Image-Guided Percutaneous Drainage of Abdominal Abscesses in Pediatric Patients
Abstract
1. Introduction
2. Background
3. Imaging and Diagnosis
4. Treatment
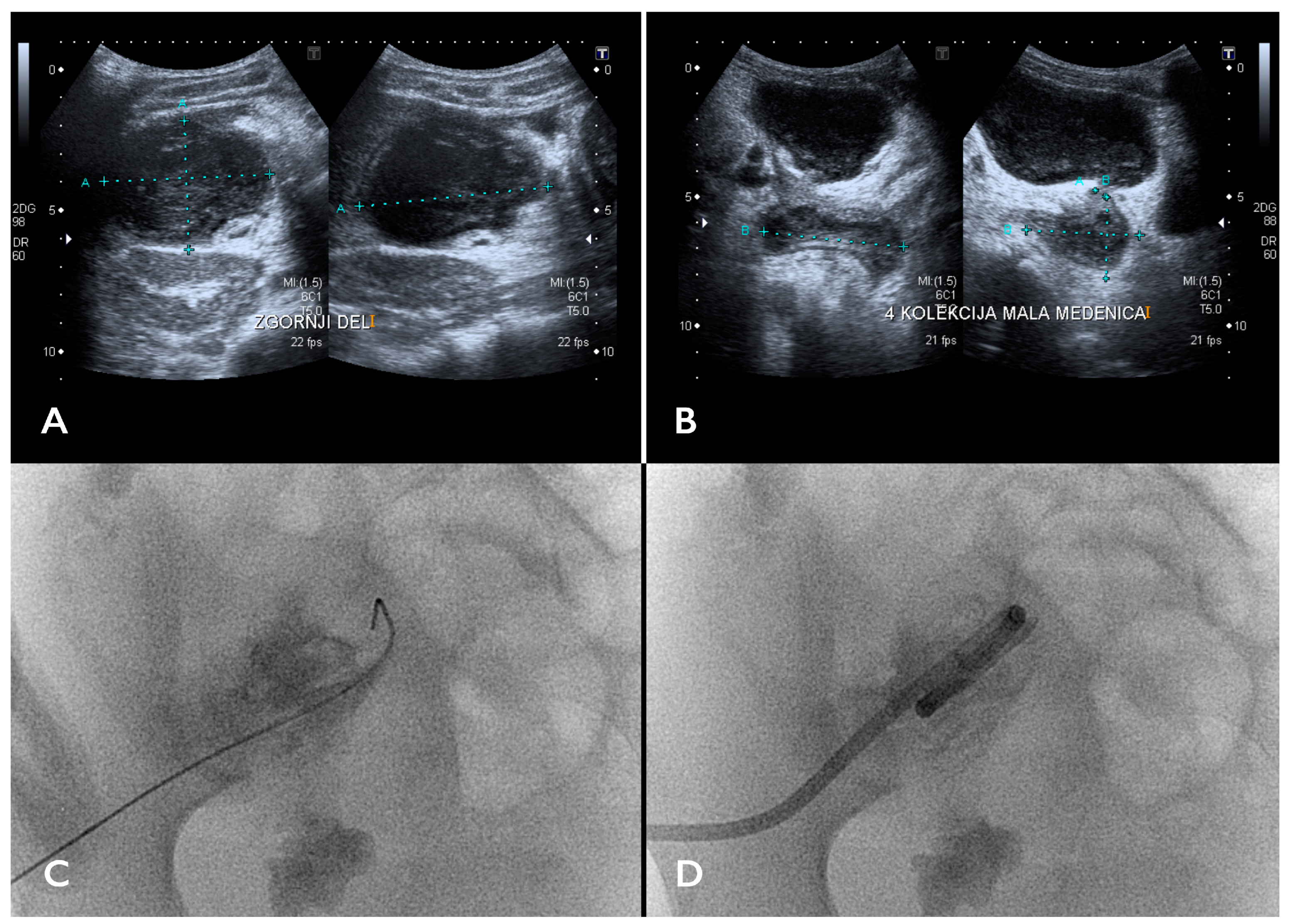
5. Image-Guided Percutaneous Abscess Drainage
5.1. IPAD Basics
5.2. Access Pathway
5.3. Catheter Selection and Insertion
5.4. Sedation and General Anesthesia
5.5. Catheter Management
5.6. Efficacy and Complications
5.7. Follow-Up Imaging
6. Review of the Literature
- -
- clinical trial, randomized controlled trial, case series, or systematic review;
- -
- a clear focus on intra-abdominal abscesses;
- -
- a clear focus on percutaneous drainage in the pediatric population; one paper on abscess needle aspiration without drainage was also deemed appropriate for inclusion;
- -
- studies focusing on surgical drainage or medical therapy were excluded;
- -
- due to the fact that percutaneous drainage techniques have been well established for decades with little technical innovation and also considering the relative scarcity of published research, no time limit was applied during the literature search.
7. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Wallace, M.J.; Chin, K.W.; Fletcher, T.B.; Bakal, C.W.; Cardella, J.F.; Grassi, C.J.; Grizzard, J.D.; Kaye, A.D.; Kushner, D.C.; Larson, P.A.; et al. Quality Improvement Guidelines for Percutaneous Drainage/Aspiration of Abscess and Fluid Collections. J. Vasc. Interv. Radiol. 2010, 21, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Gervais, D.A.; Brown, S.D.; Connolly, S.A.; Brec, S.L.; Harisinghani, M.G.; Mueller, P.R. Percutaneous Imaging-Guided Abdominal and Pelvic Abscess Drainage in Children. RadioGraphics 2004, 24, 737–754. [Google Scholar] [CrossRef]
- McGahan, J.P. The History of Interventional Ultrasound. J. Ultrasound Med. 2004, 23, 727–741. [Google Scholar] [CrossRef] [PubMed]
- van Sonnenberg, E.; Wittich, G.R.; Edwards, D.K.; Casola, G.; von Waldenburg Hilton, S.; Self, T.W.; Keightley, A.; Withers, C. Percutaneous Diagnostic and Therapeutic Interventional Radiologic Procedures in Children: Experience in 100 Patients. Radiology 1987, 162, 601–605. [Google Scholar] [CrossRef]
- Newman, K.; Ponsky, T.; Kittle, K.; Dyk, L.; Throop, C.; Gieseker, K.; Sills, M.; Gilbert, J. Appendicitis 2000: Variability in Practice, Outcomes, and Resource Utilization at Thirty Pediatric Hospitals. J. Pediatr. Surg. 2003, 38, 372–379. [Google Scholar] [CrossRef]
- Bieluch, V.M.; Tally, F.P. Pathophysiology of Abscess Formation. Clin. Obs. Obstet. Gynaecol. 1983, 10, 93–103. [Google Scholar] [CrossRef]
- Bowman, J.K. Abscess Incision and Drainage. Prim. Care 2022, 49, 39–45. [Google Scholar] [CrossRef]
- Lopez, N.; Kobayashi, L.; Coimbra, R. A Comprehensive Review of Abdominal Infections. World J. Emerg. Surg. 2011, 6, 7. [Google Scholar] [CrossRef]
- Nielsen, O.L.; Iburg, T.; Aalbaek, B.; Leifsson, P.S.; Agerholm, J.S.; Heegaard, P.; Boye, M.; Simon, S.; Jensen, K.B.; Christensen, S.; et al. A Pig Model of Acute Staphylococcus Aureus Induced Pyemia. Acta Vet. Scand. 2009, 51, 14. [Google Scholar] [CrossRef][Green Version]
- Zhang, R.G.; Wang, X.D.; Zhang, X.L.; Yang, Y.S. An Experimental Model for Staphylococcus Aureus Hepatic Abscess in Bama Minipig. Genet. Mol. Res. 2014, 13, 7113–7122. [Google Scholar] [CrossRef]
- Hogan, M.J. Appendiceal Abscess Drainage. Tech. Vasc. Interv. Radiol. 2003, 6, 205–214. [Google Scholar] [CrossRef] [PubMed]
- Guilcher, G.M.T.; Rivard, L.; Huang, J.T.; Wright, N.A.M.; Anderson, L.; Eissa, H.; Pelletier, W.; Ramachandran, S.; Schechter, T.; Shah, A.J.; et al. Immune Function in Childhood Cancer Survivors: A Children’s Oncology Group Review. Lancet Child Adolesc. Health 2021, 5, 284–294. [Google Scholar] [CrossRef] [PubMed]
- Brodszki, N.; Jönsson, G.; Skattum, L.; Truedsson, L. Primary Immunodeficiency in Infection-Prone Children in Southern Sweden: Occurrence, Clinical Characteristics and Immunological Findings. BMC Immunol. 2014, 15, 31. [Google Scholar] [CrossRef] [PubMed]
- Brook, I.; Hunter, V.; Walker, R.I. Synergistic Effect of Bacteroides, Clostridium, Fusobacterium, Anaerobic Cocci, and Aerobic Bacteria on Mortality and Induction of Subcutaneous Abscesses in Mice. J. Infect. Dis. 1984, 149, 924–928. [Google Scholar] [CrossRef] [PubMed]
- Witzigmann, H.; Geissler, F.; Uhlmann, D.; Hauss, J. Intra-Abdominal Abscess. Chirurg 1998, 69, 813–820. [Google Scholar] [CrossRef] [PubMed]
- Menichetti, F.; Sganga, G. Definition and Classification of Intra-Abdominal Infections. J. Chemother. 2009, 21 (Suppl. S1), 3–4. [Google Scholar] [CrossRef] [PubMed]
- Jeffrey, R.B.; Federle, M.P.; Tolentino, C.S. Periappendiceal Inflammatory Masses: CT-Directed Management and Clinical Outcome in 70 Patients. Radiology 1988, 167, 13–16. [Google Scholar] [CrossRef]
