A National School Health Campaign in Lebanon on Children Aged between 3 and 12 Years Old: Concordance Level between Parents’ Reports and Medical Visit Findings about Physical and Mental Health
Abstract
:1. Introduction
2. Materials and Methods
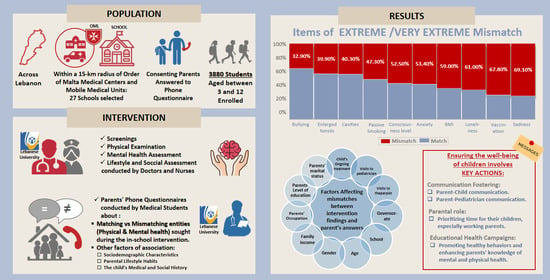
2.1. Study Design and Participants
- (1)
- The first step consists of the physical exam performed in schools by both a medical doctor and a nurse. Additionally, each child was interviewed in a private and suitable environment by the nurse to obtain information on their mental health. These interactions lasted approximately 10 to 15 min per student. This step occurred over the period of 14 November to 19 November 2022.
- (2)
- The second step entailed interviewing the parents of these children. These interviews were conducted over the phone by very well-trained representatives of our organization, which consisted of medical students. After obtaining the parents’ consent, the parents were asked to respond to a questionnaire dealing with the physical and mental state of their children, modeling aspects that medical doctors and nurses examined during the first step. The aim of this step was to determine the differences between findings during medical visits and data provided by students to nurses compared to parents’ responses. Our analytical study emphasizes this discordance. The interviews with parents took place within the first ten days of December 2022 and lasted for about thirty to thirty-five minutes per phone call. In comparing the information collected from children and their parents, we aimed to determine the key gaps/discrepancies in this study or how they could shape individual perceptions of reported health conditions.
2.2. Data Collection
2.3. Variables
2.4. Statistical Analysis
2.5. Ethical Consideration
3. Results
3.1. Socio-Demographic Characteristics
3.2. Mismatching and Their Socio-Demographic Factors
3.3. Category of Items of Very Extreme Mismatch and Their Socio-Demographic Determinants
3.3.1. Sadness
3.3.2. Incomplete Vaccination
3.3.3. Withdrawal/Loneliness
3.3.4. BMI
3.3.5. Anxiety/Worry
3.3.6. Level of Consciousness
3.4. Category of Items of Extreme Mismatch and Their Socio-Demographic Determinants
3.4.1. Oral Cavities/Enlarged Tonsils
3.4.2. Bullying
3.5. Category of Items of Moderate and Mild Mismatches
4. Discussion
4.1. Physical Health
4.1.1. Incomplete Vaccination
4.1.2. BMI
4.1.3. Oral Cavities/Enlarged Tonsils
4.1.4. Other Items (Vision Problems, Ear Problems, Skin Lesions, Apparent Skin Infection, Bad Posture, etc.)
4.2. Mental Health
4.2.1. Sadness
4.2.2. Withdrawal/Loneliness
4.2.3. Anxiety and Bullying
4.3. Strengths and Limitations
4.4. Perspectives
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Johnston, R.; Fowler, C.; Wilson, V.; Kelly, M. Opportunities for Nurses to Increase Parental Health Literacy: A Discussion Paper. Issues Compr. Pediatr. Nurs. 2015, 38, 266–281. [Google Scholar] [CrossRef] [PubMed]
- Morrison, A.K.; Glick, A.F.; Yin, H.S. Health Literacy: Implications for Child Health. Pediatr. Rev. 2019, 40, 263–277. [Google Scholar] [CrossRef] [PubMed]
- Sanders, L.; Shaw, J.S.; Guez, G.; Baur, C.; Rudd, R.E. Health Literacy and Child Health Promotion: Implications for Research, Clinical Care, and Public Policy. Pediatrics 2009, 124, S306–S314. [Google Scholar] [CrossRef] [PubMed]
- De Buhr, E.; Tannen, A. Parental Health Literacy and Health Knowledge, Behaviours and Outcomes in Children: A Cross-Sectional Survey. BMC Public Health 2020, 20, 1096. [Google Scholar] [CrossRef]
- Modern University of Business and Science. Supporting School Health in Disadvantaged Rural Areas in Bekaa and Southern Lebanon. Available online: https://www.mubs.edu.lb/Uploads/who_report.pdf (accessed on 14 February 2023).
