Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial
Abstract
1. Introduction
2. Methods
2.1. Protocols and Registration
2.2. Definitions and Diagnosis
2.3. Inclusion and Exclusion Criteria
2.4. Searching Strategy
2.5. Data Extraction
2.6. Risk of Bias Assessment
2.7. Statistical Analysis
3. Results
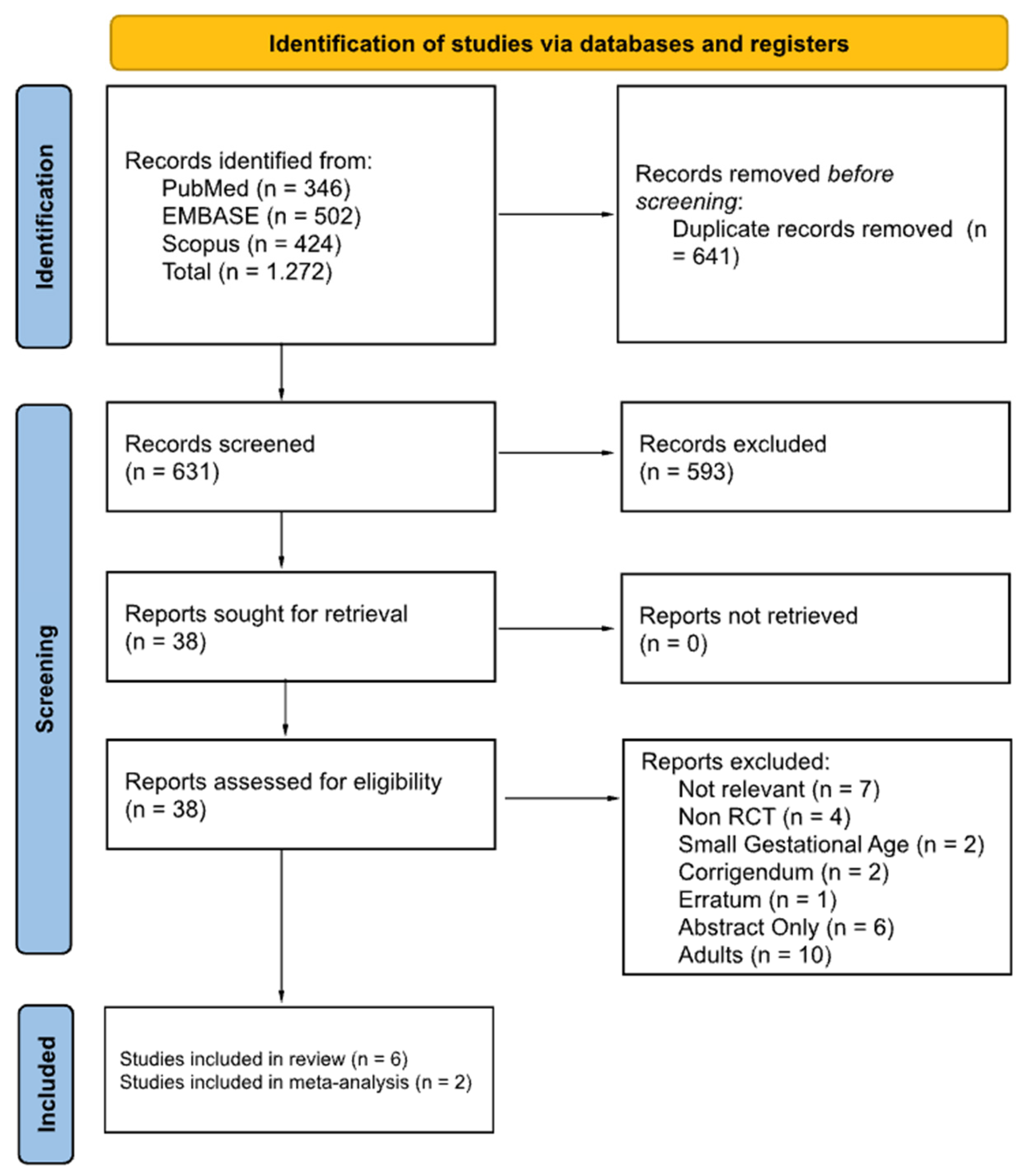
3.1. Searching Result and Study Characteristics
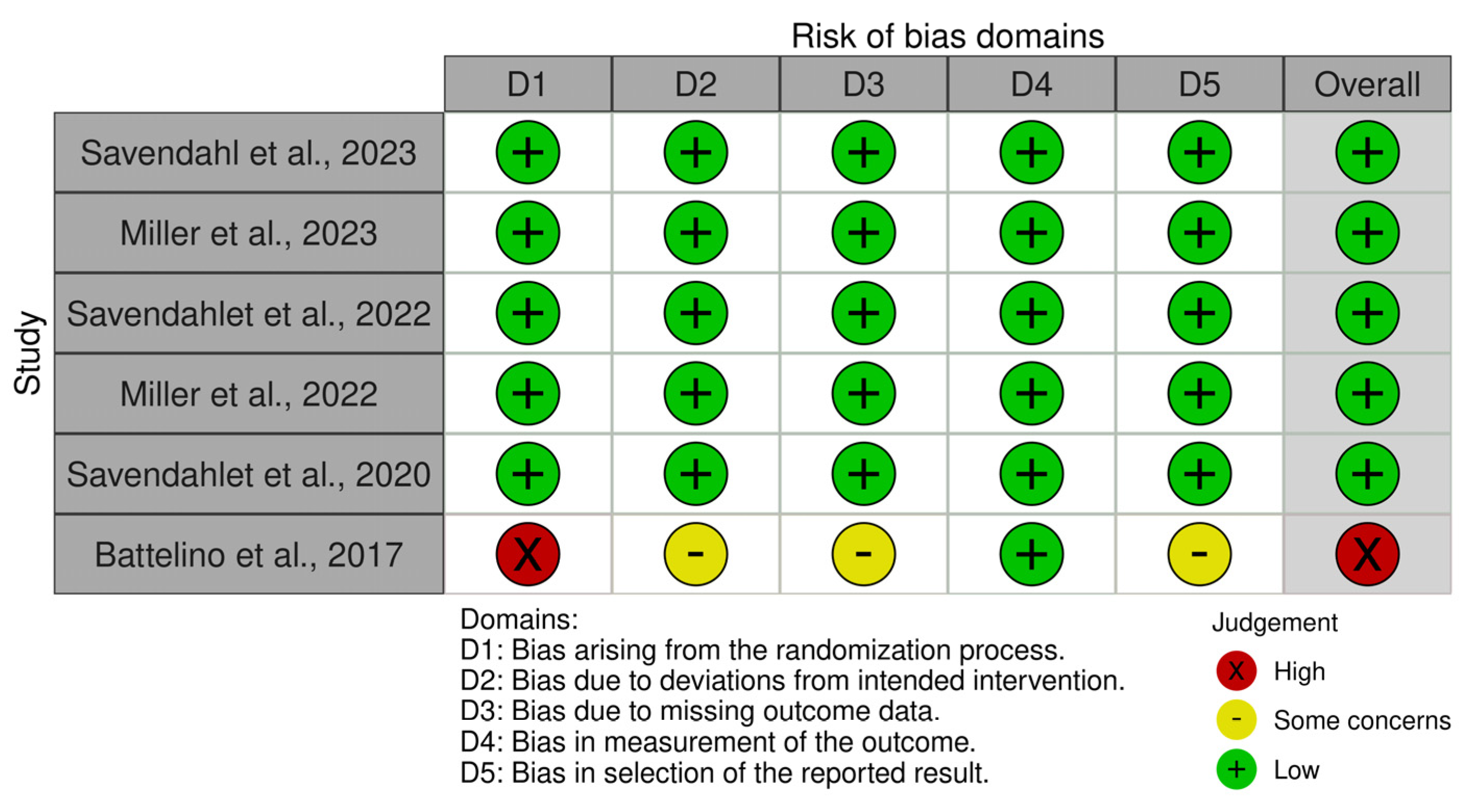
3.2. Quality Assessment
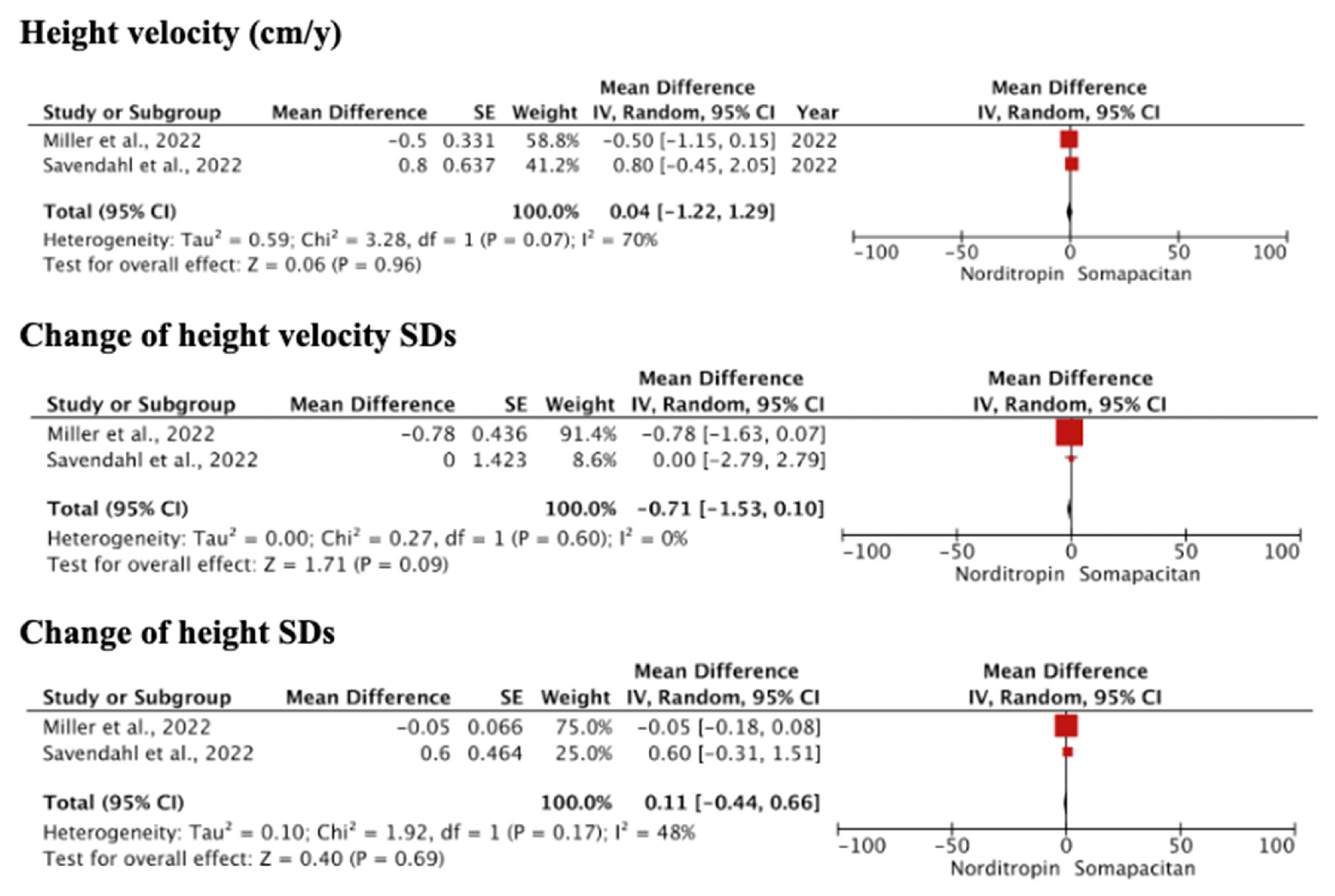
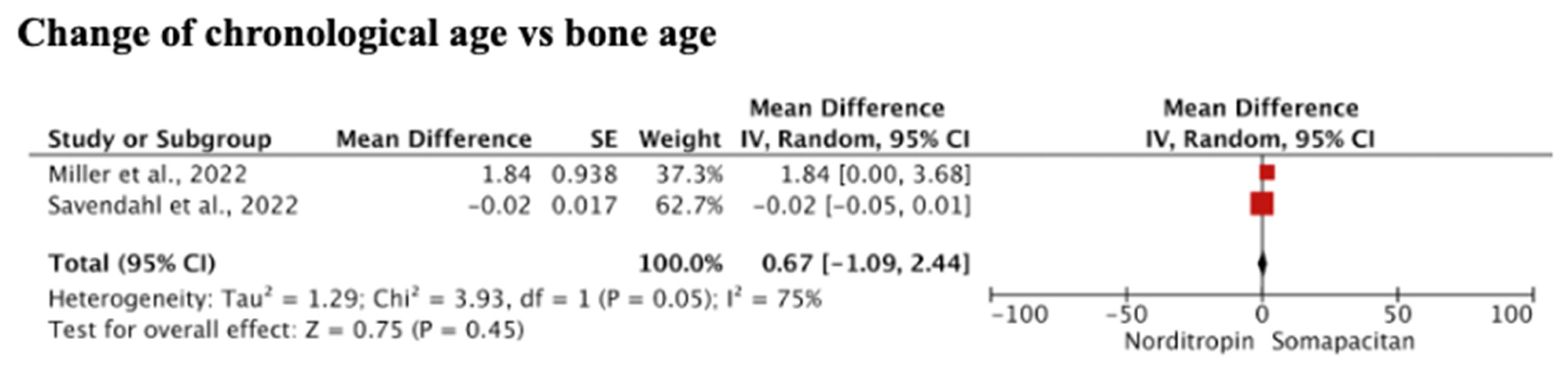
3.3. Efficacy of Somapacitan Compared to Daily Growth Hormone/Norditropin
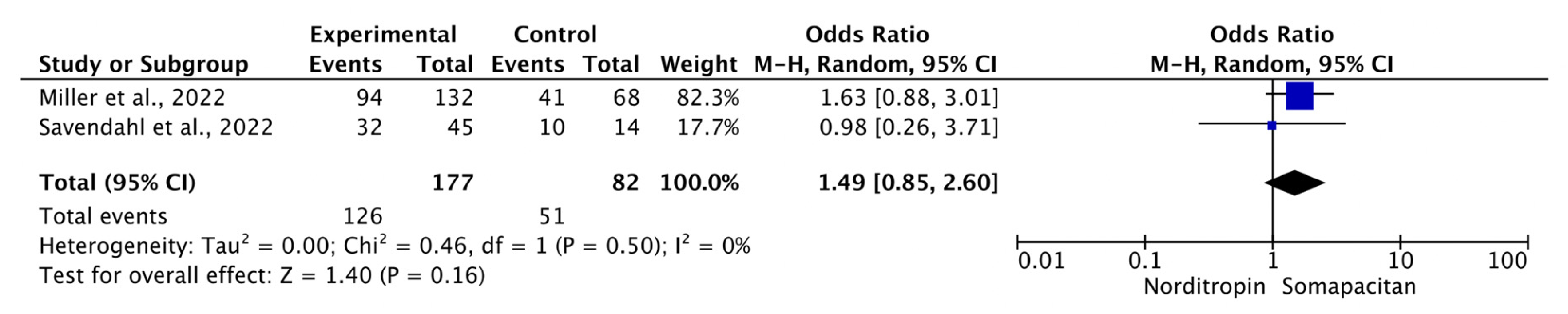
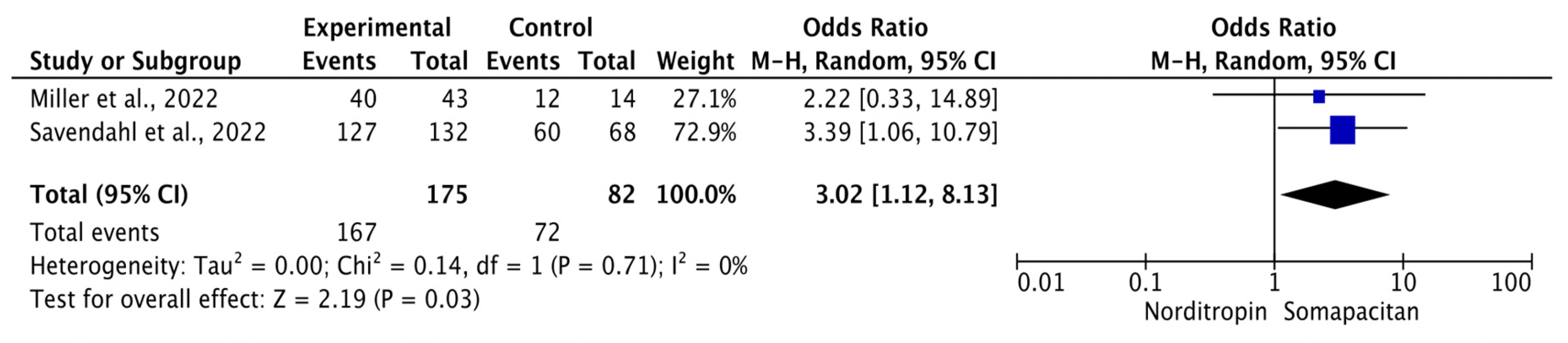
3.4. Adverse Event of Somapacitan Compared to Daily Growth Hormone/Norditropin
3.5. Treatment Adherence of Somapacitan Compared to Daily Growth Hormone/Norditropin
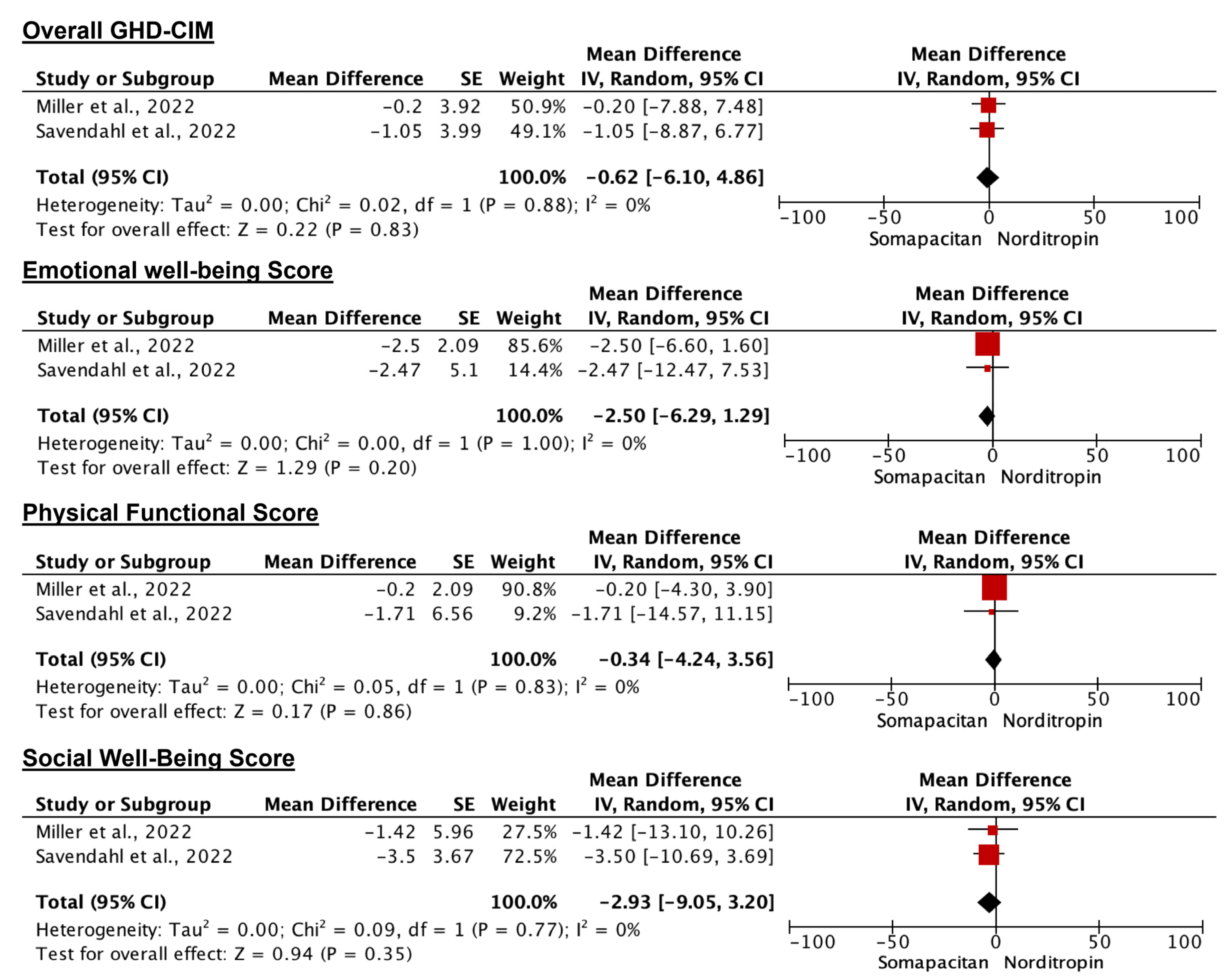
3.6. Disease Burden
4. Discussion
4.1. Efficacy, Safety, and Adherence
4.2. Limitations
4.3. Recommendation
