4. Discussion
Habits related with oral health are acquired during early childhood; thus, the oral health of children is mainly affected by the knowledge of the parents related to oral health [
25]. As indicated clearly in the previous literature [
25,
26,
27,
28], oral health knowledge is mandatory to implement good oral health behaviors. Furthermore, reflection of the knowledge in attitudes and practices constitutes a second and important step on the path to achieving good oral health. Because of some barriers related with parents and children, it is sometimes very hard to put knowledge into practice. Mothers are generally recognized as principal caregivers [
29]. Thus, this study was conducted on dentist mothers with a high level of oral health knowledge for a number of reasons: firstly, in order to examine their oral health practices; secondly, to clarify the most significant barriers related to children and mothers; and, lastly, to examine facilitators in order to overcome these barriers in the oral health promotion of young children.
A study by Wigen and Wang [
8] showed that children of parents with low education levels were 12 times more likely to develop cavities before the age of 5 than other children. Another study [
30] reported that, considering the educational background, illiterate mothers have insufficient knowledge, attitudes, and bad practices regarding the oral hygiene of their children. In most of the previous literature [
26,
27,
30,
31,
32,
33,
34,
35,
36], it has been shown that highly educated parents have significantly better knowledge, attitudes, and practices towards the oral health care of their children. The education levels of the parents participating in the current study were high and they mostly exhibited good attitudes and practices while promoting their young children’s oral health. Oral health knowledge is the first and most important step in oral health promotion of young children. It is obvious that, without knowledge, there will be no good attitudes and practices towards oral health care.
Dietary behaviors are also critical in the progression of dental caries, and it is clear that sugar consumption in children is associated with caries development [
8]. In the literature, a number of studies [
37,
38,
39,
40,
41,
42] have examined the parental knowledge of dietary habits related to the formation of dental caries. The results of these studies [
37,
38,
39,
40,
41,
42] supported the assumption that the vast majority of parents have good knowledge of the importance of dietary habits and the role of sweet and sticky foods in the development of dental caries. Practical reflection of the knowledge into nutrient consumption habits was shown in the current study in order to provide good oral health. Previous studies [
5,
24,
31,
36,
40,
43,
44,
45,
46] have reported higher cariogenic food consumption among children compared to the current study. In some studies [
24,
31], it is stated that the high rate of cariogenic food consumption in children of mothers with high educational status is an issue that should be evaluated in terms of the prevention of early childhood caries. This situation highlights the need for oral and dental health education to be given to all mothers regardless of their education and socioeconomic status. Furthermore, in this study, mothers reported that cariogenic feeding occurred when the children were away from their mothers in the school and family environments as in line with previous studies [
43,
47]. Children’s access to cariogenic foods should be restricted in the school environment and extended family members should pay attention to the sensitivity of parents regarding the consumption of such foods.
Primary prevention of ECC includes preventing bottle feeding, including milk or any other sugary drinks, during nights and avoiding breastfeeding after 12 months [
48]. In some studies [
4,
39,
42,
49], the knowledge and awareness of the parents about the effect of night feeding on the formation of dental caries were found to be satisfactory. On the other hand, others [
38,
40,
41,
45] have reported that parents did not have sufficient knowledge about the consequences of night feeding in young children. In addition to the knowledge and awareness of the parents, night feeding practices are an important issue that must be discussed. The results of the current study reveal better night feeding practices than those found in previous studies [
26,
31,
50].
The majority of mothers who participated in this study could not clean their children’s teeth after night feeding. The reasons for not being able to clean their children’s teeth after night feeding in most cases were to not wake the baby up, followed by being tired and other reasons. Therefore, according to the results of the present study, dentist mothers were knowledgeable about the impact of night feeding on oral health and they were in an effort to breastfeed their children. The reasons for the prolongation of night feeding after 1 year of age in this study might be because of breastfeeding habits, nearly half of the babies never used pacifiers, and mothers thought that they could perform oral cleaning when their children woke up in the morning and, thus, this would not allow plaque build-up and they did not use sugar-containing foods anyway.
