Red Code Management in a Pediatric Emergency Department: A Retrospective Study
Abstract
:1. Introduction
1.1. Background
1.1.1. Triage
1.1.2. RCs Management
2. Materials and Methods
2.1. Hospital and Emergency Department Organization
2.2. Data Collection
2.3. Red Code Definition
2.4. Pathologic Items Definition
2.5. Statistical Analysis
2.6. Strenghts and Limits
3. Results
3.1. Population Study
3.2. ED Admission Vital Signs
3.3. Vascular Access
3.4. Emergency Tests
3.5. Therapeutic Approach
3.6. Mortality Rate
3.7. Hospital Admission
3.8. Diagnostic Pathways
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Simon Junior, H.; Schvartsman, C.; Sukys, G.d.A.; Farhat, S.C.L. Pediatric emergency triage systems. Rev. Paul. Pediatr. Orgao Soc. Pediatr. Sao Paulo 2022, 41, e2021038. [Google Scholar] [CrossRef] [PubMed]
- Ødegård, S.S.; Tran, T.; Næss-Pleym, L.E.; Risnes, K.; Døllner, H. A validity study of the rapid emergency Triage and treatment system for children. Scand. J. Trauma. Resusc. Emerg. Med. 2021, 29, 18. [Google Scholar] [CrossRef] [PubMed]
- Biban, P.; Spada, S.; Silvagni, D.; Benedetti, M.; Ghizzi, C. Management of red codes in the paediatric emergency room. Ital. J. Pediatr. 2014, 40, A60. [Google Scholar] [CrossRef]
- Galeazzo, B.; Rubin, G.; Moretti, C. Analisi epidemiologica degli accessi per Codice Rosso in Pronto Soccorso Pediatrico. Med. Bambino 2012, XV, 6. [Google Scholar]
- Thiongane, A.; Ndongo, A.A.; Sow, A.; Keita, Y.; Boiro, D.; Dieng, Y.J.; Basse, I.; Seck, N.; Hilaire, L.A.; Faye, P.M.; et al. Epidemiology of Admissions in a Pediatric Emergency Department in Albert Royer Hospital Dakar. Open J. Pediatr. 2022, 12, 188–195. [Google Scholar] [CrossRef]
- Squillaci, D.; Tumminelli, C.; Molina Ruiz, I.; Calligaris, L.; Poropat, F.; Barbi, E.; Amaddeo, A.; Cozzi, G. Terapia farmacologica in urgenza. Med. Bambino 2022, 41, 441–450. [Google Scholar] [CrossRef]
- Urbino, A.F. Pediatria d’Urgenza; BioMedia: Milan, Italy, 2020; Volume 1. [Google Scholar]
- Piccotti, E.; Magnani, M.; Tubino, B.; Sartini, M.; Pietro, P.D. Assessment of the Triage System in a Pediatric Emergency Department. A pilot study on critical codes. Prev. Med. Hyg. 2008, 49, 120–123. [Google Scholar]
- American Heart Association. PALS Supporto Vitale Avanzato Pediatrico, Manuale per Operatori, 2021a ed.; American Heart Association: Dallas, TX, USA, 2021. [Google Scholar]
- Meyburg, J.; Bernhard, M.; Hoffmann, G.F.; Motsch, J. Principles of pediatric emergency care. Dtsch. Arztebl. Int. 2009, 106, 739–747. [Google Scholar] [CrossRef] [PubMed]
- Festekjian, A.; Glavinic, J. Pediatric septic shock: Recognition and management in the emergency department. Pediatr. Emerg. Med. Pract. 2022, 19, 1–24. [Google Scholar]
- Mendelson, J. Emergency Department Management of Pediatric Shock. Emerg. Med. Clin. N. Am. 2018, 36, 427–440. [Google Scholar]
- Mastrangelo, M.; Baglioni, V. Management of Neurological Emergencies in Children: An Updated Overview. Neuropediatrics 2021, 52, 242–251. [Google Scholar] [CrossRef]
- Pandey, M.; Lyttle, M.D.; Cathie, K.; Munro, A.; Waterfield, T.; Roland, D. Point-of-care testing in Paediatric settings in the UK and Ireland: A cross-sectional study. BMC Emerg. Med. 2022, 22, 6. [Google Scholar] [CrossRef]
- Ministero della Salute. Triage Intraospedaliero Aggiornamento Linee Guida 2016. Available online: https://www.salute.gov.it/imgs/C_17_pubblicazioni_3145_allegato.pdf (accessed on 12 April 2023).
