Qualitative Insights into Key Angelman Syndrome Motor Related Concepts Reported by Caregivers—A Thematic Analysis of Semi-Structured Interviews
Abstract
:1. Introduction
2. Materials and Methods
2.1. Design and Participants
2.2. Ethical Considerations
2.3. Study Materials
2.4. Recruitment and Interviews
2.5. Analysis
3. Results
3.1. Sociodemographics
3.2. Analysis of Concepts
3.2.1. Saturation Analysis
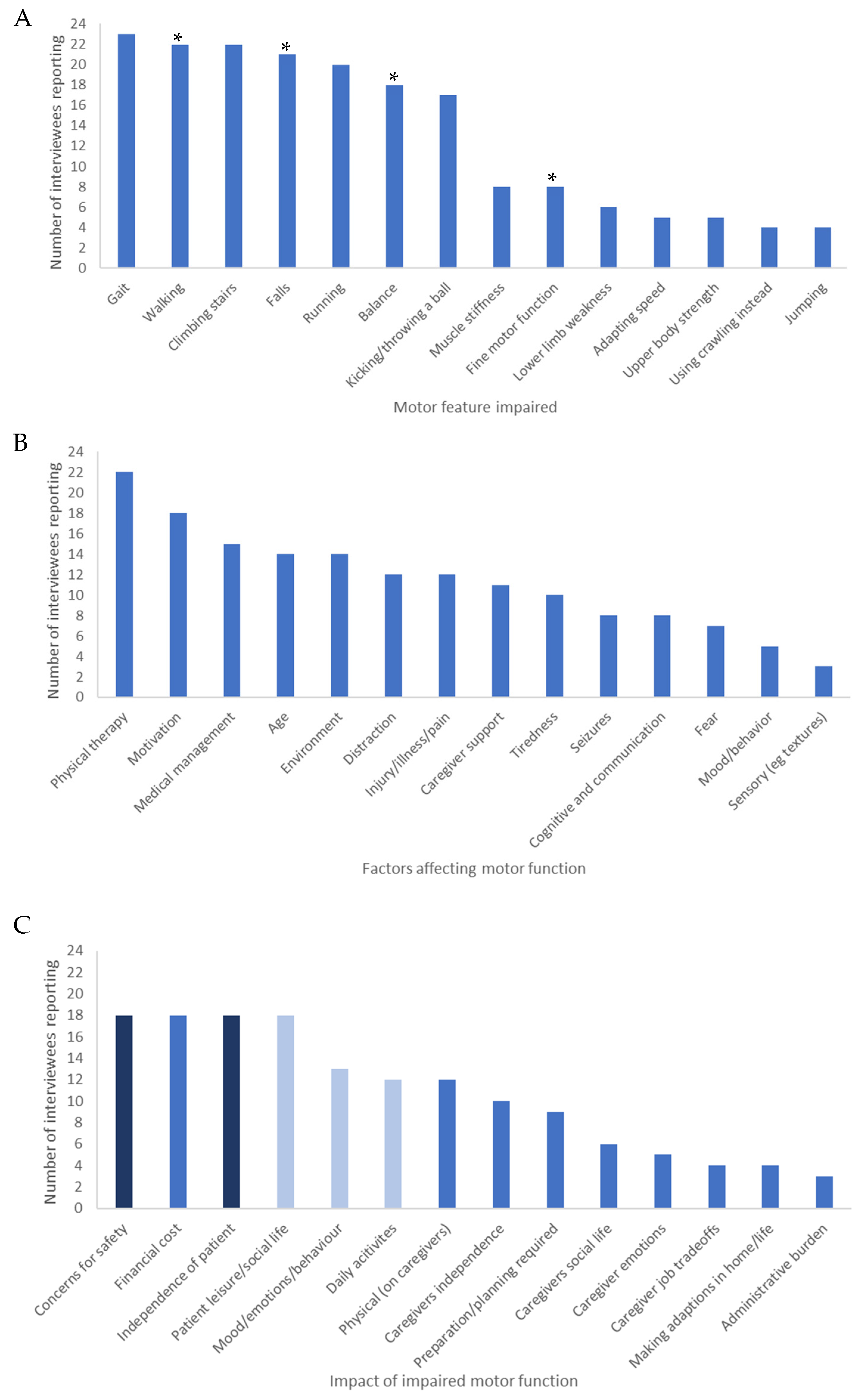
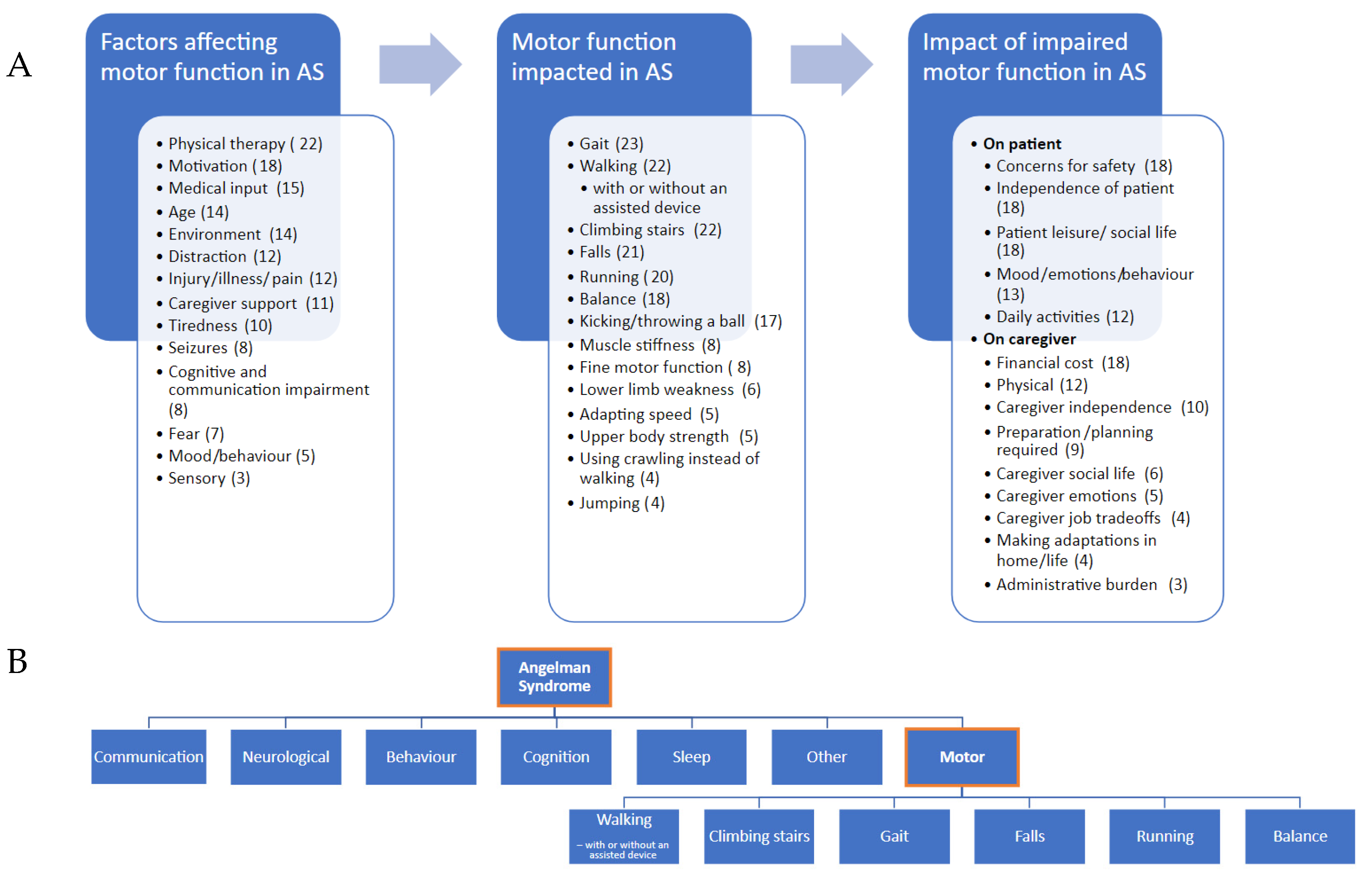
3.2.2. Motor Features Impacted in AS
“Independence is driven by walking ability to be able to go up and interact with people. Even if he had a higher level of social and communication abilities, certainly, that would be limited if he was not able to approach people independently”.Clinician discussing an 8-year-old male, USA
“So the motor thing on its own means nothing. How can we separate just motor function?”Mother of a 5-year-old female, Chile
“At the beginning, it was a very significant burden. Now that she’s managing to walk, not so much”.Mother of a 5-year-old female, Chile
3.2.3. Factors Affecting Impaired Motor Function in AS
3.2.4. Impact of Impaired Motor Function
“For gastrointestinal issues, there are medications that are fully reimbursed… There is less of a financial impact on the communication aspect”Mother of a 1-year old female, France
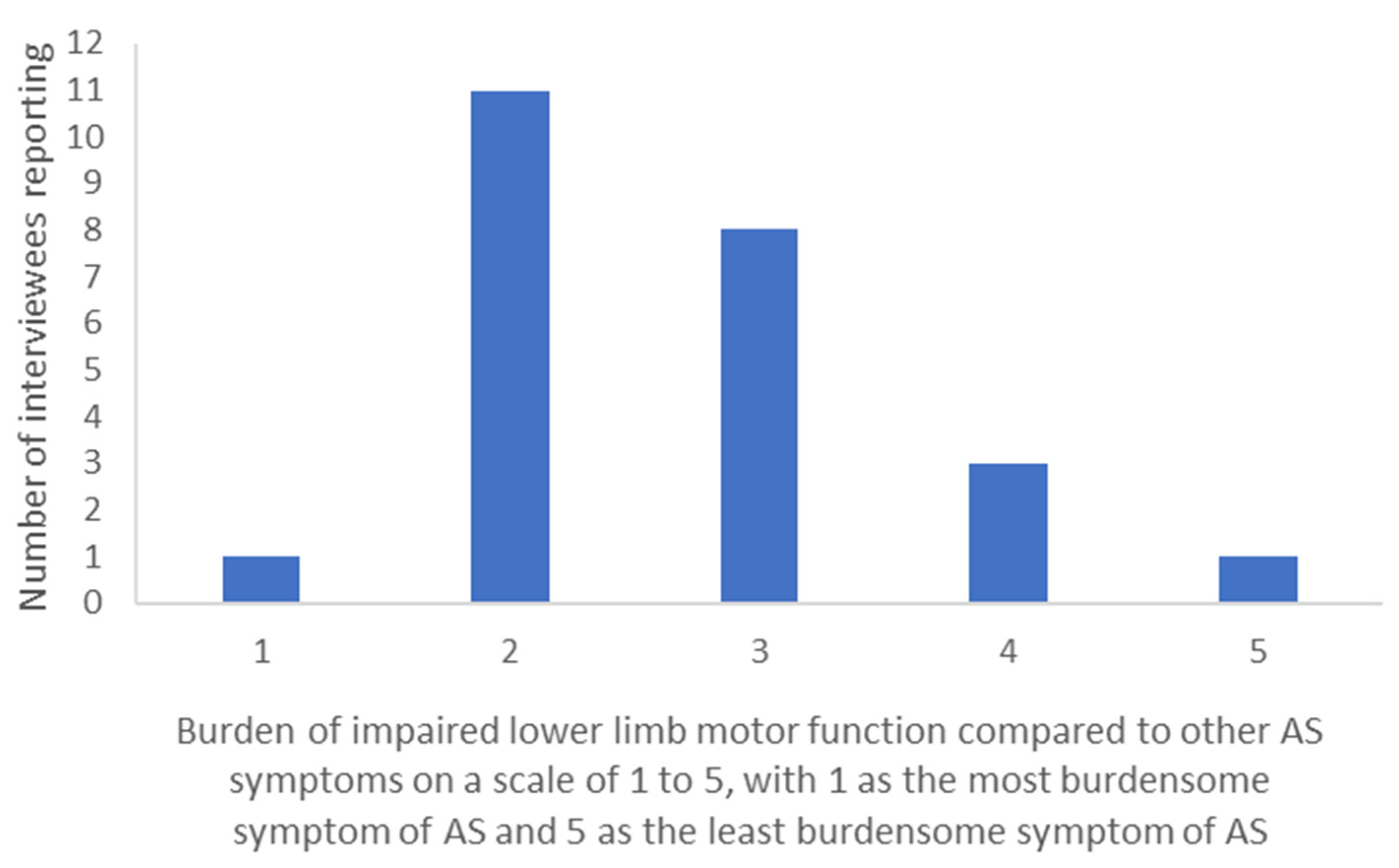
3.2.5. Relevance of Motor Function to Clinical Trials
“I think he would be able to go at a normal pace for an hour, that would be pretty life-changing for us”.Mother of a 6-year-old male, USA
“If she could walk independently. Just being able to get up and walk independently would have the biggest impact”.Mother of a 22-year-old female, USA
“That [improvement of motor function] would not be the gross motor, but the fine motor skills. That’s the eating part”.Mother of a 4-year-old female, Belgium
3.3. A Motor Function Concept Model of AS
