What Mothers Know about Newborn Bloodspot Screening and the Sources They Use to Acquire This Knowledge: A Pilot Study in Flanders
Abstract
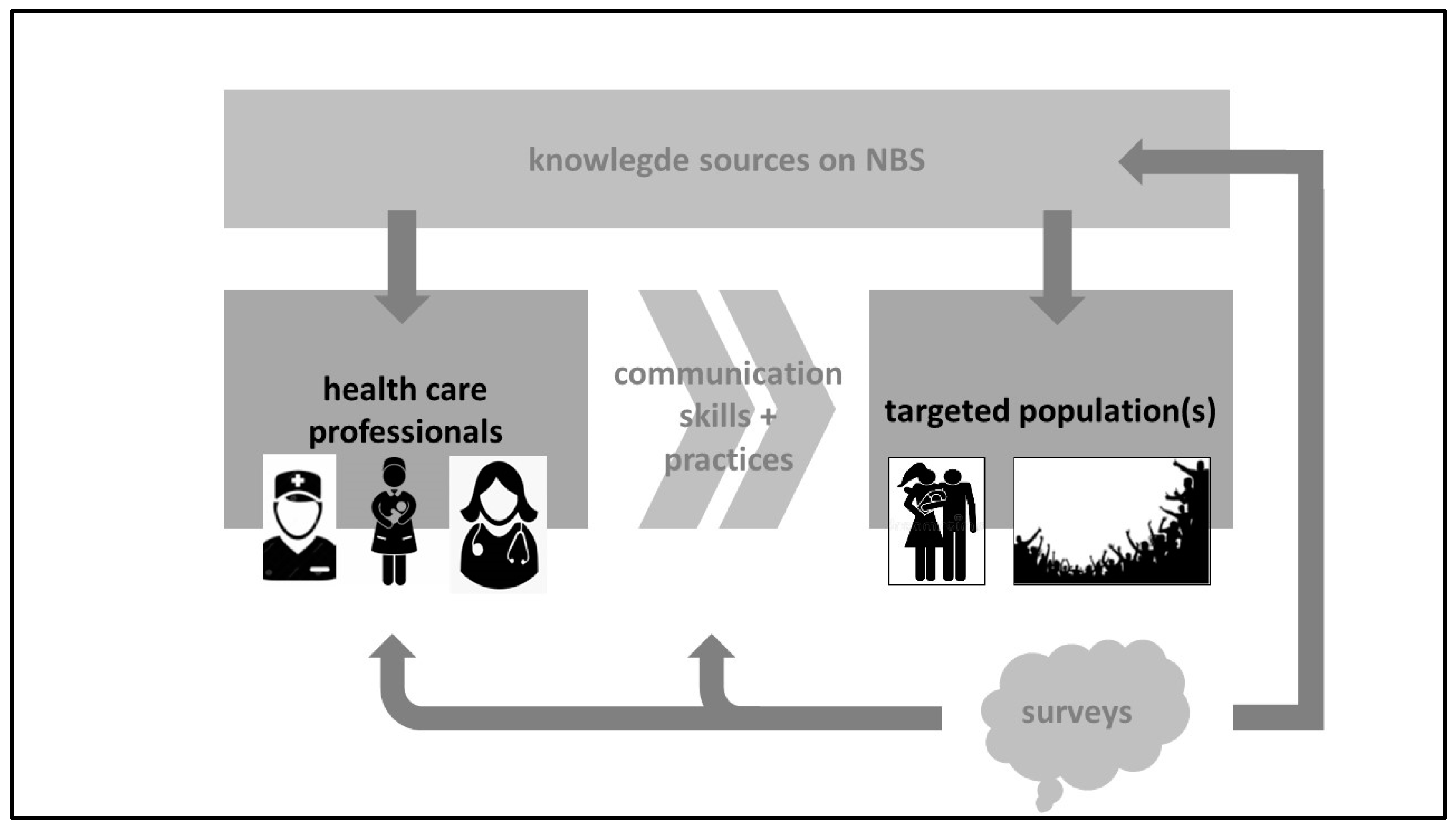
:1. Introduction
2. Materials and Methods
2.1. Perinatal Health Care Structures in Flanders and the Study Setting
2.2. Questionnaire
2.3. Data Collection and Analysis
2.4. Ethics, Privacy, and Data Management
3. Results
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Loeber, J.G.; Platis, D.; Zetterström, R.H.; Almashanu, S.; Boemer, F.; Bonham, J.R.; Borde, P.; Brincat, I.; Cheillan, D.; Dekkers, E.; et al. Neonatal Screening in Europe Revisited: An ISNS Perspective on the Current State and Developments Since 2010. Int. J. Neonatal Screen. 2021, 7, 15. [Google Scholar] [CrossRef] [PubMed]
- Franková, V.; Driscoll, R.O.; Jansen, M.E.; Loeber, J.G.; Kozich, V.; Bonham, J.; Borde, P.; Brincat, I.; Cheillan, D.; Dekkers, E.; et al. Regulatory landscape of providing information on newborn screening to parents across Europe. Eur. J. Hum. Genet. 2021, 29, 67–78. [Google Scholar] [CrossRef]
- IJzebrink, A.; van Dijk, T.; Franková, V.; Loeber, J.G.; Kožich, V.; Henneman, L.; Jansen, M.E. Informing Parents about Newborn Screening: A European Comparison Study. Int. J. Neonatal Screen. 2021, 7, 13. [Google Scholar] [CrossRef] [PubMed]
