Assessment of Sensory Processing Issues in Children with Neurodevelopmental Disorders and Experiences of Maltreatment
Abstract
:1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Data Collection
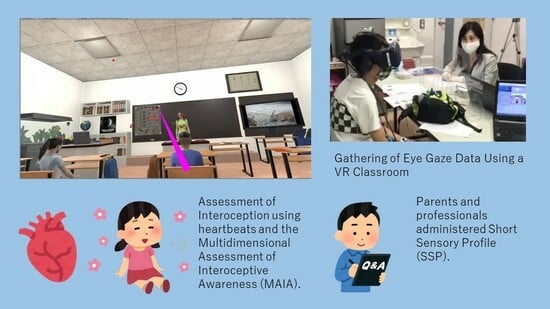
2.2.1. Gathering of Eye Gaze Data Using a VR Classroom
2.2.2. Short Sensory Profile
2.2.3. Interoception
2.2.4. Performance Test (Quiz)
2.3. Data Analysis
3. Results
3.1. Group Differences in Gaze (Table 2, Figure 1)
| Total (n = 24) | DM (n = 9) | DD (n = 8) | TD (n = 7) | |
|---|---|---|---|---|
| Characteristics | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD |
| Gazing time from 0 to 15 s (second) | ||||
| Teacher | 9.25 ± 3.50 | 8.01 ± 3.96 | 10.83 ± 3.33 | 9.05 ± 2.72 |
| p = 0.486 | ||||
| Notice | 1.17 ± 1.14 | 1.03 ± 1.36 | 0.98 ± 1.13 | 1.57 ± 0.89 |
| p = 0.432 | ||||
| Others | 4.58 ± 3.28 | 5.96 ± 3.63 | 3.19 ± 2.46 | 4.38 ± 3.35 |
| p = 0.350 | ||||
| Gazing time from 15 to 30 s (second) | ||||
| Teacher | 8.51 ± 3.95 | 8.04 ± 4.30 | 10.03 ± 3.96 | 7.39 ± 3.45 |
| p = 0.340 | ||||
| Notice | 1.48 ± 1.57 | 1.56 ± 2.02 | 1.23 ± 1.31 | 1.68 ± 1.35 |
| p = 0.842 | ||||
| Others | 5.01 ± 3.83 | 5.41 ± 3.67 | 3.74 ± 3.86 | 5.94 ± 4.19 |
| p = 0.395 | ||||
| Gazing time from 30 to 45 s (second) | ||||
| Teacher | 9.57 ± 3.75 | 8.79 ± 4.77 | 11.63 ± 2.36 | 8.21 ± 2.87 |
| p = 0.132 | ||||
| Notice | 1.11 ± 1.09 | 1.11 ± 1.34 | 0.87 ± 1.13 | 1.37 ± 0.70 |
| p = 0.332 | ||||
| Others | 4.33 ± 3.58 | 5.09 ± 4.23 | 2.51 ± 2.37 | 5.42 ± 3.47 |
| p = 0.161 | ||||
| Gazing time from 45 to 60 s (second) | ||||
| Teacher | 6.44 ± 3.68 | 3.76 ± 1.86 | 8.19 ± 4.12 | 7.86 ± 3.21 |
| KW = 6.394 | ||||
| p = 0.041 | ||||
| Notice | 2.30 ± 1.84 | 1.28 ± 1.90 | 2.71 ± 1.43 | 3.15 ± 1.77 |
| p = 0.080 | ||||
| Others | 6.26 ± 4.38 | 9.96 ± 2.41 | 4.10 ± 4.43 | 3.99 ± 3.21 |
| KW = 9.810 | DDM-DD = −9.458 | DTD-DM = −9.190 | ||
| p = 0.007 | pDM-DD = 0.018 | pTD-DM = 0.030 | ||
| Gazing time from 60 to 75 s (second) | ||||
| Teacher | 7.26 ± 3.24 | 4.92 ± 3.00 | 8.90 ± 2.47 | 8.38 ± 2.80 |
| KW = 7.138 | DDM-DD = 8.444 | |||
| p = 0.028 | pDM-DD = 0.042 | |||
| Notebook | 0.75 ± 0.95 | 0.14 ± 0.2 | 1.11 ± 1.21 | 1.13 ± 0.89 |
| p = 0.052 | ||||
| Others | 6.32 ± 3.14 | 8.14 ± 3.52 | 4.99 ± 2.48 | 5.49 ± 2.44 |
| p = 0.149 | ||||
| Quiz score | 78.33 ± 22.00 | 75.56 ± 21.86 | 70.00 ± 23.9 | 91.43 ± 15.74 |
| p = 0.145 | ||||

3.2. Difference in SSP (Table 3)