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Williams, C.A.; Beaudet, A.L.; Clayton-Smith, J.; Knoll, J.H.; Kyllerman, M.; Laan, L.A.; Magenis, R.E.; Moncla, A.; Schinzel, A.A.; Summers, J.A.; et al. Angelman Syndrome 2005: Updated Consensus for Diagnostic Criteria. Am. J. Med. Genet. Part A 2006, 140A, 413–418. [Google Scholar] [CrossRef] [PubMed]
- Williams, C.A.; Driscoll, D.J.; Dagli, A.I. Clinical and Genetic Aspects of Angelman Syndrome. Genet. Med. 2010, 12, 385–395. [Google Scholar] [CrossRef] [PubMed]
- Kyllerman, M. Chapter 32—Angelman Syndrome. In Handbook of Clinical Neurology; Dulac, O., Lassonde, M., Sarnat, H.B., Eds.; Pediatric Neurology Part I; Elsevier: Amsterdam, The Netherlands, 2013; Volume 111, pp. 287–290. [Google Scholar]
- Wheeler, A.C.; Sacco, P.; Cabo, R. Unmet Clinical Needs and Burden in Angelman Syndrome: A Review of the Literature. Orphanet J. Rare Dis. 2017, 12, 164. [Google Scholar] [CrossRef]
- Clayton-Smith, J.; Pembrey, M.E. Angelman Syndrome. J. Med. Genet. 1992, 29, 412–415. [Google Scholar] [CrossRef]
- Markati, T.; Duis, J.; Servais, L. Therapies in Preclinical and Clinical Development for Angelman Syndrome. Expert. Opin. Investig. Drugs 2021, 30, 709–720. [Google Scholar] [CrossRef] [PubMed]
- Grieco, J.C.; Romero, B.; Flood, E.; Cabo, R.; Visootsak, J. A Conceptual Model of Angelman Syndrome and Review of Relevant Clinical Outcomes Assessments (COAs). Patient 2019, 12, 97–112. [Google Scholar] [CrossRef]
- Willgoss, T.; Cassater, D.; Connor, S.; Krishnan, M.L.; Miller, M.T.; Dias-Barbosa, C.; Phillips, D.; McCormack, J.; Bird, L.M.; Burdine, R.D.; et al. Measuring What Matters to Individuals with Angelman Syndrome and Their Families: Development of a Patient-Centered Disease Concept Model. Child. Psychiatry Hum. Dev. 2021, 52, 654–668. [Google Scholar] [CrossRef]
- Grieco, J.; Ciarlone, S.; Gieron-Korthals, M.; Schoenberg, M.; Smith, A.; Philpot, R.; Heussler, H.; Banko, J.; Weeber, E. An Open-Label Pilot Trial of Minocycline in Children as a Treatment for Angelman Syndrome. BMC Neurol. 2014, 14, 232. [Google Scholar] [CrossRef]
- Bird, L.M.; Tan, W.-H.; Bacino, C.A.; Peters, S.U.; Skinner, S.A.; Anselm, I.; Barbieri-Welge, R.; Bauer-Carlin, A.; Gentile, J.K.; Glaze, D.G.; et al. A Therapeutic Trial of Pro-Methylation Dietary Supplements in Angelman Syndrome. Am. J. Med. Genet. A 2011, 155A, 2956–2963. [Google Scholar] [CrossRef]
