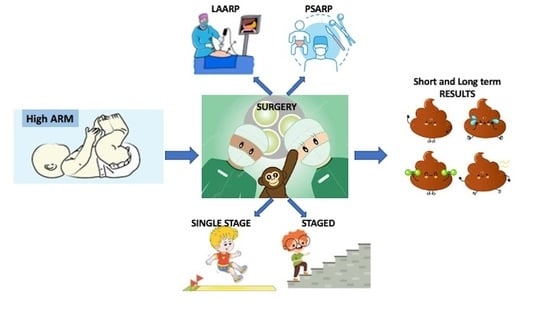
Short and Long-Term Outcomes of PSARP versus LAARP and Single versus Staged Repair for Infants with High-Type Anorectal Malformations: A Systematic Review and Meta-Analysis
Abstract
:1. Introduction
2. Material and Methods
2.1. Data Sources and Study Selection
2.2. Statistical Analysis
2.3. Quality Assessment
3. Results
- Seven papers (254 pts; 121 PSARP, 133 LAARP) in the systematic review and in the meta-analysis to compare the postoperative outcomes of PSARP and LAARP in infants with high-type ARMs [1,2,3,8,9,10,11]. Only one randomized controlled study was included [10]. One further study prospectively evaluated the outcomes of the patients [1]. All other studies were retrospective.
3.1. PSARP versus LAARP Procedures
3.2. Single-Stage versus Staged Procedures
4. Discussion
Limitations of the Study
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Conflicts of Interest
References
- England, R.J.; Warren, S.L.; Bezuidenhout, L.; Numanoglu, A.; Millar, A.J. Laparoscopic repair of anorectal malformations at the Red Cross War Memorial Children’s Hospital: Taking stock. J. Pediatr. Surg. 2012, 47, 565–570. [Google Scholar] [CrossRef] [PubMed]
- Tong, Q.-S.; Tang, S.-T.; Pu, J.-R.; Mao, Y.-Z.; Wang, Y.; Li, S.-W.; Cao, Q.-Q.; Ruan, Q.-L. Laparoscopically assisted anorectal pull-through for high imperforate anus in infants: Intermediate results. J. Pediatr. Surg. 2011, 46, 1578–1586. [Google Scholar] [CrossRef] [PubMed]
- Kimura, O.; Iwai, N.; Sasaki, Y.; Tsuda, T.; Deguchi, E.; Ono, S.; Furukawa, T. Laparoscopic versus open abdominoperineal rectoplasty for infants with high-type anorectal malformation. J. Pediatr. Surg. 2010, 45, 2390–2393. [Google Scholar] [CrossRef] [PubMed]
- Xiao, H.; Huang, R.; Chen, L. The midterm outcomes of 1-stage versus 3-stage laparoscopic-assisted anorectoplasty in anorectal malformations with rectoprostatic fistula and rectobulbar fistula: A retrospective cohort study. Medicine 2018, 97, e11843. [Google Scholar] [CrossRef] [PubMed]
- Leva, E.; Macchini, F.; Arnoldi, R.; Di Cesare, A.; Gentilino, V.; Fumagalli, M.; Mosca, F.; Bhuiyan, A.; Torricelli, M.; Banu, T. Single-stage surgical correction of anorectal malformation associated with rectourinary fistula in male neonates. J. Neonatal Surg. 2013, 2, 3. [Google Scholar] [CrossRef] [PubMed]
- Nagdeve, N.; Naik, H.; Bhingare, P. Neonatal posterior sagittal anorectoplasty for a subset of males with high anorectal malformations. J. Indian Assoc. Pediatr. Surg. 2011, 16, 126–128. [Google Scholar] [CrossRef]