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Murray, P.G.; Dattani, M.T.; Clayton, P.E. Controversies in the Diagnosis and Management of Growth Hormone Deficiency in Childhood and Adolescence. Arch. Dis. Child. 2016, 101, 96–100. [Google Scholar] [CrossRef] [PubMed]
- Tornese, G. ‘Growth Hormone Deficiency’ or Rather ‘Short Stature Unresponsive to Stimulation Tests’? Arch. Dis. Child. 2023, 108, 176–177. [Google Scholar] [CrossRef] [PubMed]
- Brod, M.; Alolga, S.L.; Beck, J.F.; Wilkinson, L.; Højbjerre, L.; Rasmussen, M.H. Understanding Burden of Illness for Child Growth Hormone Deficiency. Qual. Life Res. 2017, 26, 1673–1686. [Google Scholar] [CrossRef] [PubMed]
- Brod, M.; Højbjerre, L.; Alolga, S.L.; Beck, J.F.; Wilkinson, L.; Rasmussen, M.H. Understanding Treatment Burden for Children Treated for Growth Hormone Deficiency. Patient 2017, 10, 653–666. [Google Scholar] [CrossRef] [PubMed]
- Wilson, T.A.; Rose, S.R.; Cohen, P.; Rogol, A.D.; Backeljauw, P.; Brown, R.; Hardin, D.S.; Kemp, S.F.; Lawson, M.; Radovick, S.; et al. Update of Guidelines for the Use of Growth Hormone in Children: The Lawson Wilkins Pediatric Endocrinology Society Drug and Therapeutics Committee. J. Pediatr. 2003, 143, 415–421. [Google Scholar] [CrossRef] [PubMed]
