Management and Outcomes of Tibial Eminence Fractures in the Pediatric Population: A Systematic Review
Abstract
:1. Introduction
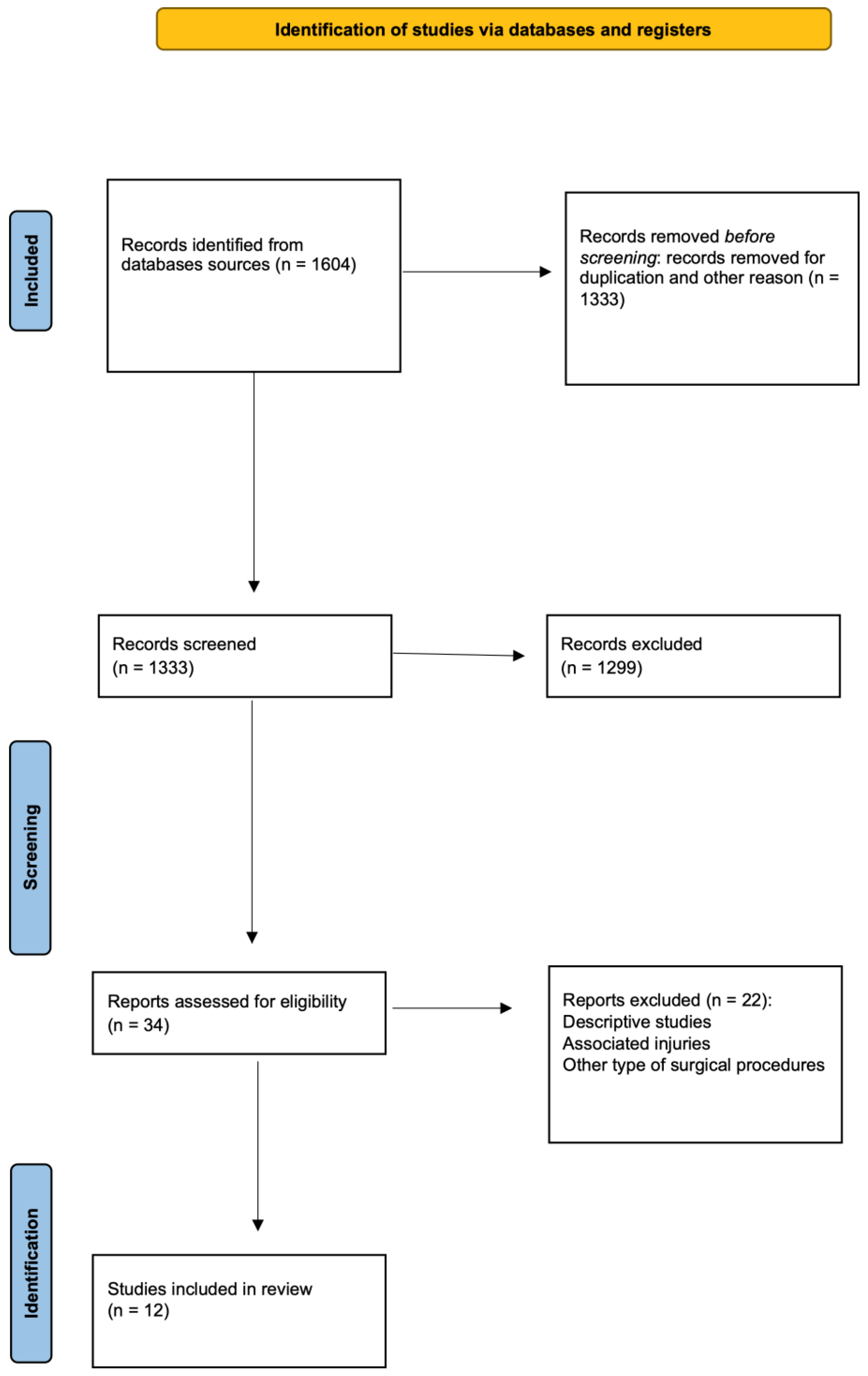
2. Material and Methods
2.1. Search Criteria
2.2. Inclusion and Exclusion Criteria
2.3. Study Screening
2.4. Data Collection
| First Author (YoP) | Patient Initially/Final | Type of Treatment | Age/SD or Range (Year) | FU/SD or Range (Months) | Male (%) | Type of Trauma, No of Patients | Complications |
|---|---|---|---|---|---|---|---|
| Zheng (2021) * [11] | 10/10 | Open | 10.9/1.53 | 27.1/11.8 | 50% | NA | NA |
| 24/24 | Arthroscopic screw | 10.9/2 | 27.5/11.8 | 45.8% | NA | NA | |
| Edmonds (2015) * [12] | 29/29 | Open | 12.2/3 | 81.6/24 | 82.7% | NA | Arthrofibrosis |
| 28/28 | Arthroscopic suture | 12.4/2 | 81.6/24 | 64.3% | NA | Arthrofibrosis | |
| Watts (2016) * [13] | 13/13 | Open | 11.5/2.6 | 12.7/14.3 | 53.8% | NA | Arthrofibrosis |
| 8/8 | Arthroscopic screw | 12.9/2.7 | 13.9/10.5 | na | NA | NA | |
| 9/9 | Arthroscopic suture | 12.9/2.7 | 13.9/10.5 | na | NA | NA | |
| Xu (2016) [14] | 21/21 | Arthroscopic suture | 15.3/13–17 | 43.4/40–47 | 71.4% | Sport (9), car accident (8), other (3) | NA |
| Zhao (2018) [15] | 22/22 | Arthroscopic suture | 11.3/8–16 | 34.5/24–46 | 59% | NA | NA |
| Callanan (2019) * [16] | 33/33 | Arthroscopic suture | 12.4/12–15 | 24/NA | 66.7% | Sport (30), other (3) | Arthrofibrosis, implant removal, other |
| 35/35 | Arthroscopic screw | 12.2/3.3 | 48/NA | 77.1% | Sport (28), other (7) | Arthrofibrosis, implant removal, other | |
| Çağlar (2021) [17] | 28/28 | Arthroscopic suture | 14.2/8–18 | 55.7/28.8–87.6 | 60.1% | Other (28) | Arthrofibrosis |
| Russu (2021) [18] | 12/12 | Arthroscopic suture | 14.3/2.1 | 6/NA | 33% | Sport (12) | NA |
| Honeycutt (2020) [19] | 35/35 | Open | 11.2/3.3 | 48/NA | 77% | Sport (28), other (7) | Arthrofibrosis, implant removal, other |
| Chalopin (2022) [20] | 20/17 | Arthroscopic suture | 12/7.15 | 28/16–48 | 47% | NA | NA |