- Vlaanderen Is Zorg. Bevolkingsonderzoek, Aangeboren Aandoeningen, Draaiboek. Available online: https://aangeboren.bevolkingsonderzoek.be/wp-content/uploads/2023/06/draaiboek_vroedvrouwen_dec22.pdf (accessed on 17 September 2023).
- Vlaanderen Is Zorg. Bevolkingsonderzoek, Aangeboren Aandoeningen. Available online: https://aangeboren.bevolkingsonderzoek.be/nl/aa/aangeboren-aandoeningen-0 (accessed on 28 July 2023).
- Detmar, S.; Hosli, E.; Dijkstra, N.; Nijsingh, N.; Rijnders, M.; Verweij, M. Information and informed consent for neonatal screening: Opinions and preferences of parents. Birth 2007, 34, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Kenniscentrum, KCE. Available online: https://www.kce.fgov.be/en/publications/all-reports/organisation-of-maternity-services-in-belgium (accessed on 28 July 2023).
- Studiecentrum voor Perinatale Epidemiologie. Perinatale Gezondheid in Vlaanderen. Jaar. 2021. Available online: https://zeg.paddlecms.net/sites/default/files/2022-11/SPE-Perinatale%20gezondheid%20in%20Vlaanderen-2021-FINAL.pdf (accessed on 28 July 2023).
- STATBEL. Belgium in Figures. Available online: https://statbel.fgov.be/en/news/level-education-mapped-out (accessed on 28 July 2023).
- De Morgen. Available online: https://www.demorgen.be/nieuws/ruim-99-procent-van-baby-s-in-vlaanderen-gescreend-op-aangeboren-aandoeningen~bcd7016d/?referrer=https%3A%2F%2Fwww.google.com%2F (accessed on 28 July 2023).