- Allen, D.B.; Backeljauw, P.; Bidlingmaier, M.; Biller, B.M.K.; Boguszewski, M.; Burman, P.; Butler, G.; Chihara, K.; Christiansen, J.; Cianfarani, S.; et al. GH Safety Workshop Position Paper: A Critical Appraisal of Recombinant Human GH Therapy in Children and Adults. Eur. J. Endocrinol. 2016, 174, P1–P9. [Google Scholar] [CrossRef] [PubMed]
- Rosenfeld, R.G.; Bakker, B. Compliance and Persistence in Pediatric and Adult Patients Receiving Growth Hormone Therapy. Endocr. Pract. 2008, 14, 143–154. [Google Scholar] [CrossRef]
- Kapoor, R.R.; Burke, S.A.; Sparrow, S.E.; Hughes, I.A.; Dunger, D.B.; Ong, K.K.; Acerini, C.L. Monitoring of Concordance in Growth Hormone Therapy. Arch. Dis. Child. 2008, 93, 147–148. [Google Scholar] [CrossRef]
- Miller, B.; Crawford, M.; McNamara, A. Reduced Medication Possession Ratio Is Associated with Lower Response to Growth Hormone Therapy. In Proceedings of the Pediatric Academic Societies’ Meeting, Vancouver, BC, Canada, 3–6 May 2014. [Google Scholar]