| Total (n = 24) | DM (n = 9) | DD (n = 8) | TD (n = 7) | |
|---|---|---|---|---|
| Characteristics | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD |
| SSP | ||||
| Tactile Sensitivity | 9.71 ± 2.27 | 8.33 ± 1.41 | 11.13 ± 1.81 | 9.86 ± 2.79 |
| KW = 6.912 | DDM-DD = 8.757 | |||
| p = 0.032 | pDM-DD = 0.028 | |||
| Taste/Smell Sensitivity | 6.42 ± 2.39 | 6.11 ± 1.62 | 8.38 ± 2.72 | 4.57 ± 0.79 |
| KW = 8.763 | DDD-TD = −10.643 | |||
| p = 0.013 | pDD-TD = 0.009 | |||
| Movement Sensitivity | 3.96 ± 1.46 | 3.33 ± 1.00 | 4.25 ± 1.75 | 4.43 ± 1.51 |
| KW = 4.494 | ||||
| p = 0.106 | ||||
| Under-Responsive/Seeks Sensation | 11.92 ± 5.06 | 11.67 ± 5.89 | 15.38 ± 3.89 | 8.29 ± 1.70 |
| KW = 9.492 | DDD-TD = −10.911 | |||
| p = 0.009 | pDD-TD = 0.007 | |||
| Auditory Filtering | 14.71 ± 6.17 | 14.33 ± 6.38 | 19.38 ± 3.58 | 9.86 ± 4.49 |
| KW = 9.474 | DDD-TD = −11.223 | |||
| p = 0.009 | pDD-TD = 0.006 | |||
| Low Energy/Weak | 12.96 ± 7.14 | 11.44 ± 7.45 | 17.38 ± 7.23 | 9.86 ± 4.45 |
| KW = 5.279 | ||||
| p = 0.071 | ||||
| Visual/Auditory Sensitivity | 7.13 ± 2.46 | 6.44 ± 2.01 | 8.75 ± 2.76 | 6.14 ± 1.86 |
| KW = 6.123 | ||||
| p = 0.047 | ||||
| SSP Total | 66.79 ± 19.67 | 61.67 ± 20.49 | 84.63 ± 8.96 | 53.00 ± 12.00 |
| KW = 12.325 | DDM-DD = 9.049 | DDD-TD = −12.152 | ||
| p = 0.002 | pDM-DD = 0.025 | pDD-TD = 0.003 | ||
3.3. Interoception Differences (Table 4)
| Total (n = 24) | DM (n = 9) | DD (n = 8) | TD (n = 7) | |
|---|---|---|---|---|
| Characteristics | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD |
| MAIA | ||||
| Noticing | 1.38 ± 1.15 | 1.17 ± 0.97 | 0.81 ± 1.01 | 2.29 ± 1.10 |
| KW = 5.844 | ||||
| p = 0.054 | ||||
| Not-Distracting | 3.11 ± 1.43 | 3.22 ± 1.51 | 3.25 ± 1.62 | 2.81 ± 1.26 |
| KW = 0.585 | ||||
| p = 0.746 | ||||
| Not-Worrying | 2.78 ± 0.98 | 2.93 ± 0.81 | 2.29 ± 1.09 | 3.14 ± 0.96 |
| KW = 1.708 | ||||
| p = 0.426 | ||||
| Attention Regulation | 1.79 ± 1.29 | 1.59 ± 1.22 | 1.27 ± 1.17 | 2.65 ± 1.22 |
| KW = 4.590 | ||||
| p = 0.101 | ||||
| Emotional Awareness | 2.87 ± 3.94 | 4.00 ± 6.20 | 1.45 ± 1.58 | 3.03 ± 0.86 |
| KW = 5.626 | ||||
| p = 0.06 | ||||
| Self-Regulation | 1.78 ± 1.40 | 1.72 ± 1.27 | 0.94 ± 0.81 | 2.83 ± 1.53 |
| KW = 6.904 | DDD-TD = 9.545 | |||
| p = 0.032 | pDD-TD = 0.027 | |||
| Body Listening | 1.26 ± 1.04 | 1.15 ± 0.82 | 0.58 ± 0.64 | 2.19 ± 1.09 |
| KW = 8.552 | DDD-TD = 10.536 | |||
| p = 0.014 | pDD-TD = 0.010 | |||
