Lifestyle Factors in Myopic Spanish Children
Abstract
1. Introduction
2. Materials and Methods
3. Results
3.1. Demographic Data
Homogeneity Analysis
3.2. Association between Myopia and Axial Length Rates with Lifestyle Factors
4. Discussion
4.1. Clinical Data
4.2. Demographic and Lifestyle Factors
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Modjtahedi, B.S.; Ferris, F.L.; Hunter, D.G.; Fong, D.S. Public Health Burden and Potential Interventions for Myopia. Ophthalmology 2018, 125, 628–630. Available online: https://www.embase.com/search/results?subaction=viewrecord&id=L2000644061&from=export (accessed on 27 October 2023). [CrossRef] [PubMed]
- Morgan, I.G.; French, A.N.; Ashby, R.S.; Guo, X.; Ding, X.; He, M.; Rose, K.A. The epidemics of myopia: Aetiology and prevention. In Progress in Retinal and Eye Research; Elsevier Ltd.: Amsterdam, The Netherlands, 2018; Volume 62, pp. 134–149. [Google Scholar]
- Resnikoff, S.; Jonas, J.B.; Friedman, D.; He, M.; Jong, M.; Nichols, J.J.; Ohno-Matsui, K.; Smith, E.L., III; Wildsoet., C.F.; Taylor, H.R.; et al. Myopia—A 21st century public health issue. In Investigative Ophthalmology and Visual Science; Association for Research in Vision and Ophthalmology Inc.: Rockville, MD, USA, 2019; Volume 60, pp. Mi–Mii. [Google Scholar]
- Lawrenson, J.G.; Shah, R.; Huntjens, B.; Downie, L.E.; Virgili, G.; Dhakal, R.; Verkicharla, P.K.; Li, D.; Mavi, S.; Kernohan, A.; et al. Interventions for myopia control in children: A living systematic review and network meta-analysis. Cochrane Database Syst. Rev. 2023, 2023, CD014758. [Google Scholar]
- Yam, J.C.; Zhang, X.J.; Kam, K.W.; Chen, L.J.; Tham, C.C.; Pang, C.P. Myopia control and prevention: From lifestyle to low-concentration atropine. The 2022 Josh Wallman Memorial Lecture. Ophthalmic Physiol. Opt. 2023, 43, 299–310. Available online: https://onlinelibrary.wiley.com/doi/full/10.1111/opo.13118 (accessed on 27 October 2023). [CrossRef] [PubMed]
- Flitcroft, D.I.; He, M.; Jonas, J.B.; Jong, M.; Naidoo, K.; Ohno-Matsui, K.; Rahi, J.; Resnikoff, S.; Vitale, S.; Yannuzzi, L. IMI—Defining and classifying myopia: A proposed set of standards for clinical and epidemiologic studies. Investig. Ophthalmol. Vis. Sci. 2019, 60, M20–M30. [Google Scholar] [CrossRef]
- Recko, M.; Stahl, E.D. Childhood myopia: Epidemiology, risk factors, and prevention. Mol. Med. 2015, 112, 116–121. [Google Scholar]
- Holden, B.A.; Fricke, T.R.; Wilson, D.A.; Jong, M.; Naidoo, K.S.; Sankaridurg, P.; Wong, T.Y.; Naduvilath, T.; Resnikoff, S. Global Prevalence of Myopia and High Myopia and Temporal Trends from 2000 through 2050. Ophthalmology 2016, 123, 1036–1042. [Google Scholar] [CrossRef]
- Williams, K.M.; Bertelsen, G.; Cumberland, P.; Wolfram, C.; Verhoeven, V.J.; Anastasopoulos, E.; Buitendijk, G.H.S.; Cougnard-Gregoire, A.; Creuzot-Garcher, C.; Erke, M.G.; et al. Increasing Prevalence of Myopia in Europe and the Impact of Education. Ophthalmology 2015, 122, 1489–1497. Available online: http://creativecommons.org/licenses/by/4.0/ (accessed on 29 September 2023). [CrossRef]
- IMI—Industry Guidelines and Ethical Considerations for Myopia Control Report—Search Results—PubMed. Available online: https://pubmed.ncbi.nlm.nih.gov/?term=IMI+–+Industry+Guidelines+and+Ethical+Considerations+for+Myopia+Control+Report (accessed on 2 March 2020).
