1. Introduction
The ASD literature consistently highlights that when guardians actively participate in the oral care routine of their child, it can foster a positive experience and effectively mitigate certain obstacles to care [
1]. Little is known about what caregivers for children with intellectual disabilities would consider “successful assistance” (e.g., specific support tools and monitoring needed) for achieving better oral health. Research has identified a number of factors that contribute to poor oral health in children with ASD, including difficulty tolerating home and professional oral care, sensory processing differences, uncooperative behaviors, communication impairments, and challenges finding and accessing professional oral care services [
2]. Caregivers are typically trained to provide oral hygiene to the child by performing it at the same time of day, in the same room, with the same toothbrush/toothpaste. They are typically shown a hand-over-hand technique, with the child holding the brush themselves and the caregiver’s hand over the child’s. Caregivers are instructed to brush after the child to ensure all areas are effectively cleaned. Unfortunately, many children with ASD have been aggressively opposed to routine brushing [
2]. With advancements in children’s accessibility to smartphones and similar devices, the popularity and preference for smart toothbrushes have increased. A prior study highlighted that smart toothbrushes enhance motivation by stimulating interest in oral hygiene, thus refining brushing techniques [
3]. Similarly, another study utilized mobile applications linked to a “smart brush” to enhance oral hygiene practices and habits. This study involved 68 children (aged 6–12 years) divided randomly into three groups. Group I received an electric toothbrush, group II received a smart toothbrush (ST), and group III used a manual toothbrush. The ST group recorded “scores” while brushing different areas of the oral cavity. Exclusively for the ST group, dentists provided feedback via the application on a weekly basis, based on brushing time, condition, and score of the teeth obtained through the application. The authors concluded that the utilization of smart toothbrushes effectively delivered dental health education and demonstrated a reduction in plaque for children aged 6–12 years [
4].
ASD was first described in 1943 by Leo Kanner and consists of the following subtypes: (a) autism disorder, (b) Asperger’s syndrome, (c) Rett’s syndrome, (d) childhood disintegrative disorder, and (e) pervasive developmental disorder not otherwise specified [
5]. Few studies have documented the oral health status of children with ASD [
6,
7,
8,
9], and studies where toothbrushing has been tested with this population have shown that using visual aids such as visual pedagogy, picture exchange communication systems, and video modeling systems can improve the oral hygiene of children with ASD [
10,
11,
12,
13,
14]. However, little is known about whether these aids can serve as “successful assistance” for children with ASD in pursuit of better oral health as judged by their caregivers.
Smart connected technologies offer significant promise for improving the oral healthcare experience by monitoring compliance, demonstrating errors, and recording outcomes, all while gamifying the oral hygiene experience. The Colgate Kids Smart Electric Toothbrush (Smart E-Toothbrush) is a smart toothbrush that utilizes an augmented reality experience to engage children during toothbrushing through the use of games. The Smart E-Toothbrush provides guidance on brushing technique, and brushing rewards are given for successful oral hygiene performance on a cell phone/tablet application (app). In short, upon registration, the virtual reality game allows users to travel through a set of imaginary worlds to collect cartoon masks. There are five masks per world. The areas inside the mouth are divided into 16 zones, and users are guided to brush all 16 zones of their teeth. If the child brushes the correct zone and defeats the monster, he/she will gain diamonds. Users can earn up to 15 diamonds per zone. With perfect technique as brushing improves, users can collect up to 240 diamonds in one brushing session. As they improve their scores, they can purchase additional masks to try on in the photo booth window of the app and continue the game. At the end of the brushing session, users will see the stars they have won. The number of stars is decided by the number of diamonds. The more diamonds users collect, the more stars they will receive.
Studies have shown that children with autism often have specific sensory sensitivities, communication difficulties, and behavioral challenges that can impact their oral hygiene practices, dental visits, and overall oral health status [
6,
8,
15]. This study used a “consumer approach” aimed to capture caregiver experiences, such as how easy and enjoyable the use of the toothbrush and app seemed to be for their child with ASD, as well as how useful the caregiver found the connected toothbrush. These insights will help determine the value of utilizing smart toothbrush technologies and augmented reality experiences by caregivers for the engagement of children with ASD in oral hygiene.
