Missed Monteggia Injuries in Children and Adolescents: A Treatment Algorithm
Abstract
:1. Introduction
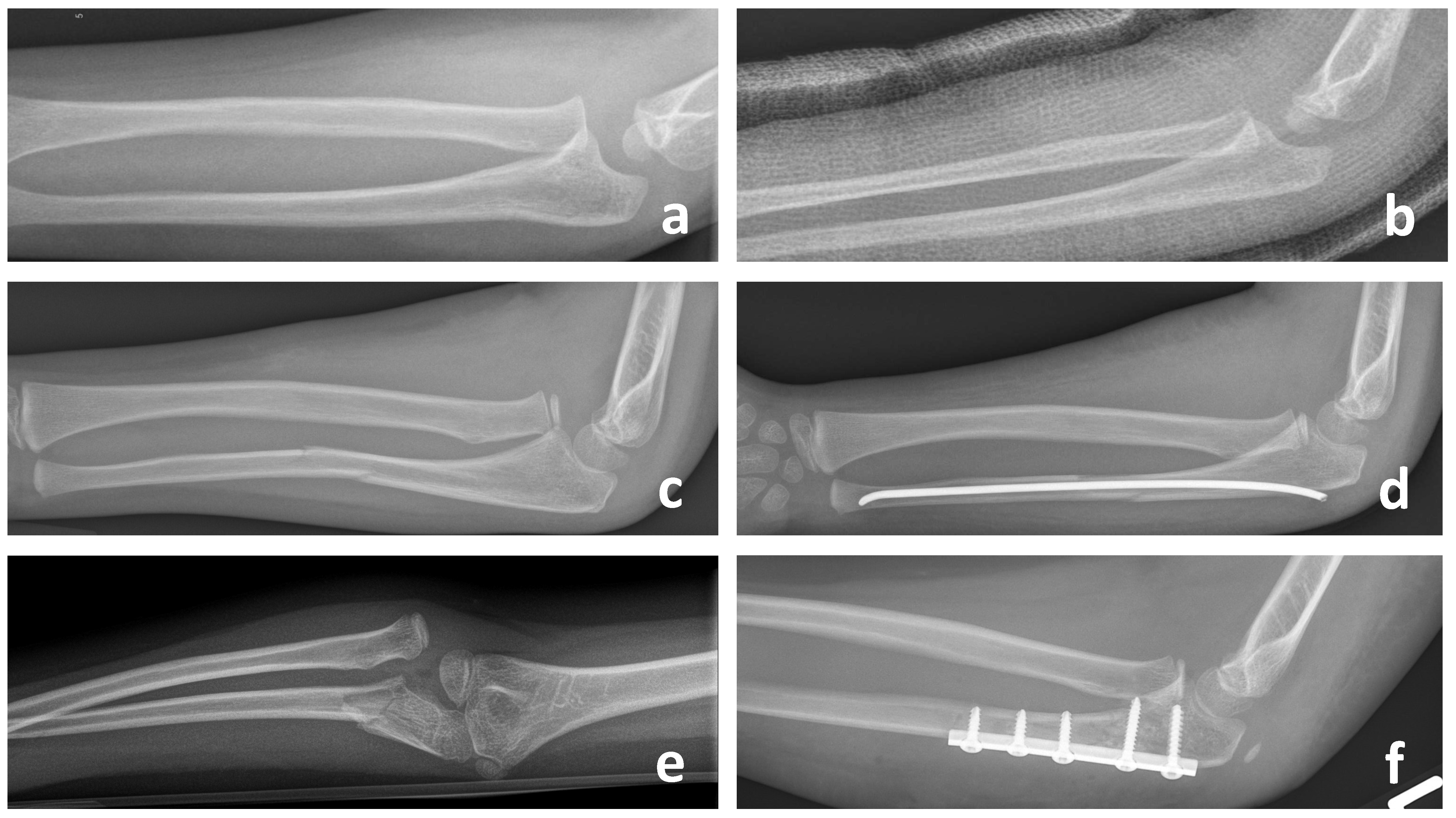
2. Examination and Radiographic Assessment
3. Physical Therapy
4. Operative Therapy
4.1. Reconstruction Procedures
4.1.1. Ulnar Osteotomy and Correction with External Fixator
4.1.2. Ulnar Osteotomy and Correction with Plate Osteosynthesis
4.1.3. Ulnar Osteotomy and Correction via Gradual Lengthening with External Fixator
4.1.4. Annular Ligament Reconstruction (ALR)
4.2. Rescue Procedures
4.2.1. Functional Radial Head Resection According to Slongo
4.2.2. Radial Head Resection with or without Hemi-Interposition Arthroplasty
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Bado, J.L. The Monteggia lesion. Orthop. Relat. Res. 1967, 50, 71–86. [Google Scholar] [CrossRef]
- Lidder, S.; Heidari, N.; Amerstorfer, F.; Grechenig, S.; Weinberg, A.M. Median nerve palsy following elastic stable intramedullary nailing of a Monteggia fracture: An unusual case and review of the literature. Case Rep. Med. 2011, 2011, 682454. [Google Scholar] [CrossRef] [PubMed]
- Bado, J.L. La lesion de Monteggia; Inter-Medica-Sarandi: Sarandë, Albania, 1958; 140p. [Google Scholar]
- Gleeson, A.P.; Beattie, T.F. Monteggia fracture-dislocation in children. Emerg. Med. J. 1994, 11, 192–194. [Google Scholar] [CrossRef] [PubMed]
- Goyal, T.; Arora, S.S.; Banerjee, S.; Kandwal, P. Neglected Monteggia fracture dislocations in children: A systemic review. J. Pediatr. Orthop. Part B 2015, 24, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Goh, S.H. Monteggia fracture-dislocation with bowing of the ulna: A pitfall for the unwary emergency physician. Eur. J. Emerg. Med. 2008, 15, 281–282. [Google Scholar] [CrossRef]
- Kim, H.T.; Conjares, J.N.V.; Suh, J.T.; Yoo, I.C. Chronic head dislo- cation in Children, part 1: Pathologic changes preventing stable reduction and surgical correction. J. Pediatr. Orthop. 2002, 22, 583–590. [Google Scholar] [CrossRef]
- Kontakis, G.M.; Pasku, D.; Pagkalos, J.; Katonus, P.G. The natural history of a mistreated ipsilateral Galeazzi and Monteggia lesion: Report of a case 39 years post-injury. Acta Orthop. Belg. 2008, 74, 546–549. [Google Scholar]
- Ring, D. Monteggia fractures. Orthop. Clin. N. Am. 2013, 44, 59–66. [Google Scholar] [CrossRef]
- Beutel, B.G. Monteggia fractures in pediatric and adult populations. Orthopedics 2012, 35, 138–144. [Google Scholar] [CrossRef]
- David-West, K.S.; Wilson, N.I.; Sherlock, D.A.; Bennet, G.C. Missed Monteggia injuries. Injury 2005, 36, 1206–1209. [Google Scholar] [CrossRef]