| Trust | 2.21 ± 1.53 | 1.93 ± 1.08 | 1.38 ± 1.69 | 3.52 ± 1.05 |
| KW = 8.366 | DDD-TD = 10.384 | |||
| p = 0.015 | pDD-TD = 0.013 | |||
| Interoception | 0.72 ± 0.16 | 0.56 ± 0.21 | 0.65 ± 0.18 | 0.81 ± 0.07 |
| KW = 6.074 | DTD-DM = 8.714 | |||
| p = 0.048 | pTD-DM = 0.043 |
3.4. Group Differences in Quizzes
4. Discussion
4.1. Gaze
4.2. SSP
4.3. Interoception
4.4. Limitations of This Study and Future Issues
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Fast, K.; Wentz, E.; Roswall, J.; Strandberg, M.; Bergman, S.; Dahlgren, J. Prevalence of attention-deficit/hyperactivity disorder and autism in 12-year-old children: A population-based cohort. Dev. Med. Child Neurol. 2023, 16, 1015749. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Education, Culture, Sports, Science and Technology. Results of a Survey on Students with Special Educational Needs in 2022. Available online: https://www.mext.go.jp/b_menu/houdou/2022/1421569_00005.htm (accessed on 27 November 2023).
- Ministry of Education, Culture Sports, Science and Technology. Results of a Survey on Students with Special Educational Needs in 2012. Available online: https://www.mext.go.jp/a_menu/shotou/tokubetu/hattatu.htm (accessed on 24 January 2024).
- Leitner, Y. The co-occurrence of autism and attention deficit hyperactivity disorder in children-what do we know? Front. Hum. Neurosci. 2014, 8, 268. [Google Scholar] [CrossRef] [PubMed]
- Hours, C.; Recasens, C.; Baleyte, J.-M. ASD and ADHD Comorbidity: What Are We Talking About? Front. Psychiatry 2022, 13, 837424. [Google Scholar] [CrossRef]
- WHO. Fact Sheets on Child Maltreatment. Available online: https://www.who.int/news-room/fact-sheets/detail/child-maltreatment (accessed on 20 January 2024).
- WHO. The Global Status Report on Preventing Violence against Children 2020. Available online: https://iris.who.int/bitstream/handle/10665/332394/9789240004191-eng.pdf?sequence=1 (accessed on 20 January 2024).
- Statistics Bureau, Ministry of Internal Affairs and Communications. Social Security, Tables 23–22. Japan Statistical Yearbook 2019. Available online: https://www.stat.go.jp/english/data/nenkan/72nenkan/1431-23.html (accessed on 27 November 2023).
- U.S. Department of Health & Human Services. The Children’s Bureau. Child Maltreatment 2021. Available online: https://www.acf.hhs.gov/sites/default/files/documents/cb/cm2021.pdf (accessed on 24 January 2024).
