Mirabela Adina Dima, Florin Gorun, Zoran Laurentiu Popa, and et al. 2023. "Comparative Analysis of Hematological and Biochemical Changes in Neonates among Women with and without COVID-19 Infection during Pregnancy" Children 10, no. 8: 1370. https://doi.org/10.3390/children10081370
APA StylePopescu, D.-E., Cerbu, S., Rosca, I., Lungu, N., Trușculescu, A. A., Belengeanu, V., Manea, A. M., Dima, M. A., Gorun, F., Popa, Z. L., Crisan, D. C., & Boia, M. (2023). Comparative Analysis of Hematological and Biochemical Changes in Neonates among Women with and without COVID-19 Infection during Pregnancy. Children, 10(8), 1370. https://doi.org/10.3390/children10081370