- Savoia, P.; Jayanthi, S.K.; Chammas, M.C. Focused Assessment with Sonography for Trauma (FAST). J. Med. Ultrasound. 2023, 31, 101–106. [Google Scholar] [CrossRef] [PubMed]
- Colbachini, P.C.M.; Marson, F.A.L.; Peixoto, A.O.; Sarti, L.; Fraga, A.M.A. Air Rescue for Pediatric Trauma in a Metropolitan Region of Brazil: Profiles, Outcomes, and Overtriage Rates. Front. Pediatr. 2022, 10, 890405. [Google Scholar] [CrossRef]
- Rzońca, E.; Świeżewski, S.P.; Gałązkowski, R.; Bień, A.; Kosowski, A.; Leszczyński, P.; Rzońca, P. Neonatal Transport in the Practice of the Crews of the Polish Medical Air Rescue: A Retrospective Analysis. Int. J. Environ. Res. Public Health 2020, 17, 705. [Google Scholar] [CrossRef]
- Aeimchanbanjong, K.; Pandee, U. Validation of different pediatric triage systems in the emergency department. World J. Emerg. Med. 2017, 8, 223–227. [Google Scholar] [CrossRef]
- Duncan, H.; Hutchison, J.; Parshuram, C.S. The pediatric early warning system score: A severity of illness score to predict urgent medical need in hospitalized children. J. Crit. Care 2006, 21, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Sá, R.A.R.D.; Melo, C.L.; Dantas, R.B.; Delfim, L.V.V. Acesso vascular por via intraóssea em emergências pediátricas. Rev. Bras. Ter. Intensiva 2012, 24, 407–414. [Google Scholar] [CrossRef] [PubMed]
- Nijssen-Jordan, C. Emergency department utilization and success rates for intraosseous infusion in pediatric resuscitations. CJEM 2000, 2, 10–14. [Google Scholar] [CrossRef]
- Kikodze, N.; Tvildiani, D.; Nemsadze, K. Pediatric Emergency Cases Managed with Intraosseous Access: Indications, Complication and Outcomes. Int. J. Sci. 2019, 47, 22–30. [Google Scholar]
- Mittiga, M.R.; Geis, G.L.; Kerrey, B.T.; Rinderknecht, A.S. The Spectrum and Frequency of Critical Procedures Performed in a Pediatric Emergency Department: Implications of a Provider-Level View. Ann. Emerg. Med. 2013, 61, 263–270. [Google Scholar] [CrossRef]
- Gold, D.; Levine, M.; Hsu, D.; Way, D.P.; Shefrin, A.E.; Lam, S.H.F.; Lewiss, R.; Marin, J.R.; the PEM POCUS Curriculum Task Force. Design of a point-of-care ultrasound curriculum for pediatric emergency medicine fellows: A Delphi study. AEM Educ. Train. 2021, 5, e10700. [Google Scholar] [CrossRef] [PubMed]
- MPH JWTM. Randomized Controlled Trial of Inferior Vena Cava Ultrasonography in the Management and Disposition of Pediatric Patients Undergoing Evaluation for Sepsis and Dehydration. 2023; Report No.: NCT02568189. Available online: https://clinicaltrials.gov/study/NCT02568189 (accessed on 1 January 2023).