| Zhang (2020) [21] | 21/21 | Arthroscopic suture | 12.7/2.1 | 24/22.6–34 | 66.7% | NA | NA |
| Quinlan (2021) [22] | 97/66 | Arthroscopic suture | 10.7/4–17 | 69.6/12–142.8 | 50% | NA | NA |
2.5. Level of Evidence and Studies Quality Assessment
2.6. Statistical Analysis
3. Results
3.1. Demographic and Clinical Data of All Patients
3.2. Demographic and Clinical Data of ORIF
3.3. Demographic and Clinical Data of Arthroscopic Treatment
3.4. Demographic and Clinical Data of Arthroscopic Suture Treatment
3.5. Demographic and Clinical Data of ARIF
3.6. Comparison between Open and Arthroscopic Treatment
3.7. Comparison between Arthroscopic Suture and Arthroscopic-Guided Screw Fixation Treatment
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Data Availability Statement
Conflicts of Interest
References
- Wiley, J.J.; Baxter, M.P. Tibial Spine Fractures in Children. Clin. Orthop. Relat. Res. 1990, 255, 54–60. [Google Scholar] [CrossRef]
- DeFrancesco, C.J.; Wilson, L.; Lebrun, D.G.; Memtsoudis, S.G.; Fabricant, P.D. Pediatric Tibial Spine Fractures: Exploring Case Burden by Age and Sex. Orthop. J. Sports Med. 2021, 9, 23259671211027237. [Google Scholar] [CrossRef] [PubMed]
- Axibal, D.P.; Mitchell, J.J.; Mayo, M.H.; Chahla, J.; Dean, C.S.; Palmer, C.E.; Campbell, K.; Vidal, A.F.; Rhodes, J.T. Epidemiology of Anterior Tibial Spine Fractures in Young Patients: A Retrospective Cohort Study of 122 Cases. J. Pediatr. Orthop. 2019, 39, E87–E90. [Google Scholar] [CrossRef]
- Meyers, M.H.; McKeever, F.M. Fracture of the Intercondylar Eminence of the Tibia. J. Bone Jt. Surg. Am. 1959, 41-A, 209–222. [Google Scholar] [CrossRef]
- Green, D.; Tuca, M.; Luderowski, E.; Gausden, E.; Goodbody, C.; Konin, G. A New, MRI-Based Classification System for Tibial Spine Fractures Changes Clinical Treatment Recommendations When Compared to Myers and Mckeever. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 86–92. [Google Scholar] [CrossRef] [PubMed]
