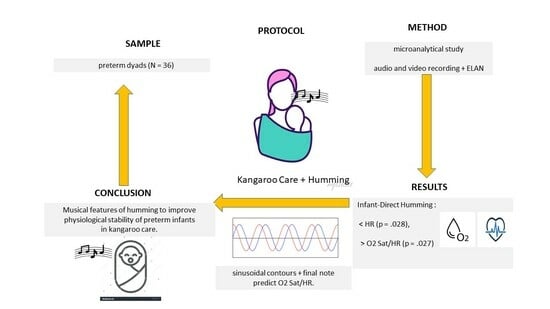
Maternal Humming during Kangaroo Care: Effects on Preterm Dyads’ Physiological Parameters
Abstract
:1. Background
Purpose of the Present Study
2. Method
2.1. Design
2.2. Measures
2.2.1. Recording, Minute-by-Minute, Mothers’ and Infants’ HRs and O2 Saturation
2.2.2. Maternal Vocalizations during the Protocol
2.2.3. Humming Melodic Contours and the Lengthening of the Final Note
2.3. Sample Selection Process
2.4. Participants
2.5. Reliability
3. Results
3.1. Comparison of Outcomes across Conditions
3.2. Effects of Melodic Contours and Lengthening of the Final Note on Preterm Infants’ Hysiological Parameters
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Mulky, S.B.; dú Plessis, A. The Critical Role of the Central Autonomic Nervous System in Fetal-Neonatal Transition. Semin. Pediatr. Neurol. 2018, 28, 29–37. [Google Scholar] [CrossRef]
- Als, H.; McAnulty, G.B. The Newborn Individualized Developmental Care and Assessment Program (NIDCAP) with Kangaroo Mother Care (KMC): Comprehensive Care for Preterm Infants. Curr. Women’s Health Rev. 2011, 7, 288–301. [Google Scholar] [CrossRef] [PubMed]
- Fluharty, M.; Nemeth, L.S.; Logan, A.; Nichols, M. What do neonatal intensive care unit policies tell us about kangaroo care implementation? A Realist Review. Adv. Neonatal Care 2021, 21, E76–E85. [Google Scholar] [CrossRef] [PubMed]
- Buil, A.; Carchon, I.; Apter, G.; Laborne, F.; Granier, M.; Devouche, E. Kangaroo supported diagonal flexion positioning: New insights into skin-to-skin contact for communication between mothers and very preterm infants. Arch. Pédiatrie 2016, 23, 913–920. [Google Scholar] [CrossRef] [PubMed]
- Buil, A.; Sankey, C.; Caeymaex, L.; Gratier, M.; Apter, G.; Vitte, L.; Devouche, E. Skin-to-skin SDF positioning: The key to intersubjective intimacy between mother and very preterm newborn—A pilot matched-pair case-control study. Front. Psychol. 2022, 13, 790313. [Google Scholar] [CrossRef] [PubMed]
- Buil, A.; Caeymaex, L.; Mero, S.; Sankey, C.; Apter, G.; Devouche, E. Kangaroo supported diagonal flexion positioning: Positive impact on maternal stress and postpartum depression risk and on skin-to-skin practice with very preterm infants. J. Neonatal Nurs. 2019, 25, 86–92. [Google Scholar] [CrossRef]
- Arnon, S.; Diamant, C.; Bauer, S.; Regev, R.; Sirota, G.; Litmanovitz, I. Maternal singing during kangaroo care led to autonomic stability in preterm infants and reduced maternal anxiety. Acta Paediatr. 2014, 103, 1039–1044. [Google Scholar] [CrossRef] [PubMed]
- Filippa, M.; Panza, C.; Ferrari, F.; Frassoldati, R.; Kuhn, P.; Balduzzi, S.; D’Amico, R. Systematic review of maternal voice interventions demonstrates increased stability in preterm infants. Acta Paediatr. 2017, 106, 1220–1229. [Google Scholar] [CrossRef] [PubMed]
- Filippa, M.; Della Casa, E.; D’Amico, R.; Picciolini, O.; Lunardi, C.; Sansavini, A.; Ferrari, F. Effects of early vocal contact in the neonatal intensive care unit: Study protocol for a multi-centre, randomised clinical trial. Int. J. Environ. Res. Public Health 2021, 18, 3915. [Google Scholar] [CrossRef]
- Filippa, M.; Nardelli, M.; Della Casa, E.; Berardi, A.; Picciolini, O.; Meloni, S.; Lunardi, C.; Cecchi, A.; Sansavini, A.; Corvaglia, L.; et al. Maternal Singing but Not Speech Enhances Vagal Activity in Preterm Infants during Hospitalization: Preliminary Results. Children 2022, 9, 140. [Google Scholar] [CrossRef]