- McLenon, J.; Rogers, M.A.M. The Fear of Needles: A Systematic Review and Meta-analysis. J. Adv. Nurs. 2019, 75, 30–42. [Google Scholar] [CrossRef]
- Battelino, T.; Rasmussen, M.H.; De Schepper, J.; Zuckerman-Levin, N.; Gucev, Z.; Sävendahl, L. Somapacitan, a Once-weekly Reversible Albumin-binding GH Derivative, in Children with GH Deficiency: A Randomized Dose-escalation Trial. Clin. Endocrinol. 2017, 87, 350–358. [Google Scholar] [CrossRef]
- Novo Nordisk. FDA Approves Once-Weekly Sogroya® for the Treatment of Children Living with Growth Hormone Deficiency; Novo Nordisk: Seattle, WA, USA, 2023. [Google Scholar]
- Mameli, C.; Orso, M.; Calcaterra, V.; Wasniewska, M.G.; Aversa, T.; Granato, S.; Bruschini, P.; Guadagni, L.; d’Angela, D.; Spandonaro, F.; et al. Efficacy, Safety, Quality of Life, Adherence and Cost-Effectiveness of Long-Acting Growth Hormone Replacement Therapy Compared to Daily Growth Hormone in Children with Growth Hormone Deficiency: A Systematic Review and Meta-Analysis. Pharmacol. Res. 2023, 193, 106805. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Kim, J.H.; Chae, H.W.; Chin, S.O.; Ku, C.R.; Park, K.H.; Lim, D.J.; Kim, K.J.; Lim, J.S.; Kim, G.; Choi, Y.M.; et al. Diagnosis and Treatment of Growth Hormone Deficiency: A Position Statement from Korean Endocrine Society and Korean Society of Pediatric Endocrinology. Endocrinol. Metab. 2020, 35, 272–287. [Google Scholar] [CrossRef] [PubMed]
- Grimberg, A.; DiVall, S.A.; Polychronakos, C.; Allen, D.B.; Cohen, L.E.; Quintos, J.B.; Rossi, W.C.; Feudtner, C.; Murad, M.H. Guidelines for Growth Hormone and Insulin-Like Growth Factor-I Treatment in Children and Adolescents: Growth Hormone Deficiency, Idiopathic Short Stature, and Primary Insulin-Like Growth Factor-I Deficiency. Horm. Res. Paediatr. 2017, 86, 361–397. [Google Scholar] [CrossRef] [PubMed]
- Plachy, L.; Amaratunga, S.A.; Dusatkova, P.; Maratova, K.; Neuman, V.; Petruzelkova, L.; Zemkova, D.; Obermannova, B.; Snajderova, M.; Kolouskova, S.; et al. Isolated Growth Hormone Deficiency in Children with Vertically Transmitted Short Stature: What Do the Genes Tell Us? Front. Endocrinol. 2023, 13, 1102968. [Google Scholar] [CrossRef] [PubMed]