- Gifford, K.L.; Richdale, K.; Kang, P.; Aller, T.A.; Lam, C.S.; Liu, Y.M.; Michaud, L.; Mulder, J.; Orr, J.B.; Rose, K.A.; et al. IMI—Clinical management guidelines report. Investig. Ophthalmol. Vis. Sci. 2019, 60, M184–M203. [Google Scholar] [CrossRef]
- Morgan, I.G.; Wu, P.C.; Ostrin, L.A.; Tideman, J.W.; Yam, J.C.; Lan, W.; Baraas, R.C.; He, X.; Sankaridurg, P.; Saw, S.-M.; et al. IMI Risk Factors for Myopia. Investig. Ophthalmol. Vis. Sci. 2021, 62, 3. Available online: https://pubmed.ncbi.nlm.nih.gov/33909035/ (accessed on 21 March 2023). [CrossRef]
- Jonas, J.B.; Ang, M.; Cho, P.; Guggenheim, J.A.; He, M.G.; Jong, M.; Logan, N.S.; Liu, M.; Morgan, I.; Ohno-Matsui, K.; et al. IMI Prevention of Myopia and Its Progression. Investig. Ophthalmol. Vis. Sci. 2021, 62, 6. Available online: https://pubmed.ncbi.nlm.nih.gov/33909032/ (accessed on 21 March 2023). [CrossRef]
- Galvis, V.; Tello, A.; Camacho, P.A.; Parra, M.M.; Merayo-Lloves, J. Bio-environmental factors associated with myopia: An updated review. Arch. Soc. Española Oftalmol. 2017, 92, 307–325. [Google Scholar] [CrossRef] [PubMed]
- Eppenberger, L.S.; Sturm, V. The role of time exposed to outdoor light for myopia prevalence and progression: A literature review. Clin. Ophthalmol. 2020, 14, 1875–1890. [Google Scholar] [CrossRef] [PubMed]
- Dhakal, R.; Shah, R.; Huntjens, B.; Verkicharla, P.K.; Lawrenson, J.G. Time spent outdoors as an intervention for myopia prevention and control in children: An overview of systematic reviews. Ophthalmic Physiol. Opt. 2022, 42, 545–558. [Google Scholar] [CrossRef] [PubMed]
- Hua, W.J.; Jin, J.X.; Wu, X.Y.; Yang, J.W.; Jiang, X.; Gao, G.P.; Tao, F.-B. Elevated light levels in schools have a protective effect on myopia. Ophthalmic Physiol. Opt. 2015, 35, 252–262. Available online: https://www.embase.com/search/results?subaction=viewrecord&id=L612844443&from=export (accessed on 20 April 2023). [CrossRef] [PubMed]
- Han, X.; Liu, C.; Chen, Y.; He, M. Myopia prediction: A systematic review. Eye 2022, 36, 921–929. Available online: https://pubmed.ncbi.nlm.nih.gov/34645966/ (accessed on 27 October 2023). [CrossRef] [PubMed]
- Martínez-Albert, N.; Bueno-Gimeno, I.; Gené-Sampedro, A. Risk Factors for Myopia: A Review. J. Clin. Med. 2023, 12, 6062. [Google Scholar] [CrossRef]
- Alvarez-Peregrina, C.; Martinez-Perez, C.; Villa-Collar, C.; González-Pérez, M.; González-Abad, A.; Sánchez-Tena, M.Á.; On Behalf of Grupo de Investigación Alain Afflelou. The Prevalence of Myopia in Children in Spain: An Updated Study in 2020. Int. J. Environ. Res. Public Health 2021, 18, 12375. Available online: https://pubmed.ncbi.nlm.nih.gov/34886101/ (accessed on 9 October 2023). [CrossRef]
- Alvarez-Peregrina, C.C.; Sanchez-Tena, M.A.M.A.; Martinez-Perez, C.C.; Villa-Collar, C.C. Prevalence and Risk Factors of Myopia in Spain. J. Ophthalmol. 2019, 2019, 1–7. [Google Scholar] [CrossRef]
- Fernández-Montero, A.; Olmo-Jimenez, J.M.; Olmo, N.; Bes-Rastrollo, M.; Moreno-Galarraga, L.; Moreno-Montañés, J.; Martínez-González, M.A. The impact of computer use in myopia progression: A cohort study in Spain. Prev. Med. 2015, 71, 67–71. [Google Scholar] [CrossRef]
- Tideman, J.W.L.; Polling, J.R.; Vingerling, J.R.; Jaddoe, V.W.V.; Williams, C.; Guggenheim, J.A.; Klaver, C.C.W. Axial length growth and the risk of developing myopia in European children. Acta Ophthalmol. 2018, 96, 301–309. Available online: https://www.embase.com/search/results?subaction=viewrecord&id=L619862104&from=export (accessed on 20 October 2023). [CrossRef]
- Matamoros, E.; Ingrand, P.; Pelen, F.; Bentaleb, Y.; Weber, M.; Korobelnik, J.F.; Souied, E.; Leveziel, N. Prevalence of Myopia in France. Medicine 2015, 94, e1976. Available online: https://www.embase.com/search/results?subaction=viewrecord&id=L608444586&from=export (accessed on 10 June 2023). [CrossRef] [PubMed]
- Rudnicka, A.R.; Kapetanakis, V.V.; Wathern, A.K.; Logan, N.S.; Gilmartin, B.; Whincup, P.H.; Cook, D.G.; Owen, C.G. Global Variations and Time trends in the Prevalence of Childhood Myopia, a Systematic Review and Quantitative Meta-Analysis: Implications for Aetiology and Early Prevention. Br. J. Ophthalmol. 2016, 100, 882–890. [Google Scholar] [CrossRef] [PubMed]
- Galvis, V.; Tello, A.; Rey, J.J.; Serrano-Gómez, S.; Prada, A.M. Estimation of ocular axial length with optometric parameters is not accurate. Contact Lens. Anterior Eye 2022, 45, 101448. [Google Scholar] [CrossRef]