- Menon, P.; Rao, K.L.N.; Sinha, A.K.; Lokesha, K.; Samujh, R.; Mahajan, J.K.; Kanojia, R.P.; Bawa, M. Anorectal Malformations in Males: Pros and Cons of Neonatal versus Staged Reconstruction for High and Intermediate Varieties. J. Indian Assoc. Pediatr. Surg. 2017, 22, 83–86. [Google Scholar]
- Bailez, M.M.; Cuenca, E.S.; Mauri, V.; Solana, J.; Di Benedetto, V. Outcome of males with high anorectal malformations treated with laparoscopic-assisted anorectal pull-through: Preliminary results of a comparative study with the open approach in a single institution. J. Pediatr. Surg. 2011, 46, 473–477. [Google Scholar] [CrossRef]
- Yazaki, Y.; Koga, H.; Ochi, T.; Okawada, M.; Doi, T.; Lane, G.J.; Yamataka, A. Surgical management of recto-prostatic and recto-bulbar anorectal malformations. Pediatr. Surg. Int. 2016, 32, 939–944. [Google Scholar] [CrossRef]
- Yang, J.; Zhang, W.; Feng, J.; Guo, X.; Wang, G.; Weng, Y.; Sun, X.; Yu, D. Comparison of clinical outcomes and anorectal manometry in patients with congenital anorectal malformations treated with posterior sagittal anorectoplasty and laparoscopically assisted anorectal pull through. J. Pediatr. Surg. 2009, 44, 2380–2383. [Google Scholar] [CrossRef]
- Lin, C.L.; Wong KK, Y.; Lan LC, L.; Chen, C.C.; Tam, P.K.H. Earlier appearance and higher incidence of the rectoanal relaxation reflex in patients with imperforate anus repaired with laparoscopically assisted anorec- toplasty. Surg. Endosc. 2003, 17, 1646–1649. [Google Scholar] [CrossRef]
- Agrawal, V.; Sharma, D.; Tiwari, A.; Mishra, R.; Acharya, H. Transperineal Intracath Meconiolysis and Evacuation Technique of “Distended” Bowel Evacuation for One-Stage Laparoscopic Anorectoplasty for High Anorectal Malformations in Males. J. Laparoendosc. Adv. Surg. Tech. A 2020, 30, 701–705. [Google Scholar] [CrossRef]
- Liu, G.; Yuan, J.; Geng, J.; Wang, C.; Li, T. The treatment of high and intermediate anorectal malformations: One stage or three procedures? J. Pediatr. Surg. 2004, 39, 1466–1471. [Google Scholar] [CrossRef] [PubMed]
- Lauriti, G.; Di Renzo, D.; Chiesa, P.L.; Zani, A.; Pierro, A. One-stage repair of anorectal malformations in females with vestibular fistula: A systematic review and meta-analysis. Pediatr. Surg. Int. 2019, 35, 77–85. [Google Scholar] [CrossRef] [PubMed]
- Hartford, L.; Brisighelli, G.; Gabler, T.; Westgarth-Taylor, C. Single-stage procedures for anorectal malformations: A systematic review and meta-analysis. J. Pediatr. Surg. 2022, 57, 75–84. [Google Scholar] [CrossRef] [PubMed]
- PROSPERO International Prospective Register of Systematic Reviews. Available online: https://www.crd.york.ac.uk/prospero (accessed on 31 January 2024).
