The MapMe Body Scales: Validity and Reliability of a Biometrically Accurate, Photorealistic Set of Child Body Size Scales
Abstract
:1. Introduction
1.1. An Inability to Detect Unhealthy Weight in Children
1.2. How Can Visual Tools Help?
1.3. Study Rationale
2. Methods
2.1. Sample Size
2.2. Participants
2.3. Ethics and Pre-Registration
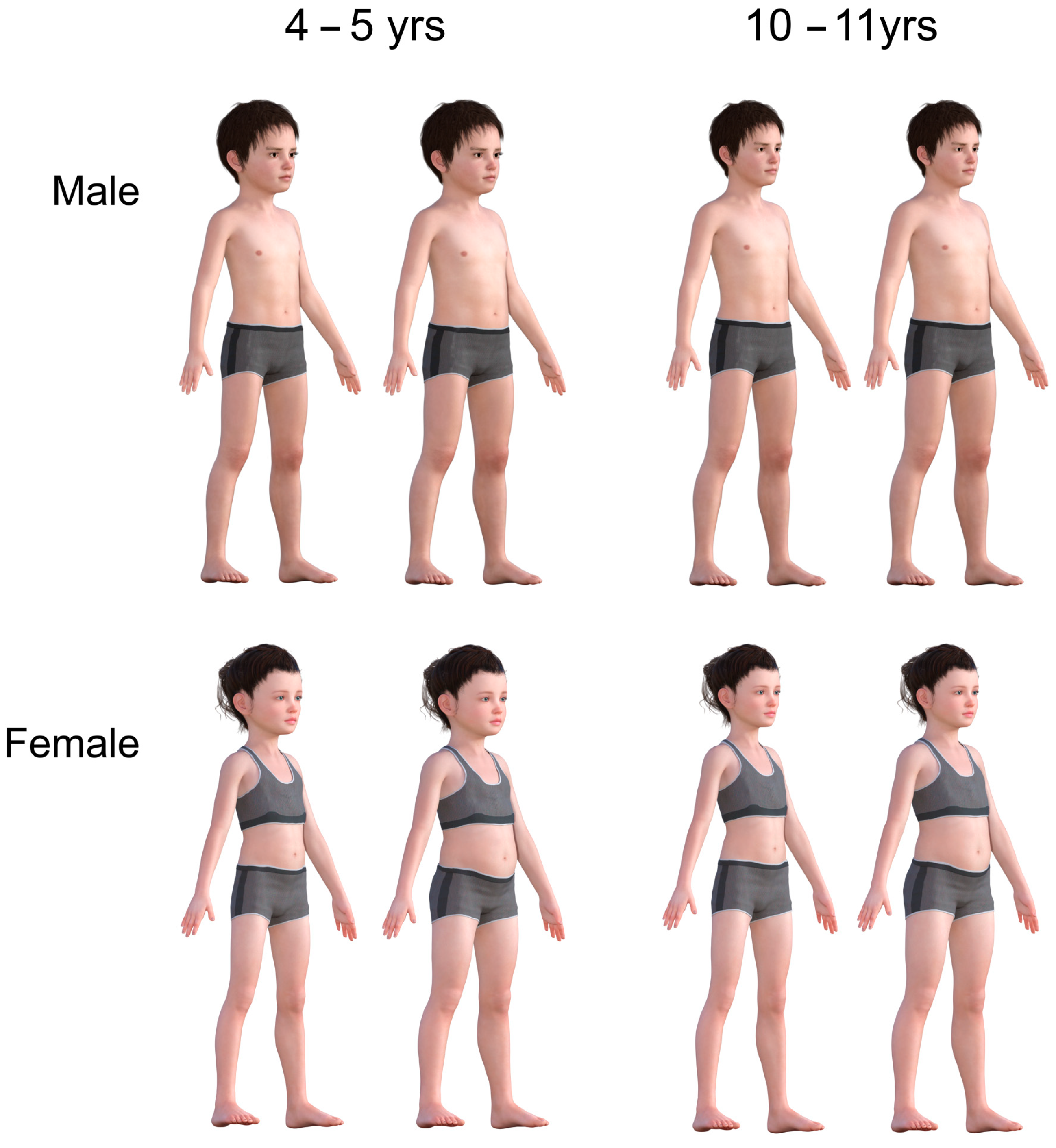
2.4. Stimulus Generation
2.5. Procedure
3. Results
3.1. Univariate Statistics
3.2. Validation of Stimuli: Rank Ordering
3.3. Validation of Stimuli: VAS Ratings
3.4. Test-Retest Reliability
4. Discussion
4.1. Summary of Findings
4.2. Future Directions
4.3. Study Strengths and Limitations
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Abarca-Gómez, L.; Abdeen, Z.A.; Hamid, Z.A.; Abu-Rmeileh, N.M.; Acosta-Cazares, B.; Acuin, C.; Adams, R.J.; Aekplakorn, W.; Afsana, K.; Aguilar-Salinas, C.A.; et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: A pooled analysis of 2416 population-based measurement studies in 128.9 million children, adolescents, and adults. Lancet 2017, 390, 2627–2642. [Google Scholar] [CrossRef] [PubMed]
- NCD Risk Factor Collaboration. Worldwide trends in underweight and obesity from 1990 to 2022: A pooled analysis of 3663 population-representative studies with 222 million children, adolescents, and adults. Lancet. 2024, 403, 1027–1050. [Google Scholar] [CrossRef] [PubMed]
- Sahoo, K.; Sahoo, B.; Choudhury, A.K.; Sofi, N.Y.; Kumar, R.; Bhadoria, A.S. Childhood obesity: Causes and consequences. J. Fam. Med. Prim. Care 2015, 4, 187. [Google Scholar] [CrossRef]
- Geserick, M.; Vogel, M.; Gausche, R.; Lipek, T.; Spielau, U.; Keller, E.; Pfäffle, R.; Kiess, W.; Körner, A. Acceleration of BMI in early childhood and risk of sustained obesity. N. Engl. J. Med. 2018, 379, 1303–1312. [Google Scholar] [CrossRef]
- Rankin, J.; Matthews, L.; Cobley, S.; Han, A.; Sanders, R.; Wiltshire, H.D.; Baker, J.S. Psychological consequences of childhood obesity: Psychiatric comorbidity and prevention. Adolesc. Health Med. Ther. 2016, 7, 125–146. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.C.; McPherson, K.; Marsh, T.; Gortmaker, S.L.; Brown, M. Health and economic burden of the projected obesity trends in the USA and the UK. Lancet 2011, 378, 815–825. [Google Scholar] [CrossRef]
- Caprio, S.; Daniels, S.R.; Drewnowski, A.; Kaufman, F.R.; Palinkas, L.A.; Rosenbloom, A.L.; Schwimmer, J.B. Influence of race, ethnicity, and culture on childhood obesity: Implications for prevention and treatment: A consensus statement of Shaping America’s Health and the Obesity Society. Diabetes Care 2008, 31, 2211. [Google Scholar] [CrossRef]