- Mutti, D.O.; Hayes, J.R.; Mitchell, G.L.; Jones, L.A.; Moeschberger, M.L.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Twelker, J.D.; Zadnik, K. Refractive error, axial length, and relative peripheral refractive error before and after the onset of myopia. Investig. Ophthalmol. Vis. Sci. 2007, 48, 2510–2519. [Google Scholar] [CrossRef] [PubMed]
- Ojaimi, E.; Rose, K.A.; Smith, W.; Morgan, I.G.; Martin, F.J.; Mitchell, P. Methods for a population-based study of myopia and other eye conditions in school children: The Sydney myopia study. Ophthalmic Epidemiol. 2005, 12, 59–69. [Google Scholar] [CrossRef] [PubMed]
- Jos, R.; Sebastian, D.; Iribarren, R.; Lanca, C.; Saw, S.M. Axial growth and lens power loss at myopia onset in singaporean children. Investig. Ophthalmol. Vis. Sci. 2019, 60, 3091–3099. [Google Scholar]
- Verkicharla, P.K.; Kammari, P.; Das, A.V. Myopia progression varies with age and severity of myopia. PLoS ONE 2020, 15, e0241759. [Google Scholar] [CrossRef]
- Jones-Jordan, L.A.; Sinnott, L.T.; Chu, R.H.; Cotter, S.A.; Kleinstein, R.N.; Manny, R.E.; Mutti, D.O.; Twelker, J.D.; Zadnik, K.; CLEERE Study Group. Myopia progression as a function of sex, age, and ethnicity. Investig. Ophthalmol. Vis. Sci. 2021, 62, 36. [Google Scholar] [CrossRef]
- Tricard, D.; Marillet, S.; Ingrand, P.; Bullimore, M.A.; Bourne, R.R.A.; Leveziel, N. Progression of myopia in children and teenagers: A nationwide longitudinal study. Br. J. Ophthalmol. 2022, 106, 1104–1109. Available online: https://www.embase.com/search/results?subaction=viewrecord&id=L634493094&from=export (accessed on 10 September 2023). [CrossRef]
- Bullimore, M.A.; Lee, S.S.Y.; Schmid, K.L.; Rozema, J.J.; Leveziel, N.; Mallen, E.A.H.; Jacobsen, N.; Iribarren, R.; Verkicharla, P.K.; Polling, J.R.; et al. IMI—Onset and Progression of Myopia in Young Adults. Investig. Ophthalmol. Vis. Sci. 2023, 64, 2. [Google Scholar] [CrossRef]
- Jones, L.A.; Sinnott, L.T.; Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Zadnik, K. Parental history of myopia, sports and outdoor activities, and future myopia. Investig. Ophthalmol. Vis. Sci. 2007, 48, 3524–3532. [Google Scholar] [CrossRef] [PubMed]
- Mutti, D.O.; Mitchell, G.L.; Moeschberger, M.L.; Jones, L.A.; Zadnik, K. Parental myopia, near work, school achievement, and children’s refractive error. Investig. Ophthalmol. Vis Sci. 2002, 43, 3633–3640. [Google Scholar]
- Kurtz, D.; Hyman, L.; Gwiazda, J.E.; Manny, R.; Li, M.D.; Wang, Y.; Scheiman, M.; COMET Group. Role of parental myopia in the progression of myopia and its interaction with treatment in COMET children. Investig. Ophthalmol. Vis. Sci. 2007, 48, 562–570. [Google Scholar] [CrossRef] [PubMed]
- Chua, S.Y.L.; Sabanayagam, C.; Cheung, Y.B.; Chia, A.; Valenzuela, R.K.; Tan, D.; Wong, T.Y.; Cheng, C.Y.; Saw, S.M. Age of onset of myopia predicts risk of high myopia in later childhood in myopic Singapore children. Ophthalmic Physiol. Opt. 2016, 36, 388–394. [Google Scholar] [CrossRef]
- Bullimore, M.A.; Brennan, N.A. Myopia: An ounce of prevention is worth a pound of cure. Ophthalmic Physiol. Opt. 2023, 43, 116–121. [Google Scholar] [CrossRef] [PubMed]
- Mountjoy, E.; Davies, N.M.; Plotnikov, D.; Smith, G.D.; Rodriguez, S.; Williams, C.E.; Guggenheim, J.A.; Atan, D. Education and myopia: Assessing the direction of causality by mendelian randomisation. BMJ 2018, 361, k2022. [Google Scholar] [CrossRef] [PubMed]
- Dutheil, F.; Oueslati, T.; Delamarre, L.; Castanon, J.; Maurin, C.; Chiambaretta, F.; Baker, J.S.; Ugbolue, U.C.; Zak, M.; Lakbar, I.; et al. Myopia and Near Work: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2023, 20, 875. [Google Scholar] [CrossRef]
- Philipp, D.; Vogel, M.; Brandt, M.; Rauscher, F.G.; Hiemisch, A.; Wahl, S.; Guggenheim, J.A.; Atan, D. The relationship between myopia and near work, time outdoors and socioeconomic status in children and adolescents. BMC Public Health 2022, 22, 2058. [Google Scholar] [CrossRef]
- Dirani, M.; Crowston, J.G.; Wong, T.Y. From reading books to increased smart device screen time. Br. J. Ophthalmol. 2019, 103, 1–2. [Google Scholar] [CrossRef]
- Rideout, V. The Common Sense Census: Media Use by Tweens and Teens in America, A Common Sense Media Research Study, United States. 2015. Available online: https://www.icpsr.umich.edu/web/ICPSR/studies/38018/versions/V1 (accessed on 21 June 2021).