- Institute of Medicine (US). Committee on Comprehensive School Health Programs in Grades K-12. In Schools & Health: Our Na-tion’s Investment Allensworth, 1st ed.; Allensworth, D., Lawson, E., Nicholson, L., Wyche, J., Eds.; National Academies Press: Washington, DC, USA, 1997. [Google Scholar] [CrossRef]
- Pomerantz, E.M.; Moorman, E.A.; Litwack, S.D. The How, Whom, and Why of Parents’ Involvement in Children’s Academic Lives: More Is Not Always Better. Rev. Educ. Res. 2007, 77, 373–410. [Google Scholar] [CrossRef]
- Martí, M.A.; Merz, E.C.; Repka, K.R.; Landers, C.; Noble, K.G.; Duch, H. Parent Involvement in the Getting Ready for School Intervention Is Associated with Changes in School Readiness Skills. Front. Psychol. 2018, 9, 759. [Google Scholar] [CrossRef]
- Hemmingsson, H.; Ólafsdóttir, L.B.; Egilson, S.Þ. Agreements and Disagreements between Children and Their Parents in Health-Related Assessments. Disabil. Rehabil. 2016, 39, 1059–1072. [Google Scholar] [CrossRef]
- Federico, A.; Shi, D.; Bradshaw, J. Agreement between Parental Report and Clinician Observation of Infant Developmental Skills. Front. Psychol. 2021, 12, 734341. [Google Scholar] [CrossRef]
- Poulain, T.; Vogel, M.; Meigen, C.; Spielau, U.; Hiemisch, A.; Kieß, W. Parent-Child Agreement in Different Domains of Child Behavior and Health. PLoS ONE 2020, 15, e0231462. [Google Scholar] [CrossRef]
- Killion, L.; Hughes, S.O.; Wendt, J.C.; Pease, D.; Nicklas, T.A. Minority Mothers’ Perceptions of Children’s Body Size. Int. J. Pediatr. Obes. 2006, 1, 96–102. [Google Scholar] [CrossRef]
- Ruiter, E.L.M.; Saat, J.J.E.H.; Molleman, G.; Fransen, G.A.J.; Van Der Velden, K.; Van Jaarsveld, C.H.M.; Engels, R.C.M.E.; Assendelft, W.J.J. Parents’ Underestimation of Their Child’s Weight Status. Moderating Factors and Change over Time: A Cross-Sectional Study. PLoS ONE 2020, 15, e0227761. [Google Scholar] [CrossRef]
- Williams, S.L.; Polaha, J. Rural Parents’ Perceived Stigma of Seeking Mental Health Services for Their Children: Development and Evaluation of a New Instrument. Psychol. Assess. 2014, 26, 763–773. [Google Scholar] [CrossRef]
- Weems, C.F.; Feaster, D.J.; Horigian, V.E.; Robbins, M.S. Parent and Child Agreement on Anxiety Disorder Symptoms Using the DISC Predictive Scales. Assessment 2010, 18, 213–216. [Google Scholar] [CrossRef]
- Save the Children. Bullying in Lebanon. Lebanon October 2018. Available online: https://lebanon.savethechildren.net/sites/lebanon.savethechildren.net/files/library/Bullying%20in%20Lebanon-%20Full%20research.pdf (accessed on 14 February 2023).
- Matta, P.; Mouallem, R.E.; Akel, M.; Hallit, S.; Khalife, M.-C.F. Parents’ Knowledge, Attitude and Practice towards Children’s Vaccination in Lebanon: Role of the Parent-Physician Communication. BMC Public Health 2020, 20, 1439. [Google Scholar] [CrossRef] [PubMed]
- Pediatric History & Physical Exam (Children Are Not Just Little Adults). Available online: https://www.ped.med.utah.edu/cai/howto/H&P%20write-up.pdf (accessed on 14 February 2023).