- Dobner, J.; Kaser, S. Body mass index and the risk of infection-from underweight to obesity. Clin. Microbiol. Infect. 2018, 24, 24–28. [Google Scholar] [CrossRef]
- Diaz, J.R.; De Las Cagigas, A.; Rodriguez, R. Micronutrient deficiencies in developing and affluent countries. Eur. J. Clin. Nutr. 2003, 57, S70–S72. [Google Scholar] [CrossRef]
- van Grieken, A.; Renders, C.M.; Wijtzes, A.I.; Hirasing, R.A.; Raat, H. Overweight, obesity and underweight is associated with adverse psychosocial and physical health outcomes among 7-year-old children: The ‘Be active, eat right’ study. PLoS ONE 2013, 8, e67383. [Google Scholar] [CrossRef]
- Berge, J.M.; Everts, J.C. Family-based interventions targeting childhood obesity: A meta-analysis. Child. Obes. 2011, 7, 110–121. [Google Scholar] [CrossRef] [PubMed]
- Ickes, M.J.; McMullen, J.; Haider, T.; Sharma, M. Global school-based childhood obesity interventions: A review. Int. J. Environ. Res. Public Health 2014, 11, 8940–8961. [Google Scholar] [CrossRef] [PubMed]
- Lukens, C.T.; Silverman, A.H. Systematic review of psychological interventions for pediatric feeding problems. J. Pediatr. Psychol. 2014, 39, 903–917. [Google Scholar] [CrossRef] [PubMed]
- Rhee, K.E.; De Lago, C.W.; Arscott-Mills, T.; Mehta, S.D.; Davis, R.K. Factors associated with parental readiness to make changes for overweight children. Pediatrics 2005, 116, e94–e101. [Google Scholar] [CrossRef] [PubMed]
- Lundahl, A.; Kidwell, K.M.; Nelson, T.D. Parental underestimates of child weight: A meta-analysis. Pediatrics 2014, 133, e689–e703. [Google Scholar] [CrossRef]
- Parry, L.L.; Netuveli, G.; Parry, J.; Saxena, S. A systematic review of parental perception of overweight status in children. J. Ambul. Care Manag. 2008, 31, 253–268. [Google Scholar] [CrossRef]
- Queally, M.; Doherty, E.; Matvienko-Sikar, K.; Toomey, E.; Cullinan, J.; Harrington, J.M.; Kearney, P.M. Do mothers accurately identify their child’s overweight/obesity status during early childhood? Evidence from a nationally representative cohort study. Int. J. Behav. Nutr. Phys. Act. 2018, 15, 56. [Google Scholar] [CrossRef]
- Benson, L.; Baer, H.J.; Kaelber, D.C. Trends in the diagnosis of overweight and obesity in children and adolescents: 1999–2007. Pediatrics 2009, 123, e153–e158. [Google Scholar] [CrossRef]
- Perrin, E.M.; Skinner, A.C.; Steiner, M.J. Parental recall of doctor communication of weight status: National trends from 1999 through 2008. Arch. Pediatr. Adolesc. Med. 2012, 166, 317–322. [Google Scholar] [CrossRef]
- Evans, E.H.; Tovée, M.J.; Hancock, P.J.; Cornelissen, P.L. How do looking patterns, anti-fat bias, and causal weight attributions relate to adults’ judgements of child weight? Body Image 2023, 44, 9–23. [Google Scholar] [CrossRef]