Dental caries is a transmissible infectious disease in which Streptococcus mutans is generally considered to be the main etiological agent. Sharing food and utensils with children, breastfeeding, and sleeping together, which includes close contact with the child, can facilitate the transfer of saliva from adults to children, causing early colonization of streptococcus mutans [
4,
26]. In previous studies [
31,
38,
39,
40,
42,
45,
50,
51,
52], the knowledge and awareness of parents about this fact were found to be insufficient. However, in other studies [
53,
54], it was found to be high. The findings of this study were found to be below expectations fortunately; a majority of the mothers (55.77%) never shared utensils with their children.
White spot lesions, as in opaque and milky-white color, are the early signs of dental caries and, if not treated, restorative treatment is mandatory [
55]. Nearly 12% of all children had white spot lesions and 16.67% had cavitated carious lesions in this study. In order to prevent caries formation, oral hygiene practices should start in the first year of infancy before the first tooth eruption to protect young children from dental caries [
4,
28]. Tooth buds of babies can be cleaned with gauze or a muslin cloth from birth [
29]. In the study of Elison et al. [
29], starting tooth brushing as early as possible was accepted by almost all mothers. Kamil et al. [
42] stated that approximately 44% of the participants reported that it is important to start cleaning the mouth of the infants immediately after birth. In some studies [
4,
32,
50,
53,
56], it was found that most of the participants started brushing their babies’ teeth when the first deciduous teeth erupted. On the other hand, in other studies [
27,
34,
49,
57,
58], most of the parents thought that their children should brush their teeth later on and after all primary teeth have erupted. In this study, most of the mothers said they started brushing their children’s teeth after the eruption of the first primary teeth, in accordance with previous research [
4,
32,
50,
53,
56,
59]. In this study, nearly 75% of mothers said they started toothbrushing immediately after birth and at least after the eruption of the first primary teeth. Furthermore, previous research [
27,
32,
34,
60] suggests that caregivers may not have clear information about whether fluoride toothpaste is suitable for children under three years of age. In this study, half of the mothers reported using fluoride-free toothpaste and only 33.78% of children use fluoridated toothpaste. These findings were found to be low when compared with Elison et al.’s study [
29] in which all mothers reported they used fluoridated toothpaste. In a recent study, higher parental education level was found to be associated with the use of non-fluoridated dentifrice [
61].
In the study of Akshehri and Nasim [
4], 20.98% of the parents reported that they provided oral hygiene only with water, 27.87% with wet cotton, 28.20% with a toothbrush, and 10.16% with toothpaste. In another study [
38], it was reported that 32% of the parents used a toothbrush and toothpaste and 13.7% used finger brushes and toothpaste/powder in order to clean their children’s teeth. Sultan et al. [
52] reported that 81% of mothers preferred a toothbrush and toothpaste. In this study, it was determined that a toothbrush or finger brush without toothpaste was generally used among children aged 0–2 years. If toothpaste was used for children in this age group, fluoride-free paste was preferred. In our opinion, fluoride paste is not preferred by mothers because babies in this age group have a risk of swallowing paste, which can cause dental fluorosis. A recent review reported that children who start brushing with fluoride toothpaste after 24 months have a reduced risk of dental fluorosis compared to children who use fluoride toothpaste before 24 months of age [
62]. Brushing the child’s teeth twice a day with toothpaste containing at least 1000 ppm fluoride is very effective in reducing dental caries. The amount of paste appropriate for the age of the child should be used. This amount should be the size of a smear for children under 3 years old and a pea-grain-sized amount for children aged 3 to 6 years old [
59]. This knowledge is important for parents to avoid excess toothpaste ingestion [
49]. In this study, more than half of mothers reported that they used a smear layer of toothpaste and 43.8% used a pea-sized amount of toothpaste, which is line with previous studies [
40,
49,
50]. The results of the study of Wright et al. [
62] showed that usage of fluoridated toothpaste among children below 6 years of age is effective in caries control. However, researchers have reported that swallowing pea-sized amounts or larger can cause mild fluorosis. Furthermore, only 28% of all mothers applied professional fluoride varnish/gel to their children in the current study. Among the non-fluoride-applied group, the number of children between 0 and 2 years old was found to be statistically higher than those from other age groups. This may be due to the fact that the children of dentist mothers do not consume a cariogenic diet and the mothers regularly brush their babies’ teeth and that the mothers consider them to be in the low-caries-risk group as they are constantly under their control. Furthermore, dentist mothers understand the importance of mechanical plaque removal and may use other products including other remineralization agents rather than fluoride.