- Franková, V.; Dohnalová, A.; Pešková, K.; Hermánková, R.; O’Driscoll, R.; Ješina, P.; Kožich, V. Factors influencing parental awareness about newborn screening. Int. J. Neonatal Screen. 2019, 5, 35. [Google Scholar] [CrossRef] [PubMed]
- Kasem, A.; Razeq, N.M.A.; Abuhammad, S.; Alkhazali, H. Mothers’ knowledge and attitudes about newborn screening in Jordan. J. Community Genet. 2022, 13, 215–225. [Google Scholar] [CrossRef] [PubMed]
- Etchegary, H.; Nicholls, S.G.; Tessier, L.; Simmonds, C.; Potter, B.K.; Brehaut, J.C.; Pullman, D.; Hayeems, R.; Zelenietz, S.; Lamoureux, M.; et al. Consent for newborn screening: Parents’ and health-care professionals’ experiences of consent in practice. Eur. J. Hum. Genet. 2016, 24, 1530–1534. [Google Scholar] [CrossRef] [PubMed]
- Pinel, J.; Bellanger, A.; Jamet, C.; Moreau, C. Information and parental consent for French neonatal screening: A qualitative study on parental opinion. Int. J. Neonatal Screen. 2023, 9, 26. [Google Scholar] [CrossRef] [PubMed]
- Odenwald, B.; Brockow, I.; Hanauer, M.; Lüders, A.; Nennstiel, U. Is Our Newborn Screening Working Well? A Literature Review of Quality Requirements for Newborn Blood Spot Screening (NBS) Infrastructure and Procedures. Int. J. Neonatal Screen. 2023, 9, 35. [Google Scholar] [CrossRef] [PubMed]
- van Dijk, T.; Kater, A.; Jansen, M.; Dondorp, W.J.; Blom, M.; Kemp, S.; Langeveld, M.; Cornel, M.C.; van der Pal, S.M.; Henneman, L. Expanding neonatal bloodspot screening: A multi-stakeholder perspective. Front. Pediatr. 2021, 9, 706394. [Google Scholar] [CrossRef] [PubMed]
- Davis, T.C.; Humiston, S.G.; Arnold, C.L.; Bocchini, J.A., Jr.; Bass, P.F., 3rd; Kennen, A.M.; Bocchini, A.; Kyler, P.K.; Lloyd-Puryear, M. Recommendations for effective newborn screening communication: Results of focus groups with parents, providers, and experts. Pediatrics 2006, 117, S326–S340. [Google Scholar] [CrossRef] [PubMed]
- Nicholls, S.G.; Southern, K.W. Parental decision-making and acceptance of newborn bloodspot screening: An exploratory study. PLoS ONE 2013, 8, e79441. [Google Scholar] [CrossRef] [PubMed]
| Knowledge questions, closed |
| Diseases screened for with the NBS have severe consequences if not treated appropriately. |
| The likelihood that an infant has a disease screened for is low. |
| For the NBS, some blood is collected from the heel of the infant. |
| In the event of an abnormal NBS, additional investigations in the hospital are needed. |
| A normal NBS provides certainty that the infant is perfectly healthy. |
| The NBS test is reliable, as an infant with a given disease screened for will very likely be detected. |
| In the event of uncertainties, a second NBS is indicated. |
| The NBS is compulsory for any newborn. |
| A healthy person can still be the carrier of a genetic disease. |
| When the NBS is NORMAL, parents will NOT receive a notification. |
| Immediately after the NBS analysis, the blood sample will be destroyed. |
| Are you aware of the recent extension of diseases screened for with the NBS? |
| Knowledge questions, multiple choice, including open answers |
| Who was involved to inform you about the NBS (you can provide multiple answers)? (midwife, nurse, obstetrician, general practitioner, information session during pregnancy, friends or peers, website ‘aangeboren.bevolkingsonderzoek.be’, television or radio, journals or magazines, the NBS folder, social media, I have not received information, others) |
| What was the most relevant source of information on NBS for you (you can provide multiple answers)? (midwife, nurse, obstetrician, general practitioner, information session during pregnancy, friends or peers, website ‘aangeboren.bevolkingsonderzoek.be’, television or radio, journals or magazines, the NBS folder, social media, I have not received information, others) |