- Loewy, J.; Stewart, K.; Dassler, A.; Telsey, A.; Homel, P. The effects of music therapy on vital signs, feeding, and sleep in premature infants. Pediatrics 2013, 131, 902–918. [Google Scholar] [CrossRef]
- Haslbeck, F.B.; Jakab, A.; Held, U.; Bassler, D.; Bucher, H.-U.; Hagmann, C. Creative music therapy to promote brain function and brain structure in preterm infants: A randomized controlled pilot study. NeuroImage Clin. 2020, 25, 102171. [Google Scholar] [CrossRef]
- Shoemark, H. Contingent singing: The musicality of companionship with the hospitalized newborn infant. In Therapeutic Voice Work in Music Therapy; Baker, F., Uhlig, S., Eds.; Jessica Kingsley: London, UK, 2011; pp. 229–249. [Google Scholar]
- Shoemark, H. Time Together: A feasible program to promote parent-infant interaction in the NICU. Music. Ther. Perspect. 2018, 36, 6–16. [Google Scholar] [CrossRef]
- Shoemark, H. Returning musicality to parents: Constructing a strategy using parental voice. Int. J. Birth Parent Educ. 2019, 6, 29–32. [Google Scholar]
- Palazzi, A.; Filippa, M.; Meschini, R.; Piccinini, C.A. Music therapy enhances preterm infant’s signs of engagement and sustains maternal singing in the NICU. Infant Behav. Dev. 2021, 64, 101596. [Google Scholar] [CrossRef]
- Yakobson, D.; Gold, C.; Beck, B.D.; Elefant, C.; Bauer-Rusek, S.; Arnon, S. Effects of Live Music Therapy on Autonomic Stability in Preterm Infants: A Cluster-Randomized Controlled Trial. Children 2021, 8, 1077. [Google Scholar] [CrossRef] [PubMed]
- Snow, S.; Bernardi, N.F.; Sabet-Kassouf, N.; Moran, D.; Lehmann, A. Exploring the experience and effects of vocal toning. J. Music Ther. 2018, 55, 221–250. [Google Scholar] [CrossRef] [PubMed]
- Kalyani, B.G.; Venkatasubramanian, G.; Arasappa, R.; Rao, N.P.; Kalmady, S.V.; Behere, R.V.; Rao, H.; Vasudev, M.K.; Gangadhar, B.N. Neurohemodynamic correlates of ‘OM’ chanting: A pilot functional magnetic resonance imaging study. Int. J. Yoga 2011, 4, 3–6. [Google Scholar] [CrossRef] [PubMed]
- Bernardi, N.F.; Codrons, E.; Di-Leo, R.; Vandoni, M.; Cavallaro, F.; Vita, G.; Bernardi, L. Increase in Synchronization of Autonomic Rhythms between Individuals When Listening to Music. Front. Physiol. 2017, 8, 785. [Google Scholar] [CrossRef] [PubMed]
- Gick, M.L. Singing, health and well-being: A health psychologist’s review. Psychomusicology 2011, 21, 176–207. [Google Scholar] [CrossRef]
- Gick, M.L.; Jennifer, J.N. Singing for respiratory health: Theory, evidence and challenges. Health Promot. Int. 2016, 3, 725–734. [Google Scholar] [CrossRef]
- Arnon, S.; Shapsa, A.; Forman, L.; Regev, R.; Bauer, S.; Litmanovitz, I.; Dolfin, T. Live Music is Beneficial to Preterm Infants in the Neonatal Intensive Care Unit Environment. Birth 2006, 33, 131–136. [Google Scholar] [CrossRef]
- Garunkstiene, R.; Buinauskiene, J.; Uloziene, I.; Markuniene, E. Controlled trial of live versus recorded lullabies in preterm infants. Nord. J. Music. Ther. 2014, 23, 71–88. [Google Scholar] [CrossRef]
- Namjoo, R.; Mehdipour-Rabori, R.; Bagherian, B.; Nematollahi, M. Comparing the effectiveness of mother’s live lullaby and recorded lullaby on physiological responses and sleep of preterm infants: A clinical trial study. J. Complement. Integr. Med. 2021, 19, 121–129. [Google Scholar] [CrossRef]