- Flipsen, M.; Ham, J.; van der Zwan, A.; Mader, K. Radial head resection and hemi- interposition arthroplasty in patients with multiple hereditary exostoses: Description of a new surgical technique. J. Pediatr. Orthop. 2018, 27, 289–295. [Google Scholar] [CrossRef] [PubMed]
- Chen, W.S. Late neuropathy in chronic dislocation of the radial head. Report of two cases. Acta Orthop. Scand. 1992, 63, 343–344. [Google Scholar] [CrossRef] [PubMed]
- Støren, G. Traumatic dislocation of the radial head as an isolated lesion in children. Acta Orthop. Scand. 1958, 116, 144–147. [Google Scholar]
- Kunkel, S.; Cornwall, R.; Little, K.; Jain, V.; Mehlman, C.; Tamai, J. Limitations of the Radiocapitellar Line for Assessment of Pediatric Elbow Radiographs. J. Pediatr. Orthop. 2021, 31, 628–632. [Google Scholar] [CrossRef]
- Lincoln, T.L.; Mubarak, S.J. ‘Isolated’ traumatic radial-head dislocation. J. Pediatr. Orthop. 1994, 14, 454–457. [Google Scholar] [CrossRef]
- Hirayama, T.; Takemitsu, Y.; Yagihara, K.; Mikita, A. Operation for chronic dislocation of the radial head in children. Reduction by osteotomy of the ulna. J. Bone Jt. Surg. Br. 1987, 69, 639–642. [Google Scholar] [CrossRef]
- Kim, H.T.; Park, B.G.; Suh, J.T.; Yoo, I.C. Chronic radial head dislocation in children, part 2: Results of open treatment and factors affecting final outcome. J. Pediatr. Orthop. 2002, 22, 591–597. [Google Scholar] [CrossRef]
- Freedman, L.; Luk, K.; Leong, J.C. Radial head reduction after a missed Monteggia fracture: Brief report. J. Bone Jt. Surg. Br. 1988, 70, 846–847. [Google Scholar] [CrossRef]
- Horii, E.; Nakamura, R.; Koh, S.; Inagaki, H.; Yajima, H.; Nakao, E. Surgical treatment for chronic radial head dislocation. J. Bone Jt. Surg. Am. 2002, 84-A, 1183–1188. [Google Scholar] [CrossRef]
- Wang, M.N.; Chang, W.N. Chronic posttraumatic anterior dislocation of the radial head in children: Thirteen cases treated by open reduction, ulna osteotomy, and annular ligament reconstruction throught a Boyd incision. J. Orthop. Trauma. 2006, 20, 1–5. [Google Scholar] [CrossRef]
- Nakamura, K.; Hirachi, K.; Uchiyama, S.; Takahara, M.; Minami, A.; Imaeda, T.; Kato, H. Long-Term clinical and radiographic outcomes after open reduction for missed monteggia fracture-dislocations in children. J. Bone Jt. Surg. Am. 2009, 91, 1394–1404. [Google Scholar] [CrossRef]
- Rahbek, O.; Deutch, S.R.; Kold, S.; Søjbjerg, J.O.; Møller-Madsen, B. Long-term outcome after ulnar osteotomy for missed Monteggia fracture dislocation in children. J. Child. Orthop. 2011, 5, 449–457. [Google Scholar] [CrossRef]
- Yildirim, A.; Nas, K. Rehabilitation of neglected Monteggia fracture: Dislocations in children. J. Back Musculoskelet. Rehabil. 2017, 30, 1251–1257. [Google Scholar] [CrossRef]