- Martin, G.S.; Mannino, D.M.; Moss, M. The Effect of Age on the Development and Outcome of Adult Sepsis. Crit. Care Med. 2006, 34, 15–21. [Google Scholar] [CrossRef]
- D’Souza, N.; Nugent, K. Appendicitis. Am. Fam. Physician 2016, 93, 142–143. [Google Scholar]
- Kim, S.K.; Ko, S.H.; Jeong, K.Y.; Lee, J.S.; Choi, H.S.; Hong, H.P. Acute Phlegmonous Gastritis Complicated by Subphrenic Abscess. J. Emerg. Med. 2021, 60, e49–e52. [Google Scholar] [CrossRef]
- Capolupo, G.T.; Mascianà, G.; Carannante, F.; Caricato, M. Hepatic Portal Venous Gas after Colonoscopy: A Case Report and Review. Int. J. Surg. Case Rep. 2018, 51, 54–57. [Google Scholar] [CrossRef] [PubMed]
- Hogan, M.J.; Marshalleck, F.E.; Sidhu, M.K.; Connolly, B.L.; Towbin, R.B.; Saad, W.A.; Cahill, A.M.; Crowley, J.; Heran, M.K.S.; Hohenwalter, E.J.; et al. Society of Interventional Radiology Standards of Practice Committee and Society for Pediatric Radiology Interventional Radiology Committee. Quality Improvement Guidelines for Pediatric Abscess and Fluid Drainage. J. Vasc. Interv. Radiol. 2012, 23, 1397–1402. [Google Scholar] [CrossRef] [PubMed]
- Connolly, B.; Racadio, J.; Towbin, R. Practice of ALARA in the Pediatric Interventional Suite. Pediatr. Radiol. 2006, 36 (Suppl. S2), 163–167. [Google Scholar] [CrossRef] [PubMed]
- Duszak, R.L.; Levy, J.M.; Akins, E.W.; Bakal, C.W.; Denny, D.D.; Martin, L.G.; Van Moore, A.; Pentecost, M.J.; Roberts, A.C.; Vogelzang, R.L.; et al. Percutaneous Catheter Drainage of Infected Intra-Abdominal Fluid Collections. American College of Radiology. ACR Appropriateness Criteria. Radiology 2000, 215, 1067–1075. [Google Scholar] [PubMed]
- Klibanov, A.L.; Hossack, J.A. Ultrasound in Radiology: From Anatomic, Functional, Molecular Imaging to Drug Delivery and Image-Guided Therapy. Investig. Radiol. 2015, 50, 657–670. [Google Scholar] [CrossRef] [PubMed]
- Maher, M.M.; Kealey, S.; McNamara, A.; O’Laoide, R.; Gibney, R.G.; Malone, D.E. Management of Visceral Interventional Radiology Catheters: A Troubleshooting Guide for Interventional Radiologists. Radiographics 2002, 22, 305–322. [Google Scholar] [CrossRef]
- Arani, K.; Nandalur, K.; Tucker, C.M.; Bloom, D.A. Image-Guided Percutaneous Drainage in the Pediatric Population: A Primer for Radiologists. J. Clin. Imaging Sci. 2011, 1, 31. [Google Scholar] [CrossRef]
- Lobo, V.; Hunter-Behrend, M.; Cullnan, E.; Higbee, R.; Phillips, C.; Williams, S.; Perera, P.; Gharahbaghian, L. Caudal Edge of the Liver in the Right Upper Quadrant (RUQ) View Is the Most Sensitive Area for Free Fluid on the FAST Exam. West. J. Emerg. Med. 2017, 18, 270–280. [Google Scholar] [CrossRef]
- Phillip, V.; Braren, R.; Lukas, N.; Schmid, R.M.; Geisler, F. Arterial Pseudoaneurysm within a Pancreatic Pseudocyst. Case Rep. Gastroenterol. 2018, 12, 513–518. [Google Scholar] [CrossRef]
- Halvorsen, R.A.; Foster, W.L.; Wilkinson, R.H.; Silverman, P.M.; Thompson, W.M. Hepatic Abscess: Sensitivity of Imaging Tests and Clinical Findings. Gastrointest. Radiol. 1988, 13, 135–141. [Google Scholar] [CrossRef]
- Moomjian, L.N.; Clayton, R.D.; Carucci, L.R. A Spectrum of Entities That May Mimic Abdominopelvic Abscesses Requiring Image-Guided Drainage. Radiographics 2018, 38, 1264–1281. [Google Scholar] [CrossRef] [PubMed]
- Huang, D.Y.; Yusuf, G.T.; Daneshi, M.; Ramnarine, R.; Deganello, A.; Sellars, M.E.; Sidhu, P.S. Contrast-Enhanced Ultrasound (CEUS) in Abdominal Intervention. Abdom. Radiol. 2018, 43, 960–976. [Google Scholar] [CrossRef] [PubMed]