- Keute, M.; Miller, M.T.; Krishnan, M.L.; Sadhwani, A.; Chamberlain, S.; Thibert, R.L.; Tan, W.-H.; Bird, L.M.; Hipp, J.F. Angelman Syndrome Genotypes Manifest Varying Degrees of Clinical Severity and Developmental Impairment. Mol. Psychiatry 2021, 26, 3625–3633. [Google Scholar] [CrossRef]
- Peters, S.U.; Bird, L.M.; Kimonis, V.; Glaze, D.G.; Shinawi, L.M.; Bichell, T.J.; Barbieri-Welge, R.; Nespeca, M.; Anselm, I.; Waisbren, S.; et al. Double-Blind Therapeutic Trial in Angelman Syndrome Using Betaine and Folic Acid. Am. J. Med. Genet. A 2010, 152A, 1994–2001. [Google Scholar] [CrossRef] [PubMed]
- Gentile, J.K.; Tan, W.-H.; Horowitz, L.T.; Bacino, C.A.; Skinner, S.A.; Barbieri-Welge, R.; Bauer-Carlin, A.; Beaudet, A.L.; Bichell, T.J.; Lee, H.-S.; et al. A Neurodevelopmental Survey of Angelman Syndrome with Genotype-Phenotype Correlations. J. Dev. Behav. Pediatr. 2010, 31, 592. [Google Scholar] [CrossRef] [PubMed]
- Poleur, M.; Markati, T.; Servais, L. The Use of Digital Outcome Measures in Clinical Trials in Rare Neurological Diseases: A Systematic Literature Review. Orphanet J. Rare Dis. 2023, 18, 224. [Google Scholar] [CrossRef] [PubMed]
- Servais, L.; Camino, E.; Clement, A.; McDonald, C.M.; Lukawy, J.; Lowes, L.P.; Eggenspieler, D.; Cerreta, F.; Strijbos, P. First Regulatory Qualification of a Novel Digital Endpoint in Duchenne Muscular Dystrophy: A Multi-Stakeholder Perspective on the Impact for Patients and for Drug Development in Neuromuscular Diseases. Digit. Biomark. 2021, 5, 183–190. [Google Scholar] [CrossRef]
- Burdekin, E.D.; Fogel, B.L.; Jeste, S.S.; Martinez, J.; Rexach, J.E.; DiStefano, C.; Hyde, C.; Safari, T.; Wilson, R.B. The Neurodevelopmental and Motor Phenotype of SCA21 (ATX-TMEM240). J. Child. Neurol. 2020, 35, 953–962. [Google Scholar] [CrossRef]
- Costales, J.L.; Kolevzon, A. Phelan-McDermid Syndrome and SHANK3: Implications for Treatment. Neurotherapeutics 2015, 12, 620–630. [Google Scholar] [CrossRef]