- Chen, L.; Kim, Y.; Santucci, K.A. Use of ultrasound measurement of the inferior vena cava diameter as an objective tool in the assessment of children with clinical dehydration. Acad. Emerg. Med. Off. J. Soc. Acad. Emerg. Med. 2007, 14, 841–845. [Google Scholar] [CrossRef]
- Özkan, E.A.; Kılıç, M.; Çalışkan, F.; Baydın, A. Evaluation of the Inferior Vena Cava Diameter in Dehydrated Children Using Bedside Ultrasonography. Emerg. Med. Int. 2022, 2022, 6395474. [Google Scholar] [CrossRef]
- Indinnimeo, L.; Chiappini, E.; Miraglia Del Giudice, M. The Italian Panel for the management of acute asthma attack in children Roberto Bernardini. Guideline on management of the acute asthma attack in children by Italian Society of Pediatrics. Ital. J. Pediatr. 2018, 44, 46. [Google Scholar] [CrossRef]
- Global Initiative for Asthma. Global Strategy for Asthma Management and Prevention. May 2023. Available online: www.ginasthma.org (accessed on 12 April 2023).
- Babl, F.E.; Weiner, D.L.; Bhanji, F.; Davies, F.; Berry, K.; Barnett, P. Advanced training in pediatric emergency medicine in the United States, Canada, United Kingdom, and Australia: An international comparison and resources guide. Ann. Emerg. Med. 2005, 45, 269–275. [Google Scholar] [CrossRef] [PubMed]
- Epstein, D.; Brill, J.E. A history of pediatric critical care medicine. Pediatr. Res. 2005, 58, 987–996. [Google Scholar] [CrossRef] [PubMed]
- Gatto, A.; Rivetti, S.; Capossela, L.; Pata, D.; Covino, M.; Chiaretti, A. Utility of a pediatric observation unit for the management of children admitted to the emergency department. Ital. J. Pediatr. 2021, 47, 11. [Google Scholar] [CrossRef]
- Zhu, C.P.; Wu, X.H.; Liang, Y.T.; Ma, W.C.; Ren, L. The mortality of patients in a pediatric emergency department at a tertiary medical center in China: An observational study. World J. Emerg. Med. 2015, 6, 212–216. [Google Scholar] [CrossRef]
- Jofiro, G.; Jemal, K.; Beza, L.; Bacha Heye, T. Prevalence and associated factors of pediatric emergency mortality at Tikur Anbessa specialized tertiary hospital: A 5 year retrospective case review study. BMC Pediatr. 2018, 18, 316. [Google Scholar] [CrossRef]
- Grither, A.; Leonard, K.; Whiteley, J.; Ahmad, F. Development, Implementation, and Provider Perception of Standardized Critical Event Debriefing in a Pediatric Emergency Department. Pediatr. Emerg. Care 2023, 40, 292–296. [Google Scholar] [CrossRef] [PubMed]
| Triage Code | Denomination | Definition | Maximum Waiting Times |
|---|---|---|---|
| 1—red | Emergency | Absence or compromission of one or more vital functions | Immediate evaluation |
| 2—orange | Urgency | Stable condition with an evolutive risk of vital functions compromission or severe pain | Evaluation within 15 min |
