Video-Recorded Airway Suctioning of Clear and Meconium-Stained Amniotic Fluid and Associated Short-Term Outcomes in Moderately and Severely Depressed Preterm and Term Infants
Abstract
:1. Introduction
2. Methods
2.1. The Delivery Ward
2.2. Data Collection
2.3. Data Processing
2.4. Ethical Consideration
3. Results
3.1. Effect of ASU on Spontaneous Breathing (Table 2)
| Variable | Suctioned Preterm Infants GA < 37 Weeks n = 19 | Non-Suctioned Preterm Infants GA < 37 Weeks n = 6 | p-Value | Suctioned Term Infants GA ≥ 37 Weeks n = 56 | Non-Suctioned Term Infants GA ≥ 37 Weeks n = 20 | p-Value |
|---|---|---|---|---|---|---|
| First Breathing Apnoea * Inadequate * Adequate * | 11 (58.0) 8 (42.0) 0 (0.0) | 3 (50.0) 3 (50.0) 0 (0.0) | 0.73 | 32 (57.1) 21 (37.5) 3 (5.4) | 11 (55.0) 8 (40.0) 1 (5.0) | 0.98 |
| Respiration before first suction episode (n = 200) Apnoea Inadequate Adequate | 30 (56.6) 18 (34.0) 5 (9.4) | N/A | N/A | 137 (93.2) 8 (5.4) 2 (1.4) | N/A | N/A |
| Respiration after first suction episode (n = 200) Apnoea Inadequate Adequate | 36 (67.9) 16 (30.2) 1 (1.9) | N/A | N/A | 31 (21.1) 98 (66.6) 18 (12.3) | N/A | N/A |
| Result of suction on respiration (n = 200) Improvement Worsening Unchanged | 0 (0.0) 6 (11.3) 47 (88.7) | N/A | N/A | 106 (72.1) 0 (0.0) 41 (27.9) | N/A | N/A |
| Respiratory support before suction (n = 200) PPV CPAP None | 39 (73.6) 10 (18.9) 4 (7.5) | N/A | N/A | 120 (81.6) 14 (9.5) 13 (8.9) | N/A | N/A |
| Respiratory support after suction (n = 200) PPV CPAP None | 39 (73.6) 13 (24.5) 1 (1.9) | N/A | N/A | 122 (83.0) 14 (9.5) 11 (7.5) | N/A | N/A |
| Suction before first ventilation | 4 (21.0) | N/A | N/A | 13 (23.2) | N/A | N/A |
| Ventilation initiated within first minute of age | 16 (84.2) | 5 (83.3) | 0.96 | 35 (62.5) | 15 (75.0) | 0.31 |
| Time to adequate respiration (min) | 9 (6–13) ** | 8 (7–12) | 0.08 | 12 (7–16) *** | 13 (10–19) | 0.85 |
| Endotracheal intubation | 8 (42.1) | 0 (0.0) | 0.05 | 10 (17.9) | 1 (5.0) | 0.16 |
| Result of suction on further respiratory support (n = 200) Improvement Worsening Unchanged | 0 (0.0) 3 (5.7) 50 (94.3) | N/A | N/A | 0 (0.0) 2 (1.4) 145 (98.6) | N/A | N/A |
| Time resp. supp. episode performed (min) | 5 (2–16) | N/A | N/A | 4 (2–9) | N/A | N/A |
3.2. Effect of ASU on HR (Table 3)
| Variable | Suctioned Preterm Infants GA < 37 Weeks n = 19 | Non-Suctioned Preterm Infants GA < 37 Weeks n = 6 | p-Value | Suctioned Term Infants GA ≥ 37 Weeks n = 56 | Non-Suctioned Term Infants GA ≥ 37 Weeks n = 20 | p-Value |
|---|---|---|---|---|---|---|
| FHR Normal Abnormal Not measured | 6 (31.6) 12 (63.1) 1 (5.3) | 4 (66.7) 2 (33.3) 0 (0.0) | 0.30 | 35 (62.5) 21 (37.5) 0 (0.0) | 10 (50.0) 7 (35.0) 3 (15.0) | 0.01 |
| 1st HR Absent <60 60–100 >100 | 1 (5.3) 7 (36.8) 5 (26.3) 6 (31.6) | 0 (0.0) 4 (66.6) 1 (16.7) 1 (16.7) | 0.62 | 6 (10.7) 17 (30.4) 16 (28.5) 17 (30.4) | 3 (15.0) 5 (25.0) 6 (30.0) 6 (30.0) | 0.72 |