- Dhamne, S.C.; Silverman, J.L.; Super, C.E.; Lammers, S.H.T.; Hameed, M.Q.; Modi, M.E.; Copping, N.A.; Pride, M.C.; Smith, D.G.; Rotenberg, A.; et al. Replicable in Vivo Physiological and Behavioral Phenotypes of the Shank3B Null Mutant Mouse Model of Autism. Mol. Autism 2017, 8, 26. [Google Scholar] [CrossRef]
- Pierpont, E.I.; Pierpont, M.E.; Mendelsohn, N.J.; Roberts, A.E.; Tworog-Dube, E.; Seidenberg, M.S. Genotype Differences in Cognitive Functioning in Noonan Syndrome. Genes Brain Behav. 2009, 8, 275–282. [Google Scholar] [CrossRef]
- Soorya, L.; Leon, J.; Trelles, M.P.; Thurm, A. Framework for Assessing Individuals with Rare Genetic Disorders Associated with Profound Intellectual and Multiple Disabilities (PIMD): The Example of Phelan McDermid Syndrome. Clin. Neuropsychol. 2018, 32, 1226–1255. [Google Scholar] [CrossRef]
- Wilson, R.B.; Elashoff, D.; Gouelle, A.; Smith, B.A.; Wilson, A.M.; Dickinson, A.; Safari, T.; Hyde, C.; Jeste, S.S. Quantitative Gait Analysis in Duplication 15q Syndrome and Nonsyndromic ASD. Autism Res. 2020, 13, 1102–1110. [Google Scholar] [CrossRef]
- Zwanenburg, R.J.; Ruiter, S.A.J.; van den Heuvel, E.R.; Flapper, B.C.T.; Van Ravenswaaij-Arts, C.M.A. Developmental Phenotype in Phelan-McDermid (22q13.3 Deletion) Syndrome: A Systematic and Prospective Study in 34 Children. J. Neurodev. Disord. 2016, 8, 16. [Google Scholar] [CrossRef] [PubMed]
- Food and Drug Administration. Guidance for Industry: Patient-Reported Outcome Measures: Use in Medical Product Development to Support Labeling Claims. Fed. Regist. 2009, 74, 65132–65133. [Google Scholar]
- Duis, J.; Skinner, A.; Carson, R.; Gouelle, A.; Annoussamy, M.; Silverman, J.L.; Apkon, S.; Servais, L.; Carollo, J. Quantitative Measures of Motor Development in Angelman Syndrome. Am. J. Med. Genet. A 2023, 191, 1711–1721. [Google Scholar] [CrossRef] [PubMed]
- Servais, L. Real-Life Assessment of Gait and Walking Behavior of Angelman Patients. In Proceedings of the ABOM Conference, Miami, FL, USA; 2022. [Google Scholar]

| Characteristic | Caregiver (n = 24) | Child/Adult with AS (n =24) |