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Hozo, S.P.; Djulbegovic, B.; Hozo, I. Estimating the mean and variance from the median, range, and the size of a sample. BMC Med. Res. Methodol. 2005, 20, 13. [Google Scholar] [CrossRef] [PubMed]
- Review Manager (RevMan). The Nordic Cochrane Centre; The Cochrane Collaboration: Copenhagen, Denmark, 2014. [Google Scholar]
- Slim, K.; Nini, E.; Forestier, D.; Kwiatkowski, F.; Panis, Y.; Chipponi, J. Methodological index for non-randomized studies (MINORS): Development and validation of a new instrument. ANZ J. Surg. 2003, 73, 712–716. [Google Scholar] [CrossRef]
- Guyatt, G.H.; Oxman, A.D.; Vist, G.E.; Kunz, R.; Falck-Ytter, Y.; Alonso-Coello, P.; Schünemann, H.J. GRADE: An emerging consensus on rating quality of evidence and strength of recommendations. BMJ 2008, 336, 924–926. [Google Scholar] [CrossRef]
- Dupont, W.D.; Plummer, W.D. Power and sample size calculations: A review and computer program. Control. Clin. Trials 1990, 11, 116–128. [Google Scholar] [CrossRef]
- Leung, M.W.Y.; Wong, B.P.Y.; Leung, A.K.P.; Cho, J.S.Y.; Leung, E.T.Y.; Chao, N.S.Y.; Chung, K.W.; Kwok, W.K.; Liu, K.K.W. Electrical stimulation and biofeedback exercise of pelvic floor muscle for children with faecal incontinence after surgery for anorectal malformation. Pediatr. Surg. Int. 2006, 22, 975–978. [Google Scholar] [CrossRef]
- Zheng, S.; Xiao, X.; Huang, Y. Single-stage correction of imperforate anus with a rectourethral or a rectovestibula fistula by semi-posterior sagittal anorectoplasty. Pediatr. Surg. Int. 2008, 24, 671–676. [Google Scholar] [CrossRef]
- Li, L.; Yu, Q.; Huang, L. One-stage correction of high imperforate anus with laparoscopy-assisted anorectoplasty. Chin. J. Minim. Invasive Surg. 2003, 3, 199–201. [Google Scholar]
- Shea, B.J.; Grimshaw, J.M.; Wells, G.A.; Boers, M.; Andersson, N.; Hamel, C.; Porter, A.C.; Tugwell, P.; Moher, D.; Bouter, L.M. Development of AMSTAR: A measurement tool to assess the methodological quality of systematic reviews. BMC Med. Res. Methodol. 2007, 7, 10. [Google Scholar] [CrossRef]







| Publication | |
|---|---|
| Language | English |
| Time period | January 1984–November 2023 |
| Subject | Human studies |
| Study type | Retrospective |
| Prospective | |
| Case-control | |
| Cohort | |
| Excluded | Case-report |
| Case series (<10 patients) | |
| Editorials | |
| Letters | |
| Grey Literature | |
| Keywords | anorectal malformation |
| posterior sagittal anorectoplasty | |
| one stage | |
| single stage | |
| laparoscopic-assisted anorectoplasty |
| 3-Stage PSARP vs. 1-Stage | |||||
|---|---|---|---|---|---|
| Paper | Pts | BW | GA | Age at Surgery | Associated Anomalies |
| Xiao [4] | 56 3-stage 36 1-stage 20 | NR | NR | 3-stage 4.9 ± 1.2 (3–7) months 1-stage 39.8 ± 8.1 (30–52) hours | 3-stage: 15 cardiac anomalies 5 VUR 5 undescended testes 2 hypospadias 6 hydronephrosis 4 spina bifida occulta 5 partial sacral agenesis 1 tethered cord 1-stage: 10 cardiac anomalies 2 VUR 1 undescended testis 1 hypospadias 2 hydronephrosis 2 spina bifida occulta 4 partial sacral agenesis |
| Leva [5] | 23 3-stage 4 1-stage 19 | 3-stage 2.9–3.4 kg 1-stage 2.4–3.5 kg | 3-stage at term 1-stage 35–41 w | 3-stage: none 1-stage: 2 ASD 1 VSD 1 pulmonary stenosis 4 VUR 3 hypospadias 1 MCKD 1 ectopic kidney | |