When toothbrushing frequency is examined, 49% of children brushed at least two times a day and nearly 6.5% brushed after each feeding. Also, 38.71% of children brushed their teeth once per day, only in the evening before bedtime in the current study. In other studies [
28,
31,
32,
34,
35,
40,
41,
52,
60,
63], toothbrushing was performed less than two times among most of the children. However, other researches [
24,
27,
29,
33,
46,
57,
64] has reported that toothbrushing was conducted at least two times a day among most of the children. Furthermore, tongue cleaning with a toothbrush or tongue cleaner has been reported to result in a significant reduction in streptococcus mutans count and plaque levels. Winnier et al. [
27] reported that 82.8% of the parents in their study regularly cleaned their child’s tongue. Similarly, in the current study, nearly 67% of the children’s tongue surface was brushed at least sometimes.
Parents’ behaviors and attitudes towards oral health can greatly affect their children’s oral-health-related behaviors [
8]. For example, if the parents brush their teeth twice a day, their children will be positively affected by brushing their teeth twice a day [
28]. Previous research [
65,
66,
67,
68,
69] has reported a direct relationship between children’s and mothers’ toothbrushing habits. During childhood, parents, especially the mother, play an important role in shaping the oral health behaviors of the child. Therefore, it can be said that consistent oral health behavior habits start to be acquired at home and parents should be informed that their own dental health habits affect their children’s oral health and, therefore, their quality of life [
68]. In accordance with the literature, in this study, nearly all of the mothers reported that their children accepted them as an example for their own toothbrushing habit and think that they are an example to their children about toothbrushing habits. In line with the literature, in the current study, it was detected that the mothers have good oral health and their children also have good oral health. Furthermore, the dental caries prevalence of dentist mothers’ children was low, as expected. It was clearly observed that the oral hygiene of the children was in a good condition as a result of their appropriate diet, good brushing habits, and constant oral check-ups by their dentist mothers.
It has been reported that supervised toothbrushing programs in schools improve the oral health of children [
70]. Although parents play the most important role in protecting their children’s oral health, children spend most of the day at school. For this reason, school teachers should also be included in the oral health education of children. Teachers can explain the importance of consuming less sugary foods and drinks to children and inform them about this issue [
68]. Parents, teachers, and dentists are mainly responsible for oral health good practices [
58]. In this study, it was found that only a limited number of children could brush their teeth at school, in line with the findings of Togoo et al. [
54]. So, most of the mothers in this study supported the development of toothbrushing protocol in order to promote toothbrushing at school under the supervision of teachers.
When the bad oral habits of the participating mothers’ children were examined, it was detected that a vast majority of children never used pacifiers and more than half did not need a pacifier during night sleep. However, it has been reported that pacifier use can decrease sudden infant death syndrome incidence and can be recommended to the mothers of healthy term infants when babies are nearly 3 to 4 weeks of age during infant nap or sleep time after breastfeeding [
71]. It was determined that the majority of the children participating in the current study did not have bad oral habits such as finger sucking, mouth breathing, bruxism, nail eating, lip biting, tongue thrusting, or lip sucking habits. Only 10.26% of children developed malocclusion due to bad oral habits. It is clear that mothers have the knowledge about the impact of oral bad habits on the developing dentition and jaws and they can apply their knowledge in practice. In previous studies, Al Jameel et al. [
39] reported that more than 86% of mothers, Jain et al. [
34] reported that 46.2% of parents, Sehrawat et al. [
32] reported that 33.1% of mothers, and Monahar and Mani [
28] reported that only 23% of the parents were educated about the consequences of oral habits such as tongue thrusting, mouth breathing, and thumb sucking on children’s developing dentition.