- Sullivan, P.M.; Knutson, J.F. Maltreatment and disabilities: A population-based epidemiological study. Child Abus. Negl. 2000, 24, 1257–1273. [Google Scholar] [CrossRef] [PubMed]
- Thornberry, C.; Olson, K. The Abuse of Individuals with Developmental Disabilities. Dev. Disabil. Bull. 2005, 33, 1–19. [Google Scholar]
- Samuel, D.; O’Malley, F.; Brink, F.W.; Crichton, K.G.; Duffy, B.; Letson, M.M.; Michaels, N.L. Characterizing child maltreatment fatalities among child victims with disabilities in the United States, 2010–2019. Child Abus. Negl. 2023, 144, 106354. [Google Scholar] [CrossRef] [PubMed]
- Ben-Sasson, A.; Hen, L.; Fluss, R.; Cermak, S.A.; Engel-Yeger, B.; Gal, E. A meta-analysis of sensory modulation symptoms in individuals with autism spectrum disorders. J. Autism Dev. Disord. 2009, 39, 1–11. [Google Scholar] [CrossRef]
- Ghanizadeh, A. Sensory processing problems in children with ADHD, a systematic review. Psychiatry Investig. 2011, 8, 89–94. [Google Scholar] [CrossRef]
- Joseph, R.Y.; Casteleijn, D.; van der Linde, J.; Franzsen, D. Sensory modulation dysfunction in child victims of trauma: A scoping review. J. Child Adolesc. Trauma 2021, 14, 455–470. [Google Scholar] [CrossRef]
- Atchison, B.J. Sensory modulation disorders among children with a history of trauma: A frame of reference for speech-language pathologists. Lang. Speech Hear. Serv. Sch. 2007, 38, 109–116. [Google Scholar] [CrossRef]
- Schafer, E.C.; Mathews, L.; Mehta, S.; Hill, M.; Munoz, A.; Bishop, R.; Moloney, M. Personal FM systems for children with autism spectrum disorders (ASD) and/or attention-deficit hyperactivity disorder (ADHD): An initial investigation. J. Commun. Disord. 2013, 46, 30–52. [Google Scholar] [CrossRef] [PubMed]
- Kojovic, N.; Ben Hadid, L.; Franchini, M.; Schaer, M. Sensory processing issues and their association with social difficulties in children with autism spectrum disorders. J. Clin. Med. 2019, 8, 1508. [Google Scholar] [CrossRef] [PubMed]
- Teicher, M.H.; Samson, J.A.; Anderson, C.M.; Ohashi, K. The effects of childhood maltreatment on brain structure, function and connectivity. Nat. Rev. Neurosci. 2016, 17, 652–666. [Google Scholar] [CrossRef] [PubMed]
- Muramatsu, K.; Hosaka, T. Current situations and issues in the Collaboration between Children’s homes and Elementary schools. Bull. Fac. Educ. Chiba Univ. 2016, 64, 123–131. [Google Scholar]
- Garfinkel, S.N.; Tiley, C.; O’Keeffe, S.; Harrison, N.A.; Seth, A.K.; Critchley, H.D. Discrepancies between dimensions of interoception in autism: Implications for emotion and anxiety. Biol. Psychol. 2016, 114, 117–126. [Google Scholar] [CrossRef] [PubMed]
- Ide-Okochi, A.; Matsunaga, N.; Sato, H. A preliminary study of assessing gaze, Interoception and school performance among children with neurodevelopmental disorders: The feasibility of VR classroom. Children 2022, 9, 250. [Google Scholar] [CrossRef] [PubMed]
- Ishizaki, Y.; Higuchi, T.; Yanagimoto, Y.; Kobayashi, H.; Noritake, A.; Nakamura, K.; Kaneko, K. Eye gaze differences in school scenes between preschool children and adolescents with high-functioning autism spectrum disorder and those with typical development. BioPsychoSocial Med. 2021, 15, 1–7. [Google Scholar] [CrossRef]
- Little, L.M.; Dean, E.; Tomchek, S.; Dunn, W. Sensory processing patterns in autism, attention deficit hyperactivity disorder, and typical development. Phys. Occup. Ther. Pediatr. 2018, 38, 243–254. [Google Scholar] [CrossRef]
- Ermer, J.; Dunn, W. The Sensory Profile: A discriminant analysis of children with and without disabilities. Am. J. Occup. Ther. 1998, 52, 283–290. [Google Scholar] [CrossRef]
- Ministry of Justice, Japan. Japanese Law Translation. Child Welfare Act (Act No. 164 of 1947). Available online: https://www.japaneselawtranslation.go.jp/ja/laws/view/4035#je_ch3at33 (accessed on 24 January 2024).