| If you have received the NBS folder, have you read this document? (yes, I have read this document fully, partial, screened; no, as I was already aware of the folder, or I already knew on the NBS, not applicable as no folder received). |
| Have you searched for other sources of information? (no; yes, on the website ‘aangeboren.bevolkingsonderzoek.be’; yes, on the internet, but other websites; yes, other folders, books or magazines; yes, I have discussed this with others; yes, as…) |
| How do you overall assess the information you have received? (Likert score 0–5, where 0 is the worse score) (clarity, appropriateness of the timing, sufficiency, usefulness) |
| Variables | Categories | Respondents | Reference Population |
|---|---|---|---|
| Maternal age | <20 years | 0.5% | 0.9% |
| 20–24 | 13.5% | 8.1% | |
| 25–29 | 39% | 32% | |
| 30–34 | 34% | 40.1% | |
| 35–39 | 9% | 15.4% | |
| ≥40 | 4% | 3.5% | |
| Brussels | 0.5% | unknown | |
| Residence | Brabant, Flemish | 15% | 14.4% |
| Antwerp | 28.5% | 34.2% | |
| Limburg | 34% | 10.9% | |
| West Flanders | 9% | 17.4% | |
| East Flanders | 13% | 23.1% | |
| Parity | Primipara | 59% | 45.2% |
| Multipara | 41% | 54.8% | |
| Education | Bachelor onwards | 61.5% | 56.2% |
| ≤High school | 38.5% | 43.8% | |
| Place of delivery | Hospital | 97% | 96% |
| Out of hospital | 3% | 4% | |
| NBS collected | Yes | 99% | >99% |
| No | 0.5% | ||
| Unclear | 0.5% | ||
| Place of NBS | Hospital | 54% | unknown |
| Home | 46% | unknown |
| Questions | Yes | No | Do Not Know |
|---|---|---|---|
| Diseases screened for with the NBS have severe consequences if not treated appropriately. | 71.5% | 3% | 25.5% |
| The likelihood that an infant has a disease screened for is low. | 51% | 11.5% | 25.5% |
| For the NBS, some blood is collected from the heel of the infant. | 26% | 72% | 1.5% |
| In the event of an abnormal NBS, additional investigations in the hospital are needed. | 73% | 3% | 22.5% |
| A normal NBS provides certainty that the infant is perfectly healthy. | 5% | 86.5% | 8.5% |
| The NBS test is reliable, as an infant with a given disease screened for will very likely be detected. | 57.5% | 6% | 36.5% |
| In the event of uncertainties, a second NBS is indicated. | 44.5% | 9% | 46.5% |
| The NBS is compulsory for any newborn. | 38% | 40% | 21.5% |
| A healthy person can still be the carrier of a genetic disease. | 88.5% | 0.5% | 11% |
| When the NBS is NORMAL, parents will NOT receive a notification. | 89% | 6% | 4.5% |
| Immediately after the NBS analysis, the blood sample will be destroyed. | 12% | 9% | 79% |
| Are you aware of the recent extension of diseases screened for with the NBS? | 61.5% | 38.5% | 0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
di Gangi, C.; Hermans, M.; Rayyan, M.; Eyskens, F.; Allegaert, K. What Mothers Know about Newborn Bloodspot Screening and the Sources They Use to Acquire This Knowledge: A Pilot Study in Flanders. Children 2023, 10, 1567. https://doi.org/10.3390/children10091567
di Gangi C, Hermans M, Rayyan M, Eyskens F, Allegaert K. What Mothers Know about Newborn Bloodspot Screening and the Sources They Use to Acquire This Knowledge: A Pilot Study in Flanders. Children. 2023; 10(9):1567. https://doi.org/10.3390/children10091567
Chicago/Turabian Styledi Gangi, Caroline, Maren Hermans, Maissa Rayyan, François Eyskens, and Karel Allegaert. 2023. "What Mothers Know about Newborn Bloodspot Screening and the Sources They Use to Acquire This Knowledge: A Pilot Study in Flanders" Children 10, no. 9: 1567. https://doi.org/10.3390/children10091567
APA Styledi Gangi, C., Hermans, M., Rayyan, M., Eyskens, F., & Allegaert, K. (2023). What Mothers Know about Newborn Bloodspot Screening and the Sources They Use to Acquire This Knowledge: A Pilot Study in Flanders. Children, 10(9), 1567. https://doi.org/10.3390/children10091567