Consumer research contributes to improving oral healthcare delivery, product development, and consumer engagement strategies. These studies can also be designed to assess factors influencing the choice of oral hygiene products in different populations [
16]. Patient-centered care encompasses dimensions beyond clinical effectiveness and patient safety; it also prioritizes the preferences of patients as “consumers” of healthcare products and services. Therefore, incorporating “behavioral guidance” research in oral health among children with autism is essential for understanding their unique needs, preferences, and challenges related to oral hygiene and dental care. This helps identify barriers that may prevent optimal oral health outcomes in this population and informs the development of tailored interventions and strategies to improve oral health behaviors and outcomes [
17].
2. Materials and Methods
2.1. Ethical Considerations
This study was conducted from August 2022 to November 2022 in accordance with the ethical principles of the Declaration of Helsinki and consistent with Good Clinical Practice Guidelines. Participants’ visits occurred at the University of Pennsylvania School of Dental Medicine, Center for Clinical and Translational Research. The study was registered in
ClinicalTrials.gov with the number NCT05552144. IRB approval was obtained through the University of Pennsylvania prior to the start of the study (approval # 850364). Study participants and caregivers were informed about the purpose, procedures, and duration. They had the opportunity to discuss the study, and caregivers signed an informed consent form, while verbal assent was obtained from child participants.
2.2. Eligibility Criteria
Study participants were children aged 5–12 years old and their responsible primary caregivers. To be included in the study, the child subjects needed to be in good general and oral health. Eligibility was determined by a review of dental and medical history and oral examination at baseline, availability for the duration of the study, and diagnosis of ASD level 1 (requiring support) or ASD level 2 (requiring substantial support). Upon oral examination, if the child presented with obvious signs of oral disease, severe dental caries, or pain as determined by the investigator, they were excluded. The oral examination focused initially on caries as part of standard care by thoroughly assessing the teeth for decay using visual inspection. Concurrently, the gums were also evaluated for visible signs of inflammation and/or bleeding upon inspection. Additionally, a comprehensive examination of oral tissues was conducted to detect any abnormalities or lesions, thus ensuring no signs of infection and/or inflammation were present in the child’s oral cavity. Children with ASD were recruited from “Kamp For Kids”, a 501c3 non-profit organization that funds and runs camps, events, and programs for children with ASD in Philadelphia, PA. Diagnosis of ASD was confirmed by reported data from the caregiver/legal representative and/or confirmed with medical records whenever available. Caregivers needed to be able to observe the child using the Smart E-Toothbrush, be available for the duration of the study, have access to either an Apple iPhone or iPad, or an Android device with access to an internet connection, be willing to download and use the app associated with the connected toothbrush, be proficient in English, and be willing to share their own and the child’s brushing experiences.