| 3—light blue | Deferred urgency | Stable condition without evolutionary risk but with implications for general health, typically requiring complex diagnostic–therapeutic interventions | Evaluation within 60 min |
| 4—green | Minor urgency | Stable condition without evolutionary risk, typically requiring simple monospecialistic diagnostic–therapeutic interventions | Evaluation within 120 min |
| 5—white | No urgency | Not urgent or of minimal clinical relevance | Evaluation within 240 min |
| Item | Criteria for Pathologic Definition |
|---|---|
| Systolic blood pressure | <70 mmHg if age < 1 year |
| OR | |
| <70 + (2 × age in years) if age > 1 year | |
| OR | |
| >the 90th percentile for age, gender, and height | |
| Multiparametric blood gas analysis (MBG) | pH < 7.35 or >7.45 |
| OR | |
| blood glucose < 60 mg/dL or >200 mg/dL | |
| OR | |
| hemoglobin < anemia cutoff according to age | |
| OR | |
| serum sodium < 135 mmol/L or >145 mmol/L | |
| Blood count | white blood cells < 5000/mm3 or >15,000/mm3 |
| OR | |
| platelets < 150,000/mm3 | |
| OR | |
| hemoglobin < anemia cutoff according to age |
| Variable | Total | Medical | Surgical |
|---|---|---|---|
| Sex, n (%) | |||
| Male | 522 (55.9%) | 438 (54.2%) | 84 (66.7%) |
| Female | 412 (44.1%) | 370 (45.8%) | 42 (33.3%) |
| Age, median (percentile25-percentile75) years | 3.2 (1.1–7.4) | 2.7 (0.9–6.8) | 6.6 (2.7–11.3) |
| Access mode to ED, n (%) | |||
| Independently | 414 (44.3%) | 404 (50%) | 10 (7.9%) |
| Ambulance | 276 (29.6%) | 194 (24%) | 82 (65.1%) |
| Transfer from another hospital | 189 (20.2%) | 157 (19.4%) | 32 (25.4%) |
| Not reported | 55 (5.9%) | 53 (6.6%) | 2 (1.6%) |
| Main finding for red code definition, n (%) | |||
| PAT | 598 (64%) | 472 (58.4%) | 126 (100%) |
| SatO2 | 301 (32.2%) | 301 (37.2%) | 0 (0%) |
| HR | 23 (2.5%) | 23 (2.8%) | 0 (0%) |
| RR | 12 (1.3%) | 12 (1.6%) | 0 (0%) |
| Comorbidities, n (%) | |||
| Yes | 355 (38%) | 344 (42.6%) | 11 (8.7%) |
| No | 577 (61.8%) | 463 (57.3%) | 114 (90.5%) |
| Not reported | 2 (0.2%) | 1 (0.1%) | 1 (0.8%) |
| Variable | Total | Medical | Surgical |
|---|---|---|---|
| AVPU, n (%) | |||
| A | 598 (64%) | 538 (66.7%) | 60 (47.6%) |
| V | 63 (6.8%) | 52 (6.4%) | 11 (8.7%) |
| P | 119 (12.7%) | 103 (12.7%) | 16 (12.7%) |
| U | 153 (16.4%) | 115 (14.2%) | 38 (30.2%) |
| Not reported | 1 (0.1%) | 0 (0%) | 1 (0.8%) |
| Skin, n (%) | |||
| Normal | 598 (64%) | 578 (71.5%) | 20 (15.9%) |
| Pathologic | 273 (29.2%) | 187 (23.2%) | 86 (68.2%) |
| Not reported | 63 (6.8%) | 43 (5.3%) | 20 (15.9%) |
| Breathing, n (%) | |||
| Spontaneous | 718 (76.9%) | 633 (78.3%) | 85 (67.5%) |
| Oxygen support | 159 (17%) | 152 (18.8%) | 7 (5.5%) |
| Intubation | 56 (6%) | 23 (2.9%) | 33 (26.2%) |
| Not reported | 1 (0.1%) | 0 (0%) | 1 (0.8%) |
| Blood pressure, n (%) | |||
| Normal | 162 (17.3%) | 109 (13.5%) | 53 (42.1%) |