- Ip, J.M.; Saw, S.M.; Rose, K.A.; Morgan, I.G.; Kifley, A.; Wang, J.J.; Mitchell, P. Role of near work in myopia: Findings in a sample of Australian school children. Investig. Ophthalmol. Vis. Sci. 2008, 49, 2903–2910. [Google Scholar] [CrossRef]
- Enthoven, C.A.; Polling, J.R.; Verzijden, T.; Tideman, J.W.L.; Al-Jaffar, N.; Jansen, P.W.; Raat, H.; Metz, L.; Verhoeven, V.J.M.; Klaver, C.C.W. Smartphone Use Associated with Refractive Error in Teenagers: The Myopia App Study. Ophthalmology 2021, 128, 1681–1688. [Google Scholar] [CrossRef] [PubMed]
- Alvarez-Peregrina, C.; Sánchez-Tena, M.Á.; Martinez-Perez, C.; Villa-Collar, C. The Relationship Between Screen and Outdoor Time With Rates of Myopia in Spanish Children. Front. Public Health 2020, 8, 560378. [Google Scholar] [CrossRef]
- Lanca, C.; Yam, J.C.; Jiang, W.J.; Tham, Y.C.; Hassan Emamian, M.; Tan, C.S.; Guo, Y.; Liu, H.; Zhong, H.; Zhu, D.; et al. Near work, screen time, outdoor time and myopia in schoolchildren in the Sunflower Myopia AEEC Consortium. Acta Ophthalmol. 2022, 100, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Pärssinen, O.; Kauppinen, M. Associations of near work time, watching TV, outdoors time, and parents’ myopia with myopia among school children based on 38-year-old historical data. Acta Ophthalmol. 2022, 100, e430–e438. Available online: https://www.embase.com/search/results?subaction=viewrecord&id=L2013237647&from=export (accessed on 17 September 2023). [CrossRef] [PubMed]
- Rose, K.A.; Morgan, I.G.; Ip, J.; Kifley, A.; Huynh, S.; Smith, W.; Mitchell, P. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 2008, 115, 1279–1285. Available online: https://pubmed.ncbi.nlm.nih.gov/18294691/ (accessed on 21 March 2023). [CrossRef] [PubMed]
- Wu, P.C.; Tsai, C.L.; Wu, H.L.; Yang, Y.H.; Kuo, H.K. Outdoor activity during class recess reduces myopia onset and progression in school children. Ophthalmology 2013, 120, 1080–1085. Available online: https://pubmed.ncbi.nlm.nih.gov/23462271/ (accessed on 26 March 2021). [CrossRef] [PubMed]