- Accousti, W.K.; Willis, R.B. Tibial Eminence Fractures. Orthop. Clin. N. Am. 2003, 34, 365–375. [Google Scholar] [CrossRef]
- Cruz, A.I.; Lee, R.J.; Kushare, I.; Baghdadi, S.; Green, D.W.; Ganley, T.J.; Ellis, H.B.; Mistovich, R.J. Tibial Spine Fractures in Young Athletes. Clin. Sports Med. 2022, 41, 653–670. [Google Scholar] [CrossRef]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA Statement for Reporting Systematic Reviews and Meta-Analyses of Studies That Evaluate Healthcare Interventions: Explanation and Elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [Green Version]
- Briggs, K.K.; Steadman, J.R.; Hay, C.J.; Hines, S.L. Lysholm Score and Tegner Activity Level in Individuals with Normal Knees. Am. J. Sports Med. 2009, 37, 898–901. [Google Scholar] [CrossRef]
- Collins, N.J.; Misra, D.; Felson, D.T.; Crossley, K.M.; Roos, E.M. Measures of Knee Function: International Knee Documentation Committee (IKDC) Subjective Knee Evaluation Form, Knee Injury and Osteoarthritis Outcome Score (KOOS), Knee Injury and Osteoarthritis Outcome Score Physical Function Short Form (KOOS-PS), Knee Outcome Survey Activities of Daily Living Scale (KOS-ADL), Lysholm Knee Scoring Scale, Oxford Knee Score (OKS), Western Ontario and McMaster Universities Osteoarthritis Index (WOMAC), Activity Rating Scale (ARS), and Tegner Activity Score (TAS). Arthritis Care Res. 2011, 63 (Suppl. S11), S208–S228. [Google Scholar] [CrossRef] [Green Version]
- Arneja, S.; Leith, J. Review Article: Validity of the KT-1000 Knee Ligament Arthrometer. J. Orthop. Surg. 2009, 17, 77–79. [Google Scholar] [CrossRef]
- Lysholm, J.; Gillquist, J. Evaluation of Knee Ligament Surgery Results with Special Emphasis on Use of a Scoring Scale. Am. J. Sports Med. 1982, 10, 150–154. [Google Scholar] [CrossRef] [PubMed]
- OCEBM Levels of Evidence Working Group. The Oxford 2011 Levels of Evidence; Oxford Centre for Evidence-Based Medicine: Oxford, UK. Available online: http://www.Cebm.Net/Index.Aspx?O=5653—Cerca Con Google (accessed on 19 May 2023).