- Pediatric Health History Questionnaire. Available online: https://www.healthparkpediatrics.com/wp-content/uploads/2021/10/Initial-Health-Questionnaire.pdf (accessed on 14 February 2023).
- Initial History Questionnaire. Available online: https://morehousehealthcare.com/documents/pediatric-initial-history-questionnaire.pdf (accessed on 14 February 2023).
- Questionnaire Parental en vue de la Visite avec le Médecin de l’éducation Nationale. Available online: http://www.abdelmalek-sayad-nanterre.ac-versailles.fr/IMG/pdf/questionnaire_parent_visite_medicale.pdf (accessed on 14 February 2023).
- Fortin, M.-F.; Gagnon, J. Fondements et Etapes du Processus de Recherche: Méthodes Quantitatives et Qualitatives, 4th ed.; Chenelière éducation: Quebec, QC, Canada, 2016. [Google Scholar]
- McHugh, M.L. Interrater reliability: The kappa statistic. Biochem. Medica 2012, 22, 276–282. [Google Scholar] [CrossRef]
- Chmura Kraemer, H.; Periyakoil, V.S.; Noda, A. Kappa coefficients in medical research. Stat. Med. 2002, 21, 2109–2129. [Google Scholar] [CrossRef] [PubMed]
- World Medical Association. World Medical Association Declaration of Helsinki: Ethical principles for medical research involving human subjects. JAMA 2013, 310, 2191–2194. [Google Scholar] [CrossRef] [PubMed]
- Viera, A.J.; Garrett, J.M. Understanding interobserver agreement: The kappa statistic. Fam. Med. 2005, 37, 360–363. [Google Scholar] [PubMed]
- Habchy, P.; Tahan, L.; Moussi, C.; Barakat, M.A.; Ghanem, L.; Kattan, O.; Njeim, A.; Abou Habib, L.; El Bitar, W.; El Asmar, B.; et al. Referrals and Determinant Factors of a National School Health Campaign in Lebanon on Children Aged between 3 and 12 Years Old. Children 2024, 11, 175. [Google Scholar] [CrossRef]
- Sakai, Y. The Vaccination Kuznets Curve: Do Vaccination Rates Rise and Fall with Income? J. Health Econ. 2018, 57, 195–205. [Google Scholar] [CrossRef] [PubMed]
- Kanyi, L. Factors Influencing Knowledge and Attitude of Mothers Towards Immunization of Children Under-Five Years in Farato, Gambia. Texila Int. J. Public Health 2021, 9, 189–199. [Google Scholar] [CrossRef]
- Becker, M.H. The Health Belief Model and Sick Role Behavior. Health Educ. Monogr. 1974, 2, 409–419. [Google Scholar] [CrossRef]
- Karimy, M.; Armoon, B.; Fayazi, N.; Koohestani, H.R. A Study on the Knowledge, Attitude, and Practices of Iranian Mothers towards Childhood Obesity. Obes. Facts 2019, 12, 669–677. [Google Scholar] [CrossRef]
- Zoghby, H.B.; Sfeir, E.; Akel, M.; Malaeb, D.; Obeïd, S.; Hallit, S. Knowledge, Attitude and Practice of Lebanese Parents towards Childhood Overweight/Obesity: The Role of Parent-Physician Communication. BMC Pediatr. 2022, 22, 209. [Google Scholar] [CrossRef]
- Hood, N.; Colabianchi, N.; Terry-McElrath, Y.M.; O’Malley, P.M.; Johnston, L.D. Physical Activity Breaks and Facilities in US Secondary Schools. J. Sch. Health 2014, 84, 697–705. [Google Scholar] [CrossRef]
- Cooper, A.M.; O’Malley, L.; Elison, S.; Armstrong, R.; Burnside, G.; Adair, P.; Dugdill, L.; Pine, C.M. Primary School-Based Behavioural Interventions for Preventing Caries. Cochrane Database Syst. Rev. 2013, 5, CD009378. [Google Scholar] [CrossRef] [PubMed]