- Meloni, M.F.; Andreano, A.; Laeseke, P.F.; Lee, F.T.; Sironi, S.; Filice, C.; Ferraioli, G. Contrast-Enhanced Ultrasonographic Findings in a Brucellar Hepatic Abscess. J. Ultrasound Med. 2008, 27, 1511–1515. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kishina, M.; Koda, M.; Tokunaga, S.; Miyoshi, K.; Fujise, Y.; Kato, J.; Matono, T.; Sugihara, T.; Murawaki, Y. Usefulness of Contrast-Enhanced Ultrasound with Sonazoid for Evaluating Liver Abscess in Comparison with Conventional B-Mode Ultrasound. Hepatol. Res. 2015, 45, 337–342. [Google Scholar] [CrossRef] [PubMed]
- Charles, H.W. Abscess Drainage. Semin. Interv. Radiol. 2012, 29, 325–336. [Google Scholar] [CrossRef] [PubMed]
- Abdeen, N.; Naz, F.; Linthorst, R.; Khan, U.; Dominguez, P.C.; Koujok, K.; Bettoli, M.; Shenouda, N. Clinical Impact and Cost-effectiveness of Noncontrast MRI in the Evaluation of Suspected Appendiceal Abscesses in Children. J. Magn. Reson. Imaging 2019, 49, e241–e249. [Google Scholar] [CrossRef] [PubMed]
- Thompson, S.M.; Gorny, K.R.; Koepsel, E.M.K.; Welch, B.T.; Mynderse, L.; Lu, A.; Favazza, C.P.; Felmlee, J.P.; Woodrum, D.A. Body Interventional MRI for Diagnostic and Interventional Radiologists: Current Practice and Future Prospects. Radiographics 2021, 41, 1785–1801. [Google Scholar] [CrossRef]
- Wagner, C.; Sauermann, R.; Joukhadar, C. Principles of Antibiotic Penetration into Abscess Fluid. Pharmacology 2006, 78, 1–10. [Google Scholar] [CrossRef]
- Collins, G.; Allaway, M.G.R.; Eslick, G.D.; Cox, M.R. Non-operative Management of Small Post-appendicectomy Intra-abdominal Abscess Is Safe and Effective. ANZ J Surg 2020, 90, 1979–1983. [Google Scholar] [CrossRef]
- Altemeier, W.A.; Culbertson, W.R.; Fullen, W.D.; Shook, C.D. Intra-Abdominal Abscesses. Am. J. Surg. 1973, 125, 70–79. [Google Scholar] [CrossRef]
- Jaffe, T.A.; Nelson, R.C. Image-Guided Percutaneous Drainage: A Review. Abdom. Radiol. 2016, 41, 629–636. [Google Scholar] [CrossRef] [PubMed]
- Siewert, B.; Tye, G.; Kruskal, J.; Sosna, J.; Opelka, F.; Raptopoulos, V.; Goldberg, S.N. Impact of CT-Guided Drainage in the Treatment of Diverticular Abscesses: Size Matters. AJR Am. J. Roentgenol. 2006, 186, 680–686. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Y.; Stringel, G.; Bezahler, I.; Maddineni, S. Nonoperative Management of Periappendiceal Abscess in Children: A Comparison of Antibiotics Alone versus Antibiotics plus Percutaneous Drainage. J. Pediatr. Surg. 2020, 55, 414–417. [Google Scholar] [CrossRef] [PubMed]
- Leanza, V.; Lo Presti, V.; Di Guardo, F.; Leanza, G.; Palumbo, M. CT-Guided Drainage with Percutaneous Approach as Treatment of E. Faecalis Post Caesarean Section Severe Abscess: Case Report and Literature Review. Il G. Chir.-J. Ital. Surg. Assoc. 2019, 40, 368–372. [Google Scholar]
- Gao, D.; Medina, M.G.; Alameer, E.; Nitz, J.; Tsoraides, S. A Case Report on Delayed Diagnosis of Perforated Crohn’s Disease with Recurrent Intra-Psoas Abscess Requiring Omental Patch. Int. J. Surg. Case Rep. 2019, 65, 325–328. [Google Scholar] [CrossRef]
- Towbin, R. Interventional Procedures in Pediatrics. Semin. Pediatr. Surg. 1992, 1, 296–307. [Google Scholar] [PubMed]
- Maher, M.M.; Gervais, D.A.; Kalra, M.K.; Lucey, B.; Sahani, D.V.; Arellano, R.; Hahn, P.F.; Mueller, P.R. The Inaccessible or Undrainable Abscess: How to Drain It. Radiographics 2004, 24, 717–735. [Google Scholar] [CrossRef] [PubMed]
- Pereira, J.K.; Chait, P.G.; Miller, S.F. Deep Pelvic Abscesses in Children: Transrectal Drainage under Radiologic Guidance. Radiology 1996, 198, 393–396. [Google Scholar] [CrossRef]