- Tsurayya, G.; Duta, T.F.; Naufal, M.A.; Alina, M.; Isitua, C.C.; Ohanu, E.C. Acceptance, Safety, and Impact on Quality of Life of Exergame for Elderly Patients with Neurodegenerative Diseases: A Systematic Review and Meta-Analysis. Narra X 2024, 1, e94. [Google Scholar] [CrossRef]
- Tsurayya, G.; Nazhifah, C.A.; Pirwanja, M.R.; Lemu, Y.K. Soya-Maize-Sorghum Ready-to-Use Therapeutic Food (SMS-RUTF) for the Management of Severe Acute Malnutrition among Children: A Systematic Review and Meta-Analysis. Narra X 2024, 1, e111. [Google Scholar] [CrossRef]
- Iqhrammullah, M.; Duta, T.F.; Alina, M.; Qanita, I.; Naufal, M.A.; Henira, N.; Tsurayya, G.; Fathima, R.; Rizki, A.Y.K.; Amirah, S. Role of Lowered Level of Serum Vitamin D on Diabetic Foot Ulcer and Its Possible Pathomechanism: A Systematic Review, Meta-Analysis, and Meta-Regression. Diabetes Epidemiol. Manag. 2024, 13, 100175. [Google Scholar] [CrossRef]
- CDC Extended BMI-for-Age Growth Charts for Children and Adolescents with Very High BMIs Media Statement. 2022. Available online: https://www.cdc.gov/nccdphp/dnpao/growthcharts/extended-growth-charts.html (accessed on 26 January 2024).