- Renouf, A.G.; Kovács, M. Concordance between Mothers’ Reports and Children’s Self-Reports of Depressive Symptoms: A Longitudinal Study. J. Am. Acad. Child Adolesc. Psychiatry 1994, 33, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Behere, A.P.; Basnet, P.; Campbell, P. Effects of Family Structure on Mental Health of Children: A Preliminary Study. Indian J. Psychol. Med. 2017, 39, 457–463. [Google Scholar] [CrossRef] [PubMed]
- Van Vulpen, K.S.; Habegar, A.; Simmons, T. Rural School-Based Mental Health Services: Parent Perceptions of Needs and Barriers. Child. Sch. 2018, 40, 104–111. [Google Scholar] [CrossRef]
- Kuebli, J.; Fıvush, R. Gender Differences in Parent-Child Conversations about Past Emotions. Sex Roles 1992, 27, 683–698. [Google Scholar] [CrossRef]
- Chaplin, T.M.; Aldao, A. Gender Differences in Emotion Expression in Children: A Meta-Analytic Review. Psychol. Bull. 2013, 139, 735–765. [Google Scholar] [CrossRef] [PubMed]
- Hossain, M.I.; Nasrin, N.; Halim, S.F.B.; Ahmed, S. Parental Awareness towards Child Health: A Study on the Parents of High School Students at Khulna City Corporation in Bangladesh. Khulna Univ. Stud. 2022, 17, 119–134. [Google Scholar] [CrossRef]
- Reuterskiöld, L.; Öst, L.; Ollendick, T.H. Exploring Child and Parent Factors in the Diagnostic Agreement on the Anxiety Disorders Interview Schedule. J. Psychopathol. Behav. Assess. 2008, 30, 279–290. [Google Scholar] [CrossRef]
- Matsunaga, M. Parents Don’t (Always) Know Their Children Have Been Bullied: Child-Parent Discrepancy on Bullying and Family-Level Profile of Communication Standards. Hum. Commun. Res. 2009, 35, 221–247. [Google Scholar] [CrossRef]
- Tes Magazine. Bullying Worse in Private Schools, New Research Shows 2020. Available online: https://www.tes.com/magazine/archive/bullying-worse-private-schools-new-research-shows (accessed on 14 February 2023).
- Girio-Herrera, E.; Owens, J.S.; Langberg, J.M. Perceived Barriers to Help-Seeking among Parents of At-Risk Kindergarteners in Rural Communities. J. Clin. Child Adolesc. Psychol. 2013, 42, 68–77. [Google Scholar] [CrossRef]
- Carlston, D.; Ogles, B.M. Age, Gender, and Ethnicity Effects on Parent–Child Discrepancy Using Identical Item Measures. J. Child Fam. Stud. 2008, 18, 125–135. [Google Scholar] [CrossRef]
- Canavera, K.; Wilkins, K.C.; Pincus, D.B.; Ehrenreich–May, J. Parent–Child Agreement in the Assessment of Obsessive-Compulsive Disorder. J. Clin. Child Adolesc. Psychol. 2009, 38, 909–915. [Google Scholar] [CrossRef]
- Beato-Fernández, L.; Barros, L.; Pereira, A.I. Father’s and Mother’s Beliefs about Children’s Anxiety. Child Care Health Dev. 2018, 44, 784–793. [Google Scholar] [CrossRef]




| Mismatch Percentage | |
|---|---|
| Very extreme | >50% |
| Extreme | 30–50% |
| Moderate | 15–30% |
| Mild | <15% |
| Frequency | Percentage | |||||
|---|---|---|---|---|---|---|
|
Nationality Total = 3380 | Lebanese Non-Lebanese | Syrian Palestinian Other | 3232 148 | 137 3 8 | 95.6 4.4 | 4.1 0.1 0.2 |
|
Gender Total = 3380 | Male Female | 1640 1740 | 48.5 51.5 | |||
|
Age Total = 3380 | 3–6 years 7–9 years 10–12 years | 1344 1012 1024 | 39.8 29.9 30.3 | |||
|
Body Mass Index (BMI) Total = 3380 | Underweight Normal weight Overweight | 1436 653 1291 | 42.5 19.3 38.2 | |||
|
School type Total = 3380 | Public Private | 1156 2224 | 34.2 65.8 | |||
|