- Jamieson, D.H.; Chait, P.G.; Filler, R. Interventional Drainage of Appendiceal Abscesses in Children. AJR Am. J. Roentgenol. 1997, 169, 1619–1622. [Google Scholar] [CrossRef]
- Chung, T.; Hoffer, F.A.; Lund, D.P. Transrectal Drainage of Deep Pelvic Abscesses in Children Using a Combined Transrectal Sonographic and Fluoroscopic Guidance. Pediatr. Radiol. 1996, 26, 874–878. [Google Scholar] [CrossRef]
- McNicholas, M.M.; Mueller, P.R.; Lee, M.J.; Echeverri, J.; Gazelle, G.S.; Boland, G.W.; Dawson, S.L. Percutaneous Drainage of Subphrenic Fluid Collections That Occur after Splenectomy: Efficacy and Safety of Transpleural versus Extrapleural Approach. AJR Am. J. Roentgenol. 1995, 165, 355–359. [Google Scholar] [CrossRef] [PubMed]
- Yakupovich, A.; Rajeswaran, S.; Green, J.; Donaldson, J.S. Role of Interventional Radiology in Children with Biliary and Gallbladder Diseases. Semin. Interv. Radiol. 2021, 38, 356–363. [Google Scholar] [CrossRef] [PubMed]
- Walser, E.; Raza, S.; Hernandez, A.; Ozkan, O.; Kathuria, M.; Akinci, D. Sonographically Guided Transgluteal Drainage of Pelvic Abscesses. AJR Am. J. Roentgenol. 2003, 181, 498–500. [Google Scholar] [CrossRef] [PubMed]
- Dial, S.; Silver, P.; Bock, K.; Sagy, M. Pediatric Sedation for Procedures Titrated to a Desired Degree of Immobility Results in Unpredictable Depth of Sedation. Pediatr. Emerg. Care 2001, 17, 414–420. [Google Scholar] [CrossRef] [PubMed]
- Mueller, P.R.; Simeone, J.F.; Butch, R.J.; Saini, S.; Stafford, S.A.; Vici, L.G.; Soto-Rivera, C.; Ferrucci, J.T. Percutaneous Drainage of Subphrenic Abscess: A Review of 62 Patients. AJR Am. J. Roentgenol. 1986, 147, 1237–1240. [Google Scholar] [CrossRef] [PubMed]
- An, S.-W.; Yoon, C.J.; Seong, N.J.; Kang, S.-G.; Han, H.-S.; Cho, J.Y.; Yoon, Y.-S.; Kim, H.-H.; Kim, Y.-J.; Woo, Y.-N.; et al. Inaccessible Postoperative Abdominal Abscess: Percutaneous Drainage Technique with Puncture of a Sinus Tract. J. Vasc. Interv. Radiol. 2013, 24, 586–591. [Google Scholar] [CrossRef] [PubMed]
- Coté, C.J.; Wilson, S.; American Academy of Pediatrics; American Academy of Pediatric Dentistry. Guidelines for Monitoring and Management of Pediatric Patients Before, During, and After Sedation for Diagnostic and Therapeutic Procedures. Pediatrics 2019, 143, e20191000. [Google Scholar] [CrossRef]
- Gamble, C.; Gamble, J.; Seal, R.; Wright, R.B.; Ali, S. Bispectral Analysis during Procedural Sedation in the Pediatric Emergency Department. Pediatr. Emerg. Care 2012, 28, 1003–1008. [Google Scholar] [CrossRef]
- Cheng, D.; Nagata, K.T.; Yoon, H.-C. Randomized Prospective Comparison of Alteplase versus Saline Solution for the Percutaneous Treatment of Loculated Abdominopelvic Abscesses. J. Vasc. Interv. Radiol. 2008, 19, 906–911. [Google Scholar] [CrossRef]
- Diamond, I.R.; Wales, P.W.; Connolly, B.; Gerstle, T. Tissue Plasminogen Activator for the Treatment of Intraabdominal Abscesses in a Neonate. J. Pediatr. Surg. 2003, 38, 1234–1236. [Google Scholar] [CrossRef]
- Gibson, C.R.; Amirabadi, A.; Goman, S.; Armstrong, N.C.; Langer, J.C.; Amaral, J.G.; Temple, M.J.; Parra, D.; John, P.R.; Connolly, B.L. Use of Tissue Plasminogen Activator in Abdominal Abscesses in Children—A Single-Center Randomized Control Trial. Can. Assoc. Radiol. J. 2021, 72, 577–584. [Google Scholar] [CrossRef] [PubMed]
- Harisinghani, M.G.; Gervais, D.A.; Hahn, P.F.; Cho, C.H.; Jhaveri, K.; Varghese, J.; Mueller, P.R. CT-Guided Transgluteal Drainage of Deep Pelvic Abscesses: Indications, Technique, Procedure-Related Complications, and Clinical Outcome. Radiographics 2002, 22, 1353–1367. [Google Scholar] [CrossRef] [PubMed]