| Type of bradycardia (brc; min) No brc Transient brc Prolonged brc | 4 (21.0) 4 (21.0) 11 (58.0) | 1 (16.7) 2 (33.3) 3 (50.0) | 0.83 | 10 (17.9) 10 (17.9) 36 (64.3) | 6 (30.0) 4 (20.0) 10 (50.0) | 0.45 |
| Infants admitted to NICU after transient and prolonged brc (n = 61 ASU infants; n = 19 non-ASU infants) | 15 (78.9) | 5 (83.3) | N/A | 46 (82.1) | 14 (70.0) | |
| Time to HR > 100 (min) | 3 (1–6) | 3 (2–6) | 1.00 | 3 (1–5) | 3 (1–5) | 0.67 |
| HR before suction episode (n = 200) Absent <60 60–100 >100 | 2 (3.8) 9 (17.0) 7 (13.2) 35 (66.0) | N/A | N/A | 4 (2.7) 20 (13.6) 27 (18.4) 96 (65.3) | N/A | N/A |
| HR after suction episode (n = 200; Total amount with HR < 100 = 65) Absent <60 60–100 >100 | 2 (3.8) 10 (18.9) 6 (11.3) 35 (66.0) | N/A | N/A | 3 (2.0) 18 (12.2) 26 (17.7) 100 (68.1) | N/A | N/A |
| Result of suction on HR (n = 200) Improvement Worsening Unchanged | 1 (1.9) 1 (1.9) 51 (96.2) | N/A | N/A | 8 (5.4) 0 (0.0) 139 (94.6) | N/A | N/A |
| Chest compression | 4 (21.0) | 0 (0.0) | 0.22 | 13 (23.2) | 5 (25.0) | 0.87 |
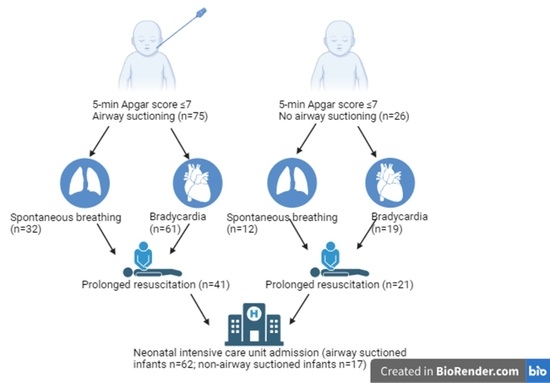
3.3. Prolonged Resuscitation (Table 1)
3.4. NICU Admission (Table 1)
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Te Pas, A.B.; Davis, P.G.; Hooper, S.B.; Morley, C.J. From liquid to air: Breathing after birth. J. Pediatr. 2008, 152, 607–611. [Google Scholar] [CrossRef] [PubMed]
- Olver, R.E.; Walters, D.V.; Wilson, S.M. Developmental regulation of lung liquid transport. Annu. Rev. Physiol. 2004, 66, 77–101. [Google Scholar] [CrossRef] [PubMed]
- Soraisham, A.S.; Lodha, A.K.; Singhal, N.; Aziz, K.; Yang, J.; Lee, S.K.; Shah, P.S.; Canadian Neonatal, N. Neonatal outcomes following extensive cardiopulmonary resuscitation in the delivery room for infants born at less than 33 weeks gestational age. Resuscitation 2014, 85, 238–243. [Google Scholar] [CrossRef] [PubMed]
- Aune, D.; Saugstad, O.D.; Henriksen, T.; Tonstad, S. Maternal body mass index and the risk of fetal death, stillbirth, and infant death: A systematic review and meta-analysis. JAMA 2014, 311, 1536–1546. [Google Scholar] [CrossRef] [PubMed]
- Aziz, K.; Chadwick, M.; Baker, M.; Andrews, W. Ante- and intra-partum factors that predict increased need for neonatal resuscitation. Resuscitation 2008, 79, 444–452. [Google Scholar] [CrossRef] [PubMed]
- Berazategui, J.P.; Aguilar, A.; Escobedo, M.; Dannaway, D.; Guinsburg, R.; de Almeida, M.F.; Saker, F.; Fernandez, A.; Albornoz, G.; Valera, M.; et al. Risk factors for advanced resuscitation in term and near-term infants: A case-control study. Arch. Dis. Child. Fetal Neonatal Ed. 2017, 102, F44–F50. [Google Scholar] [CrossRef]
- Mitchell, A.; Niday, P.; Boulton, J.; Chance, G.; Dulberg, C. A prospective clinical audit of neonatal resuscitation practices in Canada. Adv. Neonatal Care 2002, 2, 316–326. [Google Scholar] [CrossRef]