- Xiong, S.; Sankaridurg, P.; Naduvilath, T.; Zang, J.; Zou, H.; Zhu, J.; Lv, M.; He, X.; Xu, X. Time spent in outdoor activities in relation to myopia prevention and control: A meta-analysis and systematic review. Acta Ophthalmol. 2017, 95, 551–566. [Google Scholar] [CrossRef] [PubMed]
- Németh, J.; Tapasztó, B.; Aclimandos, W.A.; Kestelyn, P.; Jonas, J.B.; De Faber, J.T.H.N.; Januleviciene, I.; Grzybowski, A.; Nagy, Z.Z.; Pärssinen, O.; et al. Update and guidance on management of myopia. European Society of Ophthalmology in cooperation with International Myopia Institute. Eur. J. Ophthalmol. 2021, 31, 853–883. Available online: https://www.embase.com/search/results?subaction=viewrecord&id=L2010705869&from=export (accessed on 2 June 2023). [CrossRef]
- Choi, K.Y.; Chan, S.S.H.; Chan, H.H.L. The effect of spatially-related environmental risk factors in visual scenes on myopia. Clin. Exp. Optom. 2022, 105, 353–361. [Google Scholar] [CrossRef]
- Smith, E.L.; Hung, L.F.; Huang, J. Protective effects of high ambient lighting on the development of form-deprivation myopia in rhesus monkeys. Investig. Ophthalmol. Vis Sci. 2012, 53, 421–428. [Google Scholar] [CrossRef]
- Foreman, J.; Salim, A.T.; Praveen, A.; Fonseka, D.; Ting, D.S.W.; Guang He, M.; Bourne, R.R.A.; Crowston, J.; Wong, T.Y.; Dirani, M. Association between digital smart device use and myopia: A systematic review and meta-analysis. Lancet Digit. Health 2021, 3, e806–e818. Available online: https://www.embase.com/search/results?subaction=viewrecord&id=L2015686557&from=export (accessed on 12 May 2023). [CrossRef] [PubMed]
| N (%) | |
|---|---|
| Prematurity | 24 (7.5) |
| Growth retardation | 22 (6.9) |
| Current medical treatment | 58 (18.1) |
| Ophthalmologic history | 21 (6.6) |
| Previous ocular surgery | 4 (1.2) |
| Parental myopia | |
| None | 128 (40.3) |
| Father or mother | 115 (36.2) |
| Both | 75 (23.6) |
| Previous myopia control treatment | 75 (23.7) |
| Iris color | |
| Blue | 9 (2.8) |
| Green | 23 (7.2) |