| Nagdeve [6] | NR | NR | NR | NR | NR |
| Menon [7] | NR | NR | NR | NR | NR |
| Agrawal [12] | 15 1 stage | 2.5 ± 0.4 kg | 36 ± 5 weeks | ||
| Liu [13] | 113 3-stage 43 1-stage 65 | NR | NR | NR | 3-stage: 2 hypospadias 3 sacral anomalies 3 cryptorchidism 3 inguinal hernia 3 trisomy21 1-stage: 5 sacral anomalies 1 hypospadia 1 cryptorchidism |
| PSARP vs. LAARP | |||||
| England [1] | 53 PSARP 19 LAARP 24 | PSARP NR LAARP 3 (2–3) kg median | NR | PSARP 8 (4–39) months (median) LAARP 7 (2–15) months (median) | PSARP NR LAARP 3 VSD 1 pulmonary stenosis 1 MCKD 1 hydronephrosis 2 renal ectopia 1 VUR 3 renal agenesis 1 absent thumb 1 rib fusion 1 dysmorphism |
| Tong [2] | 61 PSARP 28 LAARP 33 | NR | NR | PSARP 4.9 (3–11) months LAARP 5.3 (3–10) months | |
| Kimura [3] | 28 PSARP 15 LAARP 13 | NR | NR | NR | NR |
| Bailez [8] | 32 PSARP 15 LAARP 17 | NR | NR | PSARP Rectoprostatic f. 29.2 months Rectovesical f. 25.7 months LAARP Rectoprostatic f. 22 months Rectovesical f. 37.5 months | 25/32 (78%) pts-associated anomalies |
| Yazaki [9] | 45 PSARP 19 LAARP 26 | NR | NR | PSARP Rectoprostatic f. 4 ± 3.5 months Rectobulbar f. 8.2 ± 5.1 months LAARP Rectoprostatic f. 7.6 ± 3 months Rectobulbar f. 8.1 ± 4 months | NR |
| Yang [10] | 23 PSARP 12 LAARP 11 | NR | NR | NR | NR |
| Lin [11] | 16 PSARP 10 LAARP 6 | NR | NR | NR | PSARP 2 hypospadias 1 hydronephrosis 1 trisomy 21 LAARP 1 cardiac anomaly 1 hypospadias 1 trisomy 21 |
| Outcomes | PSARP | LAARP | p-Value |
|---|---|---|---|
| Length of hospitalization, days | 14.4 ± 0.2 | 10.9 ± 0.5 | <0.0001 |
| Post-operative complications, n of pts (%) | 31/107 (28.9) | 30/121 (24.7) | 0.69 |
| Rectal prolapse, n of pts (%) | 19/88 (21.6) | 17/97 (17.5) | 0.95 |
| Voluntary bowel movements, n of pts (%) | 74/100 (74) | 66/79 (83.5) | 0.43 |
| Soiling, n of pts (%) | 15/33 (45.5) | 10/21 (47.6) | 0.74 |
| Outcomes | Single Stage | Staged | p-Value |
|---|---|---|---|
| Voluntary bowel movements, n of pts (%) | 61/84 (72.6) | 74/110 (67.3) | 0.55 |
| Soiling, n of pts (%) | 4/20 (20) | 6/36 (16) | 1 |
| Constipation, n of pts (%) | 6/20 (30) | 9/36 (25) | 1 |
| Item | England [1] | Tong [2] | Kimura [3] | Xiao [4] | Menon [7] | Bailez [8] | Yazaki [9] | Yang [10] | Lin [11] | Liu [13] |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. A clearly stated aim | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 2. Inclusion of consecutive patients | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 3. Prospective collection of data | 2 | 0 | 0 | 0 | 0 | 0 | 0 | 2 | 0 | 0 |
| 4. Endpoints appropriate to the aim of the study | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 5. Unbiased assessment of the study endpoint | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 6. Follow-up period appropriate to the aim of the study | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 1 | 2 |
| 7. Loss to follow-up less than 5% | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 8. Prospective calculation of the study size | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
| 9. An adequate control group | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 10. Contemporary groups | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| 11. Baseline equivalence of groups | 2 | 2 | 2 | 2 | 1 | 2 | 2 | 2 | 2 | 2 |