|---|---|---|
| Age (years) | ||
| Mean (SD) | 41.6 (9.7) | 10.8 (8.5) |
| Median (range) | 42.0 (24.0–71.0) | 7.5 (2.5–35.0) |
| Sex, n (%) | ||
| Male | 5 (21%) | 15 (63%) |
| Female | 19 (79%) | 9 (37%) |
| Relationship to individual with AS, n (%) | ||
| Mother/Stepmother | 16 (67%) | N/A |
| Father/Stepfather | 5 (21%) | N/A |
| Other * | 3 (13%) | N/A |
| Country of residence, n (%) | ||
| USA | 12 (50%) | N/A |
| Chile | 3 (13%) | N/A |
| Belgium | 2 (8%) | N/A |
| Colombia | 2 (8%) | N/A |
| France | 2 (8%) | N/A |
| Argentina | 1 (4%) | N/A |
| Jordan | 1 (4%) | N/A |
| UK | 1 (4%) | N/A |
| Employment status, n (%) | ||
| Employed, full- or part-time | 18 (75%) | N/A |
| Homemaker | 6 (25%) | N/A |
| Education status, n (%) | ||
| Secondary/high school | 1 (4%) | N/A |
| College degree | 18 (75%) | N/A |
| Postgraduate degree | 4 (17%) | N/A |
| Other ** | 1 (4%) | N/A |
| Age at confirmed diagnosis (years) | ||
| Mean (SD) | N/A | 2.0 (1.1) |
| Median (range) | N/A | 1.65 (0.6–5) |
| Ethnicity/race, n (%) | ||
| Caucasian | N/A | 14 (58%) |
| Hispanic or Latino | N/A | 9 (38%) |
| Other *** | N/A | 1 (4%) |
| Genotype, n (%) | ||
| Deletion | N/A | 15 (63%) |
| Non-deletion | N/A | 9 (37%) |
| Patient is able to speak without technological assistance, n (%) | ||
| Yes | N/A | 4 (17%) |
| No | N/A | 20 (83%) |
| Patient is able to walk ****, n (%) | ||
| Without assistance | N/A | 15 (63%) |
| With assistance | N/A | 5 (21%) |
| Unable to walk | N/A | 4 (17%) |
| Age when reaching walking milestone (years) | ||
| Mean (SD) | N/A | 3.5 (1.5) |
| Median (range) | N/A | 3.0 (1.5–7.0) |
| 1st | 2nd | 3rd | 4th | |
|---|---|---|---|---|
| Interviews included | 2, 4, 5, 9, 11, 19 | 20, 21, 22, 23, 13, 14 | 1, 7, 3, 6, 10, 12 | 24, 8, 15, 16, 17, 18 |
| New concepts arising in motor features, factors affecting and impact on motor function (in 10% of interviewees) | 40 | 2 | 0 | 0 |
|
| Theme | Impacted Motor Feature/Factor Affecting Motor Function/Impact of Impaired Motor Function | No. of Interviewees Reporting Concept Spontaneously (s) or When Probed (p) | Quote(s) to Illustrate |