- Jones, A.R.; Tovée, M.J.; Cutler, L.R.; Parkinson, K.N.; Ells, L.J.; Araujo-Soares, V.; Pearce, M.S.; Mann, K.D.; Scott, D.; Harris, J.M.; et al. Development of the MapMe intervention body image scales of known weight status for 4–5 and 10–11-year-old children. J. Public Health 2018, 40, 582–590. [Google Scholar] [CrossRef] [PubMed]
- Edvardsson, K.; Edvardsson, D.; Hörnsten, Å. Raising issues about children’s overweight–maternal and child health nurses’ experiences. J. Adv. Nurs. 2009, 65, 2542–2551. [Google Scholar] [CrossRef] [PubMed]
- King, L.A.; Loss, J.H.; Wilkenfeld, R.L.; Pagnini, D.L.; Booth, M.L.; Booth, S.L. Australian GPs’ perceptions about child and adolescent overweight and obesity the Weight of Opinion study. Br. J. Gen. Pract. 2007, 57, 124–129. [Google Scholar] [PubMed]
- Tommerup, K.; Smith, A.D.; Evans, E.H.; Croker, H.; Steptoe, A.; Tovee, M.J.; Fildes, A.; Llewellyn, C. The acceptability and feasibility of using a 3D body size scale to initiate conversations about weight in toddlerhood: A mixed-methods study. Pediatr. Obes. 2021, 16, e12715. [Google Scholar] [CrossRef] [PubMed]
- MacTavish, K.; Cistrone, A.; Kingsnorth, S.; McPherson, A.C. Communication tools used in childhood obesity discussions: A scoping review. Child Care Health Dev. 2020, 46, 651–666. [Google Scholar] [CrossRef] [PubMed]
- Lakshman, R.; Landsbaugh, J.R.; Schiff, A.; Cohn, S.; Griffin, S.; Ong, K.K. Developing a programme for healthy growth and nutrition during infancy: Understanding user perspectives. Child Care Health Dev. 2012, 38, 675–682. [Google Scholar] [CrossRef] [PubMed]
- Flower, K.B.; Perrin, E.M.; Viadro, C.I.; Ammerman, A.S. Using body mass index to identify overweight children: Barriers and facilitators in primary care. Ambul. Pediatr. 2007, 7, 38–44. [Google Scholar] [CrossRef]
- Ben-Joseph, E.P.; Dowshen, S.A.; Izenberg, N. Do parents understand growth charts? A national, internet-based survey. Pediatrics 2009, 124, 1100–1109. [Google Scholar] [CrossRef]
- Sachs, M.; Sharp, L.; Bedford, H.; Wright, C.M. ‘Now I understand’: Consulting parents on chart design and parental information for the UK-WHO child growth charts. Child Care Health Dev. 2012, 38, 435–440. [Google Scholar] [CrossRef] [PubMed]
- Cloutier, M.M.; Lucuara-Revelo, P.; Wakefield, D.B.; Gorin, A.A. My Weight Ruler: A simple and effective tool to enhance parental understanding of child weight status. Prev. Med. 2013, 57, 550–554. [Google Scholar] [CrossRef]
- McPherson, A.C.; Hamilton, J.; Kingsnorth, S.; Knibbe, T.J.; Peters, M.; Swift, J.A.; Krog, K.; Chen, L.; Steinberg, A.; Ball, G.D.C. Communicating with children and families about obesity and weight-related topics: A scoping review of best practices. Obes. Rev. 2017, 18, 164–182. [Google Scholar] [CrossRef] [PubMed]