Another important aspect in the oral health promotion of young children is parental supervised toothbrushing. Children under the age of 7 should be closely supervised when brushing their teeth for several reasons. First, children only acquire the necessary cognitive and motor skills to brush their teeth in mid-childhood. The second is that young children’s mouths are very sensitive. Therefore, if children are left unattended while brushing their teeth, they can potentially cause damage to their mouths with their toothbrushes [
29]. Brushing teeth can be taught to children in the same way as any other skill. However, in order to ensure that all areas of the mouth are cleaned each time, it should be supervised closely on a regular basis [
56]. As children grow up, they acquire both fine and gross motor skills. Ogasawara et al. [
72] explained that the skill of learning to brush teeth and the establishment of the toothbrushing habit are two different things. They also suggested that children should be given constant guidance on brushing until their toothbrushing habits are embedded in their daily lives. Unfortunately, good oral hygiene in children is often difficult due to lack of motivation and poor dexterity [
72,
73]. The AAPD guidelines also state that parents should supervise their children’s brushing at least 8 years. The age of 7–8 is the point at which fine motor skills develop [
27]. In line with the literature, in this study, more than half of the mothers thought that they should brush their children’s teeth until at least 7–8 years old. In contrast, in the study of Gussy et al. [
50], 52% of the parents reported that, around the age of four years, their children were capable of brushing their own teeth. Unfortunately, those children who brushed their teeth alone had almost twice the amount of caries than children who were helped by parents [
49]. Almost all mothers who participated in our study at least supervised and 92.9% reported brushing the teeth of their children by themselves. In line with our finding, in previous studies [
5,
34,
46,
47,
49,
55,
73,
74], most of the parents were aware and adhered to supervised toothbrushing. However, the outcomes of some reports [
19,
28,
30,
35,
38,
44,
57,
64,
75] were not in accordance with our findings and showed a lack of knowledge and practice regarding parental supervised toothbrushing among most of the participant parents. Winnier et al. [
27] noted that 48.2% of parents agreed that the supervision of brushing is required until the age 7–8 years; however, about 67.1% of the respondents reported that making their children brush themselves was a tiring task.
It was found that parents frequently faced challenging behavior during toothbrushing when their children were between 18 and 24 months old. Those challenging behaviors of children included closing mouths, crying, and wanting to do the toothbrushing by themselves [
13]. Similar findings have been reported in the current study, where nearly 33% of mothers reported that they had the most difficulty during PSB when their children were between 1 and 2 years of age. Furthermore, in this study, nearly three quarters of the mothers found it easy and only one quarter found it hard to maintain their children’s oral health care in their daily routine. Similar findings were observed by Gussy et al. [
50], where 44% of parents expressed confidence in brushing their children’s teeth. Furthermore, in this study, almost all of the mothers said they had the greatest responsibility for ensuring their children’s oral hygiene, as in the study of Dadalto et al. [
24].
Dadalto et al. [
24] examined the toothbrushing behaviors of children aged 12–38 months at home. Collaborative children who showed co-operative and participatory behaviors comprised 58.4% of the sample. Researchers reported that noncollaborative behavior was more frequent when the mother had lower education and low family income and collaborative behavior was associated with higher maternal education. Similar to previous reports [
24,
53], in this study, most of the children showed co-operative and participant behaviors rather than resistant, uncooperative, and independent behaviors. Since the dentist mothers who participated in our study had high levels of education, the findings support the assumption of Dadalto et al. [
24]. Noncompliant, difficult behaviors were reported as the most common barrier to toothbrushing by 20% of mothers in the current study. In addition, the application of physical restraint to noncooperative children in order to properly brush their teeth was not preferred by most of the mothers in this study, as in previous studies [
29,
47]. Instead, almost all mothers thought that parents’ ability to manage children’s behavior (parental skills) and interpersonal communication skills are important in protecting children’s oral and dental health. In the study of Huebner and Riedy [
18], it was reported that mothers did not want to make their children upset and scared about toothbrushing in the future.