|---|---|---|---|
| Impaired motor feature | Gait | 16s, 6p | “She has a very automatic gait. It’s a little as if she were a robot.”
|
| Walking | 14s, 8p | “Well, it impacts her ability to walk efficiently. She doesn’t walk at a normal speed. She walks with a wide gait. She is imbalanced.”
| |
| Climbing stairs | 12s, 10p | “Especially when there are hurdles or climbing stairs, this gives difficulties, and then she needs a hand to assist her.”
| |
| Falls | 13s, 8p | “Mild to moderate affects balance and he falls more frequently than he might otherwise.”
| |
| Running | 7s, 12p | “She’s not able to run yet, and sometimes when I think she’s trying, she’s walking very fast, and then she looks she’s about to fall over.”
| |
| Balance | 18s, 0p | “She has a gait with an enormous lack of balance.”
| |
| Kicking/throwing a ball | 3s, 14p | “With regard to kicking a ball, he can’t really kick a ball, but if he wants to play with a ball, he needs to be supported by his mother to be able to make a movement that pushes the ball forwards, which isn’t really kicking a ball.”
| |
| Muscle stiffness | 8s, 0p | “He’ll often keep his leg stiff, move it, and then the next leg”
| |
| Fine motor function | 8s, 0p | “He struggles to pick things up and move them, such as picking up a glass and putting it somewhere else a few meters away.”
| |
| Lower limb weakness | 6s, 0p | “The entire lower portion of his body is so weak”
| |
| Adapting speed | 5s, 0p | “I don’t think that he knows how to control the speed that he walks. It’s the same speed, the same pace, all the time, whereas you and I can walk quite faster, walk faster, walk slower, run, run as fast as Usain Bolt or things like that.”
| |
| Upper body strength | 5s, 0p | “…upper body strength, this girl is stronger than most men I know. I have a friend of mine who used to be one of the UFC champion, and she slapped him so hard that his sunglasses flew off his face 40ft.”
| |
| Using crawling instead | 4s, 0p | “It’ll be lazy or smart, or she might walk 10ft and then crawl the other 60ft to you.”