OML community health facilities Total = 3380 | Medical Mobile Units (MMUs) Medical centers | 643 2737 | 19.0 81.0 | |||
|
Governorate Total = 3380 | Beirut Mount Lebanon North/Akkar Beqaa/Baalbek Hermel South | 187 758 797 712 926 | 5.5 22.4 23.6 21.1 27.4 | |||
|
Family Income Total = 2996 | No income <USD 100 USD 100–300 USD 300–600 USD 600–900 >USD 900 | 277 1231 332 902 227 27 | 9.2 41.1 11.1 30.1 7.6 0.9 | |||
|
Mother’s occupation Total = 3201 | No work Housewife Student Unemployed Employed Self-employed Retired Disabled Health field Other | 3 2251 16 88 589 134 9 2 76 33 | 0.1 70.3 0.5 2.7 18.4 4.2 0.3 0.1 2.4 1.0 | |||
|
Father’s Occupation Total = 3093 | No work Housewife Student Unemployed Employed Self-employed Retired Disabled Health field Other | 8 5 11 213 1343 1110 118 17 35 233 | 0.3 0.2 0.4 6.9 43.4 35.9 3.8 0.5 1.1 7.5 | |||
|
Mother’s level of education Total = 3242 | No education Primary Complementary Secondary Undergraduate University graduate | 73 399 722 705 436 907 | 2.3 12.3 22.3 21.7 13.4 28.0 | |||
|
Father’s level of education Total = 3118 | No education Primary Complementary Secondary Undergraduate University graduate | 132 592 955 703 283 453 | 4.2 19.0 30.6 22.5 9.1 14.5 | |||
|
Mother’s marital status Total = 3242 | Single Married Divorced Widowed | 97 3045 71 29 | 3.0 93.9 2.2 0.9 | |||
|
Father’s marital status Total = 3118 | Single Married Divorced Widowed | 46 3031 36 5 | 1.5 97.2 1.2 0.2 | |||
|
Mother’s smoking status Total = 3242 | Never Former Occasional Current | 1939 92 393 818 | 59.8 2.8 12.1 25.2 | |||
|
Father’s smoking status Total = 3118 | Never Former Occasional Current | 986 170 296 1666 | 31.6 5.5 9.5 53.4 | |||
|
Positive medical history Total = 2240 | No Yes | 1139 1101 | 50.8 49.2 | |||
|
Positive surgical history Total = 3379 | No Yes | 2949 430 | 87.3 12.7 | |||
|
Ongoing treatment Total = 1985 | No Yes | 1680 305 | 84.6 15.4 | |||
|
Child visit to the pediatrician/doctor Total = 1969 | No Yes | 412 1557 | 20.9 79.1 | |||
|
Previous child visit to the psychologist Total = 3339 | No Yes | 3196 143 | 95.7 4.3 | |||
|
Parent belief in the importance of medical examination at school Total = 1970 | No Yes Doesn’t know | 56 1893 21 | 2.8 96.1 1.1 | |||
| Physician’s Report/Nurse’s Interview | Parents’ Questionnaire | Mismatch Percentage | Kappa Value |
|---|---|---|---|
| How often have you been sad or stressed? | Does your child express sadness? | 69.1% | 0.008 |
| Referral for incomplete vaccination | Are your child’s vaccinations up to date? | 67.8% | 0.011 |
| How often have you felt lonely? | Is your child very shy or even withdrawn? | 61.0% | 0.007 |
| BMI (underweight, overweight) | Does your child have problems with nutrition? Do you think your child is of normal weight? Too skinny? Overweight/obese? | 59.0% | 0.03 |
| How often have you been so worried about something that you could not sleep at night? | Is your child often anxious? | 53.4% | 0.034 |
| Level of consciousness (attention, alertness, orientation…) | Does your child have now or recently had a problem of being alert and oriented? | 52.5% | −0.001 |
| Physician’s Report/Nurse’s Interview | Parents’ Questionnaire | Mismatch Percentage | Kappa Value |
|---|---|---|---|
| Were you subject to passive smoking in the last 7 days? | Does someone at home smoke in the presence of your child? | 47.3% | 0.103 |