- Niles, D.E.; Cines, C.; Insley, E.; Foglia, E.E.; Elci, O.U.; Skare, C.; Olasveengen, T.; Ades, A.; Posencheg, M.; Nadkarni, V.M.; et al. Incidence and characteristics of positive pressure ventilation delivered to newborns in a US tertiary academic hospital. Resuscitation 2017, 115, 102–109. [Google Scholar] [CrossRef]
- Haumont, D.; Modi, N.; Saugstad, O.D.; Antetere, R.; NguyenBa, C.; Turner, M.; Costeloe, K.; Aelvoet, W. Evaluating preterm care across Europe using the eNewborn European Network database. Pediatr. Res. 2020, 88, 484–495. [Google Scholar] [CrossRef]
- Haumont, D.; NguyenBa, C.; Modi, N. eNewborn: The Information Technology Revolution and Challenges for Neonatal Networks. Neonatology 2017, 111, 388–397. [Google Scholar] [CrossRef]
- Kamath-Rayne, B.D.; Griffin, J.B.; Moran, K.; Jones, B.; Downs, A.; McClure, E.M.; Goldenberg, R.L.; Rouse, D.; Jobe, A.H. Resuscitation and Obstetrical Care to Reduce Intrapartum-Related Neonatal Deaths: A MANDATE Study. Matern. Child. Health J. 2015, 19, 1853–1863. [Google Scholar] [CrossRef] [PubMed]
- Janet, S.; Carrara, V.I.; Simpson, J.A.; Thin, N.W.W.; Say, W.W.; Paw, N.T.M.; Chotivanich, K.; Turner, C.; Crawley, J.; McGready, R. Early neonatal mortality and neurological outcomes of neonatal resuscitation in a resource-limited setting on the Thailand-Myanmar border: A descriptive study. PLoS ONE 2018, 13, e0190419. [Google Scholar] [CrossRef] [PubMed]
- Sotiropoulos, J.X.; Kapadia, V.; Ramachandran, S.; Oei, J.L. Ten minutes to save a baby: A narrative review of newborn assessment during first minutes of life and relationship to outcomes. Pediatr. Med. 2022, 5, 6799. [Google Scholar] [CrossRef]
- Chettri, S.; Adhisivam, B.; Bhat, B.V. Endotracheal Suction for Nonvigorous Neonates Born through Meconium Stained Amniotic Fluid: A Randomized Controlled Trial. J. Pediatr. 2015, 166, 1208–1213.e1. [Google Scholar] [CrossRef] [PubMed]
- Kumar, A.; Kumar, P.; Basu, S. Endotracheal suctioning for prevention of meconium aspiration syndrome: A randomized controlled trial. Eur. J. Pediatr. 2019, 178, 1825–1832. [Google Scholar] [CrossRef] [PubMed]
- Nangia, S.; Sunder, S.; Biswas, R.; Saili, A. Endotracheal suction in term non vigorous meconium stained neonates—A pilot study. Resuscitation 2016, 105, 79–84. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.N.; Saxena, S.; Bhriguvanshi, A.; Kumar, M. Effect of endotracheal suctioning just after birth in non-vigorous infants born through meconium stained amniotic fluid: A randomized controlled trial. Clin. Epidemiol. Glob. Health 2019, 7, 165–170. [Google Scholar] [CrossRef]
- Alsaker, T.; Klingenberg, C.; Saugstad, O.D.; Calisch, T.E.; Syltern, J.; Skåre, C.; Norwegian Resuscitation Council. Retningslinjer i Resuscitering av Nyfødte 2015. Acta Paediatr. 2015, 1–7. Available online: https://nrr.org/images/pdf/Nyfodte.pdf (accessed on 1 April 2023).