- Jain, A.; Sherman, S.N.; Chamberlin DL, A.; Carter, Y.; Powers, S.W.; Whitaker, R.C. Why don’t low-income mothers worry about their preschoolers being overweight? Pediatrics 2001, 107, 1138–1146. [Google Scholar] [CrossRef] [PubMed]
- Parkinson, K.N.; Drewett, R.F.; Jones, A.R.; Dale, A.; Pearce, M.S.; Wright, C.M.; Adamson, A.J. When do mothers think their child is overweight? Int. J. Obes. 2011, 35, 510–516. [Google Scholar] [CrossRef] [PubMed]
- Eckstein, K.C.; Mikhail, L.M.; Ariza, A.J.; Thomson, J.S.; Millard, S.C.; Binns, H.J.; Pediatric Practice Research Group. Parents’ perceptions of their child’s weight and health. Pediatrics 2006, 117, 681–690. [Google Scholar] [CrossRef]
- Hager, E.R.; McGill, A.E.; Black, M.M. Development and validation of a toddler silhouette scale. Obesity 2010, 18, 397–401. [Google Scholar] [CrossRef]
- Reifsnider, E.; Flores-Vela, A.R.; Beckman-Mendez, D.; Nguyen, H.; Keller, C.; Dowdall-Smith, S. Perceptions of children’s body sizes among mothers living on the Texas-Mexico Border (La Frontera). Public Health Nurs. 2006, 23, 488–495. [Google Scholar] [CrossRef]
- Yanover, T.; Thompson, J.K. Assessment of body image in children and adolescents. In Body Image, Eating Disorders, and Obesity in Youth: Assessment, Prevention, and Treatment, 2nd ed.; American Psychological Association: Washington, DC, USA, 2009; pp. 177–192. [Google Scholar] [CrossRef]
- Gardner, R.M.; Brown, D.L. Body image assessment: A review of figural drawing scales. Personal. Individ. Differ. 2010, 48, 107–111. [Google Scholar] [CrossRef]
- Cohn, L.D.; Adler, N.E.; Irwin, C.E.; Millstein, S.G.; Kegeles, S.M.; Stone, G. Body-figure preferences in male and female adolescents. J. Abnorm. Psychol. 1987, 96, 276–279. [Google Scholar] [CrossRef]
- Cornelissen, K.K.; Gledhill, L.J.; Cornelissen, P.L.; Tovée, M.J. Visual biases in judging body weight. Br. J. Health Psychol. 2016, 21, 555–569. [Google Scholar] [CrossRef]
- Cornelissen, P.L.; Cornelissen, K.K.; Groves, V.; McCarty, K.; Tovée, M.J. View-dependent accuracy in body mass judgements of female bodies. Body Image 2018, 24, 116–123. [Google Scholar] [CrossRef]
- Huang, J.S.; Becerra, K.; Oda, T.; Walker, E.; Xu, R.; Donohue, M.; Chen, I.; Curbelo, V.; Breslow, A. Parental ability to discriminate the weight status of children: Results of a survey. Pediatrics 2007, 120, e112–e119. [Google Scholar] [CrossRef] [PubMed]
- Truby, H.; Paxton, S.J. Development of the children’s body image scale. Br. J. Clin. Psychol. 2002, 41, 185–203. [Google Scholar] [CrossRef] [PubMed]