| Oral examination—Cavities | Does your child have now or recently had cavities? | 40.3% | 0.228 |
| Oral examination—Enlarged tonsils | Does your child have now or recently had enlarged tonsils | 39.9% | 0.044 |
| During the past 30 days, how many days were you bullied? | Is your child bullied by people around them? | 32.9% | 0.078 |
| Physician’s Report/Nurse’s Interview | Parents’ Questionnaire | Mismatch Percentage | Kappa Value |
|---|---|---|---|
| Abnormal vision exam | Does your child have a vision problem that has already been detected? | 20.5% | 0.209 |
| Abnormal ear exam | Has your child had or still has recurrent ear infections? | 18.0% | −0.007 |
| Physician’s Report/Nurse’s Interview | Parents’ Questionnaire | Mismatch Percentage | Kappa Value |
|---|---|---|---|
| Infectious skin lesions (Mycosis, Impetigo, Scabies, etc.) | Does your child have any skin lesions? | 3% | 0.039 |
| Yellowish deposits (hypercholesterolemia) | Does your child have any yellowish deposits on the skin? | 0.8% | −0.001 |
| Enlarged node or/and organ | Does your child have now or recently had persistent swollen glands or lymph nodes? | 2.8% | 0.014 |
| Early or late pubertal stage | Has your child had or still have an early or late pubertal stage? | 3.1% | −0.010 |
| Motor system (Weakness, Paralysis, Unsteady Gait, etc.) | Does your child have now or recently had a weakness, paralysis, or an unsteady gait? | 10.9% | 0.011 |
| During the past 30 days, how many days did you have at least one drink containing alcohol? | Does your child drink alcohol? | 7.2% | −0.001 |
| During the past 30 days, how many days did you use tobacco products? | Does your child smoke? | 10.5% | −0.002 |
| Skin color (Pale, Cyanotic, etc.) | Does your child have now or recently had an abnormal skin color? | 5.2% | 0.022 |
| Posture (Lordosis, Kyphosis, Scoliosis) | Does your child have now or recently had a problem in his posture (scoliosis, etc.)? | 2.5% | 0.145 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tahan, L.; Habchy, P.; Moussi, C.; Khadra, T.; Jawich, M.; Njeim, A.; Kattan, O.; Abou Habib, L.; El Bitar, W.; El Asmar, B.; et al. A National School Health Campaign in Lebanon on Children Aged between 3 and 12 Years Old: Concordance Level between Parents’ Reports and Medical Visit Findings about Physical and Mental Health. Children 2024, 11, 214. https://doi.org/10.3390/children11020214
Tahan L, Habchy P, Moussi C, Khadra T, Jawich M, Njeim A, Kattan O, Abou Habib L, El Bitar W, El Asmar B, et al. A National School Health Campaign in Lebanon on Children Aged between 3 and 12 Years Old: Concordance Level between Parents’ Reports and Medical Visit Findings about Physical and Mental Health. Children. 2024; 11(2):214. https://doi.org/10.3390/children11020214
Chicago/Turabian StyleTahan, Léa, Peter Habchy, Charbel Moussi, Tia Khadra, Melissa Jawich, Alain Njeim, Ogarite Kattan, Leila Abou Habib, Wassim El Bitar, Béchara El Asmar, and et al. 2024. "A National School Health Campaign in Lebanon on Children Aged between 3 and 12 Years Old: Concordance Level between Parents’ Reports and Medical Visit Findings about Physical and Mental Health" Children 11, no. 2: 214. https://doi.org/10.3390/children11020214