- Cao, S.; Dong, Z.-G.; Liu, L.-H.; Wie, J.-W.; Luo, Z.-B.; Peng, P. Missed Monteggia fractures in children treated by open reduction of the radial head and corrective osteotomy of the ulna. Sci. Rep. 2022, 12, 16819. [Google Scholar] [CrossRef] [PubMed]
- Delpont, M.; Jouve, J.L.; Sales de Guazy, J.; Louahem, D.; Vialle, R.; Bollini, G.; Accadbled, F.; Cottalorda, J. Proximal ulnar osteotomy in the treatment of neglected childhood Monteggia lesion. Orthop. Traumatol. Surg. Res. 2014, 100, 803–807. [Google Scholar] [CrossRef]
- Hui, J.H.P.; Sulaiman, A.R.; Lee, H.-C.; Lam, K.-S.; Lee, E.-H. Open Reduction and Annular Ligament Reconstruction With Fascia of the Forearm in Chronic Monteggia Lesions in Children. J. Pediatr. Orthop. 2005, 25, 501–506. [Google Scholar] [CrossRef]
- Koslowsky, T.C.; Mader, K.; Wulke, A.P.; Gausepohl, T. Operative treatment of chronic Monteggia lesion in younger children: A report of three cases. J. Shoulder Elb. Surg. 2006, 15, 119–121. [Google Scholar] [CrossRef] [PubMed]
- Take, M.; Tomori, Y.; Sawaizumi, T.; Majima, T.; Nanno, M.; Takai, S. Ulnar osteotomy and the ilizarov mini-fixator for pediatric chronic monteggia fracture-dislocations. Medicine 2019, 98, e13978. [Google Scholar] [CrossRef]
- Bhaskar, A. Missed Monteggia fracture in children: Is annular ligament reconstruction always required? Indian J. Orthop. 2009, 43, 389. [Google Scholar] [CrossRef] [PubMed]
- Lädermann, A.; Ceroni, D.; Lefévre, Y.; De Rosa, V.; De Coulon, G.; Kaelin, A. Surgical treatment of missed Monteggia lesions in children. J. Child Orthop. 2007, 1, 237–242. [Google Scholar] [CrossRef]
- Bae, D.S. Successful strategies for managing Monteggia injuries. J. Pediatr. Orthop. 2016, 36 (Suppl. 1), S67–S70. [Google Scholar] [CrossRef] [PubMed]
- Hasler, C.C.; von Laer, L.; Hell, A.K. Open reduction, ulnar osteotomy and external fixation for chronic anteriordislocation of the head of the radius. J. Bone Jt. Surg. Br. 2005, 87, 88–94. [Google Scholar] [CrossRef]
- Peshin, C.; Ratra, R.; Juyal, A.K. Step-cut osteotomy in neglected Monteggia fracture dislocation in pediatric and adolescent patients: A retrospective study. J. Orthop. Surg. 2020, 28, 230949902096408. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Du, M.; Pei, X.; Luo, J.; Li, Y.; Liu, Y.; Wang, X.; Coa, J.; Han, J. External Fixator-assisted Ulnar Osteotomy: A Novel Technique to Treat Missed Monteggia Fracture in Children. Orthop. Surg. 2019, 11, 102–108. [Google Scholar] [CrossRef] [PubMed]