- Bruckner, M.; Lista, G.; Saugstad, O.D.; Schmolzer, G.M. Delivery Room Management of Asphyxiated Term and Near-Term Infants. Neonatology 2021, 118, 487–499. [Google Scholar] [CrossRef]
- Kelleher, J.; Bhat, R.; Salas, A.A.; Addis, D.; Mills, E.C.; Mallick, H.; Tripathi, A.; Pruitt, E.P.; Roane, C.; McNair, T.; et al. Oronasopharyngeal suction versus wiping of the mouth and nose at birth: A randomised equivalency trial. Lancet 2013, 382, 326–330. [Google Scholar] [CrossRef]
- Klingenberg, C.; O’Donnell, C.P. Inflation breaths-A transatlantic divide in guidelines for neonatal resuscitation. Resuscitation 2016, 101, e19. [Google Scholar] [CrossRef] [PubMed]
- Patterson, J.K.; Ishoso, D.; Eilevstjonn, J.; Bauserman, M.; Haug, I.; Iyer, P.; Kamath-Rayne, B.D.; Lokangaka, A.; Lowman, C.; Mafuta, E.; et al. Delayed and Interrupted Ventilation with Excess Suctioning after Helping Babies Breathe with Congolese Birth Attendants. Children 2023, 10, 652. [Google Scholar] [CrossRef] [PubMed]
- Perlman, J. Response to: Inflation breaths-A transatlantic divide in guidelines for neonatal resuscitation. Resuscitation 2016, 101, e21. [Google Scholar] [CrossRef] [PubMed]
- Purington, C.; Eilevstjonn, J.; Dalen, I.; Yeconia, A.; Blacy, L.; Mduma, E.; Haug, I.; Holte, K.; Chang, C.; Perlman, J.; et al. Use of Suctioning during Newborn Resuscitation and Its Effects on Heart Rate in a Low-Resource Setting, Tanzania. Children 2023, 10, 1540. [Google Scholar] [CrossRef]
- Saugstad, O.D.; Robertson, N.J.; Vento, M. A critical review of the 2015 International Liaison Committee on Resuscitation treatment recommendations for resuscitating the newly born infant. Acta Paediatr. 2016, 105, 442–444. [Google Scholar] [CrossRef]
- Wyckoff, M.H.; Aziz, K.; Escobedo, M.B.; Kapadia, V.S.; Kattwinkel, J.; Perlman, J.M.; Simon, W.M.; Weiner, G.M.; Zaichkin, J.G. Part 13: Neonatal Resuscitation: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2015, 132, S543–S560. [Google Scholar] [CrossRef]
- Wyllie, J.; Perlman, J.M.; Kattwinkel, J.; Wyckoff, M.H.; Aziz, K.; Guinsburg, R.; Kim, H.S.; Liley, H.G.; Mildenhall, L.; Simon, W.M.; et al. Part 7: Neonatal resuscitation: 2015 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science with Treatment Recommendations. Resuscitation 2015, 95, e169–e201. [Google Scholar] [CrossRef]
- Cordero, L., Jr.; Hon, E.H. Neonatal bradycardia following nasopharyngeal stimulation. J. Pediatr. 1971, 78, 441–447. [Google Scholar] [CrossRef]
- Fawke, J.; Wyllie, J.; Udaeta, E.; Rudiger, M.; Ersdal, H.; Wright, M.D.; Wyckoff, M.H.; Liley, H.G.; Rabi, Y.; Weiner, G.M.; et al. Suctioning of clear amniotic fluid at birth: A systematic review. Resusc. Plus 2022, 12, 100298. [Google Scholar] [CrossRef]
- Berisha, G.; Boldingh, A.M.; Nakstad, B.; Blakstad, E.W.; Ronnestad, A.E.; Lee Solevag, A. Retrospectively Assessed Muscle Tone and Skin Colour following Airway Suctioning in Video-Recorded Infants Receiving Delivery Room Positive Pressure Ventilation. Children 2023, 10, 166. [Google Scholar] [CrossRef]
- Madar, J.; Roehr, C.C.; Ainsworth, S.; Ersdal, H.; Morley, C.; Rudiger, M.; Skare, C.; Szczapa, T.; Te Pas, A.; Trevisanuto, D.; et al. European Resuscitation Council Guidelines 2021: Newborn resuscitation and support of transition of infants at birth. Resuscitation 2021, 161, 291–326. [Google Scholar] [CrossRef] [PubMed]