| Light brown | 41 (12.8) |
| Dark brown | 247 (77.2) |
| N (%) | |
|---|---|
| School performance | |
| Outstanding | 123 (39.3) |
| Adequate | 149 (47.6) |
| Mild and severe difficulty | 39 (12.5) |
| School schedule | |
| Split schedule | 136 (51.3) |
| Intensive schedule | 122 (46) |
| Mixed schedule | 6 (2.3) |
| Extracurricular activities | |
| None | 69 (26.1) |
| Outdoors | 54 (20.5) |
| Indoors | 102 (38.6) |
| Both | 39 (14.8) |
| Use of screens at school | 138 (43.7) |
| Near-work time | |
| (after school) | |
| <2 h | 176 (67.4) |
| >2 h | 85 (32.6) |
| Screen time (weekdays) | |
| <2 h | 143 (45.1) |
| >2 h | 174 (54.9) |
| Screen time (weekends) | |
| <2 h | 76 (24.1) |
| >2 h | 240 (75.9) |
| Time spent outdoors (weekdays) | |
| <1 h | 217 (68.2) |
| 1–2 h | 82 (25.8) |
| 2–4 h | 18 (5.7) |
| >4 h | 1 (0.3) |
| Time spent outdoors (weekends) | |
| <1 h | 89 (28.1) |
| 1–2 h | 131 (41.3) |
| 2–4 h | 89 (28.1) |
| >4 h | 8 (2.5) |
| Access to green spaces out of school | 166 (63.6) |
| Home lighting conditions | |
| Natural light conditions | 256 (80.8) |
| Ceiling illumination | 267 (84.2) |
| Desk lamp | 124 (39.5) |
| SER (D) | p-Value | AL (mm) | p-Value | |
|---|---|---|---|---|
| Medical background | ||||
| No | −2.11 ± 1.90 | 0.161 | 24.54 ± 0.97 | 0.341 |
| Yes | −2.50 ± 1.90 | 24.65 ± 0.82 | ||
| Prematurity | ||||
| No | −2.25 ± 1.90 | NA | 24.54 ± 0.96 | NA |
| Yes | −2.50 ± 1.97 | 24.50 ± 1.28 | ||
| Growth retardation | ||||
| No | −2.13 ± 1.85 | NA | 24.54 ± 0.97 | NA |
| Yes | −2.50 ± 2.28 | 24.44 ± 1 | ||
| Parental myopia | ||||
| None | −2.50 ± 1.82 | 24.61 ± 1.03 | 0.667 a | |
| Father or mother | −2.00 ± 1.91 | 0.057 | 24.56 ± 1.03 | 0.075 b |
| Both | −2.00 ± 2.00 | 24.36 ± 0.78 | ||
| Myopia onset age | ||||
| <10 years old | −2.50 ± 1.99 | p < 0.01 | 24.56± 0.96 | 0.873 |
| >10 years old | −1.75 ± 1.44 | 24.54 ± 1 | ||
| Previous ocular surgery | ||||
| No | −2.25 ± 1.89 | NA | 24.53 ± 0.98 | NA |
| Yes | −2.62 ± 3.07 | 24.94 ± 1.21 | ||