- Amundson, G.M.; Towbin, R.B.; Mueller, D.L.; Seagram, C.G. Percutaneous Transgastric Drainage of the Lesser Sac in Children. Pediatr. Radiol. 1990, 20, 590–593. [Google Scholar] [CrossRef] [PubMed]
- Burnweit, C.; Wesson, D.; Stringer, D.; Filler, R. Percutaneous Drainage of Traumatic Pancreatic Pseudocysts in Children. The J. Trauma: Inj. Infect. Crit. Care 1990, 30, 1273–1277. [Google Scholar] [CrossRef]
- Dotson, J.L.; Nwomeh, B.; Andridge, R.; Anderson, S.E.; Crandall, W.V. Variation in Management of Intra-Abdominal Abscesses in Children with Crohn’s Disease. Inflamm. Bowel Dis. 2013, 19, 818–825. [Google Scholar] [CrossRef] [PubMed]
- Dotson, J.L.; Bashaw, H.; Nwomeh, B.; Crandall, W.V. Management of Intra-Abdominal Abscesses in Children with Crohn’s Disease: A 12-Year, Retrospective Single-Center Review. Inflamm. Bowel. Dis. 2015, 21, 1109–1114. [Google Scholar] [CrossRef] [PubMed]
- Linder, B.J.; Granberg, C.F. Pediatric Renal Abscesses: A Contemporary Series. J. Pediatr. Urol. 2016, 12, e1–e99. [Google Scholar] [CrossRef]
- McCann, J.W.; Maroo, S.; Wales, P.; Amaral, J.G.; Krishnamurthy, G.; Parra, D.; Temple, M.; John, P.; Connolly, B.L. Image-Guided Drainage of Multiple Intraabdominal Abscesses in Children with Perforated Appendicitis: An Alternative to Laparotomy. Pediatr. Radiol. 2008, 38, 661–668. [Google Scholar] [CrossRef]
- McNeeley, M.F.; Vo, N.J.; Prabhu, S.J.; Vergnani, J.; Shaw, D.W. Percutaneous Drainage of Intra-Abdominal Abscess in Children with Perforated Appendicitis. Pediatr. Radiol. 2012, 42, 805–812. [Google Scholar] [CrossRef]
- Narang, M.; Shah, D.; Narang, S.; Gupta, N.; Upreti, L. Ultrasound-Guided Aspiration in Addition to Antibiotics for Treatment of Liver Abscess in Children: A Randomized Controlled Trial. J. Gastroenterol. Hepatol. 2023, 38, 2070–2075. [Google Scholar] [CrossRef]
- Rypens, F.; Dubois, J.; Garel, L.; Deslandres, C.; Saint-Vil, D. Percutaneous Drainage of Abdominal Abscesses in Pediatric Crohn’s Disease. Am. J. Roentgenol. 2007, 188, 579–585. [Google Scholar] [CrossRef]
- St Peter, S.D.; Shah, S.R.; Adibe, O.O.; Sharp, S.W.; Reading, B.; Cully, B.; Holcomb, G.W.; Rivard, D.C. Saline vs Tissue Plasminogen Activator Irrigations after Drain Placement for Appendicitis-Associated Abscess: A Prospective Randomized Trial. J. Am. Coll. Surg. 2015, 221, 390–396. [Google Scholar] [CrossRef]

| Advantages | Disadvantages | |
|---|---|---|
| US | availability low cost no ionizing radiation real-time imaging of needle and catheter | lower specificity prone to image degradation operator dependent |
| CT | high specificity | ionizing radiation |
| MRI | high specificity | availability patient’s immobility, requiring anesthesia in children |
| IPAD Indications | IPAD Contraindications |
|---|---|
|
|
| Advantages | Disadvantages | |
|---|---|---|
| trocar |
|
|
| Seldinger |
|
|
| Study | Study Design | Aim | Results |
|---|---|---|---|
| Amundson GM et al., 1990 [63] | Retrospective study of four pediatric patients. | To assess the feasibility of the transgastric drainage of lesser sac abscesses following pancreatitis. | The approach is feasible. No major complications, minor complications: transient gastric venous bleeding, hematuria, and bleeding into a pseudocyst. |
| Burnweit et al., 1990 [64] | Retrospective study of 13 pediatric patients. | To assess the efficacy of the percutaneous drainage of traumatic pancreatic pseudocysts. | Six pseudocyst resolved spontaneously. Two were treated surgically. Five were treated by percutaneous drainage, with no complications or pseudocyst recurrence at the one-month follow-up. |