- Berisha, G.; Boldingh, A.M.; Blakstad, E.W.; Ronnestad, A.E.; Solevag, A.L. Management of the Unexpected Difficult Airway in Neonatal Resuscitation. Front. Pediatr. 2021, 9, 699159. [Google Scholar] [CrossRef] [PubMed]
- Boldingh, A.M.; Skare, C.; Nakstad, B.; Solevag, A.L. Suboptimal heart rate assessment and airway management in infants receiving delivery room chest compressions: A quality assurance project. Arch. Dis. Child. Fetal Neonatal Ed. 2020, 105, 545–549. [Google Scholar] [CrossRef] [PubMed]
- Weiner, M.D.F.G.M. NRP Textbook of Neonatal Resuscitation, 8th ed.; American Academy of Pediatrics: Chicago, IL, USA, 2021; pp. 33–63. [Google Scholar]
- Wyckoff, M.H.; Weiner, C.G.M.; On behalf of the Neonatal Life Support Collaborators. 2020 International Consensus on Cardiopulmonary Resuscitation and Emergency Cardiovascular Care Science With Treatment Recommendations. Pediatrics 2021, 147, e2020038505C. [Google Scholar] [CrossRef] [PubMed]
- Konstantelos, D.; Dinger, J.; Ifflaender, S.; Rudiger, M. Analyzing video recorded support of postnatal transition in preterm infants following a c-section. BMC Pregnancy Childbirth 2016, 16, 246. [Google Scholar] [CrossRef] [PubMed]
- Konstantelos, D.; Ifflaender, S.; Dinger, J.; Rudiger, M. Suctioning habits in the delivery room and the influence on postnatal adaptation—A video analysis. J. Perinat. Med. 2015, 43, 777–782. [Google Scholar] [CrossRef] [PubMed]
- Rudiger, M.; Wauer, R.R.; Schmidt, K.; Kuster, H. The Apgar score. Pediatrics 2006, 118, 1314–1315; author reply 1315–1316. [Google Scholar] [CrossRef]
- Hooper, S.B.; Polglase, G.R.; Roehr, C.C. Cardiopulmonary changes with aeration of the newborn lung. Paediatr. Respir. Rev. 2015, 16, 147–150. [Google Scholar] [CrossRef]
- Kapadia, V.; Oei, J.L.; Finer, N.; Rich, W.; Rabi, Y.; Wright, I.M.; Rook, D.; Vermeulen, M.J.; Tarnow-Mordi, W.O.; Smyth, J.P.; et al. Outcomes of delivery room resuscitation of bradycardic preterm infants: A retrospective cohort study of randomised trials of high vs low initial oxygen concentration and an individual patient data analysis. Resuscitation 2021, 167, 209–217. [Google Scholar] [CrossRef]
- Li, F.; Wu, T.; Lei, X.; Zhang, H.; Mao, M.; Zhang, J. The apgar score and infant mortality. PLoS ONE 2013, 8, e69072. [Google Scholar] [CrossRef]

| Variable | Suctioned Preterm Infants GA < 37 Weeks (n (%) or Median (IQR)) n = 19 | Non-Suctioned Preterm Infants GA < 37 Weeks (n (%) or Median (IQR)) n = 6 | p-Value | Suctioned Term Infants GA ≥ 37 Weeks (n (%) or Median (IQR)) n = 56 | Non-Suctioned Term Infants GA ≥ 37 Weeks (n (%) or Median (IQR)) n = 20 | p-Value |
|---|---|---|---|---|---|---|
| Weight (grams) | 1795 (1100–2165) | 1746 (1494–2244) | 0.64 | 3668 (3085–4093) | 3510 (3111–4130) | 0.90 |
| Apgar 1 | 3 (2–6) | 4 (2–7) | 0.68 | 3 (2–6) | 3 (2–5) | 0.99 |
| Apgar 5 | 5 (4–7) | 7 (6–7) | 0.03 | 6 (4–7) | 7 (4–7) | 0.18 |
| Apgar 10 | 8 (7–9) | 7 (7–8) | 0.83 | 8 (7–9) | 8 (6–9) | 0.31 |
| Delivery mode * Vaginal (spontaneous, forceps or vacuum) Acute Caesarean section Elective Caesarean section | 3 (15.8) 16 (84.2) 0 (0.0) | 3 (50.0) 2 (33.3) 1 (16.7) | 0.07 | 38 (67.9) 15 (26.8) 3 (5.3) | 11 (55.0) 7 (35.0) 2 (10.0) | 0.70 |
| Suction CLAF MSAF | 18 (94.7) 1 (5.3) | N/A | N/A | 50 (89.3) 6 (10.7) | N/A | N/A |
| Suction duration per episode (s) | 30 (8–47) | N/A | N/A | 16 (9–17) | N/A | N/A |