- Hudda, M.T.; Nightingale, C.M.; Donin, A.S.; Owen, C.G.; Rudnicka, A.R.; Wells, J.C.K.; Rutter, H.; Cook, D.G.; Whincup, P.H. Patterns of childhood body mass index (BMI), overweight and obesity in South Asian and black participants in the English National child measurement programme: Effect of applying BMI adjustments standardising for ethnic differences in BMI-body fatness associations. Int. J. Obes. 2018, 42, 662–670. [Google Scholar] [CrossRef]
- Nightingale, C.M.; Rudnicka, A.R.; Owen, C.G.; Cook, D.G.; Whincup, P.H. Patterns of body size and adiposity among UK children of South Asian, black African–Caribbean and white European origin: Child Heart And health Study in England (CHASE Study). Int. J. Epidemiol. 2011, 40, 33–44. [Google Scholar] [CrossRef]
- Maalin, N.; Mohamed, S.; Kramer, R.S.; Cornelissen, P.L.; Martin, D.; Tovée, M.J. Beyond BMI for self-estimates of body size and shape: A new method for developing stimuli correctly calibrated for body composition. Behav. Res. Methods 2021, 53, 1308–1321. [Google Scholar] [CrossRef]
- Faul, F.; Erdfelder, E.; Buchner, A.; Lang, A.G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behav. Res. Methods 2009, 41, 1149–1160. [Google Scholar] [CrossRef]
- Parkinson, K.N.; Jones, A.R.; Tovee, M.J.; Ells, L.J.; Pearce, M.S.; Araujo-Soares, V.; Adamson, A.J. A cluster randomised trial testing an intervention to improve parents’ recognition of their child’s weight status: Study protocol. BMC Public Health 2015, 15, 549. [Google Scholar] [CrossRef]
- Hudda, M.T.; Nightingale, C.M.; Donin, A.S.; Fewtrell, M.S.; Haroun, D.; Lum, S.; Williams, J.E.; Owen, C.G.; Rudnicka, A.R.; Wells, J.C.K.; et al. Body mass index adjustments to increase the validity of body fatness assessment in UK Black African and South Asian children. Int. J. Obes. 2017, 41, 1048–1055. [Google Scholar] [CrossRef]
- Wells, J.C.; Fewtrell, M.S. Is body composition important for paediatricians? Arch. Dis. Child. 2008, 93, 168–172. [Google Scholar] [CrossRef]
- Russian 3D Scanner. Wrap 3.3.17 [Computer Software]. 2018. Available online: https://www.russian3dscanner.com/ (accessed on 1 October 2024).
- Evans, E.H.; Tovée, M.J.; Boothroyd, L.G.; Drewett, R.F. Body dissatisfaction and disordered eating attitudes in 7-to 11-year-old girls: Testing a sociocultural model. Body Image 2013, 10, 8–15. [Google Scholar] [CrossRef]
- Public Health England. National Child Measurement Programme Operation Guidance 2024. 2024. Available online: https://www.gov.uk/government/publications/national-child-measurement-programme-operational-guidance/national-child-measurement-programme-operational-guidance-2024 (accessed on 22 April 2022).