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological Index for Non-Randomized Studies (Minors): Development and Validation of a New Instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef] [PubMed]
- Zheng, C.; Han, H.; Cao, Y. Arthroscopically Assisted Cannulated Screw Fixation for Treating Type III Tibial Intercondylar Eminence Fractures: A Short-Term Retrospective Controlled Study. Front. Surg. 2021, 8, 639270. [Google Scholar] [CrossRef]
- Edmonds, E.W.; Fornari, E.D.; Dashe, J.; Roocroft, J.H.; King, M.M.; Pennock, A.T. Results of Displaced Pediatric Tibial Spine Fractures: A Comparison Between Open, Arthroscopic, and Closed Management. J. Pediatr. Orthop. 2015, 35, 651–656. [Google Scholar] [CrossRef]
- Watts, C.D.; Larson, A.N.; Milbrandt, T.A. Open versus Arthroscopic Reduction for Tibial Eminence Fracture Fixation in Children. J. Pediatr. Orthop. 2016, 36, 437–439. [Google Scholar] [CrossRef]
- Xu, X.; Liu, Z.; Wen, H.; Pan, X. Arthroscopic Fixation of Pediatric Tibial Eminence Fractures Using Suture Anchors: A Mid-Term Follow-Up. Arch. Orthop. Trauma Surg. 2017, 137, 1409–1416. [Google Scholar] [CrossRef] [PubMed]
- Zhao, C.; Bi, Q.; Bi, M. Management of a Type Two Avulsion Fracture of the Tibial Intercondylar Eminence in Children: Arthroscopic Suture Fixation versus Conservative Immobilization. Int. Orthop. 2018, 42, 1363–1369. [Google Scholar] [CrossRef] [PubMed]
- Callanan, M.; Allen, J.; Flutie, B.; Tepolt, F.; Miller, P.E.; Kramer, D.; Kocher, M.S. Suture Versus Screw Fixation of Tibial Spine Fractures in Children and Adolescents: A Comparative Study. Orthop. J. Sports Med. 2019, 7, 2325967119881961. [Google Scholar] [CrossRef] [Green Version]
- Çağlar, C.; Yağar, H.; Emre, F.; Uğurlu, M. Mid-Term Outcomes of Arthroscopic Suture Fixation Technique in Tibial Spine Fractures in the Pediatric Population. Ulus. Travma Acil Cerrahi Derg. 2021, 27, 571–576. [Google Scholar] [CrossRef]
- Russu, O.M.; Pop, T.S.; Ciorcila, E.; Gergely, I.; Zuh, S.G.; Trâmbițaș, C.; Borodi, P.G.; Incze-Bartha, Z.; Feier, A.M.; Georgeanu, V.A. Arthroscopic Repair in Tibial Spine Avulsion Fractures Using Polyethylene Terephthalate Suture: Good to Excellent Results in Pediatric Patients. J. Pers. Med. 2021, 11, 434. [Google Scholar] [CrossRef] [PubMed]
- Honeycutt, M.W.; Rambo, A.J.; Zieman, D.P.; Nimityongskul, P. Pediatric Tibial Eminence Fracture Treatment: A Case Series Using a Bioabsorbable Screw. J. Clin. Orthop. Trauma. 2020, 11, S675–S680. [Google Scholar] [CrossRef] [PubMed]
- Chalopin, A.; Geffroy, L.; Decante, C.; Noailles, T.; Hamel, A. Arthroscopic Suture-Fixation of Anterior Tibial Intercondylar Eminence Fractures by Retensioning of the ACL and Hollowing of the Tibial Footprint: Objective and Subjective Clinical Results in a Paediatric Population. Orthop. Traumatol. Surg. Res. 2022, 108, 103270. [Google Scholar] [CrossRef] [PubMed]
- Zhang, L.; Zhang, L.; Zheng, J.; Ren, B.; Kang, X.; Zhang, X.; Dang, X. Arthroscopic Tri-Pulley Technology Reduction and Internal Fixation of Pediatric Tibial Eminence Fracture: A Retrospective Analysis. BMC Musculoskelet. Disord. 2020, 21, 408. [Google Scholar] [CrossRef]
- Quinlan, N.J.; Hobson, T.E.; Mortensen, A.J.; Tomasevich, K.M.; Adeyemi, T.; Maak, T.G.; Aoki, S.K. Tibial Spine Repair in the Pediatric Population: Outcomes and Subsequent Injury Rates. Arthrosc. Sports Med. Rehabil. 2021, 3, e1011–e1023. [Google Scholar] [CrossRef]
- Skak, S.V.; Jensen, T.T.; Poulsen, T.D.; Stürup, J. Epidemiology of Knee Injuries in Children. Acta Orthop. Scand. 1987, 58, 78–81. [Google Scholar] [CrossRef] [Green Version]