| Collins G et al., 2020 [39] | Retrospective study of 42 pediatric patients. | To assess the safety and efficacy of the non-operative management of small (<4 cm) post-appendectomy intra-abdominal abscesses. | Sixteen patients (38%) were treated with percutaneous drainage; twenty-six (62%) patients adopted non-operative management. In the drainage group, three patients required repeat percutaneous drainage and four required operative drainage. The non-operative management of post-appendectomy intra-abdominal abscesses is efficacious and safe. |
| Chung T et al., 1996 [50] | Retrospective study of seven pediatric patients. | To assess the safety and efficacy of the transrectal drainage (TRD) of deep pelvic abscesses using combined transrectal sonographic and fluoroscopic guidance. | Endovaginal US was used for initial catheter guidance, followed by fluoroscopy. General anesthesia was used in all cases. Mean catheter dwelling time: 4 days. 100% clinical success. |
| Dotson JL et al., 2013 [65] | Web-based survey of 248 pediatric gastroenterologists that were members of the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. | To assess the variation in the management of abdominal abscesses in children with Crohn’s disease. | Of the respondents, 52% would choose CT for initial imaging, 26% would choose MRI, and 21% would choose US. US would be preferred for follow-up imaging (47%), followed by MRI (33%) and CT (13%). Of the respondents, 77% would recommend percutaneous drainage as a first-line treatment and 21% as a step-up only after the failure of medical therapy. Only 2% of the respondents would recommend surgery as a first-line treatment. There were no clinically significant associations between treatment strategies and practitioners’ experience. |
| Dotson JL et al., 2015 [66] | Retrospective single-center study of 30 patients. | To determine the characteristics of the management of abdominal abscesses in children with Crohn’s disease in 28 patients who received either medical therapy or percutaneous drainage. | CT was the most common initial and follow-up imaging modality. The medical therapy group received significantly more follow-up CT imaging (67% v. 20%, p = 0.046). No significant differences were identified among the treatment groups for readmissions, complications, or abscess recurrence. After 1 year, 67% of the patients in the medical group and 60% of the patients in the percutaneous drainage group underwent surgery. |
| Gibson CR et al., 2021 [61] | Randomized controlled trial, with a sample size of 56 pediatric patients. | To evaluate the efficacy of once-per-day intracavitary tissue plasminogen activator (tPA) in the treatment of pediatric intra-abdominal abscesses. | Intracavitary tPA has no significant effect on the length of catheter dwell time, procedure time to discharge, or time to resolution. |
| Jamieson DH et al., 1997 [49] | Retrospective study of 46 pediatric patients. | To assess the clinical success rate and long-term (one-year follow-up) complications of simultaneous antibiotic and percutaneous drainage therapy of appendiceal abscesses. | Clinical success rate: 91%. Complications rate: 2%. Patients had more than one catheter inserted: 28%. Patients had additional catheters inserted in a separate session: 15%. Median catheter dwell time: 4 days. |
| Linder BJ et al., 2016 [67] | Retrospective study of three pediatric patients. | To assess the outcomes of pediatric patients with renal abscesses. | Indications for IPAD were the abscess size in two cases and the failure of medical treatment in one case. Clinical success rate: 100%. |