- Kocha, H. The use of operational criteria for evaluations of mental competency. Psychiatr. Neurol. Jpn. 2013, 115, 1057–1063. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders: DSM-5; American Psychiatric Publishing Inc.: Washington, DC, USA, 2013. [Google Scholar]
- Dunn, W. The Sensory Profile; The Psychological Corporation: San Antonio, TX, USA, 1999. [Google Scholar]
- Tani, I.; Ito, H.; Hirashima, T.; Iwanaga, R.; Hagiwara, T.; Yukihiro, R.; Uchiyama, T.; Ogasawara, M.; Kuroda, M.; Inada, N.; et al. Standardization of the Japanese Version of the Short Sensory Profile: Reliability and validity. Clin. Psychiatry 2015, 57, 419–429. [Google Scholar]
- Schandry, R. Heart beat perception and emotional experience. Psychophysiology 1981, 18, 483–488. [Google Scholar] [CrossRef] [PubMed]
- Mehling, W.E.; Price, C.; Daubenmier, J.J.; Acree, M.; Bartmess, E.; Stewart, A. The multidimensional assessment of interoceptive awareness (MAIA). PLoS ONE 2012, 7, e48230. [Google Scholar] [CrossRef] [PubMed]
- Shoji, M.; Mehling, W.E.; Hautzinger, M.; Herbert, B.M. Investigating multidimensional interoceptive awareness in a Japanese population: Validation of the Japanese MAIA-J. Front. Psychol. 2018, 9, 1855. [Google Scholar] [CrossRef] [PubMed]
- Tomoda, A.; Suzuki, H.; Rabi, K.; Sheu, Y.-S.; Polcari, A.; Teicher, M.H. Reduced prefrontal cortical gray matter volume in young adults exposed to harsh corporal punishment. Neuroimage 2009, 47, T66–T71. [Google Scholar] [CrossRef] [PubMed]
- Dupuis, A.; Mudiyanselage, P.; Burton, C.L.; Arnold, P.D.; Crosbie, J.; Schachar, R.J. Hyperfocus or flow? Attentional strengths in autism spectrum disorder. Front. Psychiatry 2022, 13, 886692. [Google Scholar] [CrossRef] [PubMed]
- Isomura, T.; Ogawa, S.; Shibasaki, M.; Masataka, N. Delayed disengagement of attention from snakes in children with autism. Front. Psychol. 2015, 6, 241. [Google Scholar] [CrossRef] [PubMed]
- Bochet, A.; Franchini, M.; Kojovic, N.; Glaser, B.; Schaer, M. Emotional vs. Neutral Face Exploration and Habituation: An Eye-Tracking Study of Preschoolers with Autism Spectrum Disorders. Front. Psychiatry 2021, 11, 568997. [Google Scholar] [CrossRef]
- Tsuboi, H. Behavioral and Emotional Characteristics of Abused Children: Child Behavior Checklist/4-18 (CBCL). Jpn. J. Educ. Psychol. 2005, 53, 110–121. [Google Scholar] [CrossRef]
- Devine, S.L.; Walker, S.C.; Makdani, A.; Stockton, E.R.; Mcfarquhar, M.J.; Mcglone, F.P.; Trotter, P.D. Childhood Adversity and Affective Touch Perception: A Comparison of United Kingdom Care Leavers and Non-care Leavers. Front. Psychol. 2020, 11, 557171. [Google Scholar] [CrossRef]