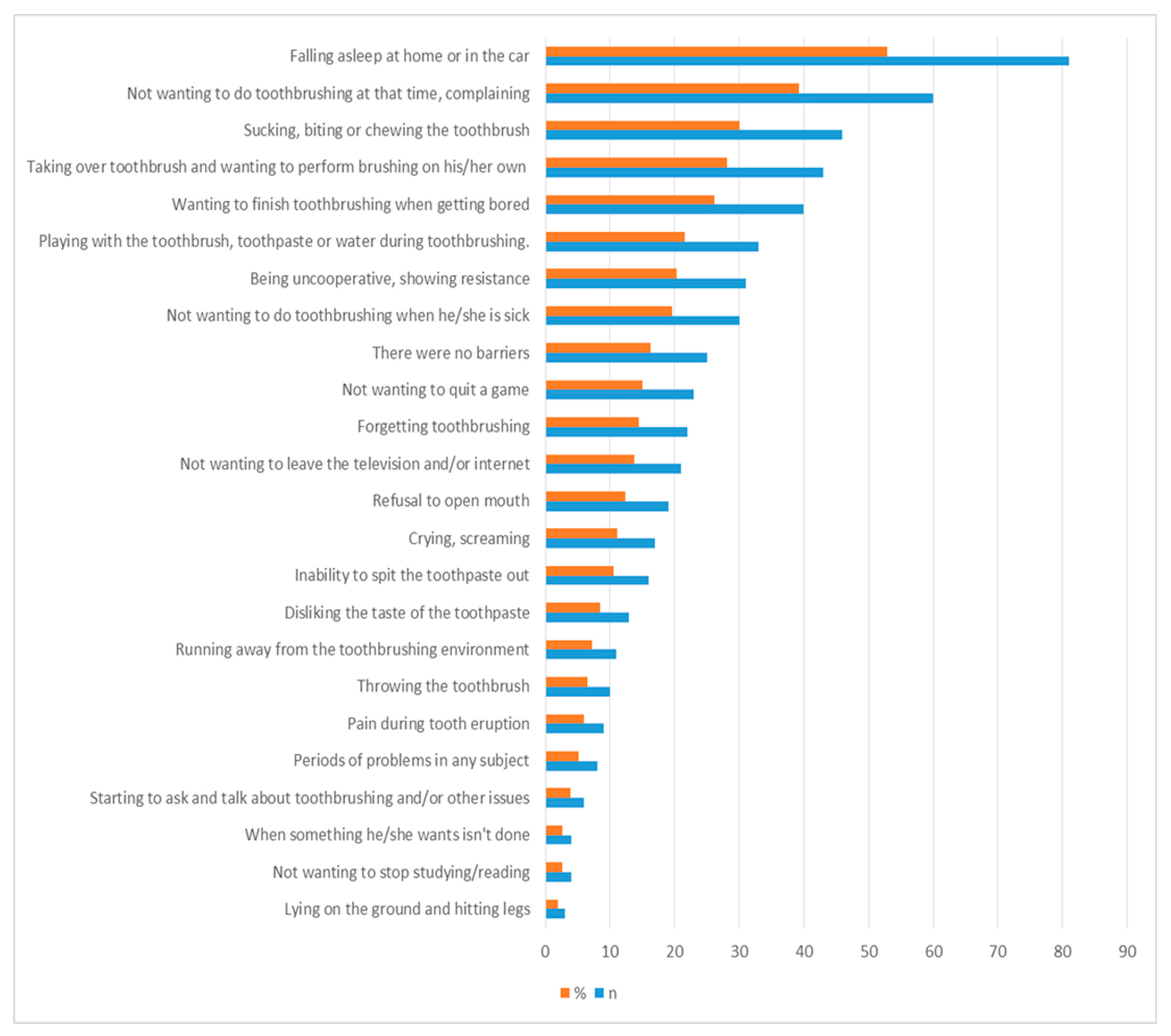
The most common barrier to toothbrushing related with children was falling asleep at home or in the car in the current study. The other barriers were children did not want to brush their teeth at that time, sucking, biting, or chewing the toothbrush during toothbrushing, taking over the toothbrush and wanting to perform brushing on their own, wanting to stop toothbrushing when they got bored, playing with the toothbrush, toothpaste, or water during toothbrushing, and not being co-operative and showing resistance and refusal to open the mouth, respectively. As reported in our study, barriers detected in previous studies included pain during teething [
47], tantrums [
47], playing with the toothbrush, toothpaste, or water during brushing [
76], taking over the toothbrush and wanting to perform the brushing on their own [
29], refusal to open their mouth [
29], falling asleep at home [
13,
29], disliking the taste of toothpaste [
29], throwing the toothbrush, lying on the ground, and hitting their legs [
13].