- Chen, H.-Y.; Wu, K.-W.; Dong, Z.-R.; Huang, S.-C.; Kuo, K.N.; Wang, T.-M. The treatment of chronic radial head dislocation in Monteggia fracture without annular ligament reconstruction. Int. Orthop. 2018, 42, 2165–2172. [Google Scholar] [CrossRef] [PubMed]
- Miyake, J.; Oka, K.; Moritomo, H.; Sugamoto, K.; Yoshikawa, H.; Murase, T. Open Reduction and 3-Dimensional Ulnar Osteotomy for Chronic Radial Head Dislocation Using a Computer-Generated Template: Case Report. J. Hand Surg. 2012, 37, 517–522. [Google Scholar] [CrossRef]
- Oka, K.; Murase, T.; Moritomo, H.; Yoshikawa, H. Corrective osteotomy for malunited both bones fractures of the forearm with radial head dislocations using a custom-made surgical guide: Two case reports. J. Shoulder Elb. Surg. 2012, 21, e1–e8. [Google Scholar] [CrossRef]
- Lu, X.; Wang, Y.K.; Zhang, J.; Zhu, Z.; Guo, Y.; Lu, M. Management of Missed Monteggia Fractures With Ulnar Osteotomy, Open Reduction, and Dual-socket External Fixation. J. Pediatr. Orthop. 2013, 33, 398–402. [Google Scholar] [CrossRef]
- Ahmed, A.A.R.Y. Gradual ulnar lengthening by an Ilizarov ring fixator for correction of Masada IIb forearm deformity without tumor excision in hereditary multiple exostosis. J. Pediatr. Orthop. B 2019, 28, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Liu, Y.; Zhao, H.; Xu, H.; Shi, W.; Li, J.; Li, Y.; Cavanese, F. To Angulate or Not to Angulate the Ulna during the Progressive Distraction Period Performed with a Monolateral External Fixator in Paediatric Patients with a Chronic Monteggia Fracture? Medicina 2022, 58, 1666. [Google Scholar] [CrossRef] [PubMed]
- Zhang, R.; Xue, F.; Liu, S.; Ruan, H.; Xu, J.; Kang, Q. Novel use of close-wedge osteotomy and monorail external fixator in the treatment of chronic Monteggia fracture. Jt. Dis. Relat. Surg. 2022, 33, 285–293. [Google Scholar] [CrossRef]
- Loose, O.; Morrsion, G.; Langendoerfer, M.; Eberhardt, T.; Wirth, F.; Fernandez, F. Radial head distalisation with an external ring fixator as a therapy option in children with chronic posttraumatic radiocapitellar disloction. Eur. J. Trauma Emerg. Surg. 2023, 49, 1803–1810. [Google Scholar] [CrossRef]
- Garg, P.; Baid, P.; Sinha, S.; Ranjan, R.; Bandyopadhyay, U.; Mitra, S.R. Outcome of radial head preserving operations in missed Monteggia fracture in children. Indian J. Orthop. 2011, 45, 404–409. [Google Scholar] [CrossRef] [PubMed]
- Park, H.; Park, K.-W.; Park, K.B.; Kim, H.W.; Eom, N.K.; Lee, D.H. Impact of open reduction on surgical strategies for missed Monteggia fracture in children. Yonsei Med. J. 2017, 58, 829–836. [Google Scholar] [CrossRef] [PubMed]