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.-Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A Revised Tool for Assessing Risk of Bias in Randomised Trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T. Measuring Inconsistency in Meta-Analyses. BMJ 2003, 327, 557–560. [Google Scholar] [CrossRef]
- Sandeep, M.; Padhi, B.K.; Yella, S.S.T.; Sruthi, K.G.; Venkatesan, R.G.; Krishna Sasanka, K.B.S.; Satapathy, P.; Mohanty, A.; Al-Tawfiq, J.A.; Iqhrammullah, M.; et al. Myocarditis Manifestations in Dengue Cases: A Systematic Review and Meta-Analysis. J. Infect. Public Health 2023, 16, 1761–1768. [Google Scholar] [CrossRef]
- Saminan, S.; Gusti, N.; Amirah, S.; Iqhrammullah, M. Role of Polymorphism in Vitamin D Receptor Gene on Diabetic Foot Ulcer: A Systematic Review and Meta-Analysis. J. Pharm. Pharmacogn. Res. 2024, 12, 348–362. [Google Scholar] [CrossRef]
- Miller, B.S.; Blair, J.C.; Rasmussen, M.H.; Maniatis, A.; Mori, J.; Böttcher, V.; Kim, H.-S.; Bang, R.B.; Polak, M.; Horikawa, R. Effective GH Replacement with Somapacitan in Children with GHD: REAL4 2-Year Results and after Switch from Daily GH. J. Clin. Endocrinol. Metab. 2023, 108, 3090–3099. [Google Scholar] [CrossRef] [PubMed]
- Sävendahl, L.; Battelino, T.; Højby Rasmussen, M.; Brod, M.; Röhrich, S.; Saenger, P.; Horikawa, R. Weekly Somapacitan in GH Deficiency: 4-Year Efficacy, Safety, and Treatment/Disease Burden Results from REAL 3. J. Clin. Endocrinol. Metab. 2023, 108, 2569–2578. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.S.; Blair, J.C.; Rasmussen, M.H.; Maniatis, A.; Kildemoes, R.J.; Mori, J.; Polak, M.; Bang, R.B.; Böttcher, V.; Stagi, S.; et al. Weekly Somapacitan Is Effective and Well Tolerated in Children with GH Deficiency: The Randomized Phase 3 REAL4 Trial. J. Clin. Endocrinol. Metab. 2022, 107, 3378–3388. [Google Scholar] [CrossRef] [PubMed]
- Sävendahl, L.; Battelino, T.; Højby Rasmussen, M.; Brod, M.; Saenger, P.; Horikawa, R. Effective GH Replacement with Once-Weekly Somapacitan vs Daily GH in Children with GHD: 3-Year Results from REAL 3. J. Clin. Endocrinol. Metab. 2022, 107, 1357–1367. [Google Scholar] [CrossRef] [PubMed]
- Sävendahl, L.; Battelino, T.; Brod, M.; Højby Rasmussen, M.; Horikawa, R.; Juul, R.V.; Saenger, P.; Furthner, D.; Piringer, B.; Auer-Hackenberg, L.; et al. Once-Weekly Somapacitan vs. Daily GH in Children with GH Deficiency: Results from a Randomized Phase 2 Trial. J. Clin. Endocrinol. Metab. 2020, 105, e1847–e1861. [Google Scholar] [CrossRef] [PubMed]
- Juul, R.V.; Rasmussen, M.H.; Agersø, H.; Overgaard, R.V. Pharmacokinetics and Pharmacodynamics of Once-Weekly Somapacitan in Children and Adults: Supporting Dosing Rationales with a Model-Based Analysis of Three Phase I Trials. Clin. Pharmacokinet. 2019, 58, 63–75. [Google Scholar] [CrossRef] [PubMed]
- Miller, B.S.; Velazquez, E.; Yuen, K.C.J. Long-Acting Growth Hormone Preparations-Current Status and Future Considerations. J. Clin. Endocrinol. Metab. 2020, 105, e2121–e2133. [Google Scholar] [CrossRef] [PubMed]
- Helleberg, H.; Bjelke, M.; Damholt, B.B.; Pedersen, P.J.; Rasmussen, M.H. Absorption, Metabolism and Excretion of Once-Weekly Somapacitan, a Long-Acting Growth Hormone Derivative, after Single Subcutaneous Dosing in Human Subjects. Eur. J. Pharm. Sci. 2021, 167, 106030. [Google Scholar] [CrossRef]
- Boguszewski, C.L. Safety of Long-Term Use of Daily and Long-Acting Growth Hormone in Growth Hormone-Deficient Adults on Cancer Risk. Best. Pract. Res. Clin. Endocrinol. Metab. 2023, 37, 101817. [Google Scholar] [CrossRef] [PubMed]
- Brod, M.; Højby Rasmussen, M.; Vad, K.; Alolga, S.; Bushnell, D.M.; Bedoin, J.; Maniatis, A. Psychometric Validation of the Growth Hormone Deficiency-Child Impact Measure (GHD-CIM). Pharmacoecon. Open 2021, 5, 505–518. [Google Scholar] [CrossRef] [PubMed]
- Haj-Ahmad, L.M.; Mahmoud, M.M.; Sweis, N.W.G.; Bsisu, I.; Alghrabli, A.M.; Ibrahim, A.M.; Zayed, A.A. Serum IGF-1 to IGFBP-3 Molar Ratio: A Promising Diagnostic Tool for Growth Hormone Deficiency in Children. J. Clin. Endocrinol. Metab. 2023, 108, 986–994. [Google Scholar] [CrossRef] [PubMed]