- Standley, J.M. Music therapy research in the NICU: An updated meta-analysis. Neonatal Netw. 2012, 31, 311–316. [Google Scholar] [CrossRef] [PubMed]
- Johnston, C.C.; Filion, F.; Nuyt, A.M. Recorded maternal voice for preterm neonates undergoing heel lance. Adv. Neonatal Care 2007, 7, 258–266. [Google Scholar] [CrossRef] [PubMed]
- Bozzette, M. Healthy preterm infant responses to taped maternal voice. J. Perinat. Neonatal Nurs. 2008, 22, 307–316. [Google Scholar] [CrossRef] [PubMed]
- Picciolini, O.; Porro, M.; Meazza, A.; Giannì, M.L.; Rivoli, C.; Lucco, G.; Barretta, F.; Bonzini, M.; Mosca, F. Early exposure to maternal voice: Effects on preterm infants’ development. Early Hum. Dev. 2014, 90, 287–292. [Google Scholar] [CrossRef] [PubMed]
- Doheny, L.; Hurwitz, S.; Insoft, R.; Ringer, S.; Lahav, A. Exposure to biological maternal sounds improves cardiorespiratory regulation in extremely preterm infants. J. Matern. Fetal Neonatal Med. 2012, 25, 1591–1594. [Google Scholar] [CrossRef] [PubMed]
- Filippa, M.; Devouche, E.; Arioni, C.; Imberty, M.; Gratier, M. Live maternal speech and singing have beneficial effects on hospitalized preterm infants. Acta Paediatr. 2013, 102, 1017–1020. [Google Scholar] [CrossRef] [PubMed]
- Cevasco, A.M. The effects of mothers’ singing on full-term and preterm infants and maternal emotional responses. J. Music Ther. 2008, 45, 273–306. [Google Scholar] [CrossRef]
- Provenzi, L.; Broso, S.; Montirosso, R. Do mothers sound good? A systematic review of the effects of maternal voice exposure on preterm infants’ development. Neurosci. Biobehav. Rev. 2018, 88, 42–50. [Google Scholar] [CrossRef]
- Trainor, L.J. Infant preferences for infant-directed versus non infant-directed playsongs and lullabies. Infant Behav. Dev. 1996, 19, 83–92. [Google Scholar] [CrossRef]
- Trainor, L.J.; Clark, E.D.; Huntley, A.; Adams, B.A. The acoustic basis of preferences for infant-directed singing. Infant Behav. Dev. 1997, 20, 383–396. [Google Scholar] [CrossRef]
- Longhi, E. ‘Songese’: Maternal structuring of musical interaction with infants. Psychol. Music 2009, 37, 195–213. [Google Scholar] [CrossRef]
- Bergeson, T.R.; Trehub, S.E. Absolute pitch and tempo in mothers’ songs to infants. Psychol. Sci. 2002, 13, 72–75. [Google Scholar] [CrossRef] [PubMed]
- Nakata, T.; Trehub, S.A. Expressive timing and dynamics in infant-directed and non-infant-directed singing. Psychomusicol. Music Mind Brain 2011, 21, 45–53. [Google Scholar] [CrossRef]
- Shenfield, T.; Trehub, S.E.; Nakata, T. Maternal singing modulates infant arousal. Psychol. Music 2003, 31, 365–375. [Google Scholar] [CrossRef]
- Trehub, S.E.; Trainor, L. Singing to infants: Lullabies and play songs. Adv. Infancy Res. 1998, 12, 43–78. [Google Scholar]
- Falk, S.; Kello, C.T. Hierarchical organization in the temporal structure of infant-direct speech and song. Cognition 2017, 163, 80–86. [Google Scholar] [CrossRef]
- Gratier, M. Expressive timing and interactional synchrony between mothers and infants: Cultural similarities, cultural differences, and the immigration experience. Cogn. Dev. 2003, 18, 533–554. [Google Scholar] [CrossRef]
- Trainor, L.J.; Adams, B. Infants’ and adults’ use of duration and intensity cues in the segmentation of tone patterns. Percept. Psychophys. 2000, 62, 333–340. [Google Scholar] [CrossRef] [PubMed]