- Cevik, H.B.; Yuvaci, F.; Bulut, G. Four different management strategies in missed Monteggia lesions in children. J. Orthop. 2020, 21, 207–212. [Google Scholar] [CrossRef] [PubMed]
- De Boeck, H. Radial neck osteolysis after annular ligament reconstruction. A case report. Clin. Orthop. Relat. Res. 1997, 342, 94–98. [Google Scholar] [CrossRef]
- Rodgers, W.B.; Waters, P.M.; Hall, J.E. Chronic monteg-gia lesions in children. J. Bone Jt. Surg. Am. 1996, 78, 1322–1329. [Google Scholar] [CrossRef] [PubMed]
- Bor, N.; Rubin, G.; Rozen, N.; Herzenberg, J.E. Chronic Anterior Monteggia Lesions in Children. J. Pediatr. Orthop. 2015, 35, 7–10. [Google Scholar] [CrossRef]
- Slongo, T.F. Korrekturosteotomie der fehlverheilten Monteggia-Verletzung mit einem Fixateur externe. Oper. Orthopädie Traumatol. 2018, 20, 435–449. [Google Scholar] [CrossRef]
- Stoll, T.M.; Willis, R.B.; Paterson, D.C. Treatment of the missed Monteggia fracture in the child. J. Bone Jt. Surg. Br. 1992, 74, 436–440. [Google Scholar] [CrossRef]
- Hresko, M.T.; Rosenberg, B.N.; Pappas, A.M. Excision of the radial head in patients younger than 18 years. J. Pediatr. Orthop. 1999, 19, 106–113. [Google Scholar] [CrossRef]
- Wegmann, H.; Heider, S.; Novak, M.; Sperl, M.; Kraus, T.; Singer, G.; Till, H. Outcome follow- ing excision of the radial head in children with open physes for impaired elbow motion. J. Shoulder Elb. Surg. 2019, 28, 525–529. [Google Scholar] [CrossRef]
- Bengard, M.J.; Calfee, R.P.; Steffen, J.A.; Goldfarb, C.A. Intermediate-term to long-term outcome of surgically and nonsurgically treated congenital, isolated radial head dislocation. J. Hand Surg. Am. 2012, 37, 2495–2501. [Google Scholar] [CrossRef]
- Factor, S.; Rotman, D.; Pritsch, T.; Allon, R.; Tordjman, D.; Atlan, F.; Rosenblatt, Y. Radial head excision and Achilles allograft interposition arthroplasty for the treatment of chronic pediatric radiocapitellar pathologies: A report of four cases. Shoulder Elb. 2021, 13, 213–222. [Google Scholar] [CrossRef]
- Kruppa, C.; Brinkemper, A.; Cibura, A.; Königshausen, M.; Reinke, C.; Schildhauer, T.A.; Dudda, M. A salvage procedure: Radial head excision in children and adolescents—Short-to-midterm outcomes and overview of the literature. J. Child. Orthop. 2023, 17, 239–248. [Google Scholar] [CrossRef]
- Johnson, J.A.; Beingessner, D.M.; Gordon, K.D.; Dunning, C.E.; Stacpoole, R.A.; King, G.J.W. Kinematics and stability of the fractured and implant- reconstructed radial head. J. Shoulder Elb. Surg. 2005, 14, 195S–201S. [Google Scholar] [CrossRef]
- Hall, J.A.; McKee, M.D. Posterolateral rotatory instability of the elbow following radial head resection. J. Bone Jt. Surg. Am. 2005, 87, 1571–1579. [Google Scholar]