| Study, Year (Ref) | Sites/Country (n) | Observation Time * | Sample Size (I/C) | Trial Phase (Number) |
|---|---|---|---|---|
| Miller et al., 2023 [26] | 86/20 | 104 weeks | 200 (132/68) | III (NCT03811535) |
| Savendahl et al., 2023 [27] | 29/11 | 208 weeks | 57 (43/14) | III (NCT02616562) |
| Miller et al., 2022 [28] | 86/20 | 52 weeks | 200 (132/68) | II (NCT03811535) |
| Savendahl et al., 2022 [29] | 29/11 | 156 weeks | 57 (43/14) | II (NCT02616562) |
| Savendahl et al., 2020 [30] | 29/11 | 52 weeks | 57 (43/14) | II (NCT02616562) |
| Battelino et al., 2017 [11] | 14/8 | 7 days | 32 (24/8) | I (NCT01973244) |
| Study (Year) [Ref] | Subjects’ Characteristics | Somapacitan® Dose (mg/kg/week) | Control | Outcomes | Injection Site Reaction (I/C) | |||
|---|---|---|---|---|---|---|---|---|
| Etiology of GHD, I/O | Sex, M/F | Age, Mean ± SD (Years) | BMI (kg/m2) [Percentile, Status] | |||||
| Miller et al., 2023 [26] | 176/24 | 149/51 | 6.4 ± 2.3 | 15.7 ± 1.5 (<1st, underweight) | 0.16 | Norditropin® (0.034 mg/kg/d) | HV (cm/y), HV SDs, height SDs, IGF-1 SDs, BA vs. CA. | NR |
| Savendahl et al., 2023 [27] | 53/4 | 34/23 | 5.95 ± 1.98 | 15.14 ± 1.20 (<1st, underweight) | 0.16 | Norditropin® (0.034 mg/kg/d) | HV (cm/y), HV SDs, height SDs, IGF-I SDS, IGFBP-3 SDs, GHD-CTB, GHD-PTB. | NR |
| Miller et al., 2022 [28] | 176/24 | 149/51 | 6.4 ± 2.3 | 15.7 ± 1.52 (<1st, underweight) | 0.16 | Norditropin® (0.034 mg/kg/d) | HV (cm/y), HV SDs, height SDs, IGF-1 SDs, BA vs. CA, GHD-CIM, GHD-CTB | 7/4 |
| Savendahl et al., 2022 [29] | 53/4 | 34/23 | 5.95 ± 1.98 | 15.14 ± 1.20 (<1st, underweight) | 0.16 | Norditropin® (0.034 mg/kg/d) | HV (cm/y), HV SDs, height SDs, IGF-I SDs, IGFBP-3 SDs, bone age, GHD-CIM | NR |
| Savendahl et al., 2020 [30] | 53/4 | 34/23 | 5.95 ± 1.98 | 15.14 ± 1.20 (<1st, underweight) | 0.04, 0.08, or 0.16 | Norditropin® (0.034 mg/kg/d) | HV (cm/y), HV SDs, height SDs, IGF-I SDs, IGFBP-3 SDs, bone age, GHD-CIM, HbA1c | 3/1 |
| Battelino et al., 2017 [11] | 23/9 | 23/9 | 8.85 ± 1.30 | 16.16 ± 2.48 (<1st, underweight) | 0.02, 0.04, 0.08, or 0.16 | Norditropin® (0.034 mg/kg/d) | Cmax, tmax, IGF-I level, IGFBP-3 level, IGF-1 SDs, IGFBP-3 SDs | 4/0 |
| Subgroups | Events with Somapacitan | Events with Norditropin | OR (95% CI) | p-Value | I2 (%) |
|---|---|---|---|---|---|
| Severity | |||||
| Mild symptoms | 117/175 | 35/82 | 1.66 (0.97, 2.85) | 0.06 | 0% |
| Moderate symptoms | 38/175 | 14/82 | 1.30 (0.66, 2.59) | 0.45 | 0% |
| Severe events | 4/175 | 2/82 | 0.58 (0.03, 11.14) | 0.72 | 57% |
| Relation to trial products | |||||
| Probably related | 16/175 | 5/82 | 1.52 (0.54, 4.32) | 0.43 | 0% |
| Possibly related | 24/175 | 11/82 | 1.03 (0.48, 2.23) | 0.93 | 0% |
| Unlikely related | 122/175 | 48/82 | 1.54 (0.89, 2.67) | 0.12 | 0% |
| Serious event | |||||
| Serious event | 10/175 | 4/82 | 1.01 (0.30, 3.40) | 0.98 | 0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Tsurayya, G.; Nazhifah, C.A.; Pirwanja, M.R.; Zulfa, P.O.; Tatroman, M.R.R.; Fakri, F.; Iqhrammullah, M. Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial. Children 2024, 11, 227. https://doi.org/10.3390/children11020227
Tsurayya G, Nazhifah CA, Pirwanja MR, Zulfa PO, Tatroman MRR, Fakri F, Iqhrammullah M. Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial. Children. 2024; 11(2):227. https://doi.org/10.3390/children11020227
Chicago/Turabian StyleTsurayya, Ghina, Cut Alifiya Nazhifah, Muhammad Rahmat Pirwanja, Putri Oktaviani Zulfa, Muhammad Raihan Ramadhan Tatroman, Fajar Fakri, and Muhammad Iqhrammullah. 2024. "Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial" Children 11, no. 2: 227. https://doi.org/10.3390/children11020227
APA StyleTsurayya, G., Nazhifah, C. A., Pirwanja, M. R., Zulfa, P. O., Tatroman, M. R. R., Fakri, F., & Iqhrammullah, M. (2024). Once-Weekly Somapacitan as an Alternative Management of Growth Hormone Deficiency in Prepubertal Children: A Systematic Review and Meta-Analysis of Randomized Controlled Trial. Children, 11(2), 227. https://doi.org/10.3390/children11020227