- Tomchek, S.D.; Dunn, W. Sensory processing in children with and without autism: A comparative study using the short sensory profile. Am. J. Occup. Ther. 2007, 61, 190–200. [Google Scholar] [CrossRef]
- Kearney, B.E.; Lanius, R.A. The Brain-body Disconnect: A Somatic Sensory Basis for Trauma-related Disorders. Front. Neurosci. 2022, 16, 1015749. [Google Scholar] [CrossRef]
- Palser, E.; Fotopoulou, A.; Pellicano, E.; Kilner, J. The link between interoceptive processing and anxiety in children diagnosed with autism spectrum disorder: Extending adult findings into a developmental sample. Biol. Psychol. 2018, 136, 13–21. [Google Scholar] [CrossRef]
- Lurie, L.A.; Hangen, E.J.; Rosen, M.L.; Crosnoe, R.; McLaughlin, K.A. Reduced growth mindset as a mechanism linking childhood trauma with academic performance and internalizing psychopathology. Child Abus. Negl. 2023, 142, 105672. [Google Scholar] [CrossRef]
- Wood, H.; Rusbridge, S.; Lei, J.; Lomax, C.; Elliston, J.; Russell, A. Exploring the Cognitive Model of Social Anxiety in Autistic Young People—The Central Role of Bodily Symptoms. J. Autism Dev. Disord. 2022, 52, 5500–5514. [Google Scholar] [CrossRef]
- Conrad, A.; Roth, W.T. Muscle relaxation therapy for anxiety disorders: It works but how? J. Anxiety Disord. 2007, 21, 243–264. [Google Scholar] [CrossRef] [PubMed]
| Total (n = 24) | DM (n = 9) | DD (n = 8) | TD (n = 7) | |
|---|---|---|---|---|
| Characteristics | Mean ± SD | Mean ± SD | Mean ± SD | Mean ± SD |
| Age | 13.08 ± 1.84 | 13.22 ± 2.59 | 12.50 ± 1.60 | 13.57 ± 0.54 |
| KW = 2.144 | ||||
| p = 0.342 | ||||
| Gender | ||||
| Male | 14 (58.3%) | 3 (33.3%) | 6 (75.0%) | 5 (71.4%) |
| Female | 10 (41.7%) | 6 (66.7%) | 2 (25.0%) | 2 (28.6%) |
| * p > 0.05 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Ide-Okochi, A.; He, M.; Tokieda, T.; Nakamura, S.; Matsunaga, N. Assessment of Sensory Processing Issues in Children with Neurodevelopmental Disorders and Experiences of Maltreatment. Children 2024, 11, 216. https://doi.org/10.3390/children11020216
Ide-Okochi A, He M, Tokieda T, Nakamura S, Matsunaga N. Assessment of Sensory Processing Issues in Children with Neurodevelopmental Disorders and Experiences of Maltreatment. Children. 2024; 11(2):216. https://doi.org/10.3390/children11020216
Chicago/Turabian StyleIde-Okochi, Ayako, Mu He, Tomofumi Tokieda, Satsuki Nakamura, and Nobutomo Matsunaga. 2024. "Assessment of Sensory Processing Issues in Children with Neurodevelopmental Disorders and Experiences of Maltreatment" Children 11, no. 2: 216. https://doi.org/10.3390/children11020216
APA StyleIde-Okochi, A., He, M., Tokieda, T., Nakamura, S., & Matsunaga, N. (2024). Assessment of Sensory Processing Issues in Children with Neurodevelopmental Disorders and Experiences of Maltreatment. Children, 11(2), 216. https://doi.org/10.3390/children11020216