- Carvalho, M.E.; Justo, J.M.; Gratier, M.; Rodrigues, H.F. Infants’ overlapping vocalizations during maternal humming: Contributions to the synchronization of preterm dyads. Psychol. Music 2020, 03057356209. [Google Scholar] [CrossRef]
- Falk, S. Melodic versus intonational coding of communicative functions: A comparison of tonal contours in infant-directed song and speech. Psychomusicol. Music Mind Brain 2011, 21, 54–68. [Google Scholar] [CrossRef]
- Carvalho, M.E.S.; de Miranda Justo, J.M.R.; Sá, C.; Gratier, M.; Rodrigues, H.F. Melodic contours of maternal humming to preterm infants in kangaroo care and infants’ overlapping vocalizations: A microanalytical study. Psychol. Music 2022, 50, 1910–1924. [Google Scholar] [CrossRef]
- Papousek, M. Intuitive parenting: A hidden source of musical stimulation in infancy. In Musical Beginnings. Origins and Development of Musical Competence; Deliege, I., Sloboda, J., Eds.; Oxford University Press: Oxford, UK, 1996; pp. 88–112. [Google Scholar]
- Carvalho, M.E.S.; Justo, J.M.; Gratier, M.; Tomé, T.; Pereira, E.; Rodrigues, H. Vocal responsiveness of preterm infants to maternal infant-directed speaking and singing during skin-to-skin contact (Kangaroo Care) in the NICU. Infant Behav. Dev. 2019, 57, 101332. [Google Scholar] [CrossRef]
- Brazelton, T.B.; Nugent, J.K. The Neonatal Behavioral Assessment Scale, 4th ed.; Mac Keith Press: London, UK, 2011. [Google Scholar]
- Gratier, M.; Devouche, E.; Guellaï, B.; Infanti, R.; Yilmaz, E.; Parlato-Oliveira, E. Early development of turn-taking in vocal interaction between mothers and infants. Front. Psychol. 2015, 6, 236–245. [Google Scholar] [CrossRef]
- Carvalho, E.; Rincon, R.; Justo, J.; Rodrigues, H. Multimodal Interaction between a Mother and Her Twin Preterm Infants (Male and Female) in Maternal Speech and Humming during Kangaroo Care: A Microanalytical Case Study. Children 2021, 8, 754. [Google Scholar] [CrossRef]
- Goldman, J.; Goldman, A. The Humming Effect: Sound Healing for Health and Happiness; Healing Arts Press: Rochester, NY, USA, 2017. [Google Scholar]
- Blumenfeld, H.; Eisenfeld, L. Does a mother singing to her premature baby affect feeding in the neonatal intensive care unit? Clin. Pediatr. 2006, 45, 65–70. [Google Scholar] [CrossRef]
- Standley, J.M. The effect of music and multimodal stimulation on responses of premature infants in neonatal intensive care. Pediatr. Nurs. 1998, 24, 532–538. [Google Scholar] [PubMed]


| Variables | n | % | M | SD | Min.–Max. |
|---|---|---|---|---|---|
| maternal age | 34.20 | 5.63 | 21–48 | ||
| maternal education | 15.33 | 3.69 | 6–24 | ||
| Portuguese nationality | 26 | 72.22 | |||
| African and Brazilian nationality | 10 | 27.78 | |||
| male infants | 20 | 55.55 | |||
| female infants | 16 | 44.44 | |||
| infants’ gestational age at birth * | 30.40 | 2.44 | 25.42–34.42 | ||
| infants’ chronological age at observation ** | 26.5 | 19.99 | 4–81 | ||
| infants’ weight at birth (g) | 1265.47 | 308.20 | 590–2017 | ||
| infants’ weight at observation (g) | 1538.05 | 237.72 | 1060–2185 |
| Physiological Parameters | Silent Baseline | Humming | Speech | |||
|---|---|---|---|---|---|---|
| M (SD) | Min.–Max. | M (SD) | Min.–Max. | M (SD) | Min.–Max. | |