| 12. Adequate statistical analyses | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 | 2 |
| Total score | 18 | 16 | 16 | 16 | 14 | 16 | 16 | 18 | 15 | 16 |
| Quality Assessment | No. of Patients | Effect | Quality | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of Studies | Study Design | Risk of Bias | Inconsistency | Indirectness | Imprecision | Other Considerations | Cases | Controls | Relative (95% CI) | Absolute (95% CI) | |
| LOS in LAARP versus PSARP | LAARP | PSARP | |||||||||
| 2 | OS | Moderate a | Low | Not serious | Serious b | None | 44 | 40 | --- | MD 3.53 lower (from 2.81 to 4.26 lower) | ⊗OOOVERY LOW |
| Complication in LAARP versus PSARP | LAARP | PSARP | |||||||||
| 6 | OS | Moderate a | Low | Not serious | Serious b | None | 30/121 (24.8%) | 31/107 (28.9%) | RR 1.12 (0.64, 1.96) | 41 fewer per 1000 (from 328 fewer to 123 more) | ⊗⊗OOLOW |
| Rectal prolapse in LAARP versus PSARP | LAARP | PSARP | |||||||||
| 6 | OS | Moderate a | Moderate | Not serious | Serious b | None | 17/97 (17.5%) | 19/88 (21.6%) | RR 0.96 (0.29, 3.15) | 41 fewer per 1000 (from 2204 fewer to 728 more) | ⊗OOOVERY LOW |
| Voluntary bowel movements in LAARP versus PSARP | LAARP | PSARP | |||||||||
| 6 | OS | Moderate a | Moderate | Not serious | Serious b | None | 66/79 (83.5%) | 74/100 (74.0%) | RR 0.93 (0.77, 1.12) | 95 more per 1000 (from 163 fewer to 312 more) | ⊗⊗OOLOW |
| Soiling in LAARP versus PSARP | LAARP | PSARP | |||||||||
| 2 | OS | Moderate a | Low | Not serious | Serious b | None | 10/21 (47.6%) | 15/33 (45.5%) | RR 0.90 (0.50, 1.62) | 21 more per 1000 (from 130 fewer to 105 more) | ⊗OOOVERY LOW |
| Voluntary bowel movements in one-stage versus staged PSARP | One stage | Staged | |||||||||
| 3 | OS | Moderate a | Moderate | Not serious | Serious b | None | 61/84 (72.6%) | 74/110 (67.3%) | RR 1.09 (0.83, 1.43) | 53 more per 1000 (from 100 fewer to 253 more) | ⊗OOOVERY LOW |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Miscia, M.E.; Lauriti, G.; Di Renzo, D.; Cascini, V.; Lisi, G. Short and Long-Term Outcomes of PSARP versus LAARP and Single versus Staged Repair for Infants with High-Type Anorectal Malformations: A Systematic Review and Meta-Analysis. Children 2024, 11, 376. https://doi.org/10.3390/children11030376
Miscia ME, Lauriti G, Di Renzo D, Cascini V, Lisi G. Short and Long-Term Outcomes of PSARP versus LAARP and Single versus Staged Repair for Infants with High-Type Anorectal Malformations: A Systematic Review and Meta-Analysis. Children. 2024; 11(3):376. https://doi.org/10.3390/children11030376
Chicago/Turabian StyleMiscia, Maria Enrica, Giuseppe Lauriti, Dacia Di Renzo, Valentina Cascini, and Gabriele Lisi. 2024. "Short and Long-Term Outcomes of PSARP versus LAARP and Single versus Staged Repair for Infants with High-Type Anorectal Malformations: A Systematic Review and Meta-Analysis" Children 11, no. 3: 376. https://doi.org/10.3390/children11030376
APA StyleMiscia, M. E., Lauriti, G., Di Renzo, D., Cascini, V., & Lisi, G. (2024). Short and Long-Term Outcomes of PSARP versus LAARP and Single versus Staged Repair for Infants with High-Type Anorectal Malformations: A Systematic Review and Meta-Analysis. Children, 11(3), 376. https://doi.org/10.3390/children11030376