- Wright, C.; Booth, I.W.; Buckler, J.M.H.; Cameron, N.; Cole, T.J.; Healy, M.J.R.; Hulse, J.A.; Preece, M.A.; Reilly, J.J.; Williams, A.F. Growth reference charts for use in the United Kingdom. Arch. Dis. Child. 2002, 86, 11–14. [Google Scholar] [CrossRef] [PubMed]
- Poulton, E.C. Bias in Quantifying Judgements; Erlbaum: Hove, UK, 2023. [Google Scholar]
- Bosker, R.; Snijders, T.A. Multilevel Analysis: An Introduction to Basic and Advanced Multilevel Modeling; SAGE: Newcastle upon Tyne, UK, 2011. [Google Scholar]
- Lorah, J. Effect size measures for multilevel models: Definition, interpretation, and TIMSS example. Large-Scale Assess. Educ. 2018, 6, 8. [Google Scholar] [CrossRef]
- Liljequist, D.; Elfving, B.; Skavberg Roaldsen, K. Intraclass correlation—A discussion and demonstration of basic features. PLoS ONE 2019, 14, e0219854. [Google Scholar] [CrossRef] [PubMed]
- Qin, S.; Nelson, L.; McLeod, L.; Eremenco, S.; Coons, S.J. Assessing test–retest reliability of patient-reported outcome measures using intraclass correlation coefficients: Recommendations for selecting and documenting the analytical formula. Qual. Life Res. 2019, 28, 1029–1033. [Google Scholar] [CrossRef]
- Jones, A.R.; Mann, K.D.; Cutler, L.R.; Pearce, M.S.; Tovée, M.J.; Ells, L.J.; Araujo-Soares, V.; Arnott, B.; Harris, J.M.; Adamson, A.J. A randomised control trial investigating the efficacy of the MapMe intervention on parental ability to correctly categorise overweight in their child and the impact on child BMI z-score change at 1 year. Children 2023, 10, 1577. [Google Scholar] [CrossRef]
- Collins, M.E. Body figure perceptions and preferences among preadolescent children. Int. J. Eat. Disord. 1991, 10, 199–208. [Google Scholar] [CrossRef]
- Mciza, Z.; Goedecke, J.H.; Steyn, N.P.; Charlton, K.; Puoane, T.; Meltzer, S.; Levitt, N.S.; Lambert, E.V. Development and validation of instruments measuring body image and body weight dissatisfaction in South African mothers and their daughters. Public Health Nutr. 2005, 8, 509–519. [Google Scholar] [CrossRef]
- Winkler, C.; Rhodes, G. Perceptual adaptation affects attractiveness of female bodies. Br. J. Psychol. 2005, 96, 141–154. [Google Scholar] [CrossRef]
- Rhodes, G.; Jeffery, L.; Boeing, A.; Calder, A.J. Visual coding of human bodies: Perceptual aftereffects reveal norm-based, opponent coding of body identity. J. Exp. Psychol. Hum. Percept. Perform. 2013, 39, 313–317. [Google Scholar] [CrossRef]
- Cornelissen, K.K.; Brokjøb, L.G.; Gumančík, J.; Lowdon, E.; McCarty, K.; Irvine, K.R.; Tovée, M.J.; Cornelissen, P.L. The Effect of Own Body Concerns on Judgments of Other Women’s Body Size. Front. Psychol. 2022, 13, 888904. [Google Scholar] [CrossRef]
- Gescheider, G.A. Psychophysical measurement of thresholds: Differential sensitivity. Psychophys. Fundam. 1997, 69, 1–15. [Google Scholar] [CrossRef]
- Jones, A.R.; Parkinson, K.N.; Drewett, R.F.; Hyland, R.M.; Pearce, M.S.; Adamson, A.J. Parental perceptions of weight status in children: The Gateshead Millennium Study. Int. J. Obes. 2011, 35, 953–962. [Google Scholar] [CrossRef] [PubMed]
- Nnyanzi, L.A. The National Child Measurement Programme: Its Value and Impact. Ph.D. Thesis, Teesside University, Middlesbrough, UK, 2012. [Google Scholar]
- Gauthier, I.; Tarr, M.J. Becoming a “Greeble” expert: Exploring mechanisms for face recognition. Vis. Res. 1997, 37, 1673–1682. [Google Scholar] [CrossRef] [PubMed]