| McCann JW et al., 2008 [68] | Retrospective study of 42 pediatric patients with a total of 100 drainage catheters inserted. | To assess the safety and efficacy of multiple percutaneous drainages in children with acute complicated appendicitis. | Clinical success rate: 92.3%. Of the patients, 43% required reintervention (the other 56% presumably had more than one catheter inserted during the first session). Mean catheter dwell time: 8.2 days. |
| McNeeley MF et al., 2012 [69] | Retrospective study of 33 pediatric patients. | To evaluate the safety and efficacy of percutaneous drainage in children with perforated appendicitis. | Technical success rate: 87.9%. Appendectomy postponement rate: 100%. Large diffuse abscesses significantly increase the rate of technical failure. |
| Narang M et al., 2023 [70] | Randomized controlled trial with a sample size of 110 pediatric patients. | To evaluate the efficacy of ultrasound-guided needle aspiration in addition to antibiotics in children with uncomplicated liver abscesses. | Needle aspiration does not affect the clinical outcome at 6 weeks in children with uncomplicated liver abscesses. Needle aspiration may slightly reduce the duration of fever and abdominal pain/abdominal tenderness. |
| Pereira JK et al., 1996 [48] | Retrospective study of 45 pediatric patients. | To evaluate the efficacy of the transrectal drainage (TRD) and/or percutaneous drainage (PD) of deep pelvic abscesses. | All the patients recovered fully—both TRD and PD are effective in treating deep pelvic abscesses. Sedation was used in 44 procedures, while general anesthesia was used in 1 procedure. Mean catheter dwell times: 4.1 days (PD) and 5.5 days (TRD). |
| Rypens F et al., 2007 [71] | Retrospective study of 15 abscesses in 14 pediatric patients. | To evaluate the safety and efficacy of the percutaneous drainage of abdominal and pelvic abscesses in pediatric Crohn’s disease. | Complete abscess resolution in eight patients, partial in seven. One minor complication: an enterocutaneous fistula. Mean catheter dwell time: 11 days. |
| St Peter SD et al., 2015 [72] | Randomized controlled trial with a sample size of 62 pediatric patients. | To evaluate the efficacy of tPA irrigations after drain placement for appendicitis-associated abscesses. | The duration of hospitalization after drainage was significantly longer with the use of tPA. Medication charges were higher with tPA. There was no difference in the total duration of hospitalization, days of drainage, or days of antibiotics. |
| van Sonnenberg E, 1987 [4] | Retrospective study of 15 abdominal fluid collections. | To evaluate the safety and efficacy of percutaneous drainage. | Initial clinical success rate: 80%. Required surgery at a later time: 13%. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Kuhelj, D.; Langel, C. Image-Guided Percutaneous Drainage of Abdominal Abscesses in Pediatric Patients. Children 2024, 11, 290. https://doi.org/10.3390/children11030290
Kuhelj D, Langel C. Image-Guided Percutaneous Drainage of Abdominal Abscesses in Pediatric Patients. Children. 2024; 11(3):290. https://doi.org/10.3390/children11030290
Chicago/Turabian StyleKuhelj, Dimitrij, and Crt Langel. 2024. "Image-Guided Percutaneous Drainage of Abdominal Abscesses in Pediatric Patients" Children 11, no. 3: 290. https://doi.org/10.3390/children11030290
APA StyleKuhelj, D., & Langel, C. (2024). Image-Guided Percutaneous Drainage of Abdominal Abscesses in Pediatric Patients. Children, 11(3), 290. https://doi.org/10.3390/children11030290