| Current medical treatment | ||||
| No | −2.25 ± 1.82 | 0.707 | 24.51 ± 1.02 | 0.341 |
| Yes | −1.87 ± 2.25 | 24.65 ± 0.82 | ||
| Ophthalmological history | ||||
| No | −2.25 ± 1.92 | NA | 24.54 ± 0.98 | NA |
| Yes | −2.00 ± 1.78 | 24.53 ± 1.13 | ||
| Previous myopia control treatment | ||||
| No | −1.75 ± 1.62 | p < 0.001 | 24.43 ± 0.96 | 0.002 |
| Yes | −3.00 ± 2.33 | 24.84 ± 1.01 | ||
| School performance | ||||
| Outstanding | −2.25 ± 2.00 | 24.50 ± 0.98 | 0.798 c | |
| Adequate | −2.25 ± 1.84 | 0.944 | 24.53 ± 0.96 | 0.511 d |
| Mild and severe difficulty | −2.25 ± 1.75 | 24.62 ± 0.95 | ||
| School schedule | ||||
| Split schedule | −2.00 ± 1.73 | 24.42 ± 0.84 | ||
| Intensive schedule | −2.00 ±1.95 | 0.537 | 24.5 ± 1.05 | 0.472 |
| Mixed schedule | −3.12 ± 1.85 | 24.92 ± 0.69 | ||
| Use of screens at school | ||||
| No | −2.00 ± 1.77 | 0.071 | 24.46 ± 1.01 | 0.135 |
| Yes | −2.50 ± 2.05 | 24.63 ± 0.96 | ||
| Extracurricular activities | ||||
| None | −2.50 ±1.84 | 0.590 | 24.42 ± 0.98 | 0.552 |
| Outdoors | −2.00 ± 2.20 | 24.66 ± 0.9 | ||
| Indoors | −2.00 ± 1.73 | 24.41 ± 0.93 | ||
| Both | −1.75 ± 1.49 | 24.43 ± 0.97 | ||
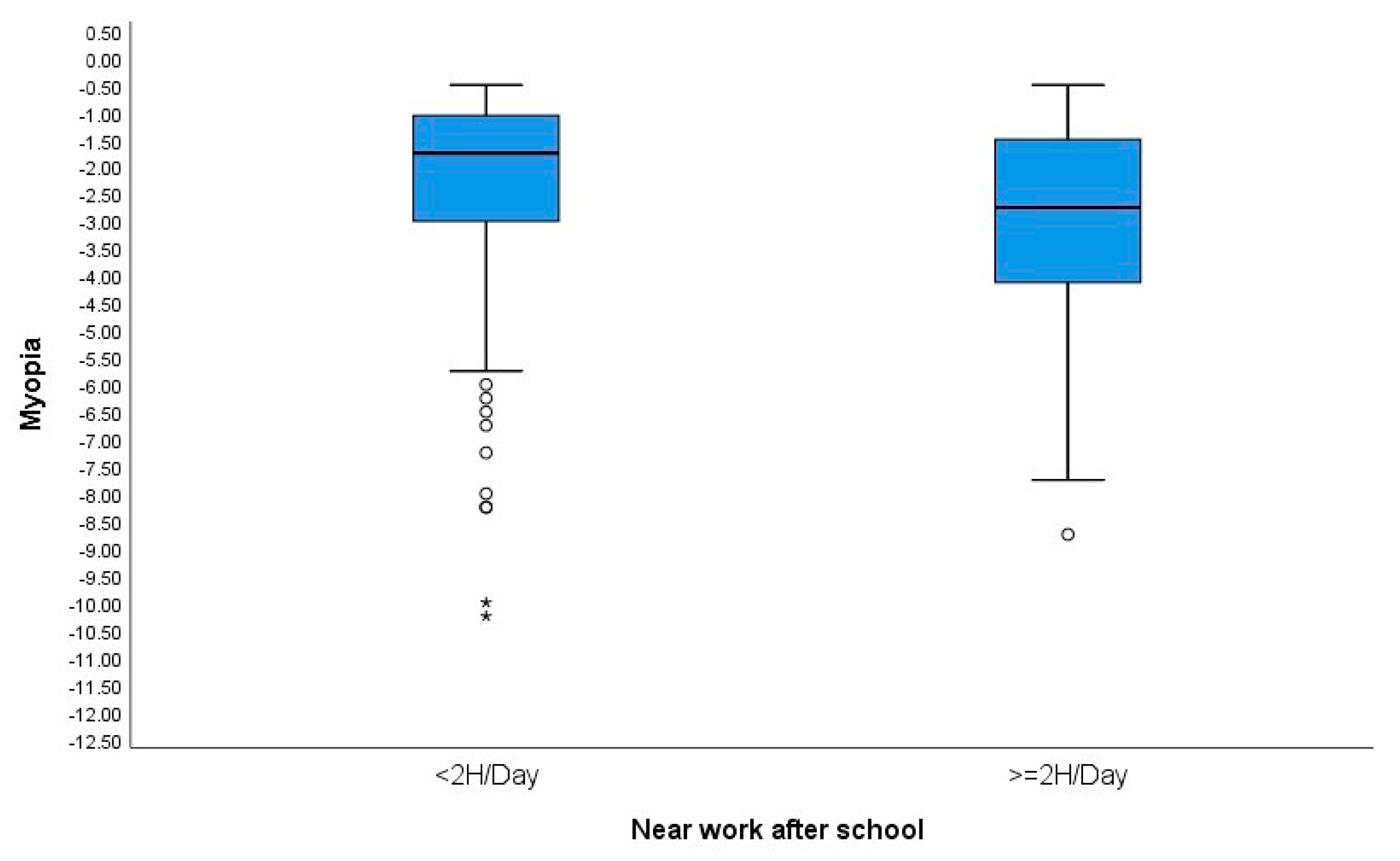
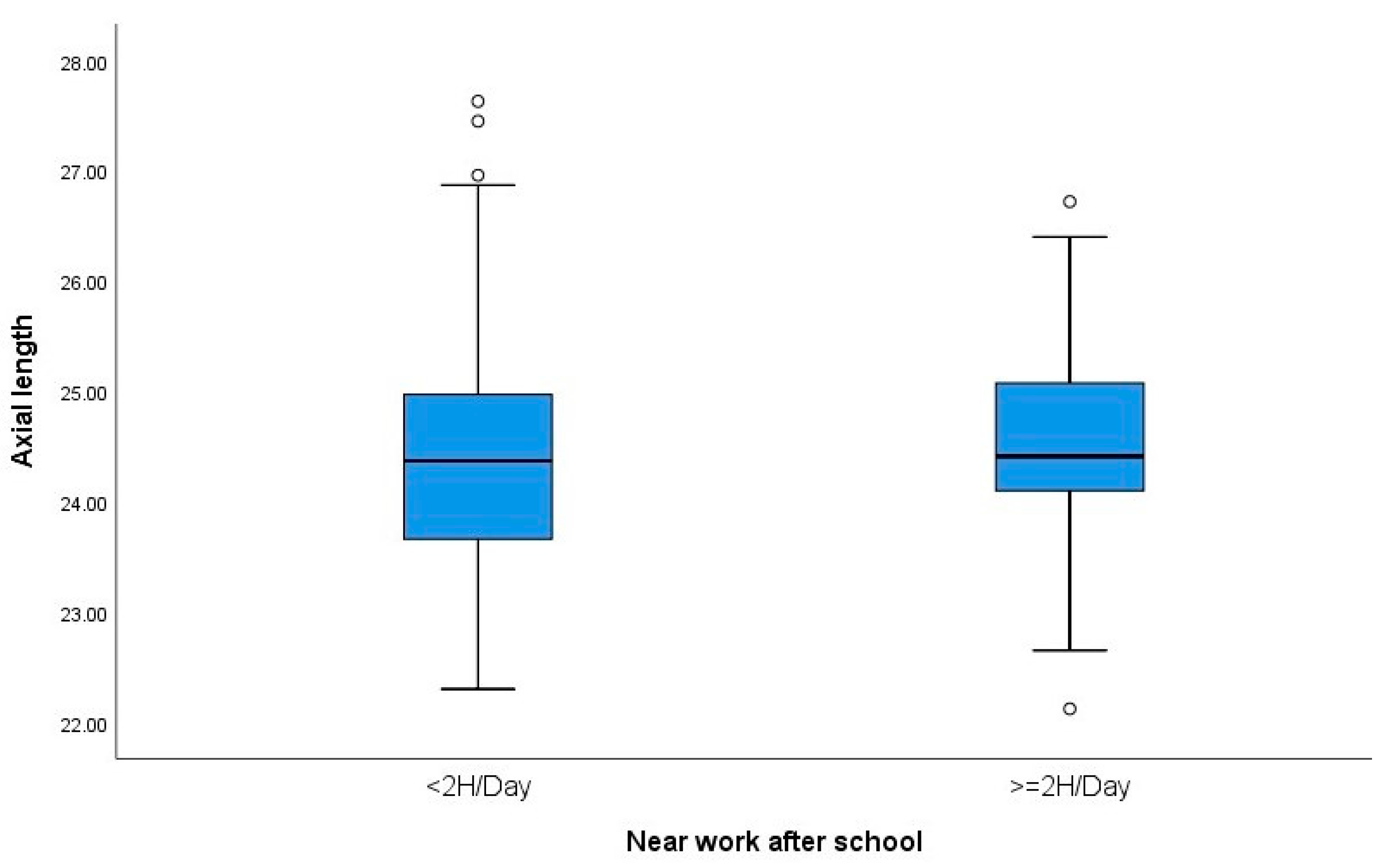
| Near-work time (after school) | ||||
| <2 h | −1.75 ± 1.83 | 0.03 | 24.45 ± 0.98 | 0.551 |
| >2 h | −2.75 ± 1.82 | 24.52 ± 0.86 | ||
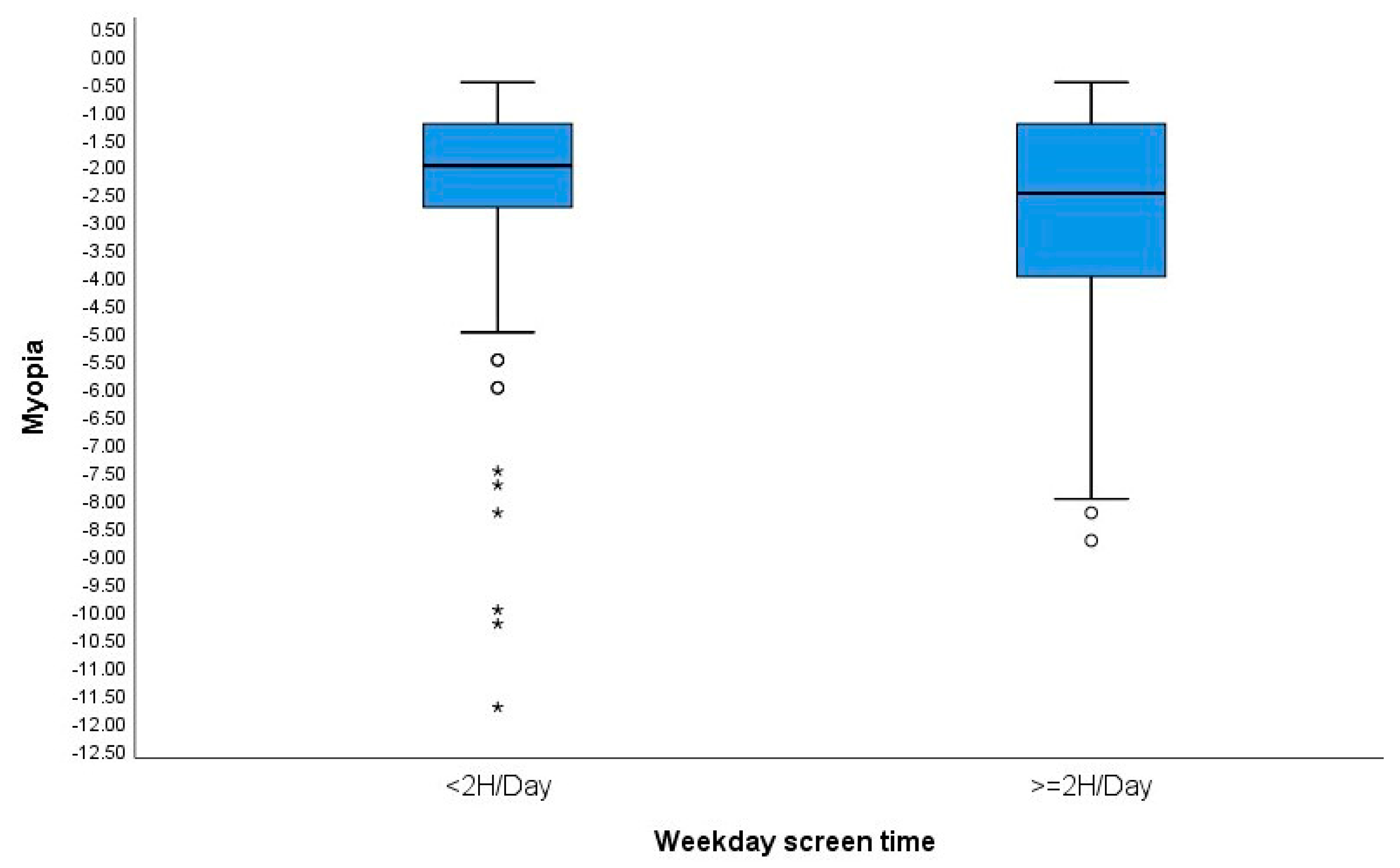
| Screen time (weekdays) | ||||
| <2 h | −2.00 ± 1.91 | 0.009 | 24.45 ± 1 | 0.172 |
| >2 h | −2.50 ± 1.88 | 24.6 ± 0.97 | ||
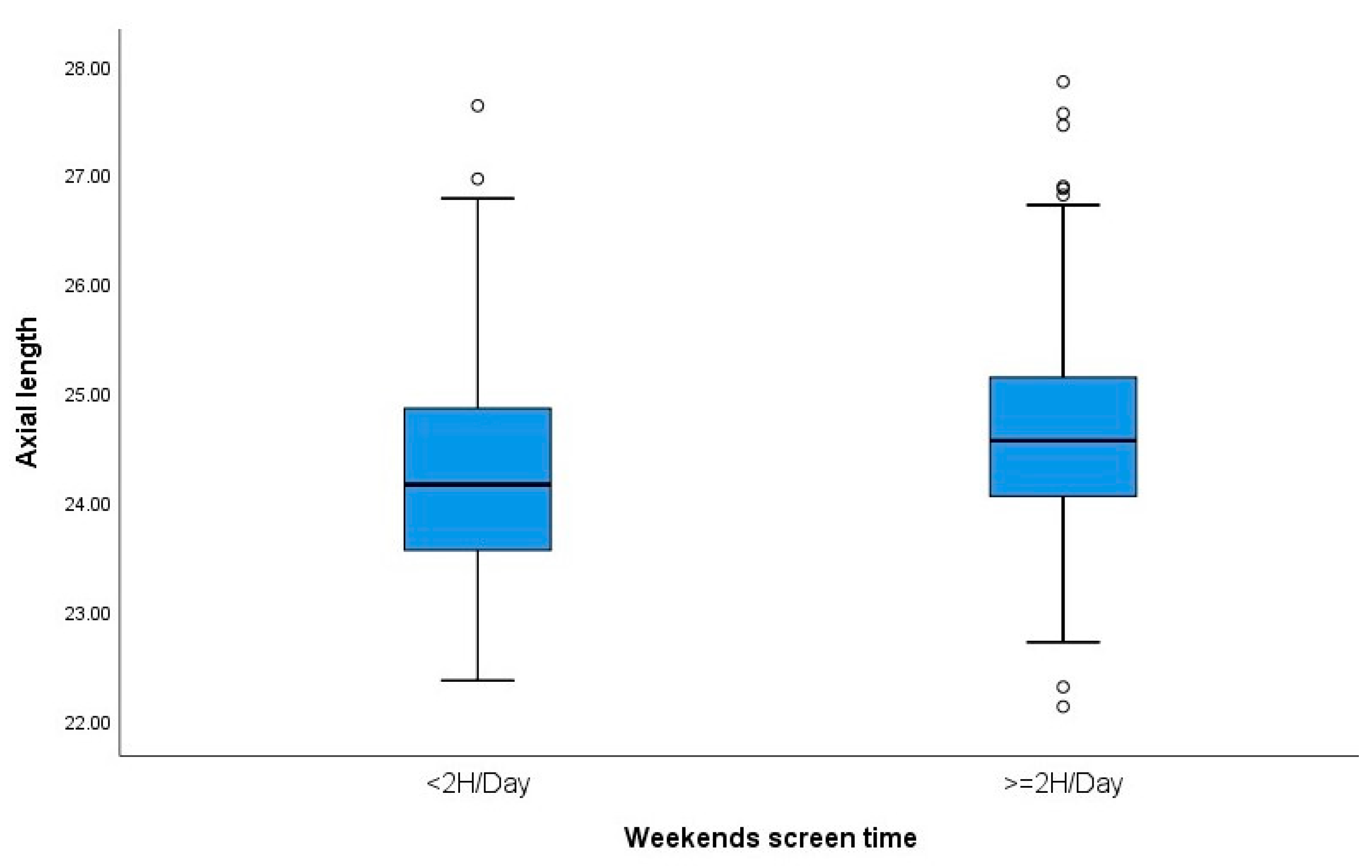
| Screen time (weekends) | ||||
| <2 h | −2.00 ± 2.30 | 0.218 | 24.33 ± 1.03 | 0.010 |
| >2 h | −2.25 ± 1.77 | 24.61 ± 0.96 | ||
| Time spent outdoors (weekday) | ||||
| <1 h 1 | −2.25 ± 1.71 | 0.994 | 24.51 ± 0.96 | 0.609 |
| 1–2 h | −2.00 ± 2.15 | 24.52 ± 1.08 | ||
| 2–4 h | −2.25 ± 2.72 | 24.77 ± 0.86 | ||
| >4 h | −4.50 | 25.11 | ||
| Time spent outdoors (weekends) | ||||
| <1 h | 2.25 ± 1.65 | 0.769 | 24.52 ± 1.06 | 0.297 |
| 1–2 h | −2.00 ± 2.05 | 24.6 ± 0.96 | ||