- Gardner, R.M.; Friedman, B.N.; Jackson, N.A. Methodological concerns when using silhouettes to measure body image. Percept. Mot. Ski. 1998, 86, 387–395. [Google Scholar] [CrossRef]
- Doll, M.; Ball GD, C.; Willows, N.D. Rating of figures used for body image assessment varies depending on the method of figure presentation. Int. J. Eat. Disord. 2004, 35, 109–114. [Google Scholar] [CrossRef]
- Office for National Statistics. 2011 Census: Aggregate Data; [data collection]. UK Data Service. SN: 7427; Office for National Statistics: Newport Beach, CA, USA, 2020. [Google Scholar] [CrossRef]
- Choo, V. WHO reassesses appropriate body-mass index for Asian populations. Lancet 2002, 36, 235. [Google Scholar] [CrossRef]
- Chatham, R.E.; Mixer, S.J. Cultural influences on childhood obesity in ethnic minorities: A qualitative systematic review. J. Transcult. Nurs. 2020, 31, 87–99. [Google Scholar] [CrossRef]
- Peña, M.M.; Dixon, B.; Taveras, E.M. Are you talking to ME? The importance of ethnicity and culture in childhood obesity prevention and management. Child. Obes. 2012, 8, 23–27. [Google Scholar] [CrossRef]

| Women | Men | |||
|---|---|---|---|---|
| M | SD | M | SD | |
| Age (years) | 22.73 | 7.50 | 29.39 | 15.03 |
| BMI (kg/m2) | 23.70 | 5.49 | 25.10 | 4.08 |
| Genetic attribution | 43.15 | 19.71 | 31.50 | 19.70 |
| Overeating attribution | 66.12 | 17.99 | 67.97 | 20.37 |
| Inactivity attribution | 63.20 | 22.61 | 67.91 | 21.25 |
| R1 | R2 | R3 | R4 | R5 | R6 | R7 | |
|---|---|---|---|---|---|---|---|
| S1 | 92.1 | 6.4 | 0.8 | 0.3 | 0.3 | 0 | 0 |
| S2 | 5.7 | 83.9 | 7.6 | 2.1 | 0.3 | 0.1 | 0.3 |
| S3 | 1.2 | 6.7 | 78.4 | 10.6 | 2.1 | 0.6 | 0.4 |
| S4 | 0.3 | 2 | 10.4 | 74.3 | 9.6 | 1.7 | 1.8 |
| S5 | 0.3 | 0.6 | 1.6 | 9.7 | 64.4 | 15.2 | 8.1 |
| S6 | 0.1 | 0.4 | 0.8 | 2.4 | 14.9 | 54.1 | 27.2 |
| S7 | 0.1 | 0.1 | 0.4 | 0.4 | 8.4 | 28.3 | 62.3 |
| BMIc | ICC | 95% CI | Interpretation |
|---|---|---|---|
| 2 | 0.88 | 0.85–0.91 | Good |
| 25 | 0.74 | 0.67–0.81 | Good |
| 50 | 0.66 | 0.56–0.74 | Moderate |
| 75 | 0.63 | 0.52–0.71 | Moderate |
| 91 | 0.75 | 0.66–0.80 | Good |
| 98 | 0.86 | 0.82–0.90 | Good |
| 99.6 | 0.83 | 0.78–0.87 | Good |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ridley, B.J.; Evans, E.H.; Cornelissen, P.L.; Kramer, R.S.S.; Tovée, M.J. The MapMe Body Scales: Validity and Reliability of a Biometrically Accurate, Photorealistic Set of Child Body Size Scales. Children 2024, 11, 1243. https://doi.org/10.3390/children11101243
Ridley BJ, Evans EH, Cornelissen PL, Kramer RSS, Tovée MJ. The MapMe Body Scales: Validity and Reliability of a Biometrically Accurate, Photorealistic Set of Child Body Size Scales. Children. 2024; 11(10):1243. https://doi.org/10.3390/children11101243
Chicago/Turabian StyleRidley, Bethany J., Elizabeth H. Evans, Piers L. Cornelissen, Robin S. S. Kramer, and Martin J. Tovée. 2024. "The MapMe Body Scales: Validity and Reliability of a Biometrically Accurate, Photorealistic Set of Child Body Size Scales" Children 11, no. 10: 1243. https://doi.org/10.3390/children11101243
APA StyleRidley, B. J., Evans, E. H., Cornelissen, P. L., Kramer, R. S. S., & Tovée, M. J. (2024). The MapMe Body Scales: Validity and Reliability of a Biometrically Accurate, Photorealistic Set of Child Body Size Scales. Children, 11(10), 1243. https://doi.org/10.3390/children11101243