| HR * | 79.02 (10.17) | 47.67–97.67 | 81.55 (10.75) | 49.00–101.00 | 83.47 (10.39) | 50.67–101.00 |
| O2 saturation ** | 97.90 (1.14) | 94.00–99.00 | 97.92 (1.10) | 94.33–99.00 | 97.75 (1.14) | 94.33–99.00 |
| P. O2 S/HR *** | 1.26 (0.19) | 0.99–2.06 | 1.22 (0.19) | 0.95–2.00 | 1.19 (0.18) | 0.95–1.93 |
| Physiological Parameters | Silent Baseline | Humming | Speech | |||
|---|---|---|---|---|---|---|
| M (SD) | Min.–Max. | M (SD) | Min.–Max. | M (SD) | Min.–Max. | |
| HR * | 156.24 (11.37) | 137.00–181.00 | 153.31 (13.54) | 119.00–185.67 | 157.32 (12.08) | 130.00–188.00 |
| O2 saturation ** | 97.68 (3.33) | 86.36–100.00 | 97.19 (3.15) | 88.00–100.00 | 97.11 (3.02) | 88.00–100.00 |
| P. O2 S/HR *** | 0.63 (0.05) | 0.52–0.73 | 0.64 (0.06) | 0.50–0.74 | 0.62 (0.06) | 0.51–0.77 |
| Physiological Parameters | Comparisons | t | df | p | Cohen’s d |
|---|---|---|---|---|---|
| HR * | BL vs. Hum | −4.89 | 33 | <0.001 | −0.839 |
| BL vs. Sp | −5.39 | 33 | <0.001 | −0.926 | |
| Hum vs. Sp | −2.04 | 32 | 0.050 | −0.355 | |
| O2 saturation ** | BL vs. Hum | −0.11 | 33 | 0.917 | −0.018 |
| BL vs. Sp | 1.59 | 33 | 0.121 | 0.273 | |
| Hum vs. Sp | 1.75 | 32 | 0.089 | −0.355 | |
| Prop. O2 saturation/HR ratio *** | BL vs. Hum | 5.06 | 33 | <0.001 | 0.868 |
| BL vs. Sp | 5.51 | 33 | <0.001 | 0.945 | |
| Hum vs. Sp | 2.29 | 32 | 0.029 | 0.398 |
| Physiological Parameters | Comparisons | t | df | p | Cohen’s d |
|---|---|---|---|---|---|
| HR * | BL vs. Hum | 1.62 | 35 | 0.114 | 0.270 |
| BL vs. Sp | −0.95 | 35 | 0.349 | −0.158 | |
| Hum vs. Sp | −2.29 | 35 | 0.028 | −0.382 | |
| O2 saturation ** | BL vs. Hum | 1.06 | 35 | 0.297 | 0.177 |
| BL vs. Sp | 1.32 | 34 | 0.195 | 0.224 | |
| Hum vs. Sp | 0.00 | 34 | 1.000 | 0.000 | |
| Prop. O2 saturation/HR *** | BL vs. Hum | −1.26 | 35 | 0.218 | −0.209 |
| BL vs. Sp | 1.37 | 34 | 0.179 | 0.232 | |
| Hum vs. Sp | 2.31 | 34 | 0.027 | 0.390 |
| Model | R | R2 | Adjusted R2 | St. Error of Estimate | R2 Change | F Change | df1 | df2 | Sig. of F Change |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 0.331 | 0.109 | 0.020 | 13.186 | 0.109 | 1.228 | 3 | 30 | 0.317 |
| 2 | 0.336 | 0.113 | −0.046 | 13.624 | 0.003 | 0.051 | 2 | 28 | 0.951 |
| 3 | 0.575 | 0.331 | 0.151 | 12.275 | 0.218 | 4.246 | 2 | 26 | 0.025 |
| Model | R | R2 | Adjusted R2 | St. Error of the Estimate | R2 Change | F Change | df1 | df2 | Sig. of F Change |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 0.369 | 0.136 | 0.050 | 0.051 | 0.136 | 1.574 | 3 | 30 | 0.216 |
| 2 | 0.395 | 0.156 | 0.005 | 0.052 | 0.020 | 0.327 | 2 | 28 | 0.724 |
| 3 | 0.587 | 0.345 | 0.168 | 0.048 | 0.189 | 3.749 | 2 | 26 | 0.037 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Carvalho, M.E.S.; Justo, J.M.R.M. Maternal Humming during Kangaroo Care: Effects on Preterm Dyads’ Physiological Parameters. Children 2024, 11, 373. https://doi.org/10.3390/children11030373
Carvalho MES, Justo JMRM. Maternal Humming during Kangaroo Care: Effects on Preterm Dyads’ Physiological Parameters. Children. 2024; 11(3):373. https://doi.org/10.3390/children11030373
Chicago/Turabian StyleCarvalho, Maria Eduarda Salgado, and João Manuel Rosado Miranda Justo. 2024. "Maternal Humming during Kangaroo Care: Effects on Preterm Dyads’ Physiological Parameters" Children 11, no. 3: 373. https://doi.org/10.3390/children11030373