| 2–4 h | −2.00 ± 1.85 | 24.44 ± 0.94 | ||
| >4 h | −4.00 ± 1.68 | 24.44 ± 0.88 | ||
| Natural light conditions | ||||
| No | −2.25 ± 1.67 | 0.293 | 24.48 ± 1 | 0.622 |
| Yes | −2.00 ± 1.96 | 24.55 ± 0.98 | ||
| Ceiling illumination | ||||
| No | −2.31 ± 2.01 | 0.548 | 24.47 ± 1.03 | 0.613 |
| Yes | −2.25 ± 1.88 | 24.55 ± 0.98 | ||
| Desk lamp | ||||
| No | −2.00 ± 1.95 | 0.025 | 24.44 ± 0.99 | 0.02 |
| Yes | −2.37 ± 1.82 | 24.68 ± 0.97 | ||
| Access to green spaces outside school | ||||
| No | −2.25 ± 2.06 | 0.462 | 24.5 ± 0.96 | 0.751 |
| Yes | −2.00 ± 1.70 | 24.47 ± 0.92 | ||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Güemes-Villahoz, N.; Gómez de Liano, R.; Porras Ángel, P.; Talavero González, P.; Bella Gala, R.; Martín García, B.; Burgos Blasco, B.; Hernández García, E.; Chamorro Herrera, M.; Hernández-Verdejo, J.L.; et al. Lifestyle Factors in Myopic Spanish Children. Children 2024, 11, 139. https://doi.org/10.3390/children11020139
Güemes-Villahoz N, Gómez de Liano R, Porras Ángel P, Talavero González P, Bella Gala R, Martín García B, Burgos Blasco B, Hernández García E, Chamorro Herrera M, Hernández-Verdejo JL, et al. Lifestyle Factors in Myopic Spanish Children. Children. 2024; 11(2):139. https://doi.org/10.3390/children11020139
Chicago/Turabian StyleGüemes-Villahoz, Noemí, Rosario Gómez de Liano, Paloma Porras Ángel, Paula Talavero González, Rafael Bella Gala, Beatriz Martín García, Bárbara Burgos Blasco, Elena Hernández García, Marta Chamorro Herrera, José Luis Hernández-Verdejo, and et al. 2024. "Lifestyle Factors in Myopic Spanish Children" Children 11, no. 2: 139. https://doi.org/10.3390/children11020139
APA StyleGüemes-Villahoz, N., Gómez de Liano, R., Porras Ángel, P., Talavero González, P., Bella Gala, R., Martín García, B., Burgos Blasco, B., Hernández García, E., Chamorro Herrera, M., Hernández-Verdejo, J. L., & Ruiz-Pomeda, A. (2024). Lifestyle Factors in Myopic Spanish Children. Children, 11(2), 139. https://doi.org/10.3390/children11020139