Exclusion criteria included children undergoing active orthodontic treatment with fixed appliances, with obvious signs of oral disease, participating in another clinical study, currently using the Smart E-Toothbrush, or deemed as unsuitable for participation due to their behavior, at the investigators’ discretion.
2.3. Type of Study and Design
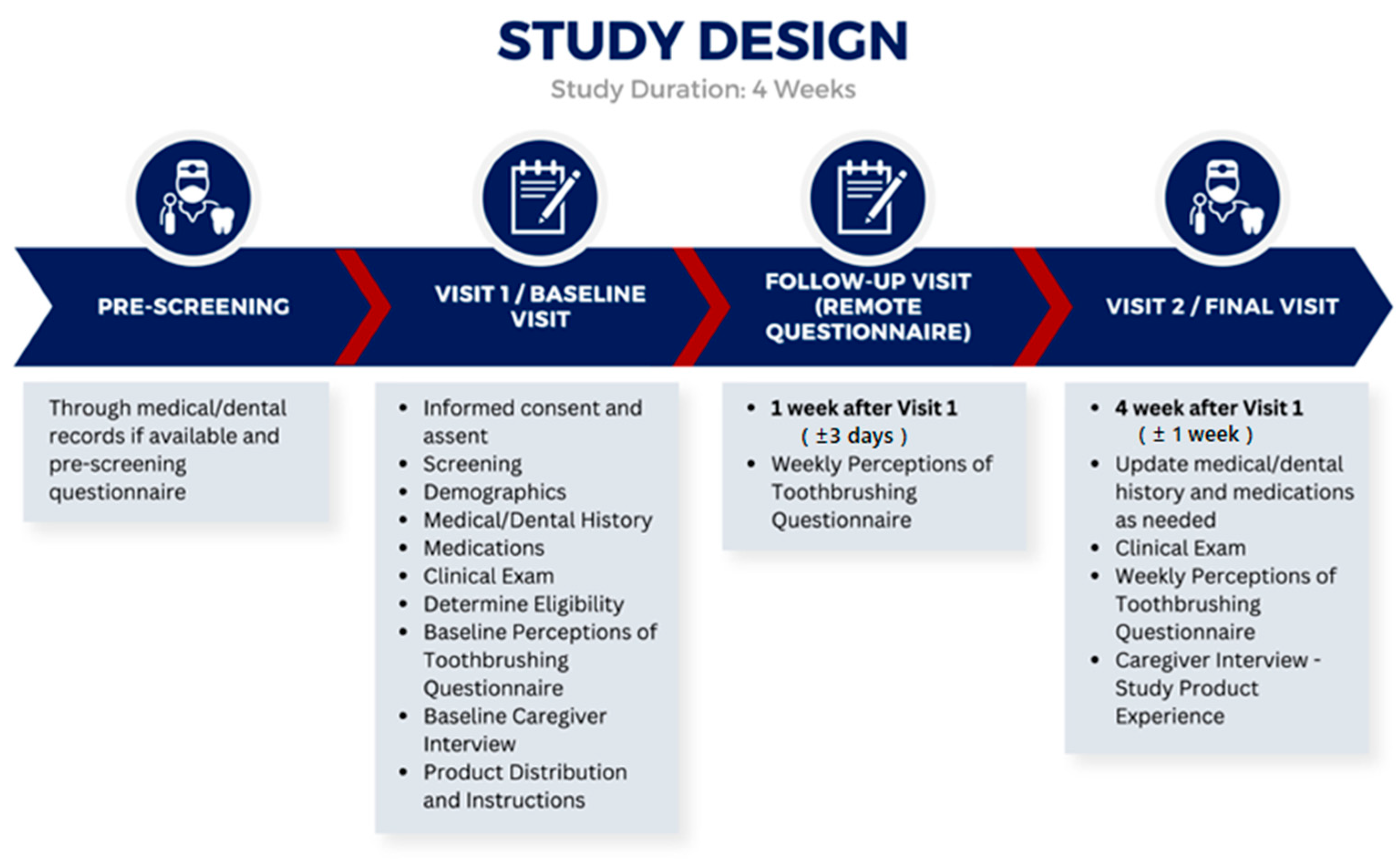
This was a single-center, pretest–posttest, non-randomized clinical study involving interviews with caregivers prior to utilization of the toothbrush and after 4 weeks of product use by the child; questionnaires were administered to caregivers at three timepoints throughout the study, and daily text message questions were sent to caregivers (
Figure 1).
To ensure that subjects were comfortable with the oral care regime proposed, toothbrushes were distributed based on the subject’s preference (Smart E-Toothbrush or manual toothbrush). All children opted to receive the Smart E-Toothbrush at the beginning of the study. All enrolled subjects were instructed to brush their teeth twice daily (morning and evening) for two minutes each time with the toothbrush provided. They were instructed to continue using the toothpaste they were using prior to enrollment or a regular toothpaste available for the study if they preferred. Introducing a new toothpaste flavor to the children was avoided as it could introduce bias to the brushing experience if, for example, the child did not like the taste of the new toothpaste. As part of the research protocol, at baseline, caregivers were asked to download the Smart E-Toothbrush app and create an account. They were then instructed to help their children follow the instructions on the app and brush their teeth while they played the Smart E-Toothbrush kids’ game.
The duration of the study was 4 weeks for all subjects. All subjects were evaluated at baseline and final visits (after 4 weeks, ±1 week, of using the toothbrush). Questionnaires were conducted at baseline, 1 week (±3 days), and 4 weeks (±1 week), and interviews were conducted at baseline and after 4 weeks (±1 week) of use of the connected toothbrush and app. At baseline, week 1, and week 4, caregivers were asked to complete a questionnaire regarding the child’s brushing habits and experience with a unique link via REDCap or complete a phone/video call with the study team. REDCap is a secure, web-based, electronic data capture system hosted at the University of Pennsylvania. Interviews with the caregiver were performed to understand the range of patient experiences, such as thoughts, feelings, intentions, observations, and behaviors at baseline and related to the use of a connected toothbrush and related smartphone app after the 4 weeks of use. Data were collected through purposive sampling with in-depth semi-structured interviews. The interviews lasted between 30 and 60 min and were audio recorded. Recordings were de-identified and used for the qualitative analyses.