| Pathologic | 39 (4.2%) | 26 (3.2%) | 13 (10.3%) |
| Not reported | 733 (78.5%) | 673 (83.3%) | 60 (47.6%) |
| Capillary refill time, n (%) | |||
| Normal | 233 (24.9%) | 224 (27.7%) | 9 (7.1%) |
| Pathologic | 64 (6.9%) | 60 (7.4%) | 4 (3.2%) |
| Not reported | 637 (68.2%) | 524 (64.9%) | 113 (89.7%) |
| Management | Medical | Surgical |
|---|---|---|
| Vascular access, n (%) | ||
| PVC | 582 (72.1%) | 110 (87.3%) |
| IO | 5 (0.6%) | 1 (0.7%) |
| CVC | 1 (0.1%) | 0 (0%) |
| IO + PVC | 12 (1.4%) | 3 (2.4%) |
| No access | 202 (25.1%) | 5 (4%) |
| Blood count, n (%) | ||
| Not performed | 254 (31.4%) | 28 (22.2%) |
| Performed | 554 (68.6%) | 98 (77.8%) |
| Pathologic | 190 (34%) | 49 (50%) |
| Blood gas analysis, n (%) | ||
| Not performed | 172 (21.3%) | 53 (42.1%) |
| Performed | 636 (78.7%) | 73 (57.9%) |
| Pathologic | 309 (48.6%) | 20 (27%) |
| Electrocardiogram, n (%) | ||
| Not performed | 637 (78.8%) | 119 (94.4%) |
| Performed | 171 (21.2%) | 7 (5.6%) |
| Pathologic | 28 (16.4%) | 2 (28.6%) |
| Ultrasound, n (%) | ||
| Not performed | 553 (68.4%) | 80 (63.5%) |
| Performed | 255 (31.6%) | 46 (36.5%) |
| Pathologic | 107 (42%) | 13 (28.3%) |
| CT scan, n (%) | ||
| Not performed | 726 (89.9%) | 45 (35.7%) |
| Performed | 82 (10.1%) | 81 (64.3%) |
| Pathologic | 25 (30.5%) | 55 (68%) |
| Anesthesiologic consultation, n (%) | ||
| Yes | 206 (25.5%) | 68 (54%) |
| No | 602 (74.5%) | 58 (46%) |
| Therapeutic Approach | Total | Medical | Surgical |
|---|---|---|---|
| Oxygen or ventilation, n (%) | 548 (58.7%) | 521 (64.5%) | 27 (21.4%) |
| Crystalloids, n (%) | 106 (11.3%) | 79 (9.8%) | 27 (21.4%) |
| Colloids, n (%) | 28 (3%) | 20 (2.5%) | 8 (6.3%) |
| Glucagon or insulin, n (%) | 26 (2.8%) | 25 (3.1%) | 1 (0.8%) |
| Electric therapy, n (%) | 0 (0%) | 0 (0%) | 0 (0%) |
| Antiseizure, n (%) | 98 (10.5%) | 96 (11.9%) | 2 (1.6%) |
| Sedatives, n (%) | 47 (5%) | 26 (3.2%) | 21 (16.7%) |
| Psychoactive drugs, n (%) | 11 (1.2%) | 11 (1.4%) | 0 (0%) |
| Antibiotics or antivirals, n (%) | 172 (18.4%) | 155 (19.2%) | 17 (13.5%) |
| Antipyretics or analgesics, n (%) | 269 (28.8%) | 233 (28.8%) | 36 (28.6%) |
| Antiemetics, n (%) | 23 (2.5%) | 17 (2.1%) | 6 (4.8%) |
| Steroids, n (%) | 260 (27.8%) | 257 (31.8%) | 3 (2.4%) |
| Drugs acting or airways, n (%) | 376 (40.2%) | 376 (46.5%) | 0 (0%) |
| Diuretics, n (%) | 12 (1.3%) | 12 (1.5%) | 0 (0%) |
| Cardioactive drugs, n (%) | 27 (2.9%) | 23 (2.8%) | 4 (3.2%) |
| Dressings, n (%) | 24 (2.6%) | 1 (0.1%) | 23 (18.3%) |
| Admission Modality | Total | Medical | Surgical |
|---|---|---|---|
| Pediatric intensive care unit, n (%) | |||
| No | 759 (81.3%) | 688 (85.1%) | 71 (56.3%) |
| Yes | 175 (18.7%) | 120 (14.9%) | 55 (43.7%) |
| Short observation unit, n (%) | |||
| No | 660 (70.7%) | 539 (66.7%) | 121 (96%) |
| Yes | 274 (29.3%) | 269 (33.3%) | 5 (4%) |