- Ikeda, M.; Sugiyama, K.; Kang, C.; Takagagi, T.; Oka, Y. Comminuted fractures of the radial head. Comparison of resection and internal fixation. J. Bone Jt. Surg. Am. 2005, 87, 76–84. [Google Scholar] [CrossRef] [PubMed]
- Ramazanian, T.; Muller-Lebschi, J.A.; Chuang, M.Y.; Vaichinger, A.M.; Fitzsimmons, J.S.; O’Driscoll, S.W. Effect of radiocapitellar Achilles disc arthroplasty on coronoid and capitellar contact pressures after radial head excision. J. Shoulder Elb. Surg. 2018, 27, 1785–1791. [Google Scholar] [CrossRef] [PubMed]
- Hergenroeder, P.T.; Gelberman, R.H. Distal radioulnar joint subluxation secondary to excision of the radial head. Orthopedics 1980, 3, 649–650. [Google Scholar] [CrossRef] [PubMed]
- Mikic, Z.D.; Vukadinovic, S.M. Late results in fractures of the radial head treated by excision. Clin. Orthop. Relat. Res. 1983, 181, 220–228. [Google Scholar] [CrossRef]
- Farr, S.; Abualruz, M.M.; Girsch, W. Radial Head Resection and Corium Interposition Arthroplasty in Skeletally Immature Patients with Isolated Posttraumatic Radial Head Arthrosis. Tech. Hand Up. Extrem. Surg. 2020, 24, 37–42. [Google Scholar] [CrossRef] [PubMed]
- Campbell, C.C.; Waters, P.M.; Emans, J.B. Excision of the radial head for congenital dislocation. J. Bone Jt. Surg. Am. 1992, 74, 726–733. [Google Scholar] [CrossRef]





| Functional Radial Head Resection | Radial Head Resection | |
|---|---|---|
| Delayed or Nonunion | 1/16 [43], 2/15 [33] | - |
| Pin Infection | 2/15 [33] | - |
| Re-dislocation | 0 [33,43,49] | - |
| Ulnar positive variance | 2/16 [43] | 3/5 [51], 12/27 [52], 1/7 [53], 4/16 [54], 3/4 [55], |
| Re-operation | 1/16 [43], 2/15 [33] | 2/5 [51], 4/16 [54], 1/4 [55], 7/27 [52], 7/27 [52] |
| Cubitus valgus | - | 1/5 [51], 3/7 [53],1/2 [56] |
| Instability | - | 1/2 [56] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Wintges, K.; Cramer, C.; Mader, K. Missed Monteggia Injuries in Children and Adolescents: A Treatment Algorithm. Children 2024, 11, 391. https://doi.org/10.3390/children11040391
Wintges K, Cramer C, Mader K. Missed Monteggia Injuries in Children and Adolescents: A Treatment Algorithm. Children. 2024; 11(4):391. https://doi.org/10.3390/children11040391
Chicago/Turabian StyleWintges, Kristofer, Christopher Cramer, and Konrad Mader. 2024. "Missed Monteggia Injuries in Children and Adolescents: A Treatment Algorithm" Children 11, no. 4: 391. https://doi.org/10.3390/children11040391
APA StyleWintges, K., Cramer, C., & Mader, K. (2024). Missed Monteggia Injuries in Children and Adolescents: A Treatment Algorithm. Children, 11(4), 391. https://doi.org/10.3390/children11040391