Text messages containing five questions were sent twice a day (AM and PM) via TWILIO, an automated short message service (SMS) platform, for caregivers to report on the toothbrushing experiences for each day. Questions were sent to gather feedback regarding difficulty with brushing using the device, caregiver satisfaction with the brushing experience, or frustration with the experience. Questions utilized a scale (0–10), where “0” would represent, for example, “not difficult at all”, “not satisfied at all”, “not frustrated at all”, or “not helpful at all”.
Caregivers were also asked about the frequency of their child’s brushing and could choose from three options: 0 = 0–1 Minutes; 1 = 1–2 min; 2 = More than 2 min. Child subjects were instructed to refrain from routine dental treatment during the course of the study.
2.4. Statistical Methods
This pilot study was conducted to examine caregivers’ and users’ experiences with a Kids Smart E-Toothbrush used by children with ASD. A priori sample size calculations for the quantitative outcomes were conducted in G*power version 3.1. With a type I error rate of 5% and 80% power, the minimum sample size needed to detect an effect size of 0.57 (2-point change on a 0–10 scale and a standard deviation for the change of 3 points) is N= 17 for a Wilcoxon signed-rank test for matched pairs. A systematic review of empirical tests for calculating sample size in qualitative research found that saturation was reached with 9–17 interviews [
18]. Based on these two sources, we enrolled seventeen children with ASD, between 5 and 12 years old, and their caregivers into the study, all of whom completed the study.
Quantitative data from the questionnaire and TWILIO: Baseline characteristics for caregivers and children (demographics, medical and dental history, and clinical findings) and adverse events were summarized with descriptive statistics. Continuous variables were summarized with means/standard deviations or medians/interquartile ranges, while categorical variables were summarized with frequencies and corresponding percentages. Two-sided non-parametric paired tests were utilized to assess changes in median scores from the answers to the perceptions of toothbrushing questionnaires between baseline and week 4. The Wilcoxon signed-rank test was implemented when the sample distributions were not heavy-tailed and when no outliers were apparent. Otherwise, the sign test was implemented. Bonferroni adjusted critical
p-values were computed to account for multiple tests. Mean scores were calculated for the TWILIO texting data for the AM and PM questions separately, and these were plotted on line graphs (
Figure A1). Data were analyzed and visualized using SAS software, Version 9.4. Copyright © 2020 SAS Institute Inc., Microsoft Corporation, Microsoft Excel 365, Version 2301, and R Statistical Software (v4.2.1; R Core Team 2022).
Qualitative data from interviews: Baseline and week 4 interviews with caregivers were transcribed. Theoretical thematic analysis was conducted at a semantic level by first carrying out per-question, line-by-line coding [
19,
20]. Next, candidate themes and sub-themes were developed from these codes, and in an iterative process, codes, themes, and sub-themes were re-defined when necessary. From the final themes and sub-themes, we created two thematic maps, one for baseline interviews and one for follow-up interviews. (
Figure 2 and
Figure 3). The interviews were conducted by a trained research coordinator at a private location within the clinical research center at Penn Dental Medicine. This individual was not involved with the care of any of the research subjects prior to or during the study.
4. Discussion
Children with special oral healthcare needs are at a greater risk for experiencing oral health disparities than the general pediatric population [
21,
22,
23]. The result of a meta-analysis suggests that children with autism spectrum disorder tend to have poorer oral hygiene, a higher risk of caries, and a lower salivary pH compared to healthy children [
24]. Dental practitioners are likely to encounter children with ASD in their practices. A recent surveillance study conducted by the Autism and Developmental Disabilities Monitoring Network (ADDM) across 11 sites in the US showed that the overall ASD prevalence per 1000 children aged 8 years was 27.6%, with one in 36 children having ASD [
25]. These findings highlight the importance of dental care and oral health management in children with ASD to address the specific factors contributing to the increased risk of caries (tooth decay) and periodontal problems in children with ASD. Some of these factors were also observed in our study, and they include irregular brushing habits due to difficulties faced by trainers and parents while brushing the children’s teeth. Additionally, the side effects of medications used to manage autism symptoms, such as psychoactive drugs or anticonvulsants, may lead to generalized gingivitis in some cases, making this population highly susceptible to the development of oral diseases, including dental caries. A recent clinical trial explored the use of PT (parent training) interventions to improve dental care for children with ASD. The results of the randomized controlled trial had similar findings when compared with our study and showed that the PT intervention was effective in increasing the frequency of daily home oral hygiene and improving oral health [
26]. The study also examined the feasibility, acceptability, and engagement of the PT intervention and showed similar caregiver experience, reporting that the intervention was well-received, with high retention, adherence, utilization, and satisfaction among participating families.