| Hospital ward, n (%) | |||
| No | 232 (24.8%) | 216 (26.7%) | 16 (12.7%) |
| Yes | 702 (75.2%) | 592 (73.3%) | 110 (87.3%) |
| Main Complaint | Mean Duration of Hospitalization, Days (SD) |
|---|---|
| Respiratory | 12 (±17) |
| Neuropsychiatric | 11 (±16) |
| Traumatic | 14 (±17) |
| Cardiologic | 10 (±14) |
| Metabolic | 7 (±4) |
| Surgical | 18 (±17) |
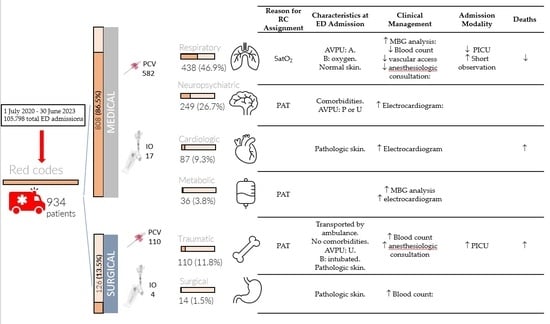
| Pathway | Reason for RC Assignment | Characteristics at ED Admission | Clinical Management | Therapeutic Approach | Admission Modality | Deaths |
|---|---|---|---|---|---|---|
| Respiratory (438 patients, 46.9%) | SatO2 | AVPU: A. B: oxygen. Normal skin. | MBG analysis: more than expected. Blood count, vascular access, and anesthesiologic consultation: less than expected. | Oxygen Steroids Drugs acting on airways Antibiotics and antivirals | PICU: less than expected. Short observation unit: more than expected. | Less than expected |
| Neuropsychiatric (249 patients, 26.7%) | PAT | Comorbidities. AVPU: P or U | Electrocardiogram: more than expected | Antiseizure Psychoactive drugs Antiemetics | ||
| Traumatic (110 patients, 11.8%) | PAT | Transported by ambulance. No comorbidities. AVPU: U. B: intubated. Pathologic skin. | Blood count and anesthesiologic consultation: more than expected. | Crystalloids Colloids Sedatives Dressings | PICU: more than expected | More than expected |
| Cardiologic (87 patients, 9.3%) | Pathologic skin. | Electrocardiogram: more than expected | Crystalloids Colloids Cardioactive drugs | More than expected | ||
| Metabolic (36 patients, 3.8%) | PAT | MBG analysis and electrocardiogram: more than expected | Crystalloids Glucagon Insulin | |||
| Surgical (14 patients, 1.5%) | Pathologic skin. | Blood count: more than expected | Dressings |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bertone, S.; Denina, M.; Pagano, M.; Delmonaco, A.G.; Castagno, E.; Bondone, C. Red Code Management in a Pediatric Emergency Department: A Retrospective Study. Children 2024, 11, 462. https://doi.org/10.3390/children11040462
Bertone S, Denina M, Pagano M, Delmonaco AG, Castagno E, Bondone C. Red Code Management in a Pediatric Emergency Department: A Retrospective Study. Children. 2024; 11(4):462. https://doi.org/10.3390/children11040462
Chicago/Turabian StyleBertone, Serena, Marco Denina, Manuela Pagano, Angelo Giovanni Delmonaco, Emanuele Castagno, and Claudia Bondone. 2024. "Red Code Management in a Pediatric Emergency Department: A Retrospective Study" Children 11, no. 4: 462. https://doi.org/10.3390/children11040462
APA StyleBertone, S., Denina, M., Pagano, M., Delmonaco, A. G., Castagno, E., & Bondone, C. (2024). Red Code Management in a Pediatric Emergency Department: A Retrospective Study. Children, 11(4), 462. https://doi.org/10.3390/children11040462