- DeFrancesco, C.J.; Tananbaum, A.; LeBrun, D.G.; Fabricant, P.D. The Incidence of Pediatric Tibial Spine Fractures Is Greater and Peaks Later in Male Patients. Arthrosc. Sports Med. Rehabil. 2022, 4, e639–e643. [Google Scholar] [CrossRef]
- Oostvogel, H.J.M.; Klasen, H.J.; Reddingius, R.E. Fractures of the Intercondylar Eminence in Children and Adolescents. Arch. Orthop. Trauma. Surg. 1988, 107, 242–247. [Google Scholar] [CrossRef]
- Furlan, D.; Pogorelić, Z.; Biočić, M.; Jurić, I.; Meštrović, J. Pediatric Tibial Eminence Fractures: Arthroscopic Treatment Using K-Wire. Scand. J. Surg. 2010, 99, 38–44. [Google Scholar] [CrossRef]
- Tegner, Y. Rating Systems in the Evaluation of Knee Ligament Injuries. Clin. Orthop. Relat. Res. 1985, 198, 42–49. [Google Scholar] [CrossRef]
- Shimberg, J.L.; Leska, T.M.; Cruz, A.I.; Patel, N.M.; Ellis, H.B.; Ganley, T.J.; Johnson, B.; Milbrandt, T.A.; Yen, Y.M.; Mistovich, R.J. A Multicenter Comparison of Open versus Arthroscopic Fixation for Pediatric Tibial Spine Fractures. J. Pediatr. Orthop. 2022, 42, 195–200. [Google Scholar] [CrossRef] [PubMed]
- Osti, L.; Buda, M.; Soldati, F.; Del Buono, A.; Osti, R.; Maffulli, N. Arthroscopic Treatment of Tibial Eminence Fracture: A Systematic Review of Different Fixation Methods. Br. Med. Bull. 2016, 118, 73–90. [Google Scholar] [CrossRef] [Green Version]
- Jääskelä, M.; Turati, M.; Lempainen, L.; Bremond, N.; Courvoisier, A.; Henri, A.; Accadbled, F.; Sinikumpu, J. Long-Term Outcomes of Tibial Spine Avulsion Fractures after Open Reduction with Osteosuturing Versus Arthroscopic Screw Fixation: A Multicenter Comparative Study. Orthop. J. Sports Med. 2023, 11, 23259671231176991. [Google Scholar] [CrossRef] [PubMed]
- Wagih, A.M. Arthroscopic Treatment of Avulsed Tibial Spine Fractures Using a Transosseous Sutures Technique. Acta Orthop. Belg. 2015, 81, 141–146. [Google Scholar]
- Vander Have, K.L.; Ganley, T.J.; Kocher, M.S.; Price, C.T.; Herrera-Soto, J.A. Arthrofibrosis after Surgical Fixation of Tibial Eminence Fractures in Children and Adolescents. Am. J. Sports Med. 2010, 38, 298–301. [Google Scholar] [CrossRef]
- Ashraf, A.; Luo, T.D.; Christophersen, C.; Hunter, L.R.; Dahm, D.L.; Mcintosh, A.L. Acute and Subacute Complications of Pediatric and Adolescent Knee Arthroscopy. Arthroscopy 2014, 30, 710–714. [Google Scholar] [CrossRef] [PubMed]
- Parikh, S.N.; Myer, D.; Eismann, E.A. Prevention of Arthrofibrosis after Arthroscopic Screw Fixation of Tibial Spine Fracture in Children and Adolescents. Orthopedics 2014, 37, e58–e65. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Almeida, A.; Roveda, G.; Valin, M.R.; de Almeida, N.C.; Sartor, V.; Alves, S.M. Complications of the screw/washer tibial fixation technique for knee ligament reconstruction. Rev. Bras. Ortop. 2015, 45, 409–414. [Google Scholar] [CrossRef] [Green Version]
- Jain, S.; Modi, P.; Dayma, R.L.; Mishra, S. Clinical Outcome of Arthroscopic Suture versus Screw Fixation in Tibial Avulsion of the Anterior Cruciate Ligament in Skeletally Mature Patients. J. Orthop. 2022, 35, 7–12. [Google Scholar] [CrossRef] [PubMed]
- Shin, Y.W.; Uppstrom, T.J.; Haskel, J.D.; Green, D.W. The Tibial Eminence Fracture in Skeletally Immature Patients. Curr. Opin. Pediatr. 2015, 27, 50–57. [Google Scholar] [CrossRef]