Additionally, there are also some barriers related with mothers in the oral health promotion of their young children. In this study, being tired was the most common barrier reported by dentist mothers. The other barriers were being outside the normal routine, not having enough time in the morning on the way to work, being sick, difficulties in guiding children’s behavior, and difficulties in controlling children, respectively. Twenty-eight percent of mothers stated that they experienced no barriers. Feeling confident and self-efficacy are some of the most important specialties in order to perform dyadic toothbrushing. In accordance with Duijster et al. [
47] and Huebner and Riedy [
18], nearly all mothers felt confident and had high self-efficacy in order to successfully establish toothbrushing for their children. Parenting skills, including manual skills and behavior management skills, are important to convince children when they do not want to brush [
13,
17,
26,
77,
78]. In the current study, only 14.8% mothers thought that they had to develop their parenting skills and only one mother felt her hand skills were not sufficient. As reported in our study, barriers also detected in previous studies were not having enough time in the morning on the way to work [
18,
29,
47], stress [
13,
29], forgetting the toothbrushing of their children [
13,
29], being outside the normal routine, such as on vacation or at the grandparents’ home [
77], and a lack of time [
32].
To overcome these mentioned barriers, parents should use facilitators in order to engage the child’s co-operation. In this study, the most common facilitator was brushing teeth together with the children. Being a model for the child during toothbrushing was also reported in the studies of Elison et al. [
29], Hubner and Riedy [
18], and Duijster et al. [
47]. Moreover, 31.8% of all mothers in our study included toothbrushing in the bedtime routine, as mentioned by previous studies [
29,
79]. Researchers [
29] have also reported that initiating toothbrushing as early as possible helps to establish a routine. Daily routinization of toothbrushing was also reported in previous studies [
13,
18,
29,
47]. As reported in our study, facilitators mentioned in previous studies included turning toothbrushing into a game [
18,
29], making sounds like ‘eee, aaa’ [
29], performing toothbrushing in order [
29], letting the child brush on their own if they do not allow the parent to brush [
13,
29], rewarding [
29], involvement of the father in toothbrushing with the mother [
29], explaining the importance of toothbrushing/consequences of not brushing [
18], singing a song to the children during toothbrushing [
18,
47], using a toothbrushing chart/sticker [
18,
47], choosing toothbrush/toothpaste that the children like, using reminders [
18], and praising the child’s toothbrushing [
47].
Strength and Limitations
To the best of our knowledge, this is the first study conducted on dentist mothers who understand the importance of primary teeth and have sufficient knowledge related to oral health. Online questionnaire studies have become one of the main survey methods used by researchers due to their ease of design and the advantages in terms of cost, time, and effort. By this way, it is possible to reach a much larger sample population by crossing geographical boundaries conducted over the internet [
80]. Thus, further studies conducted among various countries with larger sample size are encouraged. However, as an online questionnaire, this study has some limitations, such as lack of sufficiently motivating participants to respond, lack of opportunity for some participants to reach the questionnaire, being limited to internet users, and risk of participating without meeting the inclusion criteria.
This study included detailed information about early childhood caries and contributes by extensively highlighting the most important points about the oral health care of young children. It also encourages dentists to better understand the barriers/challenges faced by parents during parental supervised brushing (PSB) and summarizes the facilitators used in order to improve parental skills, self-efficacy, and achieve better PSB. We believe that this study can serve as a clinical guide for dentists in order to better motivate, educate, and promote preventive behavior shaping of the caregivers of baby/child patients.