There are a number of behavioral and comfort factors to overcome that contribute to poor oral health in children with ASD, including sensory processing differences, uncooperative behaviors, communication impairments, and difficulties tolerating home and professional care. One study reported that as few as 50% of children with ASD brushed their teeth the recommended twice per day, and 61% of parents of children with ASD reported that toothbrushing is difficult [
15]. The American Academy of Pediatric Dentistry (AAPD) recommends a number of basic behavior guidance techniques to help, including tell–show–do, voice control, nonverbal communication, and positive reinforcement. The design of a manual and battery-operated toothbrush working with an interactive app could make it easier to follow the home care guidelines recommended by AAPD [
27].
Strengths of our study, limitations, and future directions
The intent of our pilot study was to further understand the perceptions of children with ASD and their caregivers when adopting the Smart E-Toothbrush and to optimize the software.
A limitation of our methodology was the universal selection of the electronic toothbrush by all children, regardless of the choice of a manual toothbrush with gamification as an alternative. Furthermore, the small sample size contributes to the limitations of our study. Additionally, we chose not to employ randomization, a common feature of traditional case–control clinical trial designs. Consequently, our study lacked control groups. In our approach, we aimed to collect feedback from children with ASD and caregivers’ perceptions of the introduction of a novel smart toothbrush. These studies are equally important in the context of ASD as these individuals need supportive oral care from families and caregivers; thus, understanding how oral care devices can be adapted and customized to the needs of this population is important and necessary prior to the designing of large trials. We have adopted the consumer feedback approach and, working in partnership with experts, we aimed to further understand usability issues and optimization of the device and technology.
Consumer research in the realm of oral health interventions for children with ASD is aimed at gathering insights from caregivers, healthcare providers, and individuals with ASD. This approach was also noted by Floríndez et al., who advocated for collaborative efforts between families and healthcare professionals to devise impactful strategies for oral healthcare [
28]. This collaborative approach aims to mitigate the challenges associated with poor oral health among disadvantaged populations, ultimately striving to address oral health disparities among individuals with ASD [
29]. The objective is to design interventions that effectively enhance access to dental care and improve the overall oral health experience for this population and their families. In the context of our study, the successful use of any device for oral care hinges on the ability to overcome challenges, such as difficulty in getting the toothbrush into the patient’s mouth. Therefore, it is imperative to first understand patient and caregiver attitudes towards the use of a toothbrush before assessing outcomes related to plaque removal or reduction in periodontal inflammation. The primary aim of this study was to develop strategies that enable the toothbrushing process for children with ASD. To accomplish our goals, most of the data analyzed were qualitative in nature, collecting caregiver-reported outcomes like quality of toothbrushing. The lack of similar oral health trials for children and adolescents with ASD on smart e-toothbrushes limited our discussion; however, most studies emphasize the importance of flexibility from parents and caregivers in supporting oral care, including utilizing in-home services for educational sessions. This highlights the necessity to address practical and logistical barriers through innovative care models, such as leveraging telehealth and oral care devices and tools for this specific population [
26].
Our study suggested that children with ASD level 1 or 2 may benefit from more individualized parent training programs and interventions. Overall, our study aligns with published research that highlights the potential for these interventions to address a critical unmet healthcare need in this population. Further, community-based replication and expansion are needed to validate the findings and promote broader implementation of family education programs.
5. Conclusions
This study demonstrated that caregivers reported that their children with ASD had improved motivation, focus, and enjoyment while brushing utilizing the Smart Electric Toothbrush with augmented reality. According to caregivers, the children became more independent while toothbrushing and achieved better quality brushing. Caregivers’ frustration, satisfaction, and need to help the child with brushing improved over the study duration. Overall, caregivers and children participating in the study liked the features of the application and the gamification features, using the game elements to promote user engagement with the app.
Dental practitioners are likely to encounter children with ASD in their practices. A recent surveillance study conducted by the Autism and Developmental Disabilities Monitoring Network (ADDM) across 11 sites in the US showed that the overall ASD prevalence per 1000 children aged 8 years was 27.6%, with one in 36 children having ASD [
25]. Interaction with caregivers and children regarding brushing and interdental cleaning is crucial to improve oral health and prevent oral disease in this population. Simple interventions like toothbrushing are critical for improving and/or maintaining oral health in the ASD population. Additionally, smart devices, such as the one we tested, can be implemented to improve motivation and compliance with oral care. Furthermore, subjects who become more comfortable with home oral healthcare may be more amenable to dental examination.