| |
| Jumping | 4s, 0p | “He can walk, but he can’t run or jump or balance on one foot”
| |
| Factors affecting motor function | Physical Therapy impact of physical therapy on motor skills | 19s, 3p | “Through physical therapy, there’s been some progress in terms of, I think, control of movements in terms of building up tone because the issues of hypotonia are very challenging.”
|
| Motivation impact of motivation on motor skills | 18s, 0p | “It depends on the motivation. If he has an objective and a motive, he can walk a kilometre. For example, if he sees a truck, he could fall down, grab onto something or continue with his objective. If he doesn’t have motivation, he doesn’t want to walk because he’s not interested.”
| |
| Medical management impact of medical management (orthotics, medications, specialised equipment) on motor function | 13s, 2p | “When he’s wearing his AFOs, that provides more stability for him to walk compared to when he’s not wearing his orthotic devices.”
| |
| Age impacts of age on AS motor function | 14s, 0p | “Yes, and it’s been an improvement just because of her age. She’s getting more skills as she goes.”
| |
| Environment impact of the environment on motor function, including changes in surfaces that are difficult to navigate, to being stuck indoors due to COVID | 14s, 0p | “What’s hard about that is it depends on the environment. If it was in the home setting and the floor was clear, I would feel better. If there were things in her way, impediments or if we’re outside and there’s uneven surface, I would feel less safe. It depends on the environment.”
| |
| Distraction impact of being easily distracted on motor function | 12s, 0p | “Enclosed, where there aren’t lots of distractions and she can be more relaxed and calmer. Her movements are smoother. She’s more attentive to sounds and what is being said to her.”
| |
| Illness/injury/pain impact of acute illness, injuries or pain on motor function | 12s, 0p | “The worst thing is every time she gets sick, we see that there’s a drop and she falls back in her development.”
| |
| Caregiver support impact of caregiver support on motor function | 10s, 1p | “With a helping hand he can probably go a little bit further. On the treadmill, he’s gone up to 10 to 15 min I guess in that pace. When we walked unassisted without any equipment it’s starting and stopping, so is a little bit stand still.”
| |
| Tiredness impact of tiredness/poor sleep on motor function | 10s, 0p | “He would walk a little bit and then be tired and not want to walk anymore.”
| |
| Seizures Impact of seizures and medication for seizures on motor function | 8s, 0p | “Her seizure activity might impact her ability to walk. She’s going through a period where she had a lot of seizure activity, she may be more imbalanced.”
| |
| Cognitive and communication impairment impact of cognitive skills, cognitive development level and communication on motor function | 8s, 0p | “As he grows, there is also the cognitive side that develops a little more. Therefore, he becomes more curious and has a greater desire to explore and stand up.”
| |
| Fear impact of fear on motor function | 7s, 0p | “His movements worsen with fear. He’s really afraid of heights. Even to go across this bridge, between here and the conference room on the second floor, he wants a hand to hold because he’s afraid he’s going to fall off the bridge, even though there’s glass walls there. Fear hinders his movement to the point where he will sit down on the ground rather than cross a bridge.”
| |
| Mood/behaviour impact of mood/behaviour on motor function | 5s, 0p | “I think her mood plays a factor in terms of mobility on occasion, when she gets angry and mad, it seems to be more force in that.”
| |
| Sensory impact of sensory features eg changes in texture on motor function | 3s, 0p | “I feel like he can go longer outside if there’s something he’s looking forward to, walking through the sensory, like the leaves crunching or if it’s snowy. If he feels like there’s puddles to kick around and get wet, then he’ll definitely last longer outside because I think there’s just more distractions and more sensory overload.”
| |
| Impact of impaired motor function | Concerns for safety impact on safety such as navigating stairs, streets, new environments | 14s, 4p | “I think it’s a little bit of a double-edged sword because now that he’s able to walk independently. He also has no awareness of safety. He likes to leave or try to run into the street.”
|
| Financial cost impact on finances, such as costs of doctors/physios/equipment/home modifications/care | 7s, 11p | “We’ve definitely had to spend more money on wheelchairs like this particular chair was $800, so it affects that. We have to have a special lift for the van that was $10,000 for the seat to get her in and out. We have to have a van.”
| |
| Independence of individual with AS impact on independence eg to move around by themselves, to go where they want | 11s, 7p | “She has hardly any independence at all because of her inability to just go where she wants to go.”
| |
| AS individual leisure/social life impacts of leisure/social activities eg going shopping, going to the beach/park etc | 13s, 5p | “Going places is more difficult, and sometimes things we can do in places that we can go and things that I know she would really like, and because of lack of access for wheelchairs, then there are things that she can’t do. For instance, if there was a swimming pool that we can access or things like that.”