| Suction episodes before 1 min of age | 18 (34.0) | N/A | N/A | 56 (38.1) | N/A | N/A |
| Reason for suction before 1 min of age Difficult to assess Suspected obstr. airway—indicated Not indicated | 7 (38.8) 1 (5.6) 10 (55.6) | N/A | N/A | 2 (3.6) 2 (3.6) 52 (92.8) | N/A | N/A |
| Suction episodes in 1–5 min of age | 35 (66.0) | N/A | N/A | 91 (61.9) | N/A | N/A |
| Reason for suction in 1–5 min of age Difficult to assess Suspected obstr. airway—indicated Not indicated | 12 (34.3) 2 (5.7) 21 (60.0) | N/A | N/A | 36 (39.6) 6 (6.6) 49 (53.8) | N/A | N/A |
| Suction depth (n = 200) Superficial Deep Superficial plus deep | 9 (17.0) 16 (30.2) 28 (52.8) | N/A | N/A | 58 (39.5) 28 (19.0) 61 (41.5) | N/A | N/A |
| Suction total episodes/infant | 1 (1–3) | N/A | N/A | 2 (1–3) | N/A | N/A |
| Time of suction episodes performed (min) | 3 (2–12) | N/A | N/A | 6 (3–9) | N/A | N/A |
| Total suction episodes all infants (n = 200) | 53 (26.5%) | N/A | N/A | 147 (73.5%) | N/A | N/A |
| Extended resuscitation (need for resuscitation > 10 min) | 8 (42.1) | 2 (33.3) | 0.55 | 32 (57.1) | 19 (95.0) | 0.002 |
| Infant after resuscitation Normal (given to mother) Neonatal intensive care unit (n = 62 ASU infants; n = 17 non-ASU infants) Died in DR/OR | 1 (5.3) 17 (89.4) 1 (5.3) | 0 (0.0) 6 (100.0) 0 (0.0) | 0.71 | 10 (17.9) 45 (80.4) 1 (1.8) | 9 (45.0) 11 (55.0) 0 (0.0) | 0.05 |
| Therapeutic hypothermia | 0 (0.0) | 0 (0.0) | N/A | 5 (9.0) | 0 (0.0) | 0.16 |
| Outcome at 24 h Normal Neonatal intensive care unit (n = 54 ASU infants; n = 17 non-ASU infants) Died | 1 (5.3) 17 (89.4) 1 (5.3) | 0 (0.0) 6 (100.0) 0 (0.0) | 0.71 | 18 (32.1) 37 (66.1) 1 (1.8) | 9 (45.0) 11 (55.0) 0 (0.0) | 0.51 |
| Dead before hospital discharge | 4 (21.0) | 0 (0.0) | 0.22 | 1 (1.8) | 0 (0.0) | 0.54 |
| Death Early (day 0–6 from birth) Late (day 8–27 from birth) | 4 (21.0) 0 (0.0) | 0 (0.0) 0 (0.0) | 0.22 | 1 (1.8) 1 (1.8) | 0 (0.0) 0 (0.0) | 0.38 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Berisha, G.; Kvenshagen, L.N.; Boldingh, A.M.; Nakstad, B.; Blakstad, E.; Rønnestad, A.E.; Solevåg, A.L. Video-Recorded Airway Suctioning of Clear and Meconium-Stained Amniotic Fluid and Associated Short-Term Outcomes in Moderately and Severely Depressed Preterm and Term Infants. Children 2024, 11, 16. https://doi.org/10.3390/children11010016
Berisha G, Kvenshagen LN, Boldingh AM, Nakstad B, Blakstad E, Rønnestad AE, Solevåg AL. Video-Recorded Airway Suctioning of Clear and Meconium-Stained Amniotic Fluid and Associated Short-Term Outcomes in Moderately and Severely Depressed Preterm and Term Infants. Children. 2024; 11(1):16. https://doi.org/10.3390/children11010016
Chicago/Turabian StyleBerisha, Gazmend, Line Norman Kvenshagen, Anne Marthe Boldingh, Britt Nakstad, Elin Blakstad, Arild Erland Rønnestad, and Anne Lee Solevåg. 2024. "Video-Recorded Airway Suctioning of Clear and Meconium-Stained Amniotic Fluid and Associated Short-Term Outcomes in Moderately and Severely Depressed Preterm and Term Infants" Children 11, no. 1: 16. https://doi.org/10.3390/children11010016
APA StyleBerisha, G., Kvenshagen, L. N., Boldingh, A. M., Nakstad, B., Blakstad, E., Rønnestad, A. E., & Solevåg, A. L. (2024). Video-Recorded Airway Suctioning of Clear and Meconium-Stained Amniotic Fluid and Associated Short-Term Outcomes in Moderately and Severely Depressed Preterm and Term Infants. Children, 11(1), 16. https://doi.org/10.3390/children11010016