| A Clearly Stated Aim | Inclusion of Consecutive Patients | Prospective Collection of Data | Unbiased Assessment of the Study Endpoint | Endpoints Appropriate to the Study Outcomes | Follow-Up Appropriate | Loss to FU < 5% | Calculation of the Study Size | Adequate Control Group | Contemporary Groups | Baseline Equivalence of Groups | Adequate Statistical Analysis | Total | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Zheng (2021) [11] | 0 | 0 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 18 |
| Edmonds (2015) [12] | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 18 |
| Watts (2016) [13] | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 18 |
| Xu (2016) [14] | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | NA | NA | NA | NA | 10 |
| Zhao (2018) [15] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 22 |
| Callanan (2019) [16] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | 2 | 2 | 2 | 2 | 22 |
| Çağlar (2021) [17] | 2 | 0 | 0 | 2 | 2 | 2 | 2 | 0 | NA | NA | NA | NA | 10 |
| Russu (2021) [18] | 2 | 0 | 2 | 2 | 2 | 0 | 2 | 0 | NA | NA | NA | NA | 10 |
| Honeycutt (2020) [19] | 2 | 0 | 2 | 2 | 2 | 2 | 1 | 0 | NA | NA | NA | NA | 11 |
| Chalopin (2022) [20] | 2 | 0 | 2 | 2 | 2 | 2 | 1 | 0 | NA | NA | NA | NA | 11 |
| Zhang (2020) [21] | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 0 | NA | NA | NA | NA | 14 |
| Quinlan (2021) [22] | 2 | 2 | 2 | 2 | 2 | 2 | 1 | 0 | NA | NA | NA | NA | 13 |
| Variables | ORIF | ARIF | p-Value |
|---|---|---|---|
| Follow up | 50.8 SD 31.6 | 44.7 SD 22.5 | 0.08 |
| Age (years) | 11.7 SD 0.6 | 12.2 SD 1.5 | 0.0134 |
| Men | 40 | 193 | 0.123 |
| Sport injury | 2 | 79 | 0.173 |
| Days trauma | 6.3 SD 2.9 | 8.6 SD 5.9 | 0.0055 |
| Tegner score | 7.8 SD 0.9 | 7.05 SD 0.9 | 0.0196 |
| KT1000 | NA | 3.4 SD 2 | - |
| IKDC Score | 92.1 SD 3.6 | 89.7 SD 5.2 | 0.1550 |
| Lysholm score | 96.7 SD 3.2 | 91.4 SD 4.7 | <0.0001 |
| Arthrofibrosis | 4 | 32 | 0.034 |
| Implant removal | 1 | 26 | 0.006 |
| Variables | Arthrosuture | Arthroscrew | p-Value |
|---|---|---|---|
| Follow up | 47 SD 24.4 | 36.6 SD 17.2 | <0.0001 |
| Age (years) | 12.4 SD 1.4 | 11.3 SD 1.1 | <0.0001 |
| Men | 144 | 38 | 0.373 |
| Sport injury | 51 | 28 | 0.0001 |
| Days trauma | 9.24 SD 6.4 | 6.3 SD 0 | 0.01 |
| Tegner score | 7.5 SD 0.9 | 6.4 0.5 | <0.0001 |
| KT1000 | 3.4 SD 2 | NA | - |
| IKDC Score | 90.4 SD 5.6 | 86.7 SD 5.8 | 0.0034 |
| Lysholm score | 92.5 SD 4.6 | 86.2 SD 4.5 | <0.0001 |
| Arthrofibrosis | 13 | 12 | 0.0152 |
| Implant removal | 3 | 22 | <0.00001 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Limone, B.; Zambianchi, F.; Cacciola, G.; Seracchioli, S.; Catani, F.; Tarallo, L. Management and Outcomes of Tibial Eminence Fractures in the Pediatric Population: A Systematic Review. Children 2023, 10, 1379. https://doi.org/10.3390/children10081379
Limone B, Zambianchi F, Cacciola G, Seracchioli S, Catani F, Tarallo L. Management and Outcomes of Tibial Eminence Fractures in the Pediatric Population: A Systematic Review. Children. 2023; 10(8):1379. https://doi.org/10.3390/children10081379
Chicago/Turabian StyleLimone, Beatrice, Francesco Zambianchi, Giorgio Cacciola, Stefano Seracchioli, Fabio Catani, and Luigi Tarallo. 2023. "Management and Outcomes of Tibial Eminence Fractures in the Pediatric Population: A Systematic Review" Children 10, no. 8: 1379. https://doi.org/10.3390/children10081379
APA StyleLimone, B., Zambianchi, F., Cacciola, G., Seracchioli, S., Catani, F., & Tarallo, L. (2023). Management and Outcomes of Tibial Eminence Fractures in the Pediatric Population: A Systematic Review. Children, 10(8), 1379. https://doi.org/10.3390/children10081379