| |
| AS individual mood/emotions/behaviour impact on emotions and behaviour, such as anger, upset, frustration | 6s, 7p | “I think she gets angry that she can’t get somewhere, for example, even in her chair.”
| |
| Daily activities impact on skills to care for self and undertake everyday activities, such as washing, dressing, eating, brushing teeth, going to school | 8s, 4p | “In the daily activity, the lower limb function, it’s more on his adls [activities of daily living] getting him in and out of the shower. Again, you’re trying to balance on one foot when the other foot comes up to take a step over that bathtub ledge or the shower ledge, so he needs assistance there.”
| |
| Physical (on caregivers) physical impact on caregivers, usually relating to needing to pick up/carry individual with AS, resulting in caregiver injuries, pain or concern re getting injured | 11s, 1p | “My back is gone out right now. Because he’s so heavy and he can’t do things his own, like getting out of the tub. The lifting on us is super cumbersome and it is hard.”
| |
| Caregiver’s independence impaired independence of caregiver due to need to be with individual with AS | 8s, 2p | “She is always with someone, always, always. And it’s the same thing with our independence. For us, as parents to have a little time and independence, we need the help of a nanny.”
| |
| Preparation/planning required increased need for planning and preparation eg when going on a walk, going to the beach etc | 9s, 0p | “We have to consider whether things will be accessible to whatever stroller or thing that we’re using in terms of where we’re going. Will there be room for it? Will there be an elevator? If we’re going to the beach, we have to bring one that has wheels that can go on the beach so that he would be able to participate in those activities.”
| |
| Caregivers’ social life impact on caregivers social life, such as difficulty going out to parties, concerts, family events | 5s, 1p | “We can’t always go out and do the social things we want because of [name]’s behaviors.”
| |
| Caregivers’ emotions emotions resulting from individual with AS impaired motor function, including fear, upset, anxiety, stress, frustration | 5s, 0p | “The anxiety level goes up for all of us and the intensity with which you have to like walk with him, grab him, catch him. It’s a lot, so yes.”
| |
| Caregiver job tradeoffs job sacrifices due to AS impaired mobility eg giving up job, doing less hours/parttime | 4s, 0p | “My husband is the only one who works because I have to take care of him.”
| |
| Making adaptations in home/life impact on needing to make adaptations, eg getting special flooring/equipment/car | 4s, 0p | “I had to remodel our whole entire bathroom and take the bathtub out, because even with grab bars for her trying to lift her leg into the tub, she was so shaky and afraid that she couldn’t make it in there anymore.”
| |
| Administrative burden burden resulting from paperwork requirements, contacting insurance companies, sorting claims/medical equipment from said companies | 3s, 0p | “There’s regular insurance paperwork, which is a minor paper, and then there’s special needs paperwork, which feels like the Mount Everest of paperwork. Constant emails. It’s ridiculous.”
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Rogers, M.; Motola, S.; Bechichi, Y.; Cluzeau, C.; Terray, T.; Berent, A.; Panagoulias, J.; Duis, J.; Eggenspieler, D.; Servais, L. Qualitative Insights into Key Angelman Syndrome Motor Related Concepts Reported by Caregivers—A Thematic Analysis of Semi-Structured Interviews. Children 2023, 10, 1462. https://doi.org/10.3390/children10091462
Rogers M, Motola S, Bechichi Y, Cluzeau C, Terray T, Berent A, Panagoulias J, Duis J, Eggenspieler D, Servais L. Qualitative Insights into Key Angelman Syndrome Motor Related Concepts Reported by Caregivers—A Thematic Analysis of Semi-Structured Interviews. Children. 2023; 10(9):1462. https://doi.org/10.3390/children10091462
Chicago/Turabian StyleRogers, Miranda, Stéphane Motola, Yacine Bechichi, Céline Cluzeau, Tanguy Terray, Allyson Berent, Jennifer Panagoulias, Jessica Duis, Damien Eggenspieler, and Laurent Servais. 2023. "Qualitative Insights into Key Angelman Syndrome Motor Related Concepts Reported by Caregivers—A Thematic Analysis of Semi-Structured Interviews" Children 10, no. 9: 1462. https://doi.org/10.3390/children10091462
APA StyleRogers, M., Motola, S., Bechichi, Y., Cluzeau, C., Terray, T., Berent, A., Panagoulias, J., Duis, J., Eggenspieler, D., & Servais, L. (2023). Qualitative Insights into Key Angelman Syndrome Motor Related Concepts Reported by Caregivers—A Thematic Analysis of Semi-Structured Interviews. Children, 10(9), 1462. https://doi.org/10.